Prevalence of Dry Eye Symptoms and Associated Risk Factors among University Students in Poland
Abstract
1. Introduction
2. Materials and Methods
2.1. Simple Size Calculation
2.2. Study Design
2.3. Dry Eye Symptom Questionnaire Assessment
2.4. Statistical Analysis
3. Results
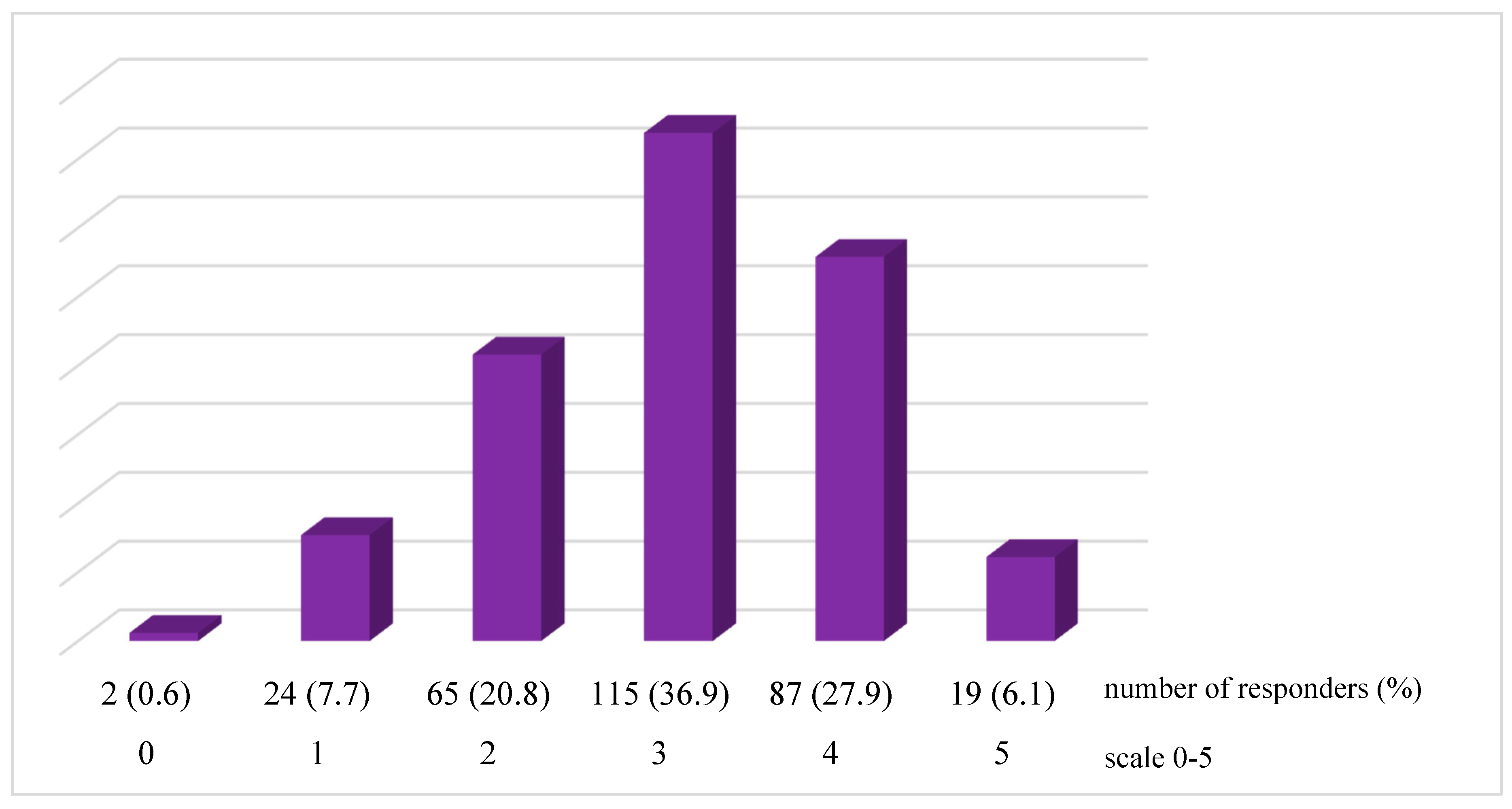
3.1. Dry Eye Symptoms Prevalence
3.2. Socio-Demographic and Clinical Risk Factors
3.3. Behavioural and Environmental Risk Factors
3.4. Medications and Comorbidities
3.5. Correlation of the OSDI and DEQ-5 Questionnaires
4. Discussion
4.1. Dry Eye Disease Prevalence
4.2. Socio-Demographical and Clinical Factors
4.3. Behavioral and Environmental Factors
4.4. Comorbidities and Medications
4.5. Correlation of the OSDI and DEQ-5 Questionnaires
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Stapleton, F.; Alves, M.; Bunya, V.Y.; Jalbert, I.; Lekhanont, K.; Malet, F.; Na, K.-S.; Schaumberg, D.; Uchino, M.; Vehof, J.; et al. TFOS DEWS II Epidemiology Report. Ocul. Surf. 2017, 15, 334–365. [Google Scholar] [CrossRef]
- Craig, J.P.; Nichols, K.K.; Akpek, E.K.; Caffery, B.; Dua, H.S.; Joo, C.-K.; Liu, Z.; Nelson, J.D.; Nichols, J.J.; Tsubota, K.; et al. TFOS DEWS II Definition and Classification Report. Ocul. Surf. 2017, 15, 276–283. [Google Scholar] [CrossRef]
- Clayton, J.A. Dry Eye. N. Engl. J. Med. 2018, 378, 2212–2223. [Google Scholar] [CrossRef] [PubMed]
- Benítez-Del-Castillo, J.; Labetoulle, M.; Baudouin, C.; Rolando, M.; Akova, Y.A.; Aragona, P.; Geerling, G.; Merayo-Lloves, J.; Messmer, E.M.; Boboridis, K. Visual acuity and quality of life in dry eye disease: Proceedings of the OCEAN group meeting. Ocul. Surf. 2017, 15, 169–178. [Google Scholar] [CrossRef] [PubMed]
- Koh, S. Mechanisms of Visual Disturbance in Dry Eye. Cornea 2016, 35 (Suppl. S1), S83–S88. [Google Scholar] [CrossRef] [PubMed]
- Morthen, M.K.; Magno, M.S.; Utheim, T.P.; Snieder, H.; Hammond, C.J.; Vehof, J. The physical and mental burden of dry eye disease: A large population-based study investigating the relationship with health-related quality of life and its determinants. Ocul. Surf. 2021, 21, 107–117. [Google Scholar] [CrossRef] [PubMed]
- Kaštelan, S.; Bakija, I.; Bogadi, M.; Orešković, I.; Kasun, B.; Gotovac, M.; Gverović Antunica, A. Psychiatric Disorders and Dry Eye Disease–A Transdisciplinary Approach. Psychiatr. Danub. 2021, 33, 580–587. [Google Scholar]
- He, Q.; Chen, Z.; Xie, C.; Liu, L.; Yang, H.; Wei, R. Relationship Between Dry Eye Disease and Emotional Disorder: The Mediating Effect of Health Anxiety. Front. Public Health 2022, 10, 771554. [Google Scholar] [CrossRef]
- Yamanishi, R.; Uchino, M.; Kawashima, M.; Uchino, Y.; Yokoi, N.; Tsubota, K. Characteristics of Individuals with Dry Eye Symptoms Without Clinical Diagnosis: Analysis of a Web-Based Survey. J. Clin. Med. 2019, 8, 721. [Google Scholar] [CrossRef]
- Vehof, J.; Snieder, H.; Jansonius, N.; Hammond, C.J. Prevalence and risk factors of dry eye in 79,866 participants of the population-based Lifelines cohort study in the Netherlands. Ocul. Surf. 2021, 19, 83–93. [Google Scholar] [CrossRef]
- Fjaervoll, K.; Fjaervoll, H.; Magno, M.; Nøland, S.T.; Dartt, D.A.; Vehof, J.; Utheim, T.P. Review on the possible pathophysiological mechanisms underlying visual display terminal-associated dry eye disease. Acta Ophthalmol. 2022, 100, 867–877. [Google Scholar] [CrossRef] [PubMed]
- Neti, N.; Prabhasawat, P.; Chirapapaisan, C.; Ngowyutagon, P. Provocation of dry eye disease symptoms during COVID-19 lockdown. Sci. Rep. 2021, 11, 24434. [Google Scholar] [CrossRef] [PubMed]
- Walt, J.G.; Rowe, M.M.; Stern, K.L. Evaluating the functional Impact of Dry Eye: The Ocular Surface Disease Index. Drug Inf. J. 1997, 31, 1436. [Google Scholar]
- Chalmers, R.L.; Begley, C.G.; Caffery, B. Validation of the 5-Item Dry Eye Questionnaire (DEQ-5): Discrimination across self-assessed severity and aqueous tear deficient dry eye diagnoses. Cont. Lens Anterior Eye 2010, 33, 55–60. [Google Scholar] [CrossRef] [PubMed]
- Schiffman, R.M.; Christianson, M.D.; Jacobsen, G.; Hirsch, J.D.; Reis, B.L. Reliability and validity of the Ocular Surface Disease Index. Arch. Ophthalmol. 2000, 118, 615–621. [Google Scholar] [CrossRef]
- Talens-Estarelles, C.; Sanchis-Jurado, V.; Esteve-Taboada, J.J.; Pons, Á.M.; García-Lázaro, S. How do different digital displays affect the ocular surface? Optom. Vis. Sci. 2020, 97, 1070–1079. [Google Scholar] [CrossRef]
- Carbonell, X.; Chamarro, A.; Oberst, U.; Rodrigo, B.; Prades, M. Problematic Use of the Internet and Smartphones in University Students: 2006–2017. Int. J. Environ. Res. Public Health 2018, 15, 475. [Google Scholar] [CrossRef]
- Yang, I.; Wakamatsu, T.; Sacho, I.; Fazzi, J.H.; de Aquino, A.C.; Ayub, G.; Rebello, P.A.; Gomes, J.; Alves, M. Prevalence and associated risk factors for dry eye disease among Brazilian undergraduate students. PLoS ONE 2021, 16, e0259399. [Google Scholar] [CrossRef]
- Aćimović, L.; Stanojlović, S.; Kalezić, T.; Dačić Krnjaja, B. Evaluation of dry eye symptoms and risk factors among medical students in Serbia. PLoS ONE 2022, 17, e0275624. [Google Scholar] [CrossRef]
- Alkabbani, S.; Jeyaseelan, L.; Rao, A.P.; Thakur, S.P.; Warhekar, P.T. The prevalence, severity, and risk factors for dry eye disease in Dubai–a cross sectional study. BMC Ophthalmol. 2021, 21, 219. [Google Scholar] [CrossRef]
- de Paiva, C.S. Effects of Aging in Dry Eye. Int. Ophthalmol. Clin. 2017, 57, 47–64. [Google Scholar] [CrossRef]
- Alkhaldi, S.A.; Allam, K.H.; Radwan, M.A.; Sweeny, L.E.; Alshammeri, S. Estimates of dry eye disease in Saudi Arabia based on a short questionnaire of prevalence, symptoms, and risk factors: The Twaiq Mountain Eye Study I. Contact. Lens Anterior Eye 2022, 2022, 101770. [Google Scholar] [CrossRef] [PubMed]
- Sullivan, D.A.; Rocha, E.M.; Aragona, P.; Clayton, J.A.; Ding, J.; Golebiowski, B.; Hampel, U.; McDermott, A.M.; Schaumberg, D.A.; Srinivasan, S.; et al. TFOS DEWS II Sex, Gender, and Hormones Report. Ocul. Surf. 2017, 15, 284–333. [Google Scholar] [CrossRef]
- Cifuentes-González, C.; Uribe-Reina, P.; Reyes-Guanes, J.; Muñoz-Ortiz, J.; Muñoz-Vargas, P.T.; Rojas-Carabali, W.; Nova-Florián, D.V.; De-Los-Ríos, A.S.; Mantilla-Hernández, R.D.; de-la-Torre, A. Ocular Manifestations Related to Antibodies Positivity and Inflammatory Biomarkers in a Rheumatological Cohort. Clin. Ophthalmol. 2022, 16, 2477–2490. [Google Scholar] [CrossRef] [PubMed]
- Sonkodi, B.; Resch, M.D.; Hortobágyi, T. Is the Sex Difference a Clue to the Pathomechanism of Dry Eye Disease? Watch out for the NGF-TrkA-Piezo2 Signaling Axis and the Piezo2 Channelopathy. J. Mol. Neurosci. 2022, 72, 1598–1608. [Google Scholar] [CrossRef]
- Boga, A.; Stapleton, F.; Briggs, N.; Golebiowski, B. Daily fluctuations in ocular surface symptoms during the normal menstrual cycle and with the use of oral contraceptives. Ocul. Surf. 2019, 17, 763–770. [Google Scholar] [CrossRef] [PubMed]
- He, B.; Iovieno, A.; Etminan, M.; Kezouh, A.; Yeung, S.N. Effects of hormonal contraceptives on dry eye disease: A population-based study. Eye 2022, 36, 634–638. [Google Scholar] [CrossRef] [PubMed]
- Moon, J.H.; Kim, K.W.; Moon, N.J. Smartphone use is a risk factor for pediatric dry eye disease according to region and age: A case control study. BMC Ophthalmol. 2016, 16, 188. [Google Scholar] [CrossRef] [PubMed]
- Donthineni, P.R.; Kammari, P.; Shanbhag, S.S.; Singh, V.; Das, A.V.; Basu, S. Incidence, demographics, types and risk factors of dry eye disease in India: Electronic medical records driven big data analytics report I. Ocul. Surf. 2019, 17, 250–256. [Google Scholar] [CrossRef]
- Osae, E.A.; Ablordeppey, R.K.; Horstmann, J.; Kumah, D.B.; Steven, P. Clinical Dry Eye and Meibomian Gland Features Among Dry Eye Patients in Rural and Urban Ghana. Clin. Ophthalmol. 2020, 14, 4055–4063. [Google Scholar] [CrossRef] [PubMed]
- Ocansey, S.; Kumi-Kyereme, A.; Awusabo-Asare, K.; Ilechie, A.A.; Boadi-Kusi, S.B.; Abraham, C.H. Utilization of eye care services among Ghanaian elderly population: Evidence from a peri-urban community. Ophthalmol. Res. 2013, 1, 89–101. [Google Scholar] [CrossRef]
- AlDarrab, A.; Khojah, A.A.; Al-Ghazwi, M.H.; Al-Haqbani, Y.J.; Al-Qahtani, N.M.; Al-Ajmi, M.N.; Alenezi, S.H.; Almasoud, M.K.; Al-Yahya, A.F. Magnitude and Determinants of Computer Vision Syndrome among College Students at a Saudi University. Middle East Afr. J. Ophthalmol. 2022, 28, 252–256. [Google Scholar] [CrossRef] [PubMed]
- Ekemiri, K.; Ezinne, N.; Kamalodeen, K.; Pierre, K.; Lalla, B.; Amiebenomo, O.; van Staden, D.; Zeried, F.; Ekemiri, C.; Agho, K.E.; et al. Online e-learning during the COVID-19 lockdown in Trinidad and Tobago: Prevalence and associated factors with ocular complaints among schoolchildren aged 11–19 years. PeerJ 2022, 10, e13334. [Google Scholar] [CrossRef] [PubMed]
- Koh, S. Contact Lens Wear and Dry Eye: Beyond the Known. Asia Pac. J. Ophthalmol. 2020, 9, 498–504. [Google Scholar] [CrossRef]
- Lim, C.H.L.; Stapleton, F.; Mehta, J.S. Review of Contact Lens-Related Complications. Eye Contact Lens Sci. Clin. Pr. 2018, 44, S1–S10. [Google Scholar] [CrossRef] [PubMed]
- Kojima, T. Contact Lens-Associated Dry Eye Disease: Recent Advances Worldwide and in Japan. Investig. Ophthalmol. Vis. Sci. 2018, 59, DES102–DES108. [Google Scholar] [CrossRef]
- Fjaervoll, H.; Fjaervoll, K.; Magno, M.; Moschowits, E.; Vehof, J.; Dartt, D.A.; Wang, M.; Tien, L.; Han, A.; Lee, J.M.; et al. Impact of blinking on ocular surface and tear film parameters. Ocul. Surf. 2018, 16, 424–429. [Google Scholar]
- Fjaervoll, H.; Fjaervoll, K.; Magno, M.; Moschowits, E.; Vehof, J.; Dartt, D.A.; Utheim, T.P. The association between visual display terminal use and dry eye: A review. Acta Ophthalmol. 2022, 100, 357–375. [Google Scholar] [CrossRef]
- Talens-Estarelles, C.; Cerviño, A.; García-Lázaro, S.; Fogelton, A.; Sheppard, A.; Wolffsohn, J.S. The effects of breaks on digital eye strain, dry eye and binocular vision: Testing the 20-20-20 rule [published online ahead of print, 2022 Aug 10]. Contact Lens Anterior Eye 2022, 10, 101744. [Google Scholar] [CrossRef]
- Jones, L.; Downie, L.E.; Korb, D.; Benitez-Del-Castillo, J.M.; Dana, R.; Deng, S.X.; Dong, P.N.; Geerling, G.; Hida, R.Y.; Liu, Y.; et al. TFOS DEWS II Management and Therapy Report. Ocul. Surf. 2017, 15, 575–628. [Google Scholar] [CrossRef]
- Bazeer, S.; Jansonius, N.; Snieder, H.; Hammond, C.; Vehof, J. The relationship between occupation and dry eye. Ocul. Surf. 2019, 17, 484–490. [Google Scholar] [CrossRef]
- Idarraga, M.A.; Guerrero, J.S.; Mosle, S.G.; Miralles, F.; Galor, A.; Kumar, N. Relationships Between Short-Term Exposure to an Indoor Environment and Dry Eye (DE) Symptoms. J. Clin. Med. 2020, 9, 1316. [Google Scholar] [CrossRef]
- Xu, L.; Zhang, W.; Zhu, X.Y.; Suo, T.; Fan, X.Q.; Fu, Y. Smoking and the risk of dry eye: A meta-analysis. Int. J. Ophthalmol. 2016, 9, 1480–1486. [Google Scholar]
- Mohidin, N.; Jaafar, A.B. Effect of Smoking on Tear Stability and Corneal Surface. J. Curr. Ophthalmol. 2020, 32, 232–237. [Google Scholar] [CrossRef] [PubMed]
- Makrynioti, D.; Zagoriti, Z.; Koutsojannis, C.; Morgan, P.B.; Lagoumintzis, G. Ocular conditions and dry eye due to traditional and new forms of smoking: A review. Contact Lens Anterior Eye 2020, 43, 277–284. [Google Scholar] [CrossRef]
- Kaštelan, S.; Bakija, I.; Bogadi, M.; Gverović Antunica, A.; Gotovac, M.; Šimunović Filipčić, I. Mental Disorders as Influencing Factors for Discordances in the Signs and Symptoms of Dry Eye Disease. Psychiatria Danubina 2021, 33 (Suppl S4), 588–595. [Google Scholar]
- Qian, L.; Wei, W. Identified risk factors for dry eye syndrome: A systematic review and meta-analysis. PLoS ONE 2022, 17, e0271267. [Google Scholar] [CrossRef]
- Liang, C.Y.; Cheang, W.M.; Wang, C.Y.; Lin, K.H.; Wei, L.C.; Chen, Y.Y.; Shen, Y.C. The association of dry eye syndrome and psychiatric disorders: A nationwide population-based cohort study. BMC Ophthalmol. 2020, 20, 123. [Google Scholar] [CrossRef] [PubMed]
- Asiedu, K.; Dzasimatu, S.K.; Kyei, S. Impact of Dry Eye on Psychosomatic Symptoms and Quality of Life in a Healthy Youthful Clinical Sample. Eye Contact Lens 2018, 44 (Suppl. S2), S404–S409. [Google Scholar] [CrossRef] [PubMed]
- Liu, Z.; Sun, S.; Sun, X.; Wu, Y.; Huang, Y. Differences of Anxiety and Depression in Dry Eye Disease Patients According to Age Groups. Front. Psychiatry 2022, 13, 930714. [Google Scholar] [CrossRef]
- Basilious, A.; Xu, C.Y.; Malvankar-Mehta, M.S. Dry eye disease and psychiatric disorders: A systematic review and meta-analysis. Eur. J. Ophthalmol. 2022, 32, 1872–1889. [Google Scholar] [CrossRef] [PubMed]
- Kitazawa, M.; Sakamoto, C.; Yoshimura, M.; Kawashima, M.; Inoue, S.; Mimura, M.; Tsubota, K.; Negishi, K.; Kishimoto, T. The Relationship of Dry Eye Disease with Depression and Anxiety: A Naturalistic Observational Study. Transl. Vis. Sci. Technol. 2018, 7, 35. [Google Scholar] [CrossRef]
- Mrugacz, M.; Ostrowska, L.; Bryl, A.; Szulc, A.; Zelazowska-Rutkowska, B.; Mrugacz, G. Pro-inflammatory cytokines associated with clinical severity of dry eye disease of patients with depression. Adv. Med. Sci. 2017, 62, 338–344. [Google Scholar] [CrossRef] [PubMed]
- Tiskaoglu, N.S.; Yazıcı, A.; Karlıdere, T.; Sari, E.; Oguz, E.Y.; Musaoglu, M.; Aslan, S.; Samet Ermiş, S. Dry Eye Disease in Patients with Newly Diagnosed Depressive Disorder. Curr. Eye Res. 2017, 42, 672–676. [Google Scholar] [CrossRef] [PubMed]
- Rakofsky, J.J.; Rakofsky, S.I.; Dunlop, B.W. Dry Those Crying Eyes: The Role of Depression and Antidepressants in Dry Eye Disease. J. Clin. Psychopharmacol. 2021, 41, 295–303. [Google Scholar] [CrossRef]
- Constable, P.A.; Al-Dasooqi, D.; Bruce, R.; Prem-Senthil, M. A Review of Ocular Complications Associated with Medications Used for Anxiety, Depression, and Stress. Clin. Optom. 2022, 14, 13–25. [Google Scholar] [CrossRef]
- Ismayilov, A.S.; Celikel, G. Effects of tricyclic antidepressants, selective serotonin reuptake inhibitors, and selective serotonin-norepinephrine reuptake inhibitors on the ocular surface. Arq. Bras. Oftalmol. 2019, 85, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Park, J.S.Y.; Sharma, R.A.; Sharma, V. Ophthalmic adverse effects of lithium. Int. Clin. Psychopharmacol. 2020, 35, 69–73. [Google Scholar] [CrossRef]
- Hasan, Z.A. Dry eye syndrome risk factors: A systemic review. Saudi J. Ophthalmol. 2022, 35, 131–139. [Google Scholar] [CrossRef]
- Leonardi, A.; Modugno, R.L.; Salami, E. Allergy and Dry Eye Disease. Ocul. Immunol. Inflamm. 2021, 29, 1168–1176. [Google Scholar] [CrossRef]
- Villani, E.; Rabbiolo, G.; Nucci, P. Ocular allergy as a risk factor for dry eye in adults and children. Curr. Opin. Allergy Clin. Immunol. 2018, 18, 398–403. [Google Scholar] [CrossRef]
- Lee, H.K.; Lee, S.M.; Lee, D.I. Corneal Lymphangiogenesis: Current Pathophysiological Understandings and Its Functional Role in Ocular Surface Disease. Int. J. Mol. Sci. 2021, 22, 11628. [Google Scholar] [CrossRef] [PubMed]
- Mastropasqua, R.; Agnifili, L.; Fasanella, V.; Nubile, M.; Gnama, A.A.; Falconio, G.; Perri, P.; Di Staso, S.; Mariotti, C. The Conjunctiva-Associated Lymphoid Tissue in Chronic Ocular Surface Diseases. Microsc. Microanal. 2017, 23, 697–707. [Google Scholar] [CrossRef]
- Huang, Q.; Zheng, Y.; Zhang, C.; Wang, W.; Liao, T.; Xiao, X.; Wang, J.; Wang, J. Association between asthma and dry eye disease: A meta-analysis based on observational studies. BMJ Open 2021, 11, e045275. [Google Scholar] [CrossRef]
- Govind, K.; Whang, K.; Khanna, R.; Scott, A.W.; Kwatra, S.G. Atopic dermatitis is associated with increased prevalence of multiple ocular comorbidities. J. Allergy Clin. Immunol. Pr. 2019, 7, 298–299. [Google Scholar] [CrossRef]
- Wong, J.; Lan, W.; Ong, L.M.; Tong, L. Non-hormonal systemic medications and dry eye. Ocul. Surf. 2011, 9, 212–226. [Google Scholar] [CrossRef]
- Kesarwani, D.; Rizvi, S.W.A.; Khan, A.A.; Amitava, A.K.; Vasenwala, S.M.; Siddiqui, Z. Tear film and ocular surface dysfunction in diabetes mellitus in an Indian population. Indian J. Ophthalmol. 2017, 65, 301–304. [Google Scholar] [PubMed]
- Paulsen, A.J.; Cruickshanks, K.J.; Fischer, M.E.; Huang, G.H.; Klein, B.E.; Klein, R.; Dalton, D.S. Dry eye in the beaver dam offspring study: Prevalence, risk factors, and health-related quality of life. Am. J. Ophthalmol. 2014, 157, 799–806. [Google Scholar] [CrossRef]
- Guannan, H.; Long, S.; Xia, H.; Dong, W.; Shaozhen, Z. Clinical characterisation and cytological study of dry eye in patients with autoimmune disease. J. Pak. Med. Assoc. 2018, 68, 353–358. [Google Scholar] [PubMed]
- Qi, Y.; Wan, Y.; Li, T.; Zhang, M.; Song, Y.; Hu, Y.; Sun, Y.; Li, L. Comparison of the Ocular Microbiomes of Dry Eye Patients With and Without Autoimmune Disease. Front. Cell. Infect. Microbiol. 2021, 11, 716867. [Google Scholar] [CrossRef]
- Bjordal, O.; Norheim, K.B.; Rødahl, E.; Jonsson, R.; Omdal, R. Primary Sjögren’s syndrome and the eye. Surv. Ophthalmol. 2020, 65, 119–132. [Google Scholar] [CrossRef] [PubMed]
- Altin Ekin, M.; Karadeniz Ugurlu, S.; Egrilmez, E.D.; Oruk, G.G. Ocular Surface Changes in Hashimoto’s Thyroiditis without Thyroid Ophthalmopathy. Eye Contact Lens 2021, 47, 32–37. [Google Scholar] [CrossRef]
- Selter, J.H.; Gire, A.I.; Sikder, S. The relationship between Graves’ ophthalmopathy and dry eye syndrome. Clin. Ophthalmol. 2015, 9, 57–62. [Google Scholar]
- Zhang, X.; Jeyalatha, M.V.; Qu, Y.; He, X.; Ou, S.; Bu, J.; Jia, C.; Wang, J.; Wu, H.; Liu, Z.; et al. Dry Eye Management: Targeting the Ocular Surface Microenvironment. Int. J. Mol. Sci. 2017, 18, 1398. [Google Scholar] [CrossRef] [PubMed]
- Chen, L.; Deng, C.; Chen, X.; Zhang, X.; Chen, B.; Yu, H.; Qin, Y.; Xiao, K.; Zhang, H.; Sun, X. Ocular manifestations and clinical characteristics of 535 cases of COVID-19 in Wuhan, China: A cross-sectional study. Acta Ophthalmol. 2020, 98, 951–959. [Google Scholar] [CrossRef] [PubMed]
- Guan, W.J.; Ni, Z.Y.; Hu, Y.; Liang, W.H.; Ou, C.Q.; He, J.X.; Liu, L.; Shan, H.; Lei, C.L.; Hui, D.S.C.; et al. China Medical Treatment Expert Group for COVID-19. Clinical Characteristics of Coronavirus Disease 2019 in China. N. Engl. J. Med. 2020, 382, 1708–1720. [Google Scholar] [CrossRef]
- Wu, P.; Duan, F.; Luo, C.; Liu, Q.; Qu, X.; Liang, L.; Wu, K. Characteristics of Ocular Findings of Patients with Coronavirus Disease 2019 (COVID-19) in Hubei Province, China. JAMA Ophthalmol. 2020, 138, 575–578. [Google Scholar] [CrossRef]

| Investigated Trait | n | % |
|---|---|---|
| Gender: | ||
| Female | 219 | 70.2 |
| Male | 93 | 29.8 |
| Age group (years): | ||
| <20 | 17 | 5.4 |
| 20–25 | 238 | 76.3 |
| 26–30 | 44 | 14.1 |
| >30 | 13 | 4.2 |
| Place of residence: | ||
| Metropolitan area | 241 | 77.2 |
| Rural area | 71 | 22.8 |
| Field of study (faculty): | ||
| Medicine | 143 | 45.8 |
| Non-medical | 169 | 54.2 |
| Refractive errors: | ||
| None | 108 | 34.9 |
| Myopia (alone) | 94 | 30.4 |
| Hyperopia (alone) | 13 | 4.2 |
| Astigmatism (alone) | 24 | 7.8 |
| Myopia and astigmatism | 67 | 21.7 |
| Hyperopia and astigmatism | 3 | 1.0 |
| Use of contact lenses (overall): | 93 | 29.8 |
| ≤1 year | 19 | 20.4 |
| 2–3 years | 17 | 18.3 |
| Over 3 years | 57 | 61.3 |
| Contact lens tolerance: | ||
| Good | 79 | 85.9 |
| Not good | 13 | 14.1 |
| Regular, daily basis use tobacco products | 74 | 23.7 |
| History of SARS-CoV-2 infection | 173 | 55.4 |
| Vaccination against COVID-19 | ||
| No | 41 | 13.1 |
| Full dose, and a third booster | 133 | 42.6 |
| Full dose (2 of two-dose, or 1 single-dose vaccine) | 134 | 43.0 |
| Incomplete dose (1 dose of two-dose vaccine) | 4 | 1.3 |
| Pharmaceutical Agent | Frequency | DEQ-5 Score | OSDI Score | |||||
|---|---|---|---|---|---|---|---|---|
| n | % | M | SD | p-Value | M | SD | p-Value | |
| Beta-blockers | 6 | 1.9 | 11.2 | 6.6 | =0.159 | 31.6 | 35.4 | =0.482 |
| Psychotropics | 38 | 12.2 | 9.4 | 5.2 | =0.014 | 30.1 | 23.1 | =0.002 |
| Anti-histamines | 33 | 10.6 | 9.4 | 5.7 | =0.054 | 28.5 | 23.3 | =0.024 |
| Analgesics | 18 | 5.8 | 7.7 | 5.8 | =0.923 | 30.4 | 26.7 | =0.062 |
| Glucocorticosteroids | 5 | 1.6 | 13 | 5.2 | =0.026 | 44.8 | 33.4 | =0.024 |
| Contraceptives | 47 | 15.1 | 9.1 | 5.3 | =0.023 | 24.7 | 20.6 | =0.127 |
| Other hormones | 34 | 10.9 | 8.8 | 5.4 | =0.170 | 26.7 | 23.7 | =0.152 |
| Health Condition | Frequency | DEQ-5 Score | OSDI Score | |||||
|---|---|---|---|---|---|---|---|---|
| n | % | M | SD | p-Value | M | SD | p-Value | |
| Arterial hypertension | 10 | 3.2 | 10.1 | 6.2 | =0.165 | 29.6 | 29.0 | =0.299 |
| Heart disease | 6 | 1.9 | 9.0 | 7.5 | =0.778 | 30.7 | 35.7 | =0.620 |
| Depression | 37 | 11.9 | 9.7 | 5.2 | =0.005 | 30.6 | 20.8 | <0.001 |
| Mental disease | 17 | 5.4 | 9.6 | 5.9 | =0.127 | 34.0 | 28.0 | =0.019 |
| Thyroid disease | 37 | 11.9 | 8.5 | 5.4 | =0.219 | 26.8 | 24.8 | =0.155 |
| Diabetes | 8 | 2.6 | 13.9 | 5.1 | =0.001 | 44.8 | 29.7 | =0.008 |
| Allergy | 77 | 24.7 | 8.7 | 4.7 | =0.023 | 25.4 | 19.6 | =0.002 |
| Acne | 13 | 4.2 | 9.5 | 6.2 | =0.242 | 30.3 | 29.0 | =0.210 |
| Independent Trait | Normal | Mild | Moderate | Severe | aOR p-Value | ||||
|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | ||
| How many hours a day do you spend in close proximity to the screen of an electronic device, e.g., mobile phone, computer, tablet, reader (not taking into account a TV set)? | |||||||||
| <4 | 29 | 21.6 | 11 | 14.3 | 6 | 13.3 | 3 | 5.4 | =1.37 =0.006 |
| 4–8 | 65 | 48.5 | 49 | 63.6 | 24 | 53.4 | 25 | 44.6 | |
| >8 | 40 | 29.9 | 17 | 22.1 | 15 | 33.3 | 28 | 50.0 | |
| How many hours a day do you spend in front of the screen of an electronic device (not taking into account a TV set), without taking breaks? | |||||||||
| <1 | 32 | 23.9 | 6 | 7.8 | 8 | 17.8 | 5 | 8.9 | =1.16 =0.016 |
| 1–2 | 56 | 41.8 | 43 | 55.8 | 19 | 42.2 | 23 | 41.1 | |
| 3–4 | 26 | 19.4 | 23 | 29.9 | 11 | 24.4 | 19 | 33.9 | |
| >4 | 20 | 14.9 | 5 | 6.5 | 7 | 5.6 | 9 | 16.1 | |
| How many hours a day do you spend outdoors? | |||||||||
| <1 | 39 | 29.1 | 25 | 32.5 | 16 | 35.6 | 21 | 37.5 | =0.261 |
| 1–4 | 75 | 56.0 | 48 | 62.3 | 22 | 49.9 | 31 | 55.4 | |
| >4 | 20 | 14.9 | 4 | 5.2 | 7 | 15.6 | 4 | 7.1 | |
| How many hours a day do you spend in air-conditioned interiors? | |||||||||
| <1 | 83 | 61.9 | 44 | 57.1 | 24 | 53.3 | 34 | 60.8 | =0.648 |
| 1–4 | 30 | 22.4 | 21 | 27.3 | 9 | 20.0 | 11 | 19.6 | |
| >4 | 21 | 15.7 | 12 | 15.6 | 12 | 26.7 | 11 | 19.6 | |
| Regular, daily basis use tobacco products | 32 | 23.9 | 11 | 14.3 | 15 | 33.3 | 16 | 28.6 | =0.078 |
| History of SARS-CoV-2 infection | 75 | 56.0 | 34 | 44.2 | 25 | 55.6 | 39 | 69.6 | =0.036 |
| Pharmaceutical Agent | Normal | Mild | Moderate | Severe | aOR * p-Value ** | ||||
|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | ||
| Psychotropics | 9 | 6.7 | 8 | 10.4 | 6 | 13.33 | 15 | 26.8 | =1.41 =0.002 |
| Anti-histamines | 12 | 9.0 | 5 | 6.5 | 6 | 13.3 | 10 | 17.9 | =0.156 |
| Analgesics | 6 | 4.5 | 3 | 3.9 | 4 | 8.9 | 5 | 8.9 | =0.433 |
| Contraceptives (females only) | 19 | 23.7 | 8 | 12.5 | 7 | 20.6 | 12 | 29.3 | =0.184 |
| Other hormones | 13 | 9.7 | 7 | 9.1 | 5 | 11.1 | 9 | 16.1 | =0.572 |
| Health Condition | Normal | Mild | Moderate | Severe | aOR * p-Value ** | ||||
|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | ||
| Arterial hypertension | 4 | 3.0 | 2 | 2.6 | 0 | 0.0 | 4 | 7.1 | =0.221 |
| Depression | 9 | 6.7 | 5 | 6.5 | 7 | 15.6 | 16 | 28.6 | =1.48 <0.001 |
| Mental disease | 3 | 2.2 | 5 | 6.5 | 2 | 4.4 | 7 | 12.7 | =1.43 =0.039 |
| Thyroid disease | 14 | 10.4 | 7 | 9.1 | 6 | 13.3 | 10 | 17.9 | =0.442 |
| Diabetes | 1 | 0.7 | 1 | 1.3 | 1 | 2.2 | 5 | 8.0 | =1.82 =0.010 |
| Allergy | 27 | 20.1 | 13 | 16.9 | 16 | 35.6 | 21 | 37.5 | =1.22 =0.008 |
| Acne | 4 | 3.0 | 4 | 5.2 | 2 | 4.4 | 3 | 5.4 | =0.830 |
| Autoimmune disease | 3 | 2.2 | 2 | 2.6 | 5 | 11.1 | 3 | 5.4 | =0.061 |
| Hormonal disorder | 11 | 8.2 | 5 | 6.5 | 3 | 6.7 | 7 | 12.5 | =0.619 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wróbel-Dudzińska, D.; Osial, N.; Stępień, P.W.; Gorecka, A.; Żarnowski, T. Prevalence of Dry Eye Symptoms and Associated Risk Factors among University Students in Poland. Int. J. Environ. Res. Public Health 2023, 20, 1313. https://doi.org/10.3390/ijerph20021313
Wróbel-Dudzińska D, Osial N, Stępień PW, Gorecka A, Żarnowski T. Prevalence of Dry Eye Symptoms and Associated Risk Factors among University Students in Poland. International Journal of Environmental Research and Public Health. 2023; 20(2):1313. https://doi.org/10.3390/ijerph20021313
Chicago/Turabian StyleWróbel-Dudzińska, Dominika, Natalia Osial, Piotr Witold Stępień, Adrianna Gorecka, and Tomasz Żarnowski. 2023. "Prevalence of Dry Eye Symptoms and Associated Risk Factors among University Students in Poland" International Journal of Environmental Research and Public Health 20, no. 2: 1313. https://doi.org/10.3390/ijerph20021313
APA StyleWróbel-Dudzińska, D., Osial, N., Stępień, P. W., Gorecka, A., & Żarnowski, T. (2023). Prevalence of Dry Eye Symptoms and Associated Risk Factors among University Students in Poland. International Journal of Environmental Research and Public Health, 20(2), 1313. https://doi.org/10.3390/ijerph20021313







