1. Introduction
There is an extensive range of products, goods, and services covered under health information technologies (HITs), and this holds for services such as assistive technology and sensors [
1,
2,
3,
4,
5,
6], cloud-based services [
7], electronic health records (EHRs) [
8,
9,
10,
11,
12,
13,
14], mobile health technologies [
15,
16,
17,
18,
19,
20,
21,
22,
23], medical devices, telemonitoring tools, and telehealth [
3,
24,
25,
26,
27,
28,
29,
30]. All the technologies mentioned above bring about the gathering, sharing, and usage of health information by individuals, healthcare personnel, and community-based healthcare institutions [
1,
8,
11].
Personal health record (PHR) is defined as “An electronic application through which individuals can access, manage and share their health information, and that of others for whom they are authorized, in a private, secure, and confidential environment” [
31]. PHRs represent an attractive and developing technology within the health systems and applications that has been gaining ground among different countries [
32]. More specifically, PHR systems are information systems that incorporate data, tools, and functions geared toward individual health. In another definition proposed by the Markle Foundation [
33], PHR is an e-application enabling individuals to access, manage, and share their health information and that of others for which they are authorised electronically, securely, privately, and confidentially.
Moreover, an individual or authorised person develops, owns, updates, and manages personal health records [
34]. Personal health records summarise an individual’s lifelong health history based on procedures, major illnesses, allergies, blood pressure, data collected from home monitoring devices, family history, immunisations, medications, laboratory test results, and information about an individual’s health history [
35,
36,
37]. Health records access can be used through tools and functionalities to manage one’s health and enable communication and record sharing with clinicians [
1,
8,
11,
38,
39].
This paper defines PHR following Assadi and Hassanein’s [
34] definition. Throughout the study, terminologies such as “consumer”, “individual”, and “patient” are interchangeable, as consumers of the PHR system do not necessarily deal with medical information and can be healthy or suffering from illness. PHR system implementation and usage success help facilitate transformative development in the delivery and management of healthcare [
37,
38,
39]. Consequently, patient and care-provider circles are assisted in their effective interaction with further innovation opportunities for care management since patients and care providers share both controls, leading to enhanced and more efficient healthcare.
Regardless of the benefits that consumers can reap from PHR system usage [
36,
40,
41,
42,
43,
44,
45], studies have revealed that their adoption has yet to be extensive [
39,
46,
47]. This is attributed by Roehrs et al. [
41] to the following challenges that users face: first, there are challenges and issues regarding collaboration and communication that include the storage and availability of data in a PHR as well as limitations regarding the types of information that may be provided by the PHR. In addition, the PHR should be customizable, usable, familiar, and comfortable for the user. The second issue relates to privacy, security, and reliability, including confidentiality, integrity, data repositories and their owners, accessing control protocols, and data transport protocols. A third challenge concerns the infrastructure of PHRs, such as the portability of devices and equipment associated with them. To support PHR solutions, efficient computer systems as well as a scalable infrastructure are necessary. Fourth, there are concerns regarding integration, such as patterns in collecting medical information and terminology used in collecting and storing personal health information. Interoperability is also critical.
To overcome these challenges and barriers, it is necessary to link technology with human behaviour issues in order to gain a better understanding of the adoption of personal health records by end-users, which will ultimately lead to higher adoption rates [
48]. Considering the potential system advantages for end-users and how interested they may be in such a system [
34,
37,
38,
39], adoption is a must for the realisation of such advantages akin to any IS [
8,
16,
49], and thus, more studies need to be conducted to shed light on how to increase PHR system adoption rates.
Concerning the above, individuals should have access to their health information and be able to control it through the use of personal health records (PHR) so that they can actively participate in the management of their healthcare and eliminate the role of the passive patient [
36,
38,
40,
50,
51]. However, users must continuously invest effort into keeping up-to-date accounts to ensure that the system can effectively support them. This effort will reduce the likelihood of inaccurate, incomplete, and outdated records in the system, as these may lead to erroneous decisions [
31].
An example of an emerging class of information system is the patient health record system, which offers access to and monitoring of useful information that is accompanied by the requirement for ongoing maintenance (for example, regular updates of a patient’s health records), thereby supporting an individual’s active role within the context for which the information system was designed [
32,
36,
38,
43,
44,
45]. Healthcare system users should have the ability to be more proactive in managing the information systems, must reflect suitable personal traits, and take support from the factors in the environment to promote their active role [
8]. This facilitates a sufficient motivation level towards system use regardless of continuous maintenance [
52].
However, despite industry predictions about increasing consumer interest and government commitment to PHR technologies, their adoption has yet to peak and continues to fall short of expectations. The expression “PHR paradox” has been used to explain the disconnection between active interest and low usage rates of PHRs [
53]. Several reasons have been proposed for the lag in adoption in the literature, which are often contradictory with intuition; often, the results are mixed [
38,
54,
55]. As a result, authors have urged more studies in the consumer adoption PHR area [
34,
37,
38,
56,
57].
More specifically, little information about health technologies in Saudi Arabia is available due to the lack of research [
58]. Several studies have overlooked the perspective of healthcare consumers (users) concerning implementing and using an integrated PHR system at the national level [
39]. Therefore, this study extends TAM by examining the factors influencing healthcare consumers’ usage of personal health records.
1.1. Literature Review
PHR Adoption
The literature on PHR has indicated that adoption barriers may be linked to technology factors such as security concerns, system usability, and ineffective healthcare provider system integration [
37,
41,
59,
60,
61]. Several personal factors have also been articulated as barriers to adopting these technologies, such as lack of technology awareness, competency, chronic medical conditions, and unrealistic expectations [
41,
57,
61,
62,
63,
64,
65]. Although several of these factors have been empirically validated, there is often a lack of consistency in the results between studies [
41,
55,
61,
66,
67,
68,
69]. The reviewed relevant studies show that chronically ill or disabled patients and their caregivers and older people’s caregivers have a higher likelihood of adopting and using PHR technologies [
70,
71,
72,
73]. This user group often views PHR technologies as useful in communicating with the correct personnel to obtain personalised care [
37,
71,
74].
According to a recent study, several factors contribute to PHR adoption, namely computer anxiety, concerns about privacy and security, and perceptions of usefulness, among others [
54,
55,
68,
75,
76,
77,
78]. Meanwhile, studies focusing on several adoption factors, including health literacy among consumers, user self-efficacy, and usability perceptions, have shown mixed or contradictory results when evaluating adoption [
54,
55,
79]. Regarding major areas that need more investigation, the review showed that PHR adoption has yet to be thoroughly examined.
In this regards, the study aim was to explain factors such as privacy, security, and usability (exogenous predictors of TAM) to offer insight into the utilization and adoption of and personal health records. The current study contributes significantly to the technology-acceptance literature in two distinct manners. Firstly, is that it is the first to examine the use of PHR in Saudi Arabia, including the extension of the TAM model, and second, it creates a context-driven model that focuses on the associations among privacy, security, and usability and personal health records utilization. Additionally, this study fills a gap in the literature regarding the moderating effects of privacy influence on the relationship between perceived ease of use and intention to use. Further, the moderating effects of usability on the relationship between perceived ease of use, perceived usefulness, and intention to use were investigated. The proposed model enriches information and knowledge regarding the acceptance of PHRs in developing nations, and by doing so, it helps satisfy calls for contextual theorising in the information systems field. The next section of the article presents a description of the proposed model and the constructs and hypotheses that are relevant to it.
1.2. Theoretical Foundation
This study adopted TAM as the underpinning theory owing to its influential and effective nature in shedding light on technology usage behaviour [
16,
18,
80,
81,
82,
83,
84,
85,
86]. TAM posits that technology use behaviour, referred to as the behaviour inclination towards accepting technology, can be measured through a user’s attitude towards using technology [
87]. Two main attitude predictors towards usage have been proposed: perceived usefulness and easiness [
87,
88]. The first refers to the belief of an individual that using technology can promote performance of task; the second defines the perception of an individual that technology use is free from effort [
87,
88]. Additionally, perceived easiness indirectly influences perceived usefulness attitudes [
16,
18]. Studies have found that TAM can effectively explain differences in technology use behaviour in different contexts and situations, including the health context, for eHealth records (EHRs) [
89], telehealth [
90], mobile health technologies [
16,
18], cloud-based services [
91], medical devices and telemonitoring tools [
92,
93], and assistive technology [
94].
However, despite the comprehensive inspection and validation of models in terms of health information systems among health professional staff, such examinations do not address consumers’ acceptance of health information systems [
16,
18,
95,
96,
97], and based on the provided evidence, such acceptance may vary from that of professionals with self-efficacy and experience, as a result of which challenges may be faced during system use [
12,
16,
95,
98]. Hence, searching for ways to enhance PHR acceptance among consumers is pertinent.
Additionally, TAM has the same weaknesses as other technology acceptance models, the first of which is that it depends on other factors to determine the attitude of individuals. In general, TAM has been widely employed to investigate internal motivations rather than external ones, as its focus is on the outcomes of IT use. The use process has been largely overlooked, highlighting the need to include external factors in the model. Consequently, a TAM extension with new variables may be able to explain PHR adoption. This study included privacy, security, and usability to extend TAM.
Both privacy and security have been researched in literature, with increasing evidence validating their influence [
99,
100,
101,
102,
103,
104,
105]. Based on a systematic review of PHR privacy policies, users are not provided with detailed descriptions of the security issues and adherence to standards and regulations when it comes to a PHR system [
104,
106]. This may be exemplified by the significant advantages of PHR use and systems privacy risks, with emphasis confined to general privacy and trust issues [
99,
101,
104]. Both security and privacy are major challenges in protecting health information systems, and even though the system’s success depends on various factors such as organisational, technical, and political issues, the authentication and cryptographic management (privacy and trust issues) for prevention of hacker attacks and unauthorised use is of major importance [
99,
104].
Added to the above, results show that new system usability and its design and user experience contributes to influence system acceptance, and in this regard, the usability of a system can be defined as the amount of effort that must be expended to use it. In general, usability is the degree to which users can effectively and efficiently use a product and the extent to which they are satisfied that they will achieve specific goals through employing a product. It is key to the use of acceptance of PHR, as evidenced by prior studies [
32,
41,
66], to facilitate PHR’s ease of use through the user interface and patient support [
38,
107,
108]. Thus, PHR stakeholders, including designers and developers, should focus on usability aspects.
1.3. Proposed Model and Hypotheses Formulation
1.3.1. Perceived Usefulness (PU)
The degree to which an individual believes that a particular technology will improve his or her job performance to an extent that includes enhancing efficiency and effectiveness [
88] can be determined by the perceived usefulness of the technology. Based on TAM studies [
88,
109], perceived usefulness is one of the top technology adoption determinants [
110,
111]. It is therefore expected that the perceived usefulness of PHR systems will serve a key role in deciding whether they are adopted. Past studies of this calibre have confirmed the key role of perceived usefulness in adoption prediction [
55,
68,
79,
112]. In this regard, the first hypothesis is reported:
Hypothesis 1 (H1). The intent to use PHR is positively influenced by PU.
1.3.2. Perceived Ease of Use (PEOU)
The level to which an individual believes that using a specific technology will be effort-free is known as PEOU [
88]. In this study, PEOU is described as a user’s belief that PHR use is free from mental and physical effort. Studies in the literature dedicated to the PEOU–intention to use PHR relationship generally confirmed the relationship [
113,
114]. Further, PEOU’s significant influence over PU and intention towards using PHR [
27,
113] was reported. In this regard, the second and third hypotheses are reported:
Hypothesis 2 (H2). The PU of PHR is positively affected by PEOU.
Hypothesis 3 (H3). The intent to utilize PHR is positively affected by PEOU.
1.3.3. Intention to Use
New technology acceptance is primarily set by intention towards using such technology, defined as an individual’s desire to engage in a particular behaviour [
115]. When referring to the use of PHRs, the intention is a plan towards using it, and according to Hsieh et al. [
114], intention towards PHR usage significantly relates to its actual use. In this regards, the fourth hypothesis is reported:
Hypothesis 4 (H4). PHR usage is positively influenced by the intention to use it.
1.3.4. Privacy and Security
An essential research topic relative to technology acceptance is the role of privacy and security and the related empirical findings [
99,
100,
101,
102]. More specifically, information privacy is the ability of an individual to manage their personal information in light of interactions and exchanges with others [
116,
117]. Healthcare providers generally manage users’ personal data and provide it to other personnel; owing to this sharing, there is the utmost concern for privacy [
118]. Currently, using electronic communication has become common, adding to the privacy, confidentiality, standardisation, and accuracy of PHR [
119,
120]. A related study by Kaelber et al. [
121] indicated that the top concern among patients regarding electronic healthcare applications of every type is security and privacy, which holds true for PHR. In another study, Featherman and Fuller [
122] stated that privacy concerns are the focus of potential e-services adopters.
Moreover, based on a systematic review of PHR privacy policies, most such policies failed to provide users with detailed descriptions of security issues and adherence to standards and regulations [
106]. In the case of perceived benefits that can be reaped from PHR, the highlights are placed on privacy and trust issues rather than the potential system-related privacy risks [
101]. It was found that 67% of people were concerned with their personal medical records privacy (Bishop et al. [
123]), indicating the importance of privacy from the patient’s viewpoint [
124]. Privacy negatively influences adopting an eHealthcare system, according to Angst and Agarwal [
118], while Li et al. [
101] revealed that privacy could not completely explain the intention to adopt. Nevertheless, other studies such as that by Whetstone and Goldsmith [
125] found that healthcare innovativeness, privacy concerns, and perceived usefulness were the top predictors of adoption intent.
According to Sabnis and Charles [
126], security is a determining factor in the decision to adopt web-based PHR, along with confidentiality and privacy. If people are convinced that their personal information is shared privately and is stored in a way that unauthorised parties will not be privy to it [
127], their concerns will be assuaged. However, the more individuals who adopt web-based PHR, the higher the risk of breach the information; therefore, privacy and security are main concerns for protecting health systems. Successful systems depend on various factors (organisational, technical, and even political), but authentication and cryptographic management are of top importance for preventing unauthorised use and attacks made by hackers [
99]. In this regards, the fifth hypothesis is reported:
Hypothesis 5 (H5). Security has a positive influence on the intention to use a PHR.
In connection to the above, patients will be more inclined to use PHR due to its ease of use and the PHR providers’ assurance that the system is credible and capable of minimising privacy risk, which would lead to higher intention towards PHR usage. Hence, the sixth hypothesis is reported:
Hypothesis 6 (H6). Privacy moderates the relationship between PEOU and the intention to use a PHR.
1.3.5. Usability
The usability concept may be defined as the effort needed towards using a computer system. According to Nielsen [
128], usability is associated with the ease with which a user can learn to manage a system, the ease of learning the fundamental system functions, the level of efficiency with which the site has been developed, the level of error avoidance, and the general user satisfaction when it comes to system management. On the whole, usability reflects how users can use a particular system [
105], and thereby, high system usability is related to lower difficulty levels of managing its functions [
88]. Usability has always been considered a major predictor of intentions towards system usage [
129].
The following statements can summarise website usability:
Easy understanding of the system structure, functions, interface, and content by a user;
Simple use of the initial stages of a website,
Speedy search for required information,
Ease of browsing in light of the time and work required to obtain the expected results,
User’s ability to control and navigate the system at any time.
Regarding health information systems, usability issues have garnered significance in system rejection/acceptance, as evidenced in computerised patient records that depend on the system’s usability [
130,
131,
132,
133,
134]. Evidence points to the fact that issues surrounding usability directly influence patient outcomes, including opportunity cost, while other issues that indirectly impact usability include coping strategies in dealing with software problems and limitations and complexity and that entail dealing with complexity strategies, breach of communication and usability of software, oversight of bias, and usability on patient safety [
131,
132,
133,
134,
135]. In this day and age, consumers are faced with an extensive array of personal health information-management tools at their convenience, and PHR’s ability to satisfy their needs depends at some level on the way product designers focus on users’ needs and a user’s involvement in the design, testing, and system re-design.
Usability of PHR indicates the perceived ease of managing a site or accessing and keeping track of health information online, and this is deemed a major factor in PHR development. Patients’ willingness to accept depends on the user-friendliness of the PHR system and ease of learning usage and browsing. Meanwhile, a complicated system could only lead to human error and dissatisfaction among the users, and eventually, rejection rather than acceptance will be the outcome [
136]. Additionally, patients will be convinced that PHR usage is easy when they can easily learn system management and memorise fundamental system functions. This would lead to higher intention towards PHR usage; in other words, PEOU and PHR intention towards use will be correlated more strongly with higher PHR usability, and in this regard, the seventh hypothesis is reported:
Hypothesis 7 (H7). The relationship between PEOU and intention to use personal health records is moderated by usability.
Additionally, if patients are convinced that PHR use will enhance their health status and quality of health services through its efficient functions and design, they will readily accept it, with higher intention towards its usage. The higher the usability of PHR, the higher the relationship between PU and intention towards PHR usage. In this regards, the eighth hypothesis is reported:
Hypothesis 8 (H8). The relationship between PU and intention to use personal health records is moderated by usability.
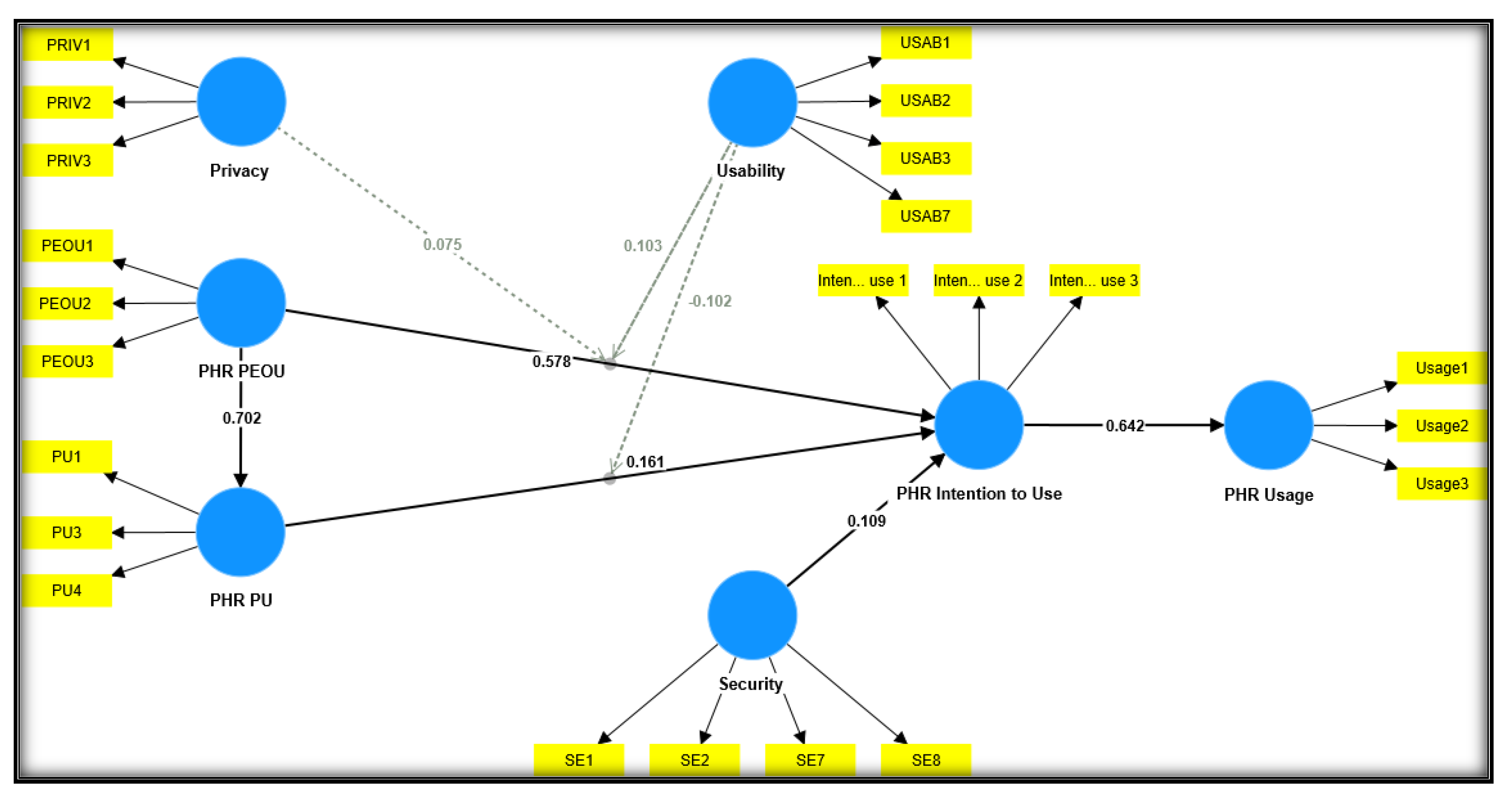
Figure 1 offers a theoretical framework overview explaining how TAM, privacy, security, usability, and PHR use are related in terms of each other.
3. Results
This study employed partial least squares (PLS)–SEM to test the proposed framework, enabling the measurement and structural models to be examined simultaneously [
149,
150,
151]. As well as being effective in addressing complex models with hierarchical structures, PLS is also highly effective in dealing with models with multiple relationships, indicators, and constructs [
152,
153,
154,
155,
156,
157]. In addition, PLS can be used to deal with problems that may arise because of small sample sizes and errors, as it only relies on a few rigid assumptions regarding the normal distribution of data to deal with such problems [
84,
152,
158,
159,
160]. PLS Version 4.0.8.4 was employed to test the proposed model, with the first step involving testing the measurement model’s reliability and validity [
159,
161,
162]. AVE, indicator reliability, internal consistency, and discriminant validity, which other authors previously proposed, were employed to determine whether the study had convergent validity [
8,
16,
84,
163,
164,
165,
166].
Table 2 contains the composite reliability (CR) values, item loadings, Cronbach’s alpha (CA), and constructs AVE. The table shows that all CA values exceeded 0.60, which were all acceptable based on Pallant [
167] and Nunnally and Bernstein [
168], and CR values exceeded 0.70 throughout the constructs, which confirmed internal consistency and appropriate nature of constructs based on Hair et al. [
166,
169,
170]. According to the results, the items of the constructs had a reliability of greater than 0.40, which was sufficient for them to be considered acceptable [
170].
In terms of convergent validity, all AVE values exceeded 0.50, which was the threshold value [
170]. Based on the squared AVE values of the constructs, the conclusion can be reached that the discriminant validity of the constructs exceeded the threshold value. Based on the fact that all the values were higher than the correlation construct values, the discriminant validity of the constructs was confirmed by the fact that all the values were higher than the correlation construct values [
170] (See
Table 3).
Perceived Usefulness (PU)
The structural model and hypotheses analysis was conducted using a main effect model, whereas an analysis of the moderation effect was carried out using an interaction model [
163,
170]. To generate the path coefficient and evaluate the significance of the effects of the study models, the PLS path algorithm was applied to the study models’ outputs. Based on past studies’ recommendations [
159,
169,
170], 5000 bootstrapping resamples were applied (refer to
Figure 1), and the path coefficients significance was determined for direct effects (refer to
Table 4) and moderating effects (refer to
Table 5).
Consistent with the study’s hypotheses, the results in the above table show the significant and positive impact of perceived usefulness on intention to use PHR (β = 0.161, t = 2.595, p < 0.005), supporting H1. As for perceived ease of use, a significant and positive effect was found on perceived usefulness to use PHR (β = 0.702, t = 21.406, p < 0.00), supporting H2, and perceived ease of use was also found to significantly influence PHR intention to use (β = 0.578, t = 10.527, p < 0.00), and thus, H3 was also supported. Intention to use PHR positively and significantly influenced PHR actual use (β = 0.642, t = 18.831, p < 0.00), confirming and supporting H4. Lastly, security positively and significantly influenced the intention to use a PHR (β = 0.109, t = 2.877), thus supporting H5.
The moderating hypotheses (H6, H7, and H8) concerning privacy and usability were examined using an interaction model. The study created three latent interaction constructs to depict the interaction between PU and PEAU (TAM-related factors and the moderating constructs (privacy and usability) and their influence on PHR intention to use, i.e., the criterion variable. A bootstrapping procedure with 5000 resampling was used, and
Table 5 contains the detailed results. Based on the positive moderation path coefficient of the interaction term between privacy and perceived ease of use (β = 0.075, t = 2.008,
p < 0.020), privacy positively moderated the PEOU–intention to use the PHR relationship, supporting H6. In essence, privacy moderated the PEOU–PHR intention to use relationship. As shown in
Figure 2 and
Table 6, privacy is a moderator in maintaining the association between perceived ease of use and intention to use PHR. Privacy strengthens the positive association between perceived ease of use and intention to use PHR.
Moving on to the moderating effect of usability, the moderation path coefficient result (β = 0.095, t = 1.903,
p < 0.029) shows that usability moderates the association between perceived ease of use and PHR intention to use, confirming H7. The result is presented in
Figure 3 and
Table 7. The moderating effect supports the positive association between perceived ease of use and PHR intention to use.
The negative moderation path coefficient of the interaction term between usability and perceived usefulness (β = −0.102, t = 1.747,
p < 0.04) is indicative of the negative moderating effect of usability on the association between perceived usefulness and PHR intention to use, and as such, H8 is also supported. The results are demonstrated in
Figure 4 and
Table 8. The results show that the usability of PHRs reduces the positive association between perceived usefulness and PHR intention to use.
Finally, the PLS structure model was evaluated using the criterion coefficient of determination (R2). According to Sarstedt et al. [
159], the rule of thumb when it comes to R2 values is such that 0.67 is deemed substantial, 0.33 is moderate, and 0.19 is weak. These findings revealed that TAM integration was successful in predicting PHR use, and with such addition, the model’s predictive power increased and managed to explain 0.492 of the variances in patients’ PHR usage and 0.548 of the variance of intention towards use. The study model succeeded in explaining 0.492 of the perceived usefulness perception of patients towards PHR.
4. Discussion
This research validates the accuracy of TAM in predicting the use of PHR among patients by supporting its assumptions with additional variables, thus strengthening the model’s predictive abilities.
The results found supported the significant association between perceived usefulness and consumers’ intention to use PHR (
p < 0.05), which is in line with past reported studies on eHealth adoption, including Alsyouf et al. [
16,
18], as well as PHR adoption, including Noblin et al. [
171], Abdekhoda et al. [
103], and Liu [
27]. These studies supported PU’s role in driving users’ behavioural intention towards PHR use. In other words, if patients believe that PHR can provide benefits, they will use it to enhance healthcare services. Healthcare quality is enhanced through this technology by eliminating waiting times, and through health profile management, users can also maintain a higher rate of health profile usage and management.
Added to the above, a significant association was found between perceived ease of use and perceived usefulness (
p < 0.00), as with the other prior literature on eHealth adoption such as that of Alsyouf et al. [
16,
18] and on PHR adoption such as that of Abdekhoda et al. [
103], Liu [
27], and Noblin et al. [
171]. Stated clearly, people who find PHRs easy to use are more likely to use them frequently, supporting their perception of their value and importance.
Moreover, the study findings supported a significant association between PEOU and PHR intention to use (
p < 0.00), as proposed in H3 and as revealed by past literature, including Alsyouf et al. [
16,
18] in the eHealth context and Abdekhoda et al. [
103] and Elsafty et al. [
172] in PHR adoption context. Based on this result, perceived ease of use among patients concerning PHR could result in increased intention towards using the system and ultimately their actual use. This result can be attributed to the importance of PEOU in PHR among patients. According to the literature, consumers’ acceptance of health informatics applications differs from that of health professionals [
16,
95,
98]. As a result of the challenges they have experienced in using the system, consumers have a low level of self-efficacy and a negative perception of the system’s usability. Therefore, it is necessary to assist patients in accepting PHRs.
Moving on to the fourth hypothesis, which proposed PHR intention influence over actual PHR use, a positive influence was found (
p < 0.00), which is in line with past studies’ findings [
8,
11,
103]. In other words, users’ behavioural intention indicates their acceptance and actual use of technology—their intention towards PHR use is a predictor of their actual use, similar to the finding in the eHealth context reported by past literature.
Security was found to have a significant association with PHR intention to use (
p < 0.04), supporting H5, and this significant relationship was also found by Saigi-Rubio et al. [
173]. If people are convinced that their personal information is shared safely, far from manipulation by unauthorised individuals [
127], their adoption of PHR will increase.
In the sixth hypothesis (H6), privacy was proposed to moderate the association between perceived ease of use and intention to use PHR, and the hypothesis was supported, indicating that privacy heightens the influence of perceived ease of use on PHR intention to use. This may be attributed to the patient’s belief that using PHRs will become easier when providers of the system can minimise privacy risks and their effects, thus contributing to higher intention to use the system.
Hypothesis 7 proposed the moderating effect of usability on the perceived ease of use–intention to use PHR relationship, and the findings supported it. Privacy with PEOU determines the level of PHR use among patients in that patients who are convinced that PHR use is easier when they can learn system management and memorise the basic functions would intend to use it. The higher the PHR usability, the stronger the PEOU–intention to use PHR relationship.
Finally, in the eighth hypothesis (H8), usability was posited to moderate the PU–intention to use the PHR relationship. Usability was found to influence the relationship between the two negatively. This result may be attributed to the notion that if patients believe that the PHR system falls short of meeting their needs owing to deactivated services or improper working of services, this would be perceived as weak system functionality; eventually, usability would harm the PU–intention to use PHR relationship.
5. Conclusions
In literature, TAM has often been used and adopted to examine various eHealth application types in different contexts. In this study, the focus is placed on PHR use, assuming that if users have a positive intention towards PHR usage in light of its usefulness, ease of use, usability, privacy, and security, they will increase their use and acceptance of it. TAM was adopted as the underpinning model to examine the study variables and to understand why eHealth applications in general, with PHR in particular, have not been extensively adopted in Saudi Arabia. Three exogenous variables, namely privacy, security, and usability, were added to TAM to examine existing values, past experiences, and needs of potential users. SEM analysis showed that the model could explain the predictive ability of the variables of PHR intention to use and actual use. Perceived usefulness, perceived ease of use, and security were found to be relevant in their direct influence on intention towards PHR use, while privacy is relevant in terms of its moderating effect on the PHR PEOU and PHR intention to use relationship. Usability was also relevant in positively moderating the PHR PEOU and PHR intention to use relationship. However, usability had a negative moderating effect on the PHR PU–PHR intention to use relationship.
Limitations and Future Research
This study has several limitations. The first limitation is the nature of the study. A cross-sectional survey requires accounting for the differences among the relationships across divisions, locations, contexts, and countries, as the meaning may disappear over time. In this case, future studies may adopt a longitudinal study instead. The second limitation is the data collected through email distribution to university members, specifically to one of the biggest Saudi universities—but a single university nonetheless, which limits the outcome’s generalizability. While the study’s target population (students, employees, and faculty members) limited the generalizability of the findings, it does provide insight into how PHR are used by a very large segment of society, which drives IT adoption in a community. Furthermore, PHRs are not only used by people who are ill but also by healthy individuals. This study is expected to pave the way for future studies that will include other segments of society. By doing so, we will be able to gain a deeper understanding of the adoption of information systems, specifically PHRs. To this end, future studies may take different settings and employ large-sized samples representing the same context.
Moreover, future studies may adopt data collection methods other than the survey questionnaire to enable comparative studies or assessments of pre-adoption and post-adoption behaviours that are valuable for health applications. A qualitative approach would also enable the acquisition and observation of life experiences, which are crucial to positional analysis—this is possible through the elicitation of narrative analysis or the explanation of the phenomenon. Future studies may also extend TAM through other external variables not examined in the study, such as the self-efficacy of technology, quality factors (the quality of service, the quality of the system, and the quality of the information), as well as satisfaction with the technologies, which are all important factors. Additionally, age, gender, and other demographic characteristics may be addressed. Notably, this study adopted TAM solely without its integration with other theories and models—future studies may integrate them and re-examine the study findings to enrich the literature and, ultimately, practice. Accordingly, this study recommends that the Population-Intervention-Environment-Transfer Model of Transferability (PIET-T) be integrated with the TAM in order to develop a wider understanding of user acceptance of official systems as well as other key elements of the transferability concept.