Relationship between Physical Activity and Sedentary Behavior, Spinal Curvatures, Endurance and Balance of the Trunk Muscles-Extended Physical Health Analysis in Young Adults
Abstract
1. Introduction
2. Materials and Methods
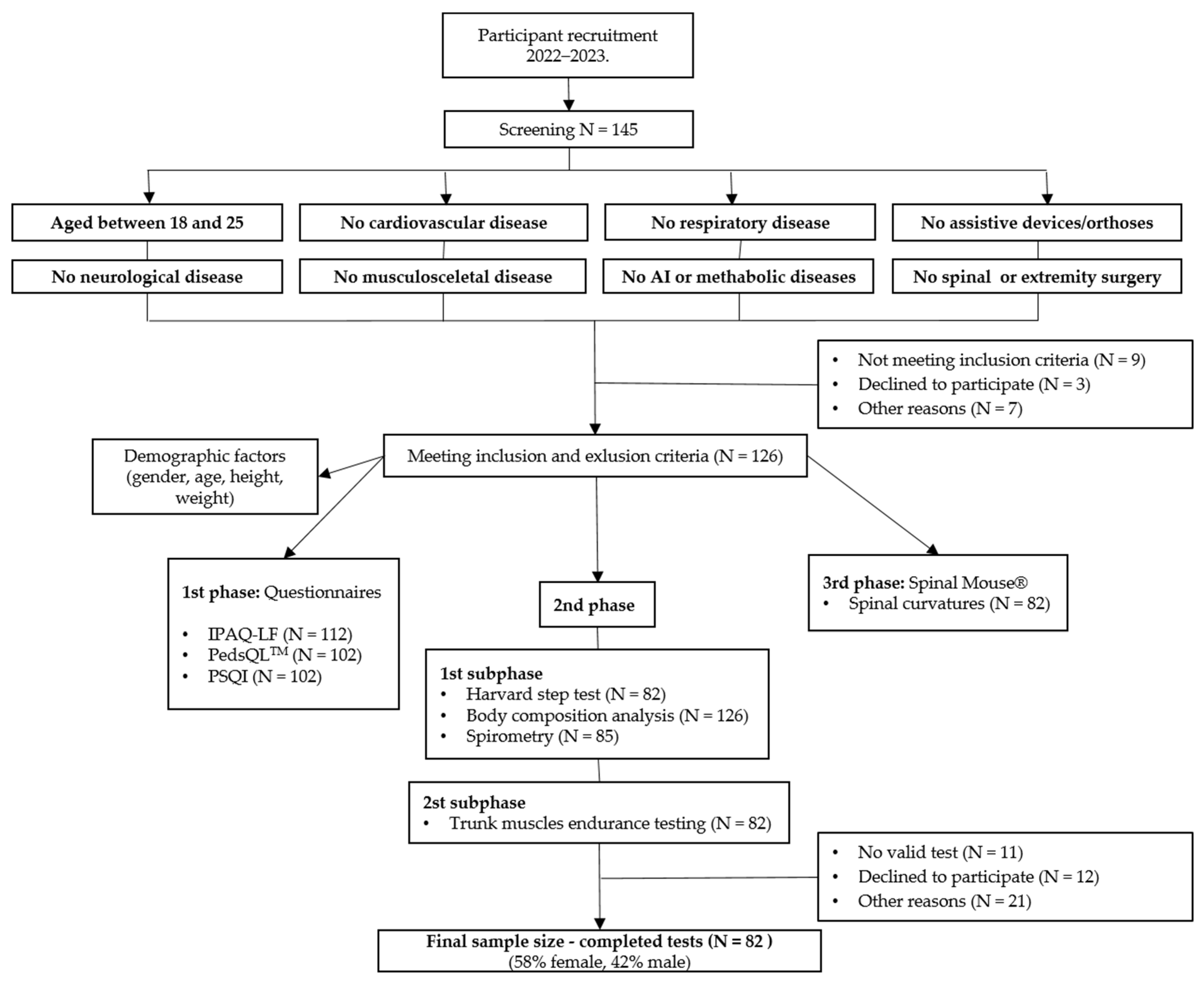
2.1. Participants
- (1)
- (2)
- The program MedCalc (© 2023 MedCalc Software Ltd., Ostend, Belgium) estimated a minimum of 123 subjects was needed to achieve 80% power with r = 0.25, α = 0.05 type I error and beta = 0.20 type II error.
2.2. Study Design
2.3. Outcome Measures
2.3.1. Questionnaires
Self-Reported Quality of Life
Self-Reported Sleep Quality
Self-Reported PA and Time Spent Sitting
2.3.2. Body Composition Analysis and Body Mass Index
2.3.3. Trunk Muscles Endurance Testing
Trunk Extensor Endurance Testing
Trunk Flexor Endurance Testing
Balance of Trunk Muscles
2.3.4. Cardiovascular Fitness
2.3.5. Spirometry
2.3.6. Evaluation of Spinal Curvatures
2.4. Statistical Analysis
3. Results
4. Discussion
4.1. PA and Sedentary Behavior (Time Spent Sitting)
4.2. Association of PA and Sedentary Behavior (Time Spent Sitting) with BMI and Body Composition (Body Fat and Muscle Mass)
4.3. Association of PA and Sedentary Behavior (Time Spent Sitting) with QoL and Sleep
4.4. Association of PA and Sedentary Behavior (Time Spent Sitting) with Posture (Trunk Muscle Endurance, Trunk Extensor/Flexor Endurance Ratio and Spinal Curvatures)
4.5. Association of PA and Sedentary Behavior (Time Spent Sitting) with Cardiorespiratory Performance (Physical Fitness Index and MVV)
5. Strengths and Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hallal, P.C.; Andersen, L.B.; Bull, F.C.; Guthold, R.; Haskell, W.; Ekelund, U. Lancet Physical Activity Series Working Group. Global physical activity levels: Surveillance progress, pitfalls, and prospects. Lancet 2012, 380, 247–257. [Google Scholar] [CrossRef] [PubMed]
- Haseler, T.; Haseler, C. Lack of physical activity is a global problem. BMJ 2022, 376, o348. [Google Scholar] [CrossRef] [PubMed]
- WHO. Global Health Risks: Mortality and Burden of Diseases Attributable to Selected Major Risks. WHO Home Page. Available online: https://apps.who.int/iris/handle/10665/44203 (accessed on 24 June 2023).
- Grasdalsmoen, M.; Eriksen, H.R.; Lønning, K.J.; Sivertsen, B. Physical exercise and body-mass index in young adults: A national survey of Norwegian university students. BMC Public Health 2019, 19, 1354. [Google Scholar] [CrossRef] [PubMed]
- WHO. Global Action Plan for Physical Activity 2018–2030: More Active People for Healthier World. WHO Home Page. Available online: https://apps.who.int/iris/handle/10665/272722 (accessed on 24 April 2023).
- Vina, J.; Sanchis-Gomar, F.; Martinez-Bello, V.; Gomez-Cabrera, M.C. Exercise acts as a drug; the pharmacological benefits of exercise. Br. J. Pharmacol. 2012, 167, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Blair, S.N.; Kohl, H.W., 3rd; Paffenbarger, R.S., Jr.; Clark, D.G.; Cooper, K.H.; Gibbons, L.W. Physical fitness and all-cause mortality: A prospective study of healthy men and women. JAMA 1989, 262, 2395–2401. [Google Scholar] [CrossRef]
- Myers, J.; Kokkinos, P.; Nyelin, E. Physical Activity, Cardiorespiratory Fitness, and the Metabolic Syndrome. Nutrients 2019, 11, 1652. [Google Scholar] [CrossRef]
- Swift, D.L.; Johannsen, N.M.; Lavie, C.J.; Earnest, C.P.; Church, T.S. The Role of Exercise and Physical Activity in Weight Loss and Maintenance. Prog. Cardiovasc. Dis. 2014, 56, 441–447. [Google Scholar] [CrossRef]
- Park, J.H.; Moon, J.H.; Kim, H.J.; Kong, M.H.; Oh, Y.H. Sedentary Lifestyle: Overview of Updated Evidence of Potential Health Risks. Korean J. Fam. Med. 2020, 41, 365–373. [Google Scholar] [CrossRef]
- Ashton, L.M.; Hutchesson, M.J.; Rollo, M.E.; Morgan, P.J.; Collins, C.E. A scoping review of risk behaviour interventions in young men. BMC Public Health 2014, 14, 957. [Google Scholar] [CrossRef]
- Kehler, T.; Grubić Kezele, T.; Fužinac-Smojver, A.; Kauzlarić-Živković, T. Association of vitamin D insufficiency and low physical activity with fatigue, headaches and psychological distress in college students, North-Mediterranean Croatia—A pilot study. Paediatr. Croat. 2021, 65, 59–66. [Google Scholar] [CrossRef]
- Güner, Ç. Quality of Life and Physical Activity among University Students. Univers. J. Educ. Res. 2018, 6, 1141–1148. [Google Scholar] [CrossRef]
- Kokandi, A.A.; Alkhalaf, J.S.; Mohammedsaleh, A. Quality of Life in Relation to the Level of Physical Activity Among Healthy Young Adults at Saudi Arabia. Biomed. Pharmacol. J. 2019, 12, 281–287. [Google Scholar] [CrossRef]
- Pears, M.; Kola-Palmer, S.; De Azevedo, L.B. The impact of sitting time and physical activity on mental health during COVID-19 lockdown. Sport Sci. Health 2021, 18, 179–197. [Google Scholar] [CrossRef]
- Jiang, L.; Cao, Y.; Ni, S.; Chen, X.; Shen, M.; Lv, H.; Hu, J. Association of Sedentary Behavior with Anxiety, Depression, and Suicide Ideation in College Students. Front. Psychiatry 2020, 11, 566098. [Google Scholar] [CrossRef] [PubMed]
- Ge, Y.; Xin, S.; Luan, D.; Zou, Z.; Liu, M.; Bai, X.; Gao, Q. Association of physical activity, sedentary time, and sleep duration on the health-related quality of life of college students in Northeast China. Health Qual. Life Outcomes 2019, 17, 124. [Google Scholar] [CrossRef]
- Zhou, H.; Dai, X.; Lou, L.; Zhou, C.; Zhang, W. Association of Sedentary Behavior and Physical Activity with Depression in Sport University Students. Int. J. Environ. Res. Public Health 2021, 19, 9881. [Google Scholar] [CrossRef]
- Peterson, N.E.; Sirard, J.R.; Kulbok, P.A.; DeBoer, M.D.; Erickson, J.M. Sedentary behavior and physical activity of young adult university students. Res. Nurs. Health 2018, 41, 30–38. [Google Scholar] [CrossRef]
- Huang, Z.; Liu, Y.; Zhou, Y. Sedentary Behaviors and Health Outcomes among Young Adults: A Systematic Review of Longitudinal Studies. Healthcare 2022, 10, 1480. [Google Scholar] [CrossRef]
- Lee, M.K.; Oh, J. The relationship between sleep quality, neck pain, shoulder pain and disability, physical activity, and health perception among middle-aged women: A cross-sectional study. BMC Women’s Health 2022, 22, 186. [Google Scholar] [CrossRef]
- Ghezelbash, F.; Shirazi-Adl, A.; Arjmand, N.; El-Ouaaid, Z.; Plamondon, A.; Meakin, J.R. Effects of sex, age, body height and body weight on spinal loads: Sensitivity analyses in a subject-specific trunk musculoskeletal model. J. Biomech. 2016, 49, 3492–3501. [Google Scholar] [CrossRef]
- Paddon-Jones, D.; Sheffield-Moore, M.; Urban, R.J.; Sanford, A.P.; Aarsland, A.; Wolfe, R.R.; Ferrando, A.A. Essential amino acid and carbohydrate supplementation ame-liorates muscle protein loss in humans during 28 days bedrest. J. Clin. Endocrinol. Metab. 2004, 89, 4351–4358. [Google Scholar] [CrossRef] [PubMed]
- Moriyama, H. The effects of exercise on joints. Clin. Calcium. 2017, 27, 87–94. [Google Scholar] [PubMed]
- Herzog, W.; Powers, K.; Johnston, K.; Duvall, M. A new paradigm for muscle contraction. Front. Physiol. 2015, 6, 174. [Google Scholar] [CrossRef] [PubMed]
- Nourbakhsh, M.R.; Massoud, A.A. Relationship between mechanical factors and incidence of low back pain. J. Orthop. Sports Phys. Ther. 2002, 32, 447–460. [Google Scholar] [CrossRef]
- Nikander, R.; Sievanen, H.; Heinonen, A.; Daly, R.M.; Uusi-Rasi, K.; Kannus, P. Targeted exercise against osteoporosis: A systematic review and meta-analysis for optimising bone strength throughout life. BMC Med. 2010, 8, 47. [Google Scholar] [CrossRef]
- González-Gálvez, N.; Vaquero-Cristóbal, R.; López-Vivancos, A.; Albaladejo-Saura, M.; Marcos-Pardo, P.J. Back Pain Related with Age, Anthropometric Variables, Sagittal Spinal Curvatures, Hamstring Extensibility, Physical Activity and Health Related Quality of Life in Male and Female High School Students. Int. J. Environ. Res. Public Health 2020, 17, 7293. [Google Scholar] [CrossRef]
- Mazic, S.; Lazovic, B.; Djelic, M.; Suzic-Lazic, J.; Djordjevic-Saranovic, S.; Durmic, T.; Zikic, D.; Gluvic, Z.; Zugic, V. Respiratory parameters in elite athletes–does sport have an influence. Rev. Port. Pneumol. 2015, 21, 192–197. [Google Scholar] [CrossRef]
- Štefan, L.; Sporiš, G.; Krističevi, T.; Knjaz, D. Associations between sleep quality and its domains and insufficient physical activity in a large sample of Croatian young adults: A cross-sectional study. BMJ Open 2018, 8, e021902. [Google Scholar] [CrossRef]
- Bangsbo, J.; Blackwell, J.; Boraxbekk, C.-J.; Caserotti, P.; Dela, F.; Evans, A.B.; Jespersen, A.P.; Gliemann, L.; Kramer, A.F.; Lundbye-Jensen, J.; et al. Copenhagen Consensus Statement 2019: Physical Activity and Ageing. Br. J. Sports Med. 2019, 53, 856–858. [Google Scholar] [CrossRef]
- Alsufiany, M.B.; Lohman, E.B.; Daher, N.S.; Gang, G.R.; Shallan, A.I.; Jaber, H.M. Non-specific chronic low back pain and physical activity: A comparison of postural control and hip muscle isometric strength: A cross-sectional study. Medicine 2020, 99, e18544. [Google Scholar] [CrossRef]
- Koumantakis, G.A.; Malkotsis, A.; Pappas, S.; Manetta, M.; Anastopoulos, T.; Kakouris, A.; Kiourtsidakis, E. Lumbopelvic sagittal standing posture associations with anthropometry, physical activity levels and trunk muscle endurance in healthy adults. Hong Kong Physiother J. 2021, 41, 127–137. [Google Scholar] [CrossRef] [PubMed]
- Heneghan, N.R.; Baker, G.; Thomas, K.; Falla, D.; Rushton, A. What is the effect of prolonged sitting and physical activity on thoracic spine mobility? An observational study of young adults in a UK university setting. BMJ Open 2018, 8, e019371. [Google Scholar] [CrossRef]
- Downs, A.; Van Hoomissen, J.; Lafrenz, A.; Deana, L.; Julka, D.L. Accelerometer-Measured Versus Self-reported Physical Activity in College Students: Implications for Research and Practice. J. Am. Coll. Health 2014, 62, 204–212. [Google Scholar] [CrossRef]
- Raynor, D.A.; Jankowiak, N.M. Accelerometry-Determined Adherence to the 2008 Physical Activity Guidelines for Americans Among College Students. Am. J. Health Educ. 2010, 41, 353–362. [Google Scholar] [CrossRef]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P.; STROBE Initiative. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. J. Clin. Epidemiol. 2008, 61, 344–349. [Google Scholar] [CrossRef] [PubMed]
- Varni, J.W.; Limbers, C.A. The PedsQL™ 4.0 Generic Core Scales Young Adult Version: Feasibility, reliability and validity in a university student population. J. Health Psychol. 2009, 14, 611–622. [Google Scholar] [CrossRef]
- Grubić Kezele, T.; Medjimurec, S.; Bukarica, M.; Čorapović, A.; Fužinac-Smojver, A. Qoality of life and level of physical activity in primary school children with juvenile idiopathic arthritis in Primorje-Gorski Kotar County. Paediatr. Croat. 2019, 63, 145–152. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Erlbaum: Hillsdale, NJ, USA, 1988. [Google Scholar]
- Buysse, D.J.; Reynolds, C.F., 3rd; Monk, T.H.; Berman, S.R.; Kupfer, D.J. The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry. Res. 1989, 28, 93–213. [Google Scholar] [CrossRef]
- Grubić Kezele, T.; Trope, Z.; Ahel, V.; Ružić, N.; Omrčen, H.; Đudarić, L.; Fužinac-Smojver, A. Upper-lower limb and breathing exercise program for improving sleep quality and psychological status in multiple sclerosis: A pilot randomized controlled trial. Brain. Impair. 2023, 24, 86–102. [Google Scholar] [CrossRef]
- Wang, L.; Wu, Y.-X.; Lin, Y.Q.; Wang, L.; Zeng, Z.-N.; Xie, X.-L.; Chen, Q.-Y.; Wei, S.-C. Reliability and validity of the Pittsburgh Sleep Quality Index among frontline COVID-19 health care workers using classical test theory and item response theory. J. Clin. Sleep Med. 2022, 18, 541–551. [Google Scholar] [CrossRef]
- “Guidelines for the Data Processing and Analysis of the International Physical Activity Questionnaire” for More Detailed Description of IPAQ Analysis and Recommendations for Data Cleaning and Processing. Available online: https://sites.google.com/view/ipaq/score (accessed on 23 June 2023).
- Booth, M.L. Assessment of Physical Activity: An International Perspective. Res. Q. Exerc. Sport 2000, 71, 114–120. [Google Scholar] [CrossRef] [PubMed]
- Dinger, M.K.; Behrens, T.K.; Han, J.L. Validity and Reliability of the International Physical Activity Questionnaire in College Students. Am. J. Health Educ. 2006, 37, 337–343. [Google Scholar] [CrossRef]
- Craig, C.L.; Marshall, A.L.; Sjostrom, M.; Bauman, A.E.; Booth, M.L.; Ainsworth, B.E.; Pratt, M.; Ekelund, U.; Yngve, A.; Sallis, J.F.; et al. International Physical Activity Questionnaire: 12-country reliability and validity. Med. Sci. Sports Exerc. 2003, 35, 1381–1395. [Google Scholar] [CrossRef]
- Tanita Home Page. Available online: https://tanita.eu/understanding-your-measurements (accessed on 13 August 2022).
- Vasold, K.L.; Parks, A.C.; Phelan, D.M.L.; Pontifex, M.B.; Pivarnik, J.M. Reliability and Validity of Commercially Available Low-Cost Bioelectrical Impedance Analysis. Int. J. Sport Nutr. Exerc. Metab. 2019, 29, 406–410. [Google Scholar] [CrossRef]
- McGil, S.M.; Childs, A.; Liebenson, C. Endurance Times for Low Back Stabilization Exercises: Clinical Targets for Testing and Training from a Normal Database. Arch. Phys. Med. Rehabil. 1999, 80, 941–944. [Google Scholar] [CrossRef] [PubMed]
- Alaranta, H.; Hurri, H.; Heliövaara, M.; Soukka, A.; Harju, R. Non-dynamometric trunk performance tests: Reliability and normative data. Scand. J. Rehabil. Med. 1994, 26, 211–215. [Google Scholar] [CrossRef] [PubMed]
- Reiman, M.P.; Krier, A.D.; Nelson, J.A.; Rogers, M.A.; Stuke, Z.O.; Smith, B.S. Comparison of different trunk endurance testing methods in college aged individuals. IJSPT 2012, 7, 539. [Google Scholar]
- Kim, H.J.; Chung, S.; Kim, S.; Shin, H.; Lee, J.; Kim, S.; Song, M.Y. Influences of trunk muscles on lumbar lordosis and sacral angle. Eur. Spine J. 2006, 15, 409–414. [Google Scholar] [CrossRef]
- Yadav, R.; Mukhopadhyay, S.; Yadav, S. Physical fitness index of non-vegetarian and lacto-vegetarian adults: A comparative study of harvard step test. Nepal Med. Coll. J. 2020, 22, 167–172. [Google Scholar] [CrossRef]
- Dempsey, T.M.; Scanlon, P.D. Pulmonary Function Tests for the Generalist: A Brief Review. Mayo. Clin. Proc. 2018, 93, 763–771. [Google Scholar] [CrossRef]
- Ruppel, G. Lung volume tests. In Manual of Pulmonary Function Testing, 10th ed.; Ruppel, G., Ed.; Mosby: St. Louis, MO, USA, 1994; pp. 1–25. ISBN 978-0323762618. [Google Scholar]
- McArdle, W.D.; Katch, F.I.; Katch, V.L. Exercise Physiology: Nutrition, Energy, and Human Performance, 8th ed.; Wolters Kluwer Health/Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2015; ISBN 978-1451191554. [Google Scholar]
- Mejia, E.A.; Hennrikus, W.L.; Schwend, R.M.; Emans, J.B. A prospective evaluation of idiopathic left thoracic scoliosis with MRI. J. Pediatr. Orthop. 1996, 16, 354–358. [Google Scholar] [CrossRef] [PubMed]
- Tüzün, C.; Yorulmaz, I.; Cindaş, A.; Vatan, S. Low back pain and posture. Clin. Rheumatol. 1999, 18, 308–312. [Google Scholar] [CrossRef] [PubMed]
- Fadaee, E.; Seidi, F.; Rajabi, R. The validity and reliability of spinal mouse device in measuring angle values of thoracic kyphosis and lumbar lordosis. J. Shahrekord. Univ. Med. Sci. 2017, 19, 137–147. [Google Scholar]
- Csepregi, É.; Gyurcsik, Z.; Veres-Balajti, I.; Nagy, A.C.; Szekanecz, Z.; Szántó, S. Effects of Classical Breathing Exercises on Posture, Spinal and Chest Mobility among Female University Students Compared to Currently Popular Training Programs. Int. J. Environ. Res. Public Health 2022, 19, 3728. [Google Scholar] [CrossRef] [PubMed]
- Cepková, A.; Zemková, E.; Šooš, Ľ.; Uvaček, M.; Muyor, J.M. Spinal curvature in female and male university students with prolonged bouts of sedentary behaviour. Res. Sq. Preprint 2022. [Google Scholar] [CrossRef]
- Hanna, F.; Daas, R.N. The relationship between sedentary behavior, back pain, and psychosocial correlates among university employees. Front. Public Health 2019, 7, 80. [Google Scholar] [CrossRef]
- WHO. Set of Recommendations on the Marketing of Foods and Non-Alcoholic Beverages to Children. WHO Home Page. Available online: https://apps.who.int/iris/handle/10665/44416 (accessed on 24 April 2023).
- Zanovec, M.; Lakkakula, A.P.; Johnson, L.G.; Turri, G. Physical Activity is Associated with Percent Body Fat and Body Composition but not Body Mass Index in White and Black College Students. Int. J. Exerc. Sci. 2009, 15, 175–185. [Google Scholar]
- You, H.W.; Tan, P.L.; Mat Ludin, A.F. The Relationship between Physical Activity, Body Mass Index and Body Composition among Students at a Pre-University Centre in Malaysia. Int. Med. J. Malays. 2020, 19. [Google Scholar] [CrossRef]
- Ode, J.J.; Pivarnik, J.M.; Reeves, M.J.; Knous, J.L. Body mass index as a predictor of percent fat in college athletes and nonathletes. Med. Sci. Sports Exerc. 2007, 39, 403–409. [Google Scholar] [CrossRef]
- Deurenberg, P.; Deurenberg, Y.M.; Wang, J.; Lin, F.P.; Schmidt, G. The impact of body build on the relationship between body mass index and percent body fat. Int. J. Obes. Relat. Metab. Disord. 1999, 23, 537–542. [Google Scholar] [CrossRef]
- Grubić Kezele, T.; Babić, M.; Štimac, D. Exploring the feasibility of a mild and short 4-week combined upper limb and breathing exercise program as a possible home base program to decrease fatigue and improve quality of life in ambulatory and non-ambulatory multiple sclerosis individuals. Neurol. Sci. 2019, 40, 733–743. [Google Scholar] [CrossRef] [PubMed]
- Grubić Kezele, T.; Fužinac-Smojver, A.; Ćurko-Cofek, B.; Jakovac, H.; Turković, K. Adult neurogenesis—Accent on subgranular and subventricular zone in mammals. Med. Flum. 2017, 53, 134–146. [Google Scholar] [CrossRef][Green Version]
- Scisciola, L.; Fontanella, R.A.; Surina; Cataldo, V.; Paolisso, G.; Barbieri, M. Sarcopenia and Cognitive Function: Role of Myokines in Muscle Brain Cross-Talk. Life 2021, 11, 173. [Google Scholar] [CrossRef] [PubMed]
- Lin, T.W.; Kuo, Y.M. Exercise benefits brain function: The monoamine connection. Brain Sci. 2013, 11, 39–53. [Google Scholar] [CrossRef] [PubMed]
- Walsh, E.I.; Smit, L.; Northey, J.; Rattray, B.; Cherbuin, N. Towards an understanding of the physical activity-BDNF-cognition triumvirate: A review of associations and dosage. Ageing Res. Rev. 2020, 60, 101044. [Google Scholar] [CrossRef] [PubMed]
- Choosingtherapy Home Page. Available online: https://www.choosingtherapy.com/tanya-peterson-ncc/ (accessed on 24 April 2023).
- Wu, X.; Tao, S.; Zhang, Y.; Zhang, S.; Tao, F. Low physical activity and high screen time can increase the risks of mental health problems and poor sleep quality among Chinese college students. PLoS ONE 2015, 10, e0119607. [Google Scholar] [CrossRef]
- Liu, W.; Yuan, Q.; Zeng, N.; McDonough, D.J.; Tao, K.; Peng, Q.; Gao, Z. Relationships between College Students’ Sedentary Behavior, Sleep Quality, and Body Mass Index. Int. J. Environ. Res. Public Health 2021, 18, 3946. [Google Scholar] [CrossRef]
- Santos, M.; Sirtoli, R.; Rodrigues, R.; López-Gil, J.F.; Martínez-Vizcaíno, V.; Guidoni, C.M.; Mesas, A.E. Relationship between free-time physical activity and sleep quality in Brazilian university students. Sci. Rep. 2023, 13, 6652. [Google Scholar] [CrossRef]
- Biswas, A.; Oh, P.I.; Faulkner, G.E.; Bajaj, R.R.; Silver, M.A.; Mitchell, M.S.; Alter, D.A. Sedentary time and its association with risk for disease incidence, mortality, and hospitalization in adults: A systematic review and meta analysis. Ann. Intern. Med. 2015, 162, 123–132. [Google Scholar] [CrossRef]
- Jankowicz-Szymańska, A.; Bibro, M.; Wódka, K.; Smoła, E. The influence of age on the body posture of women. Health Promot. Phys. Act. 2018, 1, 1–6. [Google Scholar] [CrossRef]
- Granata, K.P.; Slota, G.P.; Wilson, S.E. Influence of fatigue in neuromuscular control of spinal stability. Hum. Factors 2004, 46, 81–91. [Google Scholar] [CrossRef] [PubMed]
- Taspinar, F.; ISaracoglu, I.; Afsar, E.; Okur, E.O.; Seyyar, G.K.; Kurt, G.; Taspinar, B. Assessing the Relationship between Body Composition and Spinal Curvatures in Young Adults. Arch. Sports Med. Physiother. 2017, 2, 10–15. [Google Scholar] [CrossRef]
- Mirbagheri, S.S.; Rahmani-Rasa, A.; Farmani, F.; Amini, P.; Nikoo, M.R. Evaluating Kyphosis and Lordosis in Students by Using a Flexible Ruler and Their Relationship with Severity and Frequency of Thoracic and Lumbar Pain. Asian Spine J. 2015, 9, 416–422. [Google Scholar] [CrossRef] [PubMed]
- Hamaoka, K.; Ashizawa, R.; Hida, M.; Suganuma, I.; Yoshimoto, Y. Chronic Lumbar Pain and Insomnia in College-Aged Students. Healthcare 2022, 10, 701. [Google Scholar] [CrossRef]
- Nachemson, A. The lumbar spine. An orthopaedic challenge. Spine 1976, 1, 59–71. [Google Scholar] [CrossRef]
- Kljajević, V.; Stanković, M.; Ðorđević, D.; Trkulja-Petkovic’, D.; Jovanović, R.; Plazibat, K.; Oršolić, M.; Čurić, M.; Sporiš, G. Physical Activity and Physical Fitness among University Students-A Systematic Review. Int. J. Environ. Res. Public Health 2022, 19, 158. [Google Scholar] [CrossRef]
- Faull, O.K.; Cox, P.J.; Pattinson, K.T. Psychophysical Differences in Ventilatory Awareness and Breathlessness between Athletes and Sedentary Individuals. Front. Physiol. 2016, 7, 231. [Google Scholar] [CrossRef]
- Duffy, C.A.; Vogiatzis, A. First record of the sicklefin devilray Mobula tarapacana (Myliobatiformes: Mobulidae) from Australian waters. Zootaxa 2016, 4126, 141–145. [Google Scholar] [CrossRef]
| IPAQ-LF Domains | Mean ± SE |
|---|---|
| Type of PA (MET-min/wk) | |
| PA at work (MET-min/wk) PA during transport (MET-min/wk) PA at home or in garden (MET-min/wk) Recreation, sport, and leisure-time PA (MET-min/wk) | 1176.7 ± 259.4 926.3 ± 104.7 1002.2 ± 155.3 2469.6 ± 297.7 |
| Intensity of PA (MET-min/wk) | |
| Walking (MET-min/wk) Moderate PA (MET-min/wk) Vigorous PA (MET-min/wk) | 2184.8 ± 222.6 1523.3 ± 198.0 1865.4 ± 307.3 |
| Total PA (MET-min/wk) | 5573.9 ± 494.4 |
| Time spent sitting (min/wk) | 2489.7 ± 105.1 |
| Variable | Quartiles of Self-Reported PA (MET-min/wk) | |||||
|---|---|---|---|---|---|---|
| Q1 (672–2087) N (%) | Q2 (2088–4008) N (%) | Q3 (4009–8573) N (%) | Q4 (8574–22,062) N (%) | Total N (%) | p Value | |
| Gender | ||||||
| Female Male Total | 16 (19.5%) 3 (3.7%) 19 (23.2%) | 11 (13.4%) 9 (11.0%) 20 (24.4%) | 10 (12.2%) 11 (13.4%) 21 (25.6%) | 11 (13.4%) 11 (13.4%) 22 (26.8%) | 48 (58.5%) 34 (41.5%) 82 (100.0%) | a (df = 3) 0.703 |
| b BMI (kg/m2) | ||||||
| Normal Overweight Obese | 15 (18.3%) 4 (4.9%) 0 (0.0%) | 15 (18.3%) 3 (3.7%) 2 (2.5%) | 13 (15.8%) 7 (8.5%) 1 (1.2%) | 14 (17.1%) 7 (8.5%) 1 (1.2%) | 57 (69.5%) 21 (25.6%) 4 (4.9%) | a (df = 3) 0.549 |
| Body composition (Tanita RD-545) | ||||||
| c Visceral fat level | ||||||
| Healthy level rating | 19 (23.2%) | 20 (24.4%) | 21 (25.6%) | 22 (26.8%) | 82 (100.0%) | |
| Body fat (%) | ||||||
| Underfat Healthy Overweight Obese | 0 (0.0%) 14 (17.1%) 5 (6.1%) 0 (0.0%) | 1 (1.2%) 15 (18.3%) 2 (2.4%) 2 (2.4%) | 0 (0.0%) 14 (17.1%) 5 (6.1%) 2 (2.4%) | 1 (1.2%) 13 (15.9%) 5 (6.1%) 3 (3.7%) | 2 (2.4%) 56 (68.4%) 17 (20.7%) 7 (8.5%) | a (df = 9) 0.708 |
| Muscle mass (%) | ||||||
| Very low Low Good Increased | 0 (0.0%) 3 (3.7%) 16 (19.5%) 0 (0.0%) | 2 (2.4%) 1 (1.2%) 16 (19.5%) 1 (1.2%) | 2 (2.4%) 3 (3.7%) 16 (19.5%) 0 (0.0%) | 3 (3.7%) 2 (2.4%) 15 (18.3%) 2 (2.4%) | 7 (8.5%) 9 (11.0%) 63 (76.8%) 3 (3.7%) | a (df = 9) 0.594 |
| Physical activity (IPAQ-LF) | ||||||
| Minimum required PA per week | ||||||
| Sufficient Insufficient | 15 (18.3%) 4 (4.9%) | 1 (1.2%) 19 (23.2%) | 0 (0.0%) 21 (25.6%) | 1 (1.2%) 21 (25.6%) | 17 (20.7%) 65 (79.3%) | a (df = 3) 0.000 * |
| d PA level | ||||||
| Minimally active HEPA active | 15 (18.3%) 4 (4.9%) | 10 (12.2%) 10 (12.2%) | 10 (12.2%) 11 (13.4%) | 6 (7.3%) 16 (19.5%) | 41 (50.0%) 41 (50.0%) | a (df = 3) 0.012 * |
| Sleep quality (PSQI) | ||||||
| Good sleep quality Poor sleep quality | 3 (3.7%) 16 (19.5%) | 12 (14.6%) 8 (9.7%) | 7 (8.5%) 14 (17.0%) | 9 (11.0%) 13 (15.8%) | 31 (37.8%) 51 (62.2%) | a (df = 3) 0.038 * |
| Cardiovascular fitness (HST) | ||||||
| Poor Below average Average Good Excellent | 10 (11.7%) 0 (0.0%) 5 (6.7%) 1 (1.7%) 1 (1.7%) | 8 (10.0%) 3 (3.3%) 5 (6.7%) 4 (5.0%) 0 (0.0%) | 8 (10.0%) 1 (1.7%) 11 (13.3%) 0 (0.0%) 1 (1.7%) | 8 (10.0%) 3 (3.3%) 3 (3.3%) 5 (6.7%) 3 (3.3%) | 34 (41.7%) 7 (8.3%) 25 (30.0%) 11 (13.3%) 5 (6.7%) | a (df = 12) 0.269 |
| MVV (L/min) (Spirometry) | ||||||
| Below normal Normal | 0 (0.0%) 18 (21.7%) | 1 (1.7%) 19 (23.1%) | 2 (2.1%) 19 (23.1%) | 1 (1.7%) 22 (26.7%) | 4 (5.4%) 78 (94.6%) | a (df = 3) 0.613 |
| Variable | Quartiles of Self-Reported PA (MET-min/wk) | |||||
|---|---|---|---|---|---|---|
| Q1 (672–2087) N (%) | Q2 (2088–4008) N (%) | Q3 (4009–8573) N (%) | Q4 (8574–22,062) N (%) | Total N (%) | p Value | |
| Spinal curvatures (Spinal Mouse®) | ||||||
| a Thoracic kyphosis angle–straight posture (°) | ||||||
| Neutral kyphosis Hyperkyphosis | 7 (8.9%) 12 (14.3%) | 10 (12.6%) 9 (10.7%) | 7 (8.9%) 13 (16.1%) | 9 (10.7%) 15 (17.8%) | 33 (41.1%) 49 (58.9%) | b (df = 3) 0.697 |
| Lumbar lordosis angle–straight posture (°) | ||||||
| Hypolordosis Neutral lordosis Hyperlordosis | 0 (0.0%) 13 (16.0%) 6 (7.1%) | 0 (0.0%) 14 (17.9%) 4 (5.4%) | 3 (3.6%) 12 (14.3%) 6 (7.1%) | 0 (0.0%) 21 (25.0%) 3 (3.6%) | 3 (3.6%) 60 (73.2%) 19 (23.2%) | b (df = 6) 0.124 |
| Variable | Quartiles of Self-Reported PA (MET-min/wk) | |||||
|---|---|---|---|---|---|---|
| Q1 (672–2087) Mean ± SD or Median (Range) | Q2 (2088–4008) Mean ± SD or Median (Range) | Q3 (4009–8573) Mean ± SD or Median (Range) | Q4 (8574–22,062) Mean ± SD or Median (Range) | Total Mean ± SD or Median (Range) | p Value | |
| BMI (kg/m2) | 22.6 ± 2.5 | 23.5 ± 3.2 | 23.9 ± 2.6 | 24.9 ± 3.2 | 23.8 ± 2.9 | a Q1:Q2 = 0.781 Q1:Q3 = 0.560 Q1:Q4 = 0.089 Q2:Q3 = 0.982 Q2:Q4 = 0.457 Q3:Q4 = 0.672 |
| Body composition(Tanita RD-545) | ||||||
| Visceral fat level | 1.5 (1–4.5) | 2 (1–10) | 2.5 (1–4.5) | 3 (1–11) | 2 (1–11) | b 0.311 |
| Body fat (%) | 27.2 ± 5.8 | 24.6 ± 7.7 | 25 ± 8.3 | 24.6 ± 9.2 | 25.3 ± 7.8 | a Q1:Q2 = 0.751 Q1:Q3 = 0.835 Q1:Q4 = 0.750 Q2:Q3 = 0.998 Q2:Q4 = 1.000 Q3:Q4 = 0.998 |
| Muscle mass (%) | 68.9 ± 5.4 | 71.6 ± 7.3 | 71.2 ± 7.8 | 71.6 ± 8.8 | 70.9 ± 7.4 | a Q1:Q2 = 0.710 Q1:Q3 = 0.793 Q1:Q4 = 0.710 Q2:Q3 = 0.998 Q2:Q4 = 1.000 Q3:Q4 = 0.998 |
| Physique rating | 5 (1–5) | 5 (2–8) | 5 (2–6) | 5 (2–8) | 5 (1–8) | a Q1:Q2 = 0.671 Q1:Q3 = 0.978 Q1:Q4 = 0.909 Q2:Q3 = 0.876 Q2:Q4 = 0.963 Q3:Q4 = 0.992 |
| Physical activity (IPAQ-LF) | ||||||
| PA (MET-min/wk) | 1475 ± 421 | 3010 ± 567 | 5559 ± 1059 | 11,459 ± 4252 | 5574 ± 4478 | a Q1:Q2 = 0.000 * Q1:Q3 = 0.000 * Q1:Q4 = 0.000 * Q2:Q3 = 0.004 * Q2:Q4 = 0.000 * Q3:Q4 = 0.000 * |
| Time spent sitting (min/wk) | 2856 ± 1060 | 2629 ± 658 | 2477 ± 1001 | 2059 ± 924 | 2490 ± 952 | a Q1:Q4 = 0.046 * |
| PA level | 2 (2–3) | 2 (2–3) | 3 (2–3) | 3 (2–3) | 2 (2–3) | b 0.027 * |
| Quality of life (PedsQLTM) | ||||||
| Physical health | 79.3 ± 12.2 | 82.7 ± 11.6 | 89.7 ± 8.7 | 87.1 ± 11.1 | 84.9 ± 11.5 | a Q1:Q2 = 0.776 Q1:Q3 = 0.021 * Q1:Q4 = 0.133 Q2:Q3 = 0.180 Q2:Q4 = 0.580 Q3:Q4 = 0.860 |
| Psychosocial health | 78.9 ± 11.4 | 81.9 ± 11.5 | 81.5 ± 11.2 | 82.3 ± 9.8 | 81.2 ± 10.8 | a Q1:Q2 = 0.825 Q1:Q3 = 0.876 Q1:Q4 = 0.773 Q2:Q3 = 0.999 Q2:Q4 = 0.999 Q3:Q4 = 0.996 |
| Total score | 79.0 ± 10.1 | 82.2 ± 10.3 | 84.4 ± 9.5 | 83.9 ± 8.8 | 82.5 ± 9.7 | a Q1:Q2 = 0.774 Q1:Q3 = 0.324 Q1:Q4 = 0.400 Q2:Q3 = 0.888 Q2:Q4 = 0.938 Q3:Q4 = 0.998 |
| Sleep quality (PSQI) | 6 (2–11) | 4 (2–17) | 5 (2–8) | 5 (2–8) | 5 (2–17) | b 0.055 |
| Trunk muscle endurance | ||||||
| Trunk flexor test (sec) | 166.8 ± 32.4 | 174.7 ± 20.4 | 178.2 ± 7.0 | 180.0 ± 0.0 | 172.1 ± 21.8 | a Q1:Q2 = 0.149 Q1:Q3 = 0.253 Q1:Q4 = 0.149 Q2:Q3 = 0.990 Q2:Q4 = 1.000 Q3:Q4 = 0.988 |
| Trunk extensor test (sec) | 176.2 ± 13.8 | 136.3 ± 40.1 | 150.5 ± 37.8 | 152.1 ± 45.1 | 152.9 ± 38.6 | a Q1:Q2 = 0.039 * Q1:Q3 = 0.300 Q1:Q4 = 0.355 Q2:Q3 = 0.722 Q2:Q4 = 0.652 Q3:Q4 = 0.999 |
| Trunk extensor/flexor test ratio | 1.1 ± 0.2 | 0.7 ± 0.2 | 0.8 ± 0.2 | 0.9 ± 0.3 | 0.9 ± 0.2 | a Q1:Q2 = 0.014 * Q1:Q3 = 0.031 * Q1:Q4 = 0.066 Q2:Q3 = 0.914 Q2:Q4 = 0.427 Q3:Q4 = 0.802 |
| Spinal curvatures (Spinal Mouse®) | ||||||
| Thoracic kyphosis angle–straight posture (°) | 44.7 ± 10.3 | 47.0 ± 9.1 | 47.2 ± 6.1 | 46.9 ± 9.0 | 46.5 ± 8.7 | a Q1:Q2 = 0.919 Q1:Q3 = 0.896 Q1:Q4 = 0.925 Q2:Q3 = 0.999 Q2:Q4 = 0.999 Q3:Q4 = 0.999 |
| Lumbar lordosis angle–straight posture (°) | −34.9 ± 7.5 | −32.1 ± 8.6 | −32.0 ± 11.8 | −32.3 ± 9.2 | −32.8 ± 9.2 | a Q1:Q2 = 0.868 Q1:Q3 = 0.858 Q1:Q4 = 0.894 Q2:Q3 = 0.999 Q2:Q4 = 0.999 Q3:Q4 = 0.999 |
| Cardiovascular fitness (HST) | 54 ± 25 | 59 ± 19 | 60 ± 18 | 65 ± 22 | 59 ± 21 | a Q1:Q2 = 0.910 Q1:Q3 = 0.856 Q1:Q4 = 0.499 Q2:Q3 = 0.999 Q2:Q4 = 0.854 Q3:Q4 = 0.903 |
| MVV (L/min) (Spirometry) | 133.0 ± 35 | 153 ± 30 | 150 ± 31 | 151 ± 27 | 147 ± 31 | a Q1:Q2 = 0.325 Q1:Q3 = 0.479 Q1:Q4 = 0.447 Q2:Q3 = 0.991 Q2:Q4 = 0.995 Q3:Q4 = 0.999 |
| N = 82 | IPAQ-LF Measures | |||
|---|---|---|---|---|
| Variable | Vigorous PA (MET-min/wk) r/p | PA during Recreation, Sport and Leisure-Time (MET-min/wk) r/p | Total PA (MET-min/wk)r/p | Time Spent Sitting (min/wk) r/p |
| BMI (kg/m2) | 0.095/0.393 | 0.182/0.101 | 0.181/0.102 | −0.149/0181 |
| Body composition(Tanita RD-545) | ||||
| Visceral fat level | 0.199/0.859 | 0.121/0.276 | 0.077/0.490 | −0.144/0.195 |
| Body fat (%) | −0.254/0.021 * | −0.278/0.011 * | −0.158/0.156 | 0.041/0.716 |
| Muscle mass (%) | 0.260/0.018 * | 0.287/0.009 * | 0.165/0.137 | −0.078/0.486 |
| Physique rating | 0.154/0.166 | 0.111/0.318 | 0.101/0.364 | −0.010/0.929 |
| Quality of life (PedsQLTM) | ||||
| Physical health | 0.374/0.001 * | 0.416/0.000 * | 0.301/0.006 * | −0.246/0.026 * |
| Psychosocial health | 0.061/0.586 | 0.132/0.236 | 0.102/0.361 | −0.247/0.025 * |
| Total score | 0.197/0.075 | 0.266/0.015 * | 0.197/0.075 | −0.280/0.011 * |
| Sleep quality (PSQI) | −0.125/0.263 | −0.243/0.028 * | −0.135/0.226 | 0.142/0.202 |
| Trunk muscle endurance | ||||
| Trunk flexor test (sec) | 0.041/0.710 | −0.033/0.764 | −0.027/0.805 | −0.081/0.464 |
| Trunk extensor test (sec) | 0.070/0.530 | −0.013/0.907 | −0.006/0.956 | −0.058/0.604 |
| Trunk extensor/flexor test ratio | −0.067/0.546 | 0.002/0.980 | 0.0107/0.924 | 0.056/0.616 |
| Spinal curvatures (Spinal Mouse®) | ||||
| Thoracic kyphosis angle-straight posture (°) | 0.062/0.648 | 0.095/0.484 | 0.081/0.557 | 0.012/0.925 |
| Lumbar lordosis angle-straight posture (°) | −0.006/0.962 | −0.078/0.566 | −0.040/0.765 | −0.005/0.967 |
| Cardiovascular fitness (HST) | 0.199/0.140 | 0.221/0.100 | 0.214/0.100 | −0.093/0.493 |
| MVV (L/min) (Spirometry) | 0.175/0.196 | 0.341/0.010 * | 0.169/0.195 | −0.053/0.697 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Marijančić, V.; Grubić Kezele, T.; Peharec, S.; Dragaš-Zubalj, N.; Pavičić Žeželj, S.; Starčević-Klasan, G. Relationship between Physical Activity and Sedentary Behavior, Spinal Curvatures, Endurance and Balance of the Trunk Muscles-Extended Physical Health Analysis in Young Adults. Int. J. Environ. Res. Public Health 2023, 20, 6938. https://doi.org/10.3390/ijerph20206938
Marijančić V, Grubić Kezele T, Peharec S, Dragaš-Zubalj N, Pavičić Žeželj S, Starčević-Klasan G. Relationship between Physical Activity and Sedentary Behavior, Spinal Curvatures, Endurance and Balance of the Trunk Muscles-Extended Physical Health Analysis in Young Adults. International Journal of Environmental Research and Public Health. 2023; 20(20):6938. https://doi.org/10.3390/ijerph20206938
Chicago/Turabian StyleMarijančić, Verner, Tanja Grubić Kezele, Stanislav Peharec, Nataša Dragaš-Zubalj, Sandra Pavičić Žeželj, and Gordana Starčević-Klasan. 2023. "Relationship between Physical Activity and Sedentary Behavior, Spinal Curvatures, Endurance and Balance of the Trunk Muscles-Extended Physical Health Analysis in Young Adults" International Journal of Environmental Research and Public Health 20, no. 20: 6938. https://doi.org/10.3390/ijerph20206938
APA StyleMarijančić, V., Grubić Kezele, T., Peharec, S., Dragaš-Zubalj, N., Pavičić Žeželj, S., & Starčević-Klasan, G. (2023). Relationship between Physical Activity and Sedentary Behavior, Spinal Curvatures, Endurance and Balance of the Trunk Muscles-Extended Physical Health Analysis in Young Adults. International Journal of Environmental Research and Public Health, 20(20), 6938. https://doi.org/10.3390/ijerph20206938








