Mortality in Germany during the COVID-19 Pandemic
Abstract
:1. Introduction
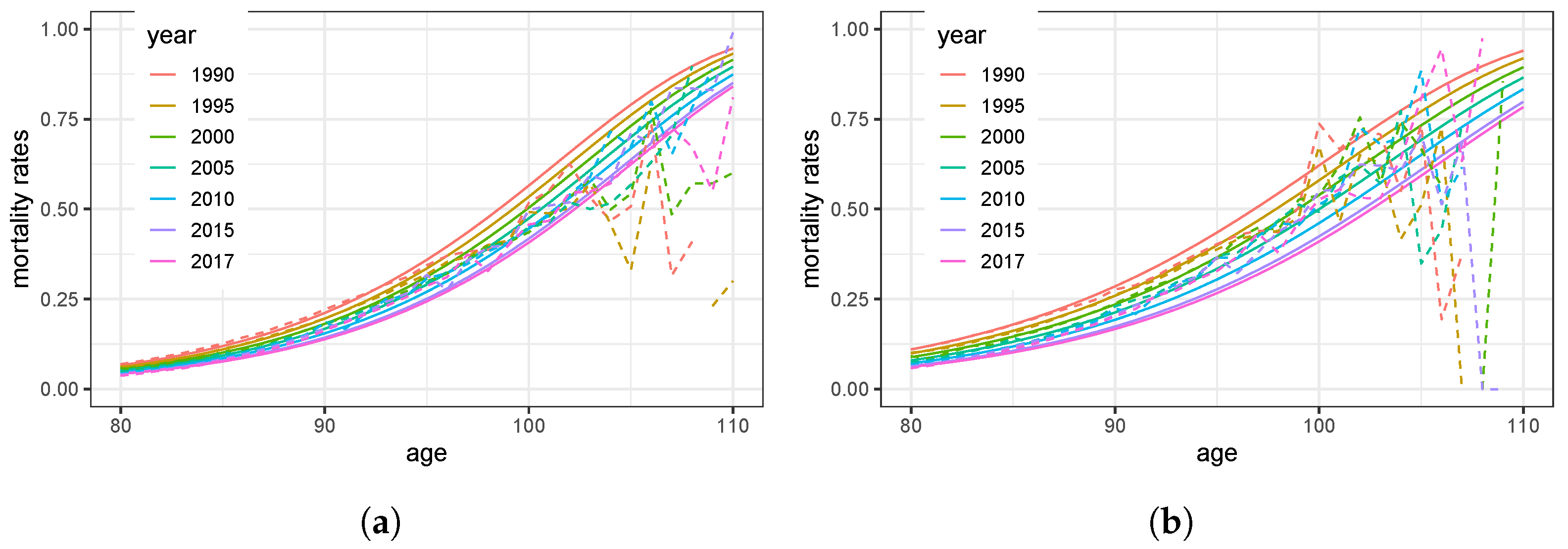
Study of several single-year extinct birth cohorts shows that mortality trajectory at advanced ages follows Gompertz’s law up to the ages 102–105 years without a noticeable deceleration.
2. Materials and Methods
2.1. Available Data
2.2. Mortality Model
2.2.1. Parametric Mortality Model
2.2.2. Decreasing Mortality, Year by Year
2.3. Estimation of Parameters
2.4. Analysis of Excess Mortality
- (i)
- if more deaths are recorded than expected, and (i.e., much greater than 1), which indicates excess mortality for the group with age x;
- (ii)
- The score in (6) is sensitive with respect to the estimated mean, and even vanishes for the crude estimator ;
- (iii)
- As follows from the central limit theorem, the quantity (6) is asymptotically normally distributed with standard parameters () for the true parameter ;
- (iv)
- For the estimate , the score (6) is the crucial quantity in our following analysis, as positive aberrations (i.e., ) indicate excess mortality for the specific age x;
- (v)
3. Results
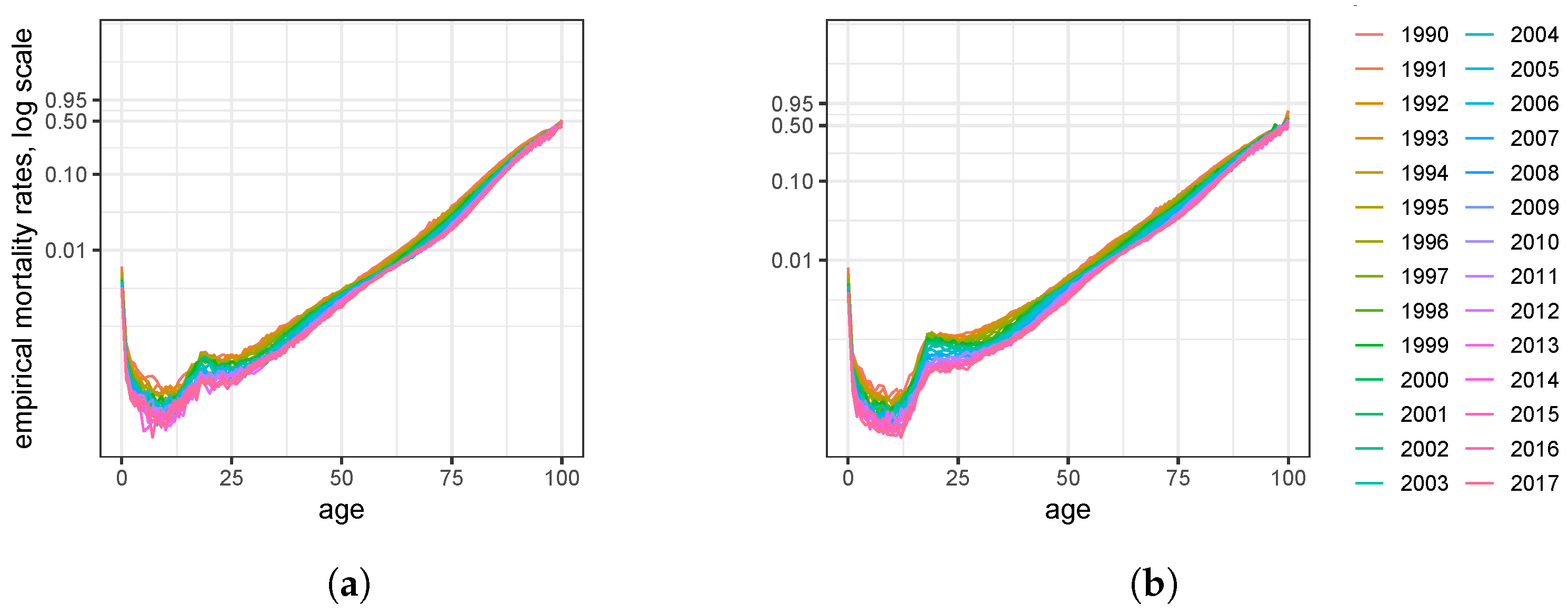
3.1. Estimators and Model Validation
3.1.1. Parameters Characterizing the Mortality of the German Population
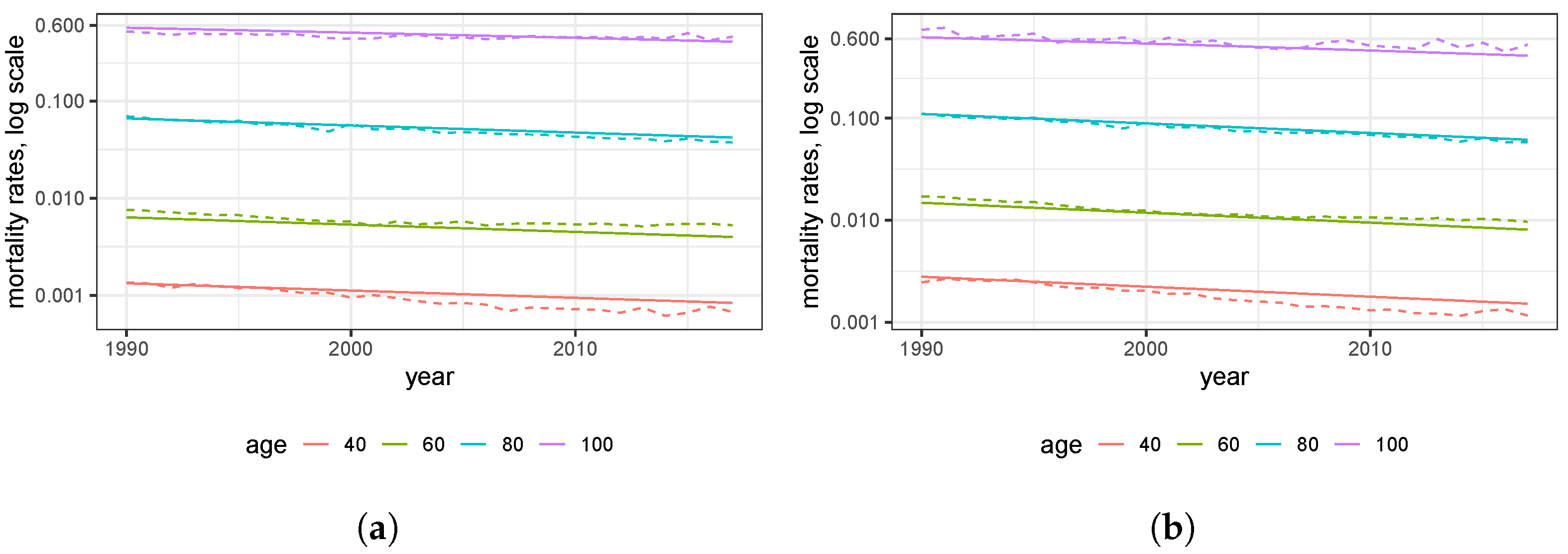
3.1.2. Mortality Trend
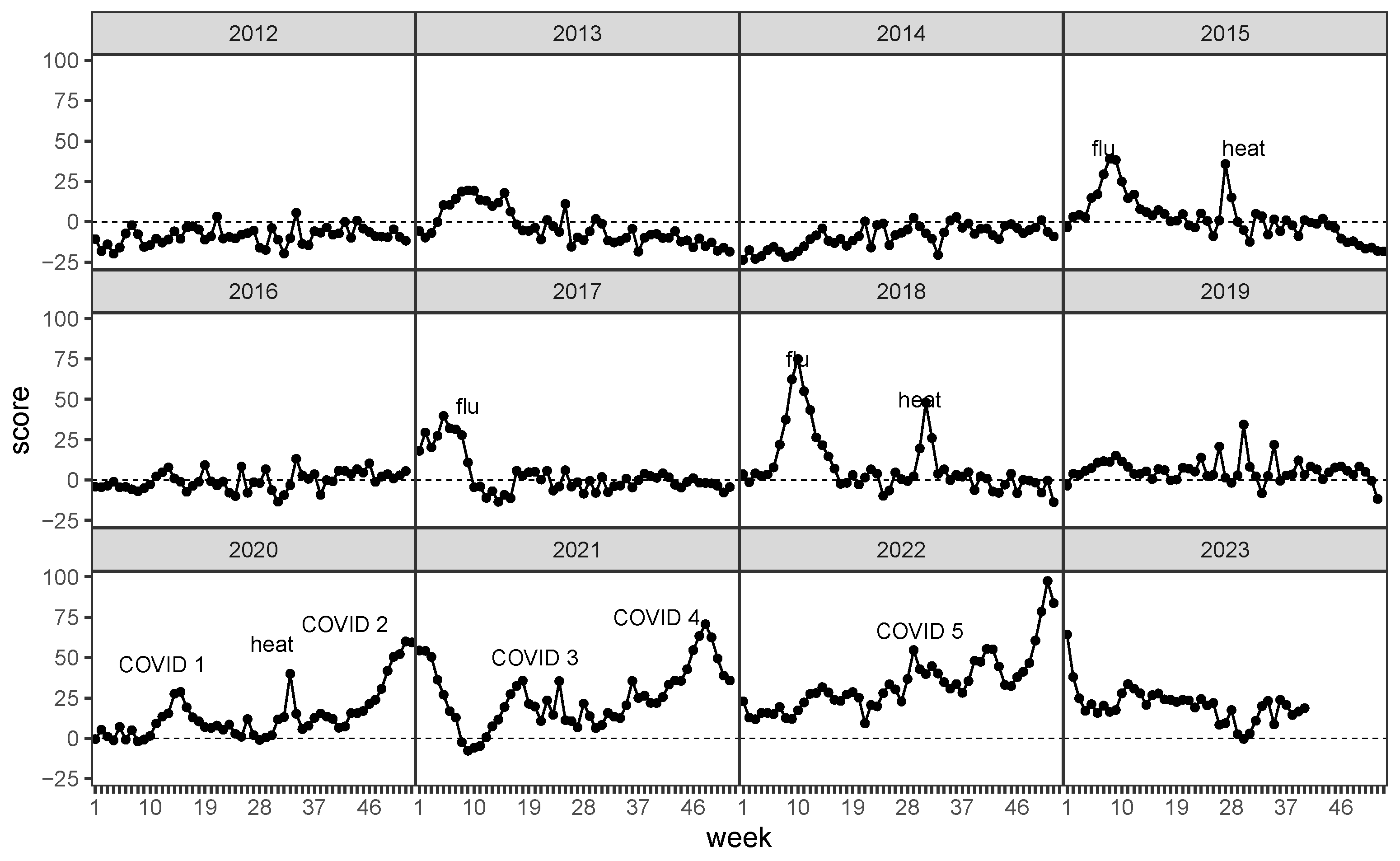
3.2. Z-Scores of the Training Data
4. Discussion
4.1. Historic Mortality Rates, Compared to COVID-19 (2020 to 2023)
- COVID-19;
- heat waves in summer;
- flu waves in winter.
4.2. Mortality of the Elderly Population
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
Appendix B
References
- Statistisches Bundesamt. Number of Deaths and Excess Mortality Weekly Deaths in Germany. Available online: https://www.destatis.de/EN/Themes/Cross-Section/Corona/Society/population_death.html (accessed on 10 October 2023).
- Koch-Institut, R. Influenza Assozierte Übersterblichkeit (Exzess-Mortalität) in Deutschland für Die Saisons von 1984 bis 2022. Statista GmbG. Zugriff 14. 2023 Juli. Available online: https://de.statista.com/statistik/daten/studie/405363/umfrage/influenza-assozierte-uebersterblichkeit-exzess-mortalitaet-in-deutschland/ (accessed on 14 July 2023).
- Impfen, N.L. Gemeldete Influenza-Krankheitsfälle in Deutschland. Available online: https://www.nali-impfen.de/monitoring-daten/krankheitsfaelle-in-deutschland/influenza/ (accessed on 14 July 2023).
- Zeng, H.; Lan, T.; Chen, Q. Five and four-parameter lifetime distributions for bathtub-shaped failure rate using Perks mortality equation. Reliab. Eng. Syst. Saf. 2016, 152, 307–315. [Google Scholar] [CrossRef]
- Missov, T.I.; Lenart, A.; Nemeth, L.; Canudas-Romo, V.; Vaupel, J.W. The Gompertz force of mortality in terms of the modal age at death. Demogr. Res. 2015, 32, 1031–1048. [Google Scholar] [CrossRef]
- Cohen, J.E.; Bohk, C.; Rau, R. Gompertz, Makeham, and Siler models explain Taylor’s law in human mortality data. Demogr. Res. 2018, 38, 773–842. [Google Scholar] [CrossRef]
- Gavrilov, L.A.; Gavrilova, N.S. Mortality Measurement at Advanced Ages: A Study of the Social Security Administration Death Master File. N. Am. Actuar. J. 2016, 12, 432–447. [Google Scholar] [CrossRef] [PubMed]
- Kontis, V.; Bennett, J.E.; Rashid, T.; Parks, R.M.; Pearson-Stuttard, J.; Guillot, M.; Asaria, P.; Zhou, B.; Battaglini, M.; Corsetti, G.; et al. Magnitude, demographics and dynamics of the effect of the first wave of the COVID-19 pandemic on all-cause mortality in 21 industrialized countries. Nat. Med. 2020, 26, 1919–1928. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Paulson, K.R.; Pease, S.A.; Watson, S.; Comfort, H.; Zheng, P.; Aravkin, A.Y.; Bisignano, C.; Barber, R.M.; Alam, T.; et al. Estimating excess mortality due to the COVID-19 pandemic: A systematic analysis of COVID-19-related mortality, 2020–21. Lancet 2022, 399, 1513–1536. [Google Scholar] [CrossRef] [PubMed]
- Karlinsky, A.; Kobak, D. Tracking excess mortality across countries during the COVID-19 pandemic with the World Mortality Dataset. eLife 2021, 10, e69336. [Google Scholar] [CrossRef] [PubMed]
- Nepomuceno, M.R.; Klimkin, I.; Jdanov, D.A.; Alustiza-Galarza, A.; Shkolnikov, V.M. Sensitivity Analysis of Excess Mortality due to the COVID-19 Pandemic. Popul. Dev. Rev. 2022, 48, 279–302. [Google Scholar] [CrossRef] [PubMed]
- Kowall, B.; Standl, F.; Oesterling, F.; Brune, B.; Brinkmann, M.; Dudda, M.; Pflaumer, P.; Jöckel, K.H.; Stang, A. Excess mortality due to COVID-19? A comparison of total mortality in 2020 with total mortality in 2016 to 2019 in Germany, Sweden and Spain. PLoS ONE 2021, 16, e0255540. [Google Scholar] [CrossRef] [PubMed]
- Achilleos, S.; Quattrocchi, A.; Gabel, J.; Heraclides, A.; Kolokotroni, O.; Constantinou, C.; Pagola Ugarte, M.; Nicolaou, N.; Rodriguez-Llanes, J.M.; Bennett, C.M.; et al. Excess all-cause mortality and COVID-19-related mortality: A temporal analysis in 22 countries, from January until August 2020. Int. J. Epidemiol. 2021, 51, 35–53. [Google Scholar] [CrossRef]
- Takahashi, Y.; Tanaka, H.; Koga, Y.; Takiguchi, S.; Ogimoto, S.; Inaba, S.; Matsuoka, H.; Miyajima, Y.; Takagi, T.; Irie, F.; et al. Change over Time in the Risk of Death among Japanese COVID-19 Cases Caused by the Omicron Variant Depending on Prevalence of Sublineages. Int. J. Environ. Res. Public Health 2023, 20, 2779. [Google Scholar] [CrossRef]
- Pérez-Gilaberte, J.B.; Martín-Iranzo, N.; Aguilera, J.; Almenara-Blasco, M.; de Gálvez, M.V.; Gilaberte, Y. Correlation between UV Index, Temperature and Humidity with Respect to Incidence and Severity of COVID 19 in Spain. Int. J. Environ. Res. Public Health 2023, 20, 1973. [Google Scholar] [CrossRef] [PubMed]
- Pisaturo, M.; Russo, A.; Pattapola, V.; Astorri, R.; Maggi, P.; Numis, F.G.; Gentile, I.; Sangiovanni, V.; Rossomando, A.; Gentile, V.; et al. Clinical Characterization of the Three Waves of COVID-19 Occurring in Southern Italy: Results of a Multicenter Cohort Study. Int. J. Environ. Res. Public Health 2022, 19, 16003. [Google Scholar] [CrossRef] [PubMed]
- El Fatinim, M.; El Khalifi, M.; Gerlach, R.; Pettersson, R. Bayesian forecast of the basic reproduction number during the COVID-19 epidemic in Morocco and Italy. Math. Popul. Stud. 2021, 28, 228–242. [Google Scholar] [CrossRef]
- Cairns, A.J.G.; Blake, D.P.; Kessler, A.; Kessler, M. The Impact of COVID-19 on Future Higher-Age Mortality. SSRN Electron. J. 2020. [Google Scholar] [CrossRef]
- Németh, L.; Jdanov, D.A.; Shkolnikov, V.M. An open-sourced, web-based application to analyze weekly excess mortality based on the Short-term Mortality Fluctuations data series. PLoS ONE 2021, 16, e0246663. [Google Scholar] [CrossRef] [PubMed]
- German Federal Statistical Office: Statistisches Bundesamt (Destatis). Available online: https://www.destatis.de/DE/Themen/Gesellschaft-Umwelt/Bevoelkerung/Sterbefaelle-Lebenserwartung/Tabellen/sonderauswertung-sterbefaelle.html?nn=209016 (accessed on 17 October 2023).
- German Federal Statistical Office: Population Data by Statistisches Bundesamt (Destatis). Population Data by Gender, Age and Year in Table 12411-0006. 2023. Available online: https://www-genesis.destatis.de/genesis//online?operation=table&code=12411-0006&bypass=true&levelindex=0&levelid=1697636155272#abreadcrumb (accessed on 16 October 2023).
- German Federal Statistical Office: Population Data by Statistisches Bundesamt (Destatis). Period Mortalities in Table 12621-0001. 2023. Available online: https://www-genesis.destatis.de/genesis//online?operation=table&code=12621-0001&bypass=true&levelindex=0&levelid=1697635998434#abreadcrumb (accessed on 16 October 2023).
- Richards, S.J. A handbook of parametric survival models for actuarial use. Scand. Actuar. J. 2012, 2012, 233–257. [Google Scholar] [CrossRef]
- Osmond, C. Using Age, Period and Cohort Models to Estimate Future Mortality Rates. Int. J. Epidemiol. 1985, 14, 124–129. [Google Scholar] [CrossRef]
- Keyfitz, N.; Caswell, H. Applied Mathematical Demography. In Statistics for Biology and Health; Springer: New York, NY, USA, 2008. [Google Scholar]
- Cairns, A.J.G.; Blake, D.P.; Dowd, K.; Coughlan, G.D.; Epstein, D.; Ong, A.; Balevich, I. A Quantitative Comparison of Stochastic Mortality Models Using Data From England and Wales and the United States. N. Am. Actuar. J. 2009, 13, 1–35. [Google Scholar] [CrossRef]
- Denuit, M.; Hainaut, D.; Trufin, J. Effective Statistical Learning Methods for Actuaries I; Springer International Publishing: Berlin/Heidelberg, Germany, 2019. [Google Scholar] [CrossRef]
- Rischatsch, M.; Pain, D.; Ryan, D.; Chiu, Y. Mortality Improvement: Understanding the Past and Framing the Future; Sigma; Swiss Re: Zurich, Switzerland, 2018; Volume 6, Available online: https://www.swissre.com/dam/jcr:81871581-01f0-450a-adec-37cc5f6534e0/sigma6_2018_en.pdf (accessed on 16 October 2023).
- Pichler, A.; Uhlig, D. Mortality in Germany during the COVID-19 pandemic. arXiv 2021, arXiv:2107.12899. [Google Scholar]
- Human Mortality Database. University of California, Berkeley (USA), and Max Planck Institute for Demographic Research (Germany). Available online: https://mortality.org/ (accessed on 9 February 2021).



| Mode M in Years | / Year | ||||
|---|---|---|---|---|---|
| women | |||||
| men |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pichler, A.; Uhlig, D. Mortality in Germany during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2023, 20, 6942. https://doi.org/10.3390/ijerph20206942
Pichler A, Uhlig D. Mortality in Germany during the COVID-19 Pandemic. International Journal of Environmental Research and Public Health. 2023; 20(20):6942. https://doi.org/10.3390/ijerph20206942
Chicago/Turabian StylePichler, Alois, and Dana Uhlig. 2023. "Mortality in Germany during the COVID-19 Pandemic" International Journal of Environmental Research and Public Health 20, no. 20: 6942. https://doi.org/10.3390/ijerph20206942
APA StylePichler, A., & Uhlig, D. (2023). Mortality in Germany during the COVID-19 Pandemic. International Journal of Environmental Research and Public Health, 20(20), 6942. https://doi.org/10.3390/ijerph20206942






