Healthy Eating as Potential Mediator of Inverse Association between Purpose in Life and Waist Circumference: Emerging Evidence from US and Chilean Cohorts
Abstract
:1. Introduction
2. Materials and Methods
2.1. Samples
2.2. Purpose in Life Assessment
2.3. Healthy Eating Pattern Evaluation
2.4. Sociodemographic, Anthropometric, and Physical Activity Information
2.5. Statistics
2.6. Ethics
3. Results
3.1. Healthy Eating Indexes and Sense of Purpose by Sociodemographic Characteristics and Nutritional Status in MIDUS and CHILEMED
3.2. Association between Sense of Purpose and Healthy Eating in MIDUS and CHILEMED
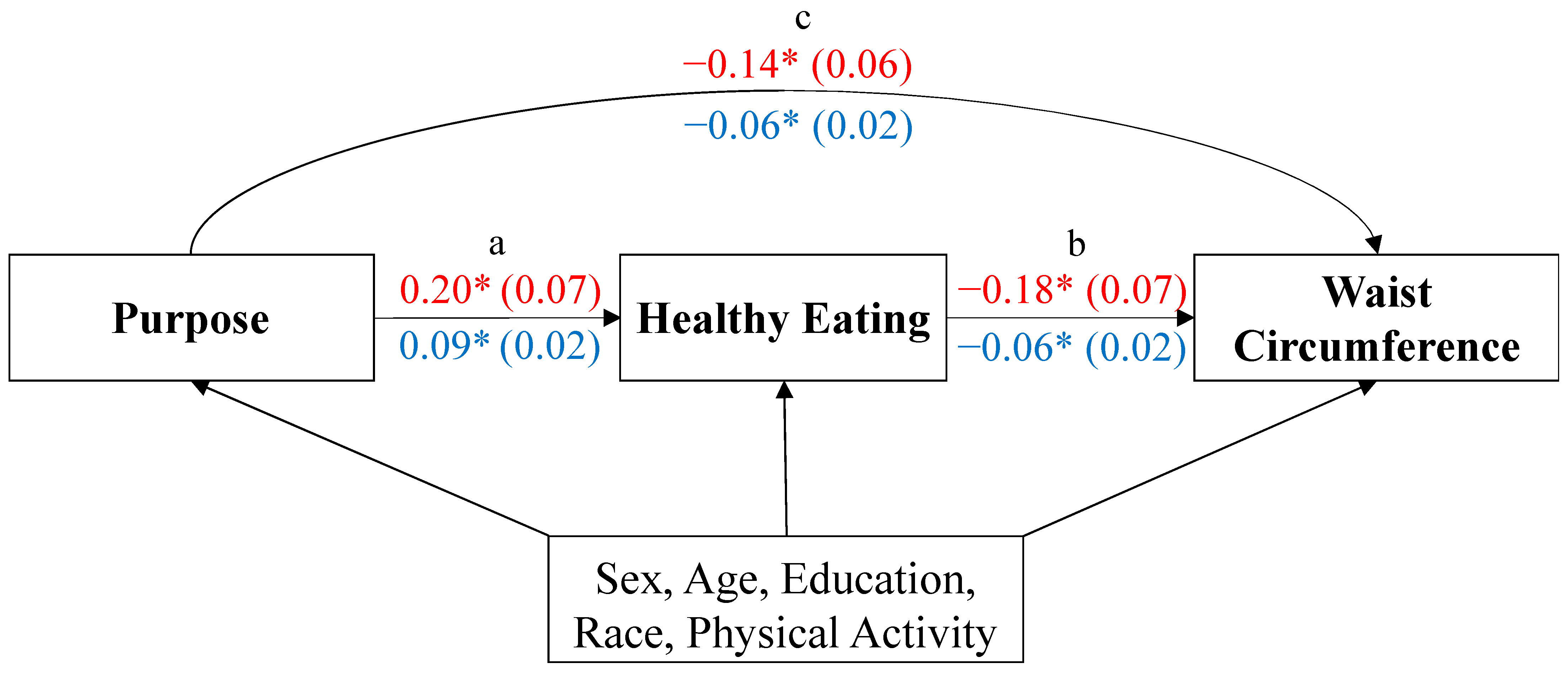
3.3. Inverse Relationship between Purpose in Life and Waist Circumference: Healthy Eating as Potential Mediator
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- The John Templeton Foundation. Psychology of Purpose; The John Templeton Foundation: West Conshohocken, PA, USA, 2018. [Google Scholar]
- Ryff, C.D. Happiness is everything, or is it? Explorations on the meaning of psychological wellbeing. J. Pers. Social Psychol. 1989, 57, 1069–1081. [Google Scholar] [CrossRef]
- Damon, W.; Menon, J.; Bronk, K.C. The development of purpose during adolescence. Appl. Develop Sci. 2003, 7, 119–128. [Google Scholar] [CrossRef]
- Scheier, M.F.; Wrosch, C.; Baum, A.; Cohen, S.; Martire, L.M.; Matthews, K.A.; Schulz, R.; Zdaniuk, B. The life engagement test: Assessing purpose in life. J. Behav. Med. 2006, 29, 291–298. [Google Scholar] [CrossRef] [PubMed]
- McKnight, P.E.; Kashdan, T.B. Purpose in life as a system that creates and sustains health and well-being: An integrative, testable theory. Rev. Gen. Psychol. 2009, 13, 242–251. [Google Scholar] [CrossRef]
- Bronk, K.C. Purpose in Life: A Critical Component of Optimal Youth Development, 1st ed.; Springer Science & Business Media: Berlin/Heidelberg, Germany, 2014. [Google Scholar]
- George, L.S.; Park, C.L. Are meaning and purpose distinct? An ex-amination of correlates and predictors. J. Posit. Psychol. 2013, 8, 365–375. [Google Scholar] [CrossRef]
- Heintzelman, S.J.; King, L.A. Life is pretty meaningful. Am. Psychol. 2014, 69, 561–574. [Google Scholar] [CrossRef]
- George, L.S.; Park, C.L. Meaning in life as comprehension, purpose, and mattering: Toward integration and new research questions. Rev. Gen. Psychol. 2016, 20, 205–220. [Google Scholar] [CrossRef]
- Martela, F.; Steger, M.F. The three meanings of meaning in life: Distinguishing coherence, purpose, and significance. J. Posit. Psychol. 2016, 11, 531–545. [Google Scholar] [CrossRef]
- Kumano, M. On the concept of well-being in Japan: Feeling shiawase as hedonic well-being and feeling ikigai as eudaimonic well-being. Appl. Res. Qual. Life 2017, 13, 419–433. [Google Scholar] [CrossRef]
- Kim, E.S.; Delaney, S.W.; Kubzansky, L.D. Sense of Purpose in Life and Cardiovascular Disease: Underlying Mechanisms and Future Directions. Curr. Cardiol. Rep. 2019, 21, 135. [Google Scholar] [CrossRef]
- Morozink, J.A.; Friedman, E.M.; Coe, C.L.; Ryff, C.D. Socioeconomic and psychosocial predictors of interleukin-6 in the MIDUS national sample. Health Psychol. 2010, 29, 626–635. [Google Scholar] [CrossRef] [PubMed]
- Cole, S.W.; Levine, M.E.; Arevalo, J.M.G.; Ma, J.; Weir, D.R.; Crimmins, E.M. Loneliness, eudaimonia, and the human conserved transcriptional response to adversity. Psychoneuroendocrinology 2015, 62, 11–17. [Google Scholar] [CrossRef] [PubMed]
- Guimond, A.J.; Shiba, K.; Kim, E.S.; Kubzansky, L.D. Sense of purpose in life and inflammation in healthy older adults: A longitudinal study. Psychoneuroendocrinology 2022, 141, 105746. [Google Scholar] [CrossRef] [PubMed]
- Tsenkova, V.K.; Love, G.D.; Singer, B.H.; Ryff, C.D. Socioeconomic status and psychological well-being predict cross-time change in glycosylated hemoglobin in older women without diabetes. Psychosom. Med. 2007, 69, 777–784. [Google Scholar] [CrossRef]
- Rasmussen, N.H.; Smith, S.A.; Maxson, J.A.; Bernard, M.E.; Cha, S.S.; Agerter, D.C.; Shah, N.D. Association of HbA1c with emotion regulation, intolerance of uncertainty, and purpose in life in type 2 diabetes mellitus. Prim. Care Diabetes 2013, 7, 213–221. [Google Scholar] [CrossRef]
- Boylan, J.M.; Tsenkova, V.K.; Miyamoto, Y.; Ryff, C.D. Psychological resources and gluco-regulation in Japanese adults: Findings from MIDJA. Health Psychol. 2017, 36, 449–457. [Google Scholar] [CrossRef]
- Hafez, D.; Heisler, M.; Choi, H.; Ankuda, C.K.; Winkelman, T.; Kullgren, J.T. Association between purpose in life and glucose control among older adults. Ann. Behav. Med. 2018, 52, 309–318. [Google Scholar] [CrossRef]
- Cohen, R.; Bavishi, C.; Rozanski, A. Purpose in life and its relationship to all-cause mortality and cardiovascular events: A meta-analysis. Psychosom. Med. 2016, 78, 122–133. [Google Scholar] [CrossRef]
- Kim, G.; Shin, S.H.; Scicolone, M.A.; Parmelee, P. Purpose in Life Protects against Cognitive Decline among Older Adults. Am. J. Geriatr. Psychiatry 2019, 27, 593–601. [Google Scholar] [CrossRef]
- Sutin, D.A.R.; Luchetti, M.; Aschwanden, D.; Stephan, Y.; Sesker, A.A.; Terracciano, A. Sense of meaning and purpose in life and risk of incident dementia: New data and meta-analysis. Arch. Gerontol. Geriatr. 2023, 105, 104847. [Google Scholar] [CrossRef]
- Shiba, K.; Kubzansky, L.D.; Williams, D.R.; VanderWeele, T.J.; Kim, E.S. Associations between Purpose in Life Mortality by SES. Am. J. Prev. Med. 2021, 61, e53–e61. [Google Scholar] [CrossRef] [PubMed]
- Shiba, K.; Kubzansky, L.D.; Williams, D.R.; VanderWeele, T.J.; Kim, E.S. Purpose in life and 8-year mortality by gender and race/ethnicity among older adults in the U.S. Prev. Med. 2022, 164, 107310. [Google Scholar] [CrossRef] [PubMed]
- Murray, C.J.; Atkinson, C.; Bhalla, K.; US Burden of Disease Collaborators. The state of US health, 1990–2010: Burden of diseases, injuries, and risk factors. JAMA 2013, 310, 591–608. [Google Scholar] [CrossRef]
- World Health Organization. Attaining the Nine Global Noncommunicable Diseases Targets: A Shared Responsibility; World Health Organization: Geneva, Switzerland, 2014. [Google Scholar]
- Holahan, C.K.; Holahan, C.J.; Suzuki, R. Purposiveness, physical activity, and perceived health in cardiac patients. Disabil. Rehabil. 2008, 30, 1772–1778. [Google Scholar] [CrossRef] [PubMed]
- Holahan, C.J.; Velasquez, K.E.; Jung, S.; North, R.J.; Pahl, S.A. Purposiveness and leisure-time physical activity in women in early midlife. Women Health 2011, 51, 661–675. [Google Scholar] [CrossRef] [PubMed]
- Hooker, S.A.; Masters, K.S. Purpose in life is associated with physical activity measured by accelerometer. J. Health Psychol. 2016, 21, 962–971. [Google Scholar] [CrossRef]
- Thege, B.K.; Urbán, R.; Kopp, M.S. Four-year prospective evaluation of the relationship between meaning in life and smoking status. Subst. Abuse Treat. Prev. Policy. 2013, 8, 8. [Google Scholar] [CrossRef]
- Morimoto, Y.; Yamasaki, S.; Ando, S.; Koike, S.; Fujikawa, S.; Kanata, S.; Endo, K.; Nakanishi, M.; Hatch, S.L.; Richards, M.; et al. Purpose in life and tobacco use among community-dwelling mothers of early adolescents. BMJ Open 2018, 8, e020586. [Google Scholar] [CrossRef]
- Lappan, S.; Thorne, C.B.; Long, D.; Hendricks, P.S. Longitudinal and reciprocal relationships between psychological well-being and smoking. Nicotine Tob. Res. 2020, 22, 18–23. [Google Scholar] [CrossRef]
- Kim, E.S.; Hershner, S.D.; Strecher, V.J. Purpose in life and incidence of sleep disturbances. J. Behav. Med. 2015, 38, 590–597. [Google Scholar] [CrossRef]
- Kim, E.S.; Strecher, V.J.; Ryff, C.D. Purpose in life and use of preventive health care services. Proc. Natl. Acad. Sci. USA 2014, 111, 16331–16336. [Google Scholar] [CrossRef] [PubMed]
- Hill, P.L.; Edmonds, G.W.; Hampson, S.E. A purposeful lifestyle is a healthful lifestyle: Linking sense of purpose to self-rated health through multiple health behaviors. J. Health Psychol. 2019, 24, 1392–1400. [Google Scholar] [CrossRef]
- Steptoe, A.; Fancourt, D. Leading a meaningful life at older ages and its relationship with social engagement, prosperity, health, biology, and time use. Proc. Natl. Acad. Sci. USA 2019, 116, 1207–1212. [Google Scholar] [CrossRef]
- Tapsell, L.C.; Neale, E.P.; Satija, A.; Hu, F.B. Foods, nutrients, and dietary patterns: Interconnections and implications for dietary guidelines. Adv. Nutr. 2016, 7, 445–454. [Google Scholar] [CrossRef]
- McAuley, E.A.; MacLaughlin, H.L.; Hannan-Jones, M.T.; King, N.; Ross, L.J. Effectiveness of diet quality indices in measuring a change in diet quality over time: A systematic review and meta-analysis of randomized controlled trials. Nutr. Rev. 2023, 81, 361–383. [Google Scholar] [CrossRef] [PubMed]
- Satia-About, J.; Patterson, R.E.; Neuhouser, M.L.; Eldet, J. Dietary acculturation: Applications to nutrition research and dietetics. J. Am. Diet. Assoc. 2002, 102, 1105–1118. [Google Scholar] [CrossRef] [PubMed]
- Markus, H.R.; Kitayama, S. Culture and the self: Implications for cognition, emotion, and motivation. Psychol. Rev. 1991, 98, 224–253. [Google Scholar] [CrossRef]
- MIDUS-Midlife in the United States, A National Longitudinal of Health and Well-Being. Timeline, Samples and Projects. Available online: https://midus.wisc.edu/index.php (accessed on 31 August 2023).
- Paccot, M. Enfoque de Riesgo para Prevención de Enfermedades Cardiovasculares (Consenso 2014); Ministerio de Salud de Chile: Santiago, Chile, 2015. [Google Scholar]
- Grundy, S.M.; Brewer, H.B., Jr.; Cleeman, J.I.; Smith, S.C., Jr.; Lenfant, C. Definition of metabolic syndrome: Report of the National Heart, Lung, and Blood Institute/American Heart Association conference on scientific issues related to definition. Circulation 2004, 109, 433–438. [Google Scholar] [CrossRef]
- Rigotti, A. Mediterranean Diet- and Psychological Well-Being Theory-Based Intervention to Reverse Metabolic Syndrome in Chile (CHILEMED). Clinicaltrials.gov; 2022. Available online: https://classic.clinicaltrials.gov/ct2/show/NCT05454904 (accessed on 31 August 2023).
- Díaz, D.; Rodríguez-Carvajal, R.; Blanco, A.; Moreno-Jiménez, B.; Gallardo, I.; Valle, C.; van Dierendonck, D. Spanish adaptation of the Psychological Well-Being Scales (PWBS). Psicothema 2006, 18, 572–577. [Google Scholar]
- Estruch, R.; Ros, E.; Salas-Salvadó, J.; Covas, M.I.; Corella, D.; Arós, F.; Gómez-Gracia, E.; Ruiz-Gutiérrez, V.; Fiol, M.; Lapetra, J.; et al. Primary Prevention of Cardiovascular Disease with a Mediterranean Diet Supplemented with Extra-Virgin Olive Oil or Nuts. N. Engl. J. Med. 2018, 378, e34. [Google Scholar] [CrossRef]
- Albert, J.M.; Nelson, S. Generalized causal mediation analysis. Biometrics 2011, 67, 1028–1038. [Google Scholar] [CrossRef] [PubMed]
- Boehm, J.K.; Kubzansky, L.D. The heart’s content: The association between positive psychological well-being and cardiovascular health. Psychol. Bull. 2012, 138, 655–691. [Google Scholar] [CrossRef]
- Kubzansky, L.D.; Huffman, J.C.; Boehm, J.K.; Hernandez, R.; Kim, E.S.; Koga, H.K.; Feig, E.H.; Lloyd-Jones, D.M.; Seligman, M.E.P.; Labarthe, D.R. Positive Psychological Well-Being and Cardiovascular Disease: JACC Health Promotion Series. J. Am. Coll. Cardiol. 2018, 72, 1382–1396. [Google Scholar] [CrossRef] [PubMed]
- Kodama, S.; Fujii, N.; Furuhata, T.; Sakurai, N.; Fujiwara, Y.; Hoshi, T. Dietary quality and its structural relationships among equivalent income, emotional well-being, and a five-year subjective health in Japanese middle-aged urban dwellers. Arch. Public Health 2015, 73, 30. [Google Scholar] [CrossRef] [PubMed]
- Kinoshita, S.; Hirooka, N.; Kusano, T.; Saito, K.; Nakamoto, H. Does Improvement in Health-Related Lifestyle Habits Increase Purpose in Life among a Health Literate Cohort? Int. J. Environ. Res. Public Health 2020, 17, 8878. [Google Scholar] [CrossRef] [PubMed]
- Pizzolato, J.E.; Brown, E.L.; Kanny, M.A. Purpose plus: Supporting youth purpose, control, and academic achievement. N. Dir. Youth Develop. 2011, 132. [Google Scholar] [CrossRef] [PubMed]
- Riches, B.R.; Benavides, C.M.; Dubon, V.X. Development of a fostering purpose intervention. Eval. Program. Plann. 2020, 83, 101857. [Google Scholar] [CrossRef] [PubMed]
- Czyżowska, N.; Gurba, E. Enhancing Meaning in Life and Psychological Well-Being Among a European Cohort of Young Adults via a Gratitude Intervention. Front. Psychol. 2022, 12, 751081. [Google Scholar] [CrossRef]
- Manco, N.; Hamby, S. A Meta-Analytic Review of Interventions That Promote Meaning in Life. Am. J. Health Promot. 2021, 35, 866–873. [Google Scholar] [CrossRef]
- Temple, N.J. The Origins of the Obesity Epidemic in the USA-Lessons for Today. Nutrients. 2022, 14, 4253. [Google Scholar] [CrossRef]
- Echeverría, G.; Dussaillant, C.; McGee, E.; Urquiaga, I.; Velasco, N.; Rigotti, A. Applying the Mediterranean diet for chronic disease prevention and treatment beyond the Mediterranean Basin. In The Mediterranean Region; Fuert-Bjelis, B., Ed.; InTechOpen: Rijeka, Croatia, 2017; pp. 401–414. [Google Scholar] [CrossRef]
- Echeverría, G.; Dussaillant, C.; McGee, E.E.; Mena, C.; Nitsche, M.P.; Urquiaga, I.; Bitran, M.; Pedrals, N.; Rigotti, A. The Mediterranean diet in the southern hemisphere: The Chilean experience. Eur. J. Clin. Nutr. 2019, 72 (Suppl. S1), 38–46. [Google Scholar] [CrossRef] [PubMed]
- Echeverría, G.; Tiboni, O.; Berkowitz, L.; Pinto, V.; Samith, B.; von Schultzendorff, A.; Pedrals, N.; Bitran, M.; Ruini, C.; Ryff, C.D.; et al. Mediterranean Lifestyle to Promote Physical, Mental, and Environmental Health: The Case of Chile. Int. J. Environ. Res. Public Health 2020, 17, 8482. [Google Scholar] [CrossRef]
- Albala, C.; Vio, F.; Kain, J.; Uauy, R. Nutrition transition in Chile: Determinants and consequences. Public Health Nutr. 2002, 5, 123–128. [Google Scholar] [CrossRef] [PubMed]
- Baumeister, R.F.; Vohs, K.D.; Aaker, J.L.; Garbinsky, E.N. Some key differences between a happy life and a meaningful life. J. Pos. Psychol. 2013, 8, 505–516. [Google Scholar] [CrossRef]
- Kris, K.; Vignoles, V.L.; de Almeida, I.; Uchida, I. Outside the “Cultural Binary”: Understanding why Latin American collectivist societies foster independent selves. Persp. Psychol. Sci. 2022, 17, 1166–1187. [Google Scholar] [CrossRef] [PubMed]
- Rosell, M.S.; Hellenius, M.L.; de Faire, U.H.; Johansson, G.K. Associations between diet and the metabolic syndrome vary with the validity of dietary intake data. Am. J. Clin. Nutr. 2003, 78, 84–90. [Google Scholar] [CrossRef] [PubMed]
| Study Samples | ||
|---|---|---|
| MIDUS (n = 2060) | CHILEMED (n = 223) | |
| Sex, % (n) | ||
| Men | 45.3 (934) | 41.7 (93) |
| Women | 54.7 (1126) | 58.3 (130) |
| Age, % (n) | ||
| <50 years | 33.6 (692) | 64.6 (144) |
| 50–65 years | 43.3 (891) | 31.8 (71) |
| >65 years | 23.1 (477) | 3.6 (8) |
| Race % (n) | ||
| White (Caucasians) | 74.9 (1543) | - |
| Non-White | 25.1 (517) | - |
| Hispanic | - | 100 (223) |
| Educational level, % (n) | ||
| High school or less | 23.7 (488) | 23.3 (52) |
| College education | 51.9 (1070) | 56.1 (125) |
| Postgraduate studies | 24.4 (502) | 20.6 (46) |
| Nutritional status, % (n) | ||
| Under or normal weight | 23.9 (491) | 4.5 (10) |
| Overweight | 33.1 (681) | 24.2 (54) |
| Obesity | 42.5 (876) | 71.3 (159) |
| Waist circumference, cm ± SD | 98.0 ± 17.9 | 104.9 ± 9.7 |
| Physical activity, % (n) | ||
| >450 METs/week | 60.8 (1252) | 35.0 (78) |
| ≤450 METs/week | 39.2 (808) | 65.0 (145) |
| MIDUS Sample | CHILEMED Sample | |||||||
|---|---|---|---|---|---|---|---|---|
| HEI (Mean Score) | p-Value | Purpose in Life (Mean Score) | p-Value | LFDI (Mean Score) | p-Value | Purpose in Life (Mean Score) | p-Value | |
| Sex | ||||||||
| Men | 5.79 | <0.001 | 38.74 | 0.004 | 6.50 | 0.45 | 29.3 | 0.48 |
| Women | 6.06 | 39.62 | 6.65 | 28.8 | ||||
| Age | ||||||||
| <50 years | 5.66 | <0.001 | 38.83 | <0.001 | 6.40 | 0.01 | 28.40 | 0.06 |
| 50–65 years | 5.96 | 39.34 | 6.85 | 30.06 | ||||
| >65 years | 6.32 | 39.58 | 7.63 | 31.38 | ||||
| Race | ||||||||
| White | 6.10 | <0.001 | 39.30 | 0.41 | ||||
| Non-White | 5.46 | 38.99 | ||||||
| Educational level | ||||||||
| Higher education or less | 5.40 | <0.001 | 37.79 | <0.001 | 6.39 | 0.36 | 30.08 | 0.02 |
| College education | 5.96 | 39.22 | 6.71 | 28.84 | ||||
| Postgraduate studies | 6.43 | 40.61 | 6.50 | 28.37 | ||||
| Nutritional Status | ||||||||
| Under or normal weight | 6.12 | <0.001 | 39.59 | 0.02 | 6.90 | 0.14 | 30.70 | 0.22 |
| Overweight | 5.98 | 39.65 | 6.88 | 29.91 | ||||
| Obesity | 5.81 | 38.69 | 6.47 | 28.63 | ||||
| Physical activity | ||||||||
| >450 METs/week | 6.13 | <0.001 | 39.93 | <0.001 | 6.61 | 0.87 | 28.29 | 0.14 |
| ≤450 METs/week | 5.63 | 38.12 | 6.58 | 29.43 | ||||
| Model 1 | Model 2 | Model 3 | ||||
|---|---|---|---|---|---|---|
| Coef | p-Value | Coef | p-Value | Coef | p-Value | |
| MIDUS HEI | ||||||
| PURPOSE IN LIFE | 0.153 | <0.001 | 0.137 | <0.001 | 0.108 | <0.001 |
| Sex | 0.211 | <0.001 | 0.237 | <0.001 | ||
| Age | 0.124 | <0.001 | 0.134 | <0.001 | ||
| Race | −0.38 | <0.001 | −0.305 | <0.001 | ||
| Education | 0.199 | <0.001 | ||||
| CHILEMED LFDI | ||||||
| PURPOSE IN LIFE | 0.208 | 0.002 | 0.151 | 0.022 | 0.163 | 0.014 |
| Sex | 0.096 | 0.458 | 0.161 | 0.224 | ||
| Age | 0.259 | <0.001 | 0.270 | <0.001 | ||
| Education | 0.365 | 0.024 | ||||
| Sample | Independent Variable | Dependent Variable | Coef | SE | p-Value |
|---|---|---|---|---|---|
| MIDUS | |||||
| Purpose in life † | Waist circumference | −0.075 | 0.021 | <0.001 | |
| HEI | Waist circumference | −0.078 | 0.022 | <0.001 | |
| Purpose in life | HEI | 0.108 | 0.021 | <0.001 | |
| CHILEMED | |||||
| Purpose in life † | Waist circumference | −0.104 | 0.065 | 0.107 | |
| LFDI | Waist circumference | −0.18 | 0.064 | 0.005 | |
| Purpose in life | LFDI | 0.191 | 0.064 | 0.003 |
| Sample | Pathway | Effect | Coef | SE | 95% CI |
|---|---|---|---|---|---|
| MIDUS | |||||
| Purpose → Waist | Direct | −0.075 | 0.022 | −0.12, −0.029 | |
| Purpose → HEI → Waist | Indirect | −0.008 | 0.003 | −0.015, −0.003 | |
| Purpose → → Waist | Total | −0.083 | 0.022 | −0.127, −0.037 | |
| CHILEMED | |||||
| Purpose → Waist | Direct | −0.104 | 0.061 | −0.215, 0.024 | |
| Purpose → LFDI → Waist | Indirect | −0.034 | 0.018 | −0.076, −0.005 | |
| Purpose → → Waist | Total | −0.139 | 0.06 | −0.247, −0.011 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Berkowitz, L.; Mateo, C.; Salazar, C.; Samith, B.; Sara, D.; Pinto, V.; Martínez, X.; Calzada, M.; von Schultzendorff, A.; Pedrals, N.; et al. Healthy Eating as Potential Mediator of Inverse Association between Purpose in Life and Waist Circumference: Emerging Evidence from US and Chilean Cohorts. Int. J. Environ. Res. Public Health 2023, 20, 7099. https://doi.org/10.3390/ijerph20237099
Berkowitz L, Mateo C, Salazar C, Samith B, Sara D, Pinto V, Martínez X, Calzada M, von Schultzendorff A, Pedrals N, et al. Healthy Eating as Potential Mediator of Inverse Association between Purpose in Life and Waist Circumference: Emerging Evidence from US and Chilean Cohorts. International Journal of Environmental Research and Public Health. 2023; 20(23):7099. https://doi.org/10.3390/ijerph20237099
Chicago/Turabian StyleBerkowitz, Loni, Camila Mateo, Cristian Salazar, Bárbara Samith, Daniela Sara, Victoria Pinto, Ximena Martínez, Mariana Calzada, Andrea von Schultzendorff, Nuria Pedrals, and et al. 2023. "Healthy Eating as Potential Mediator of Inverse Association between Purpose in Life and Waist Circumference: Emerging Evidence from US and Chilean Cohorts" International Journal of Environmental Research and Public Health 20, no. 23: 7099. https://doi.org/10.3390/ijerph20237099





