The Influence of a 9-Week Movement Program on the Body Composition of 7- to 8-Year-Old Schoolchildren in the Eastern Cape of South Africa
Abstract
1. Introduction
2. Materials and Methods
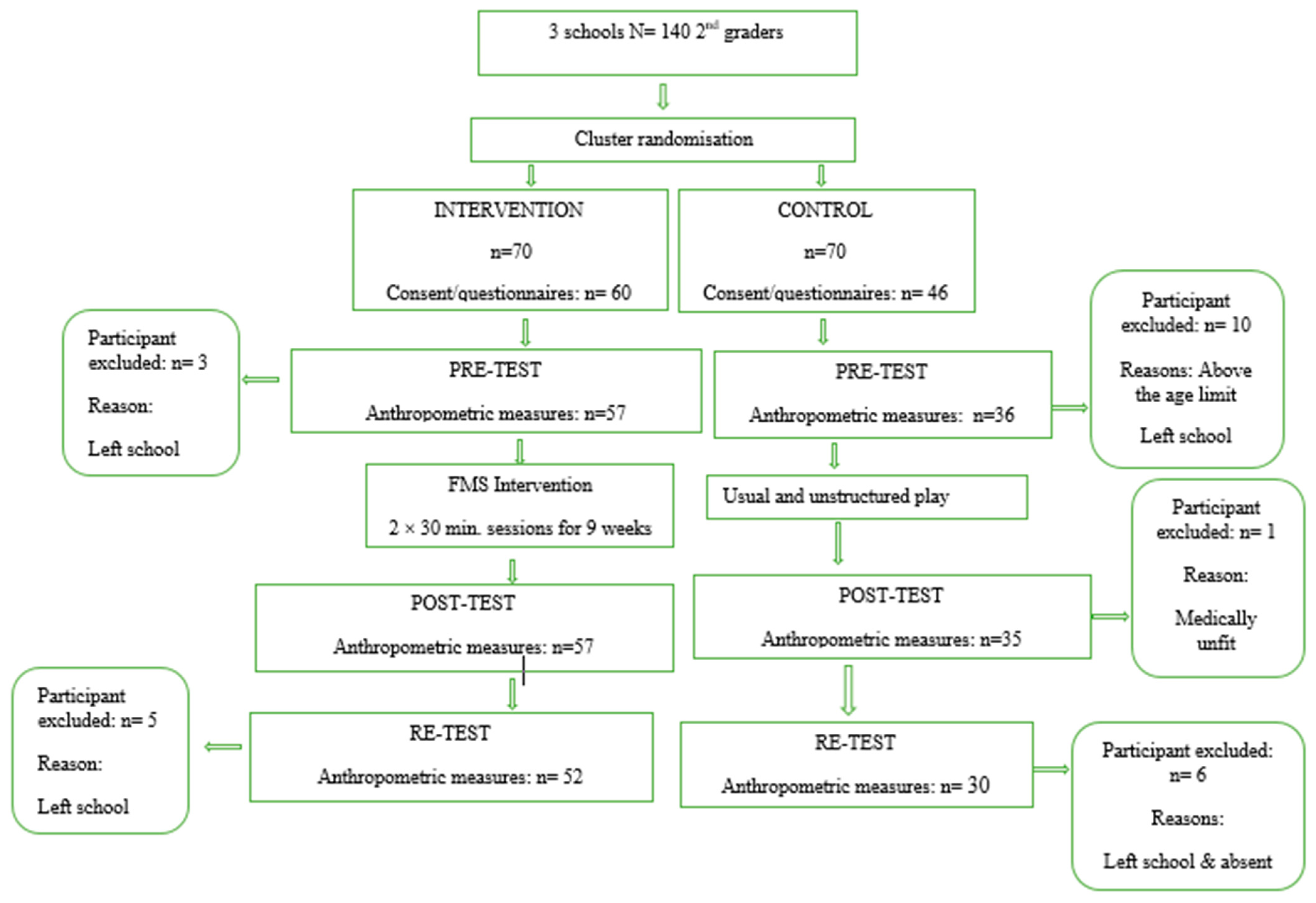
2.1. Research Design
2.2. Ethical Aspects/Considerations
2.3. Study Population
2.4. Intervention Procedure
2.5. Instrumentation
2.5.1. Anthropometry Measurements
2.5.2. Anthropometric Derived Variables
2.6. Statistical Analyses
3. Results
4. Discussion
Practical Implications
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Global Action Plan on Physical Activity 2018–2030: More Active People for a Healthier World; World Health Organization: Geneva, Switzerland, 2018. [Google Scholar]
- World Obesity Federation; World Obesity. Obesity: Missing the 2025 Global Targets. 2020. Available online: www.worldobesity.org (accessed on 3 February 2021).
- Güngőr, N.K. Overweight and obesity in children and adolescents. J. Clin. Res. Pediatr. Endocrinol. 2014, 6, 129–143. [Google Scholar] [CrossRef]
- Healthy Weight for Children (0–6 years) Framework; HSE National Childhood Programme and HSE Healthy Eating Active Living Programme: Dublin, Ireland, 2018; pp. 1–84.
- Fruh, S.M. Obesity: Risk factors, complications, and strategies for sustainable long-term weight management. J. Am. Assoc. Nurse Pract. 2017, 29, S3–S14. [Google Scholar] [CrossRef]
- El Kabbaoui, M.; Chda, A.; Bousfiha, A.; Aarab, L.; Bencheikh, R.; Tazi, A. Prevalence of and risk factors for overweight and obesity among adolescents in Morocco. East Mediterr. Health J. 2018, 24, 512–521. [Google Scholar] [CrossRef]
- Kambondo, G.; Sartorius, B. Risk factors for obesity and overfat among primary school children in Mashonaland West Province, Zimbabwe. Int. J. Environ. Res. Public Health 2018, 15, 249. [Google Scholar] [CrossRef]
- Rossouw, H.A.; Grant, C.C.; Viljoen, M. Overweight and obesity in children and adolescents: The South African problem. S. Afr. J. Sci. 2012, 108, 907. [Google Scholar] [CrossRef]
- Shisana, O.; Labadarios, D.; Rehle, T.; Simbayi, L.; Zuma, K.; Dhansay, A.; Reddy, P.; Parker, W.; Hoosain, E.; Naidoo, P.; et al. South African National Health and Nutrition Examination Survey (SANHANES-1); HSRC Press: Cape Town, South Africa, 2013; pp. 1–423. [Google Scholar]
- Sports Science Institute of South Africa. Healthy Active Kids South Africa Report Card. Discov. Vitality 2016, 1–24. [Google Scholar]
- Healthy Active Kids South Africa (HAKSA). Results from the Healthy Active Kids South Africa 2018 Report Card. S. Afr. J. Child Health 2019, 13, 130–136. [Google Scholar] [CrossRef]
- May, J.; Witten, C.; Lake, L. (Eds.) South African Child Gauge 2020; Children’s Institute, University of Cape Town: Cape Town, South Africa, 2020; pp. 1–200. [Google Scholar]
- Muthuri, S.K.; Francis, C.E.; Wachira, L.-Y.M.; LeBlanc, A.G.; Sampson, M.; Onywera, V.O.; Tremblay, M.S. Evidence of an overweight/obesity transition among school-aged children and youth in Sub-Saharan Africa: A systematic review. PLoS ONE 2014, 9, e92846. [Google Scholar] [CrossRef]
- Otitoola, O.; Oldewage-Theron, W.; Egal, A. Prevalence of overweight and obesity among selected schoolchildren and adolescents in Cofimvaba, South Africa. S. Afr. J. Clin. Nutr. 2020, 34, 97–102. [Google Scholar] [CrossRef]
- Negash, S.; Agyemang, C.; Matsha, T.E.; Peer, N.; Erasmus, R.T.; Kengne, A.P. Differential prevalence and associations of overweight and obesity by gender and population group among school learners in South Africa: A cross-sectional study. BMC Obes. 2017, 4, 29. [Google Scholar] [CrossRef]
- Pienaar, A.E. Prevalence of overweight and obesity among primary school children in a developing country: NW-CHILD longitudinal data of 6–9-yr-old children in South Africa. BMC Obes. 2015, 2, 2. [Google Scholar] [CrossRef] [PubMed]
- de Waal, E.; Pienaar, A.E. Influences of persistent overweight on perceptual-motor proficiency of primary school children: The North-West CHILD longitudinal study. BMC Pediatr. 2021, 21, 245. [Google Scholar] [CrossRef] [PubMed]
- Waters, E.; de Silva-Sanigorski, A.; Burford, B.J.; Brown, T.; Campbell, K.J.; Gao, Y.; Armstrong, R.; Prosser, L.; Summerbell, C.D. Interventions for preventing obesity in children. Cochrane Database Syst. Rev. 2011, 12, CD001871. [Google Scholar] [CrossRef] [PubMed]
- Walter, C.M. In school physical activity patterns of primary school learners from disadvantaged schools in South Africa. Afr. J Phys. Health Ed. Recreat. Dance 2011, 17, 780–789. [Google Scholar]
- Yuksel, H.S.; Sahin, F.N.; Maksimovic, N.; Drid, P.; Bianco, A. School-based intervention programs for preventing obesity and promoting physical activity and fitness: A systematic review. Int. J. Environ. Res. Public Health 2020, 17, 347. [Google Scholar] [CrossRef]
- Nqweniso, S.; du Randt, R.; Adams, L.; Degen, J.; Gall, S.; Gerber, M.; Joubert, N.; Müller, I.; Smith, D.; Seelig, H.; et al. Effects of school-based interventions on body composition of grade-4 children from lower socioeconomic communities in Gqeberha, South Africa. S. Afr. J. Child Health 2021, 15, 89–98. [Google Scholar] [CrossRef]
- Stodden, D.F.; Goodway, J.D.; Langendorfer, S.J.; Roberton, M.A.; Rudisill, M.E.; Garcia, C.; Garcia, L.E. A developmental perspective on the role of motor skill competence in physical activity: An emergent relationship. Quest 2008, 60, 290–306. [Google Scholar] [CrossRef]
- Castetbon, K.; Andreyeva, T. Obesity and motor skills among 4 to 6-year-old children in the United States: Nationally-representative surveys. BMC Pediatr. 2012, 12, 28. [Google Scholar] [CrossRef]
- Augustijn, M.J.C.M.; Deconinck, F.J.A.; D’Hondt, E.; Van Acker, L.; De Guchtenaere, A.; Lenoir, M.; Caeyenberghs, K. Reduced motor competence in children with obesity is associated with structural differences in the cerebellar peduncles. Brain Imaging Behav. 2018, 12, 1000–1010. [Google Scholar] [CrossRef]
- Greier, K.; Drenowatz, C. Bidirectional association between weight status and motor skills in adolescents. Wien. Kiln. Wochenschr. 2018, 130, 314–320. [Google Scholar] [CrossRef]
- Lopes, V.P.; Malina, R.M.; Maia, J.A.R.; Rodrigues, L.P. Body mass index and motor coordination: Non-linear relationship in children 6–10 years. Child Care Health Dev. 2018, 44, 443–451. [Google Scholar] [CrossRef] [PubMed]
- Jago, R.; Salway, R.; Emm-Collison, L.; Sebire, S.J.; Thompson, J.L.; Lawlor, D.A. Association of BMI category with change in children’s physical activity between ages 6 and 11 years: A longitudinal study. Int. J. Obes. 2021, 44, 104–113. [Google Scholar] [CrossRef] [PubMed]
- Burnett, C. National Research: State and Status of Physical Education in Public Schools of South Africa; South African Universities Physical Education Association (SAUPEA): Johannesburg, South Africa; United Nations Children’s Fund (UNICEF): Pretoria, South Africa; Department of Basic Education: Pretoria, South Africa, 2018; pp. 1–125. [Google Scholar]
- Matvienko, O.; Ahrabi-Fard, I. The effects of a 4-week after-school program on motor skills and fitness of kindergarten and first-grade students. Am. J. Health Promot. 2010, 24, 299–303. [Google Scholar] [CrossRef]
- Statsoft. Statistica for Windows. Release 5.5: General Conventions & Statistics; StatSoft: Tulsa, OK, USA, 2021. [Google Scholar]
- McKenzie, T.; Rosengard, P.; Williston, B.J. The SPARK Programs; SPARK: San Diego, CA, USA, 2006. [Google Scholar]
- Marfell-Jones, M.; Esparza-Ros, F.; Vaquero-Cristóbal, R. ISAK Accreditation Handbook; International Society for the Advancement of Kinanthropometry: Murcia, Spain, 2019. [Google Scholar]
- Cole, T.J.; Belizzi, M.C.; Flegal, K.M. Establishing a standard definition for child overweight and obesity worldwide: International survey. Br. Med. J. 2000, 320, 1240–1243. [Google Scholar] [CrossRef]
- Slaughter, M.H.; Lohman, T.G.; Boileau, R.A.; Horwill, C.A.; Stillman, R.J.; Van Loan, M.D.; Bemben, D.A. Skinfold equations for estimation of body fatness in children and youth. Hum. Biol. 1988, 60, 709–723. [Google Scholar] [PubMed]
- SPSS Inc. Statistical Package for Social Sciences Software; SPSS Inc.: Chicago, IL, USA, 2022. [Google Scholar]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences; Lawrence Erlbaum Associates: Hillsdale, NJ, USA, 1988. [Google Scholar]
- Steyn, N.P.; Labadarios, D.; Maunder, E.; Nel, J.; Lombard, C. Directors of the National Food Consumption Survey. Secondary anthropometric data analysis of the national food con-sumption survey in South Africa: The double burden. Nutrition 2005, 21, 4–13. [Google Scholar] [CrossRef]
- Monyeki, M.A.; Awotidebe, A.; Strydom, G.L.; Hans de Ridder, J.; Mamabolo, L.R.; Kemper, H.C.G. The challenges of underweight and overweight in South African children: Are we winning or losing the battle? A systematic review. Int. J. Environ. Res. Public Health 2015, 12, 1156–1173. [Google Scholar] [CrossRef]
- Nomatshila, S.C.; Mabunda, S.A.; Puoane, T.; Apalata, T.R. Prevalence of obesity and associated risk factors among children and adolescents in the Eastern Cape Province. Int. J. Environ. Res. Public Health 2022, 19, 2946. [Google Scholar] [CrossRef]
- Romieu, I.; Dossus, L.; Barquera, S.; Blottière, H.M.; Franks, P.W.; Gunter, M.; Hwalla, N.; Hursting, S.D.; Leitzmann, M.; Margetts, B.; et al. Energy balance and obesity: What are the main drivers? Cancer Causes Control 2017, 28, 247–258. [Google Scholar] [CrossRef]
- Wang, J.; Thornton, J.C.; Kolesnik, S.; Pierson, R.N. Anthropometry in body composition: An overview. Ann. N. Y. Acad. Sci. 2000, 904, 317–326. [Google Scholar] [CrossRef]
- Zask, A.; Adams, J.K.; Brooks, L.O.; Hughes, D.F. Tooty fruity vegie: An obesity prevention intervention evaluation in Australian preschools. Health Promot. J. Austr. 2012, 23, 10–15. [Google Scholar] [CrossRef] [PubMed]
- Salmon, J.; Ball, K.; Hume, C.; Booth, M.; Crawford, D. Outcomes of a group-randomized trial to prevent excess weight gain, reduce screen behaviours and promote physical activity in 10-year-old children: Switch-Play. Int. J. Obes. 2008, 32, 601–612. [Google Scholar] [CrossRef] [PubMed]
- Lubans, D.R.; Morgan, P.J.; Cliff, D.P.; Barnett, L.M.; Okely, A.D. Fundamental movement skills in children and adolescents: Review of associated health benefits. Sports Med. 2010, 40, 1019–1035. [Google Scholar] [CrossRef] [PubMed]
- Holfelder, B.; Schott, N. Relationship of fundamental movement skills and physical activity in children and adolescents: A systematic review. Psychol. Sport Exerc. 2014, 15, 382–391. [Google Scholar] [CrossRef]
- Robinson, L.E.; Stodden, D.F.; Barnett, L.M.; Lopes, V.P.; Logan, S.W.; Rodrigues, L.P.; D’Hondt, E. Motor competence and its effect on positive developmental trajectories of health. Sports Med. 2015, 45, 1273–1284. [Google Scholar] [CrossRef]
- Barnett, L.M.; Stodden, D.; Cohen, K.E.; Smith, J.J.; Lubans, D.R.; Lenoir, M.; Iivonen, S.; Miller, A.D.; Laukkanen, A.; Dudley, D.; et al. Fundamental movement skills: An important focus. J. Teach. Phys. Educ. 2016, 35, 219–225. [Google Scholar] [CrossRef]
- Bremer, E.; Cairney, J. Fundamental movement skills and health-related outcomes: A narrative review of longitudinal and intervention studies targeting typically developing children. Am. J. Lifestyle Med. 2016, 12, 148–159. [Google Scholar] [CrossRef]
- Greenway, F.L. Physiological adaptations to weight loss and factors favouring weight regain. Int. J. Obes. 2015, 39, 1188–1196. [Google Scholar] [CrossRef]
- Roberts, G.C.; Treasure, D.; Conroy, D.E. Understanding the Dynamics of Motivation in Sport and Physical Activity: An Achievement Goal Interpretation. In Handbook of Sport Psychology, 3rd ed.; Tenenbaum, G., Eklund, R., Eds.; Wiley: Hoboken, NJ, USA, 2007; pp. 3–30. [Google Scholar] [CrossRef]
- Sedumedi, C.M.; Janssen, X.; Reilly, J.J.; Kruger, H.S.; Monyeki, M.A. Association between objectively determined physical activity levels and body composition in 6–8-Year-Old children from a black South African population: BC–IT Study. Int. J. Environ. Res. Public Health 2021, 18, 6453. [Google Scholar] [CrossRef]
| Variables | Intervention Group | Control Group | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pre-Test | Post-Test | Re-Test | Pre-Test | Post-Test | Re-Test | |||||||
| Mean | Std Error | Mean | Std Error | Mean | Std Error | Mean | Std Error | Mean | Std Error | Mean | Std Error | |
| Body mass (kg) | 24.00 | 0.576 | 23.84 a–b,* | 0.576 | 25.63 | 0.578 | 23.66 | 0.725 | 24.07 | 0.726 | 25.37 | 0.730 |
| Stature (cm) | 121.81 | 0.741 | 123.41 | 0.741 | 125.43 | 0.742 | 122.08 | 0.933 | 123.45 | 0.934 | 125.48 | 0.935 |
| TSKF (mm) | 8.89 | 0.415 | 8.32 | 0.415 | 8.77 | 0.420 | 9.43 | 0.523 | 8.31 | 0.526 | 8.93 | 0.534 |
| SSKF (mm) | 5.59 | 0.366 | 5.65 | 0.366 | 5.27 b–c,* | 0.368 | 5.61 | 0.461 | 5.66 | 0.462 | 5.80 | 0.465 |
| Waist circumference | 53.34 | 0.635 | 53.07 a–b,* | 0.635 | 54.97 | 0.643 | 52.21 | 0.799 | 53.50 | 0.805 | 54.69 | 0.819 |
| Hip circumference | 63.07 | 0.712 | 64.85 | 0.712 | 66.32 | 0.717 | 61.60 | 0.895 | 66.16 | 0.899 | 66.64 | 0.908 |
| BMI | 16.17 | 0.266 | 15.57 a–b,* | 0.266 | 16.19 | 0.269 | 15.79 | 0.335 | 15.72 | 0.337 | 16.02 | 0.341 |
| Fat % | 12.82 | 0.696 | 12.49 | 0.696 | 11.04 | 0.696 | 13.58 | 0.876 | 12.15 | 0.886 | 10.36 | 0.871 |
| Sum of SKF | 14.48 | 0.796 | 13.98 | 0.796 | 12.78 | 0.796 | 15.04 | 1.002 | 13.53 | 1.011 | 11.84 | 0.998 |
| Intervention Group | Control Group | ||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Variable | Boys Mean | Girls Mean | Boys Mean | Girls Mean | Variance | p Values | |||||||||||||||
| T1 | T2 | T3 | T1 | T2 | T3 | T1 | T2 | T3 | T1 | T2 | T3 | EST | Part | Group | Time | Group * Time | Sex | Group * Sex | Time * Sex | Group * Time * Sex | |
| Body Mass | 23.7 | 23.5 | 25.2 | 24.4 | 24.1 | 26.1 | 24.4 | 24.9 | 26.1 | 23.0 | 23.3 | 24.7 | 1.0 | 17.8 | 0.892 | <0.01 | 0.141 | 0.687 | 0.222 | 0.712 | 0.943 |
| Stature | 121.7 | 123.1 | 125.2 | 121.9 | 123.7 | 125.7 | 121.4 | 122.5 | 124.6 | 122.8 | 124.4 | 126.4 | 0.6 | 30.6 | 0.919 | <0.01 | 0.567 | 0.371 | 0.585 | 0.139 | 0.927 |
| TSKF | 7.3 | 7.1 | 7.2 | 10.5 | 9.6 | 10.4 | 9.1 | 8.0 | 8.6 | 9.7 | 8.7 | 9.3 | 1.6 | 8.2 | 0.718 | <0.01 | 0.336 | 0.005 | 0.073 | 0.710 | 0.562 |
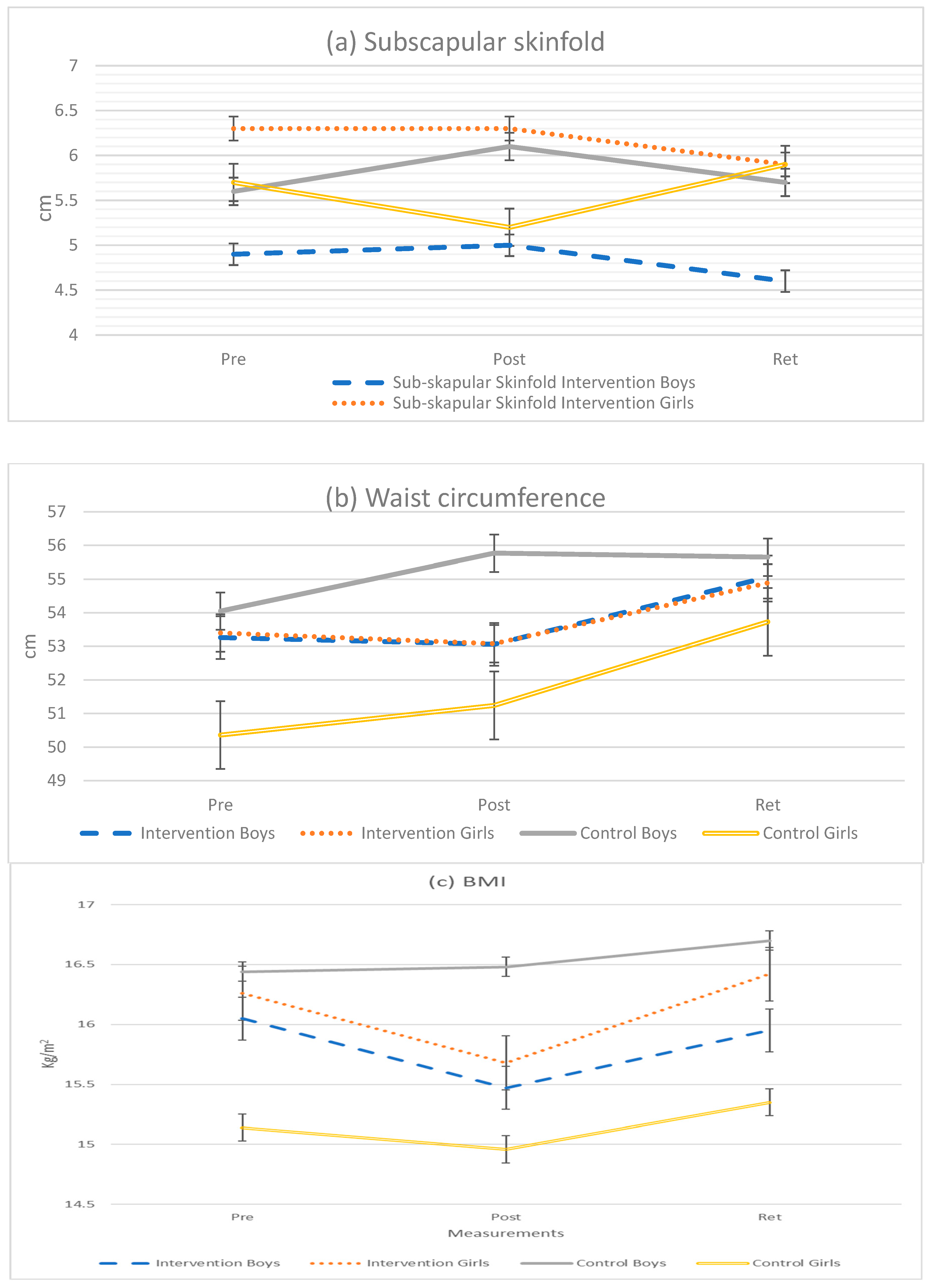
| SSKF | 4.9 | 5.0 | 4.6 | 6.3 | 6.3 | 5.9 | 5.6 | 6.1 | 5.7 | 5.7 | 5.2 | 5.9 | 0.5 | 7.1 | 0.748 | 0.587 | 0.051 | 0.341 | 0.201 | 0.026 | 0.045 |
| Waist Cir | 53.3 | 53.1 | 55.1 | 53.4 | 53.1 | 54.9 | 54.1 | 55.8 | 55.7 | 50.4 | 51.2 | 53.7 | 4.5 | 18.4 | 0.731 | <0.01 | 0.054 | 0.079 | 0.081 | 0.211 | 0.112 |
| Hip Cir. | 61.4 | 63.7 | 64.8 | 64.7 | 66.0 | 67.8 | 61.9 | 66.6 | 67.0 | 61.3 | 65.7 | 66.3 | 3.1 | 25.7 | 0.961 | <0.01 | <0.01 | 0.317 | 0.108 | 0.425 | 0.880 |
| BMI | 16.1 | 15.5 | 16.0 | 16.3 | 15.7 | 16.4 | 16.4 | 16.5 | 16.7 | 15.1 | 15.0 | 15.4 | 0.5 | 3.5 | 0.747 | <0.01 | 0.060 | 0.189 | 0.041 | 0.657 | 0.821 |
| Fat % | 10.3 | 10.2 | 8.4 | 15.3 | 14.8 | 13.6 | 12.5 | 12.1 | 9.0 | 14.7 | 12.2 | 11.7 | 15.4 | 12.2 | 0.921 | <0.01 | 0.445 | <0.01 | 0.076 | 0.376 | 0.696 |
| Sum of SKF | 12.2 | 12.1 | 10.5 | 16.7 | 15.9 | 15.1 | 14.7 | 14.2 | 11.1 | 15.4 | 12.9 | 12.6 | 15.1 | 21.0 | 0.802 | <0.01 | 0.421 | 0.038 | 0.069 | 0.280 | 0.699 |
| Intervention Group (Boys) | Intervention Group (Girls) | |||||||
|---|---|---|---|---|---|---|---|---|
| Variables/Time | Mean Diff (SD) | df | p-Value | d | Mean Diff (SD) | df | p-Value | d |
| Subscapular | ||||||||
| Pre-test—post-test | −0.09 ± 0.84 | 26 | 0.571 | 0.0 | −0.04 ± 0.92 | 29 | 0.828 | 0.0 |
| Post-test—re-test | 0.33 ± 0.77 | 23 | 0.046 | 0.2 | 0.38 ± 1.20 | 27 | 0.102 | 0.2 |
| Pre-test—re-test | 0.37 ± 0.74 | 23 | 0.023 | 0.1 | 0.31 ± 1.43 | 27 | 0.259 | 0.2 |
| Waist | ||||||||
| Pre-test—post-test | 0.22 ± 3.01 | 26 | 0.705 | 0.0 | 0.32 ± 2.64 | 29 | 0.516 | 0.1 |
| Post-test—re-test | −1.97 ± 2.11 | 23 | <0.01 | 0.4 | −1.81 ± 3.85 | 27 | 0.019 | 0.4 |
| Pre-test—re-test | −1.81 ± 3.14 | 23 | 0.010 | 0.4 | −1.53 ± 3.51 | 27 | 0.029 | 0.3 |
| BMI | ||||||||
| Pre-test—post-test | 0.58 ± 1.46 | 26 | 0.048 | 0.3 | 0.61 ± 0.81 | 29 | <0.01 | 0.3 |
| Post-test—re-test | −0.52 ± 0.60 | 23 | <0.01 | 0.3 | −0.73 ± 1.17 | 27 | 0.003 | 0.4 |
| Pre-test—re-test | 0.13 ± 1.81 | 23 | 0.723 | 0.1 | −0.15 ± 0.80 | 27 | 0.333 | 0.1 |
| Control group (Boys) | Control group (Girls) | |||||||
| Subscapular | ||||||||
| Pre-test—post-test | −0.54 ± 1.28 | 16 | 0.099 | 0.2 | 0.42 ± 0.94 | 17 | 0.076 | 0.2 |
| Post-test—re-test | 0.35 ± 1.24 | 13 | 0.312 | 0.2 | −0.69 ± 0.83 | 14 | 0.006 | 0.3 |
| Pre-test—re-test | −0.11 ± 0.91 | 13 | 0.666 | 0.0 | −0.26 ± 0.72 | 15 | 0.173 | 0.1 |
| Waist | ||||||||
| Pre-test—post-test | −1.60 ± 2.05 | 16 | 0.005 | 0.4 | −0.96 ± 3.00 | 17 | 0.194 | 0.2 |
| Post-test—re-test | −0.29 ± 2.77 | 13 | 0.699 | 0.0 | −2.52 ± 3.75 | 14 | 0.021 | 0.5 |
| Pre-test—re-test | −1.68 ± 2.13 | 13 | 0.011 | 0.3 | −3.33 ± 2.90 | 15 | <0.01 | 0.7 |
| BMI | ||||||||
| Pre-test—post-test | −0.04 ± 1.02 | 16 | 0.871 | 0.1 | 0.18 ± 0.41 | 17 | 0.083 | 0.1 |
| Post-test—re-test | −0.21 ± 0.40 | 13 | 0.067 | 0.1 | −0.38 ± 0.67 | 14 | 0.044 | 0.2 |
| Pre-test—re-test | −0.34 ± 1.05 | 13 | 0.243 | 0.2 | −0.20 ± 0.62 | 15 | 0.217 | 0.2 |
| BMI Classification | Total (93) Pre-Test | IG (57) | CG (36) | Total (92) Post-Test | IG (57) | CG (35) | Total (82) Re-Test | IG (52) | CG (30) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | N | % | N | % | N | % | N | % | N | % | N | % | |
| Underweight | 9 | 9.68 | 5 | 8.77 | 4 | 11.11 | 10 | 10.87 | 4 | 7.02 | 6 | 17.14 | 1 | 1.22 | 0 | 0 | 1 | 3.33 |
| Normal weight | 71 | 76.34 | 41 | 71.93 | 30 | 83.33 | 72 | 78.26 | 47 | 82.5 | 25 | 71.43 | 70 | 85.37 | 44 | 84.62 | 26 | 86.67 |
| Overweight | 9 | 9.68 | 8 | 14.04 | 1 | 2.78 | 8 | 8.70 | 5 | 8.77 | 3 | 8.57 | 10 | 12.19 | 7 | 13.46 | 3 | 10 |
| Obese | 4 | 4.30 | 3 | 5.26 | 1 | 2.78 | 2 | 2.17 | 1 | 1.75 | 1 | 2.86 | 1 | 1.22 | 1 | 1.92 | 0 | 0 |
| Overweight + obese | 13 | 13.98 | 11 | 19.30 | 2 | 5.56 | 10 | 10.87 | 6 | 10.52 | 4 | 11.43 | 11 | 13.41 | 8 | 15.38 | 3 | 10 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Idamokoro, M.; Pienaar, A.E.; Gerber, B.; van Gent, M.M. The Influence of a 9-Week Movement Program on the Body Composition of 7- to 8-Year-Old Schoolchildren in the Eastern Cape of South Africa. Int. J. Environ. Res. Public Health 2023, 20, 1762. https://doi.org/10.3390/ijerph20031762
Idamokoro M, Pienaar AE, Gerber B, van Gent MM. The Influence of a 9-Week Movement Program on the Body Composition of 7- to 8-Year-Old Schoolchildren in the Eastern Cape of South Africa. International Journal of Environmental Research and Public Health. 2023; 20(3):1762. https://doi.org/10.3390/ijerph20031762
Chicago/Turabian StyleIdamokoro, Mere, Anita E. Pienaar, Barry Gerber, and Maria M. van Gent. 2023. "The Influence of a 9-Week Movement Program on the Body Composition of 7- to 8-Year-Old Schoolchildren in the Eastern Cape of South Africa" International Journal of Environmental Research and Public Health 20, no. 3: 1762. https://doi.org/10.3390/ijerph20031762
APA StyleIdamokoro, M., Pienaar, A. E., Gerber, B., & van Gent, M. M. (2023). The Influence of a 9-Week Movement Program on the Body Composition of 7- to 8-Year-Old Schoolchildren in the Eastern Cape of South Africa. International Journal of Environmental Research and Public Health, 20(3), 1762. https://doi.org/10.3390/ijerph20031762






