Evaluation of the Impact of a Tourniquet Training Program: A Cross-Sectional Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Setting
2.3. Participants
2.4. Sociodemographic and Anthropometric Variables
2.5. Intervention-Related Variables
2.6. Bias
2.7. Study Size
2.8. Statistical Methods
2.9. Intervention
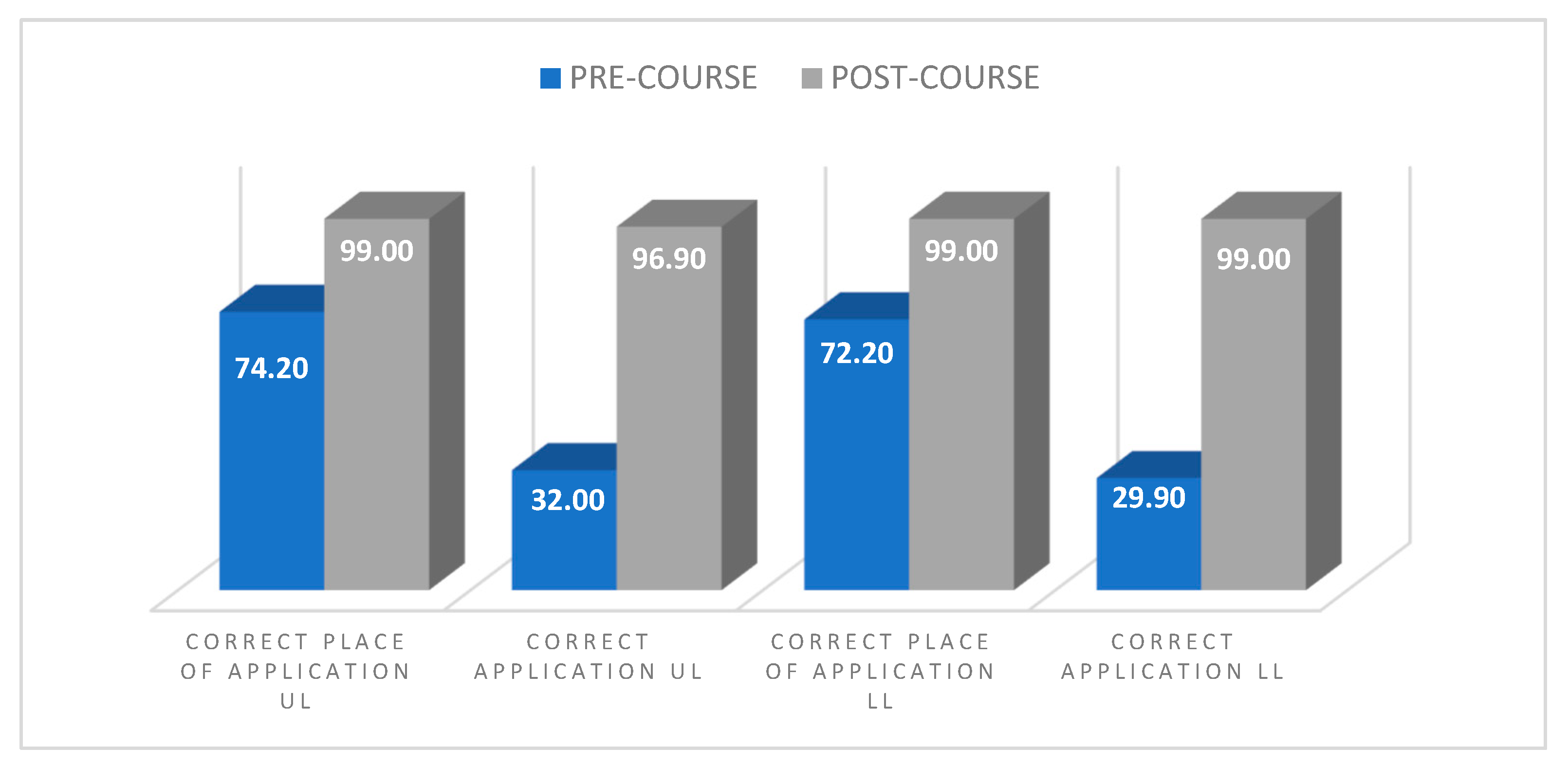
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Mabry, R.L.; Holcomb, J.B.; Baker, A.M.; Cloonan, C.C.; Uhorchak, J.M.; Perkins, D.E.; Canfield, A.J.; Hagmann, J.H. United States Army Rangers in Somalia: An Analysis of Combat Casualties on an Urban Battlefield. J. Trauma. 2000, 49, 515–529. [Google Scholar] [CrossRef] [PubMed]
- Montgomery, H.R.; Drew, B.G. Tactical Combat Casualty Care (TCCC) Update; Committee on Tactical Combat Casualty Care, Ed.; NAEMT: Clinton, MS, USA, 2020; ISBN 9780692906972. [Google Scholar]
- NAEMT PHTLS. Soporte Vital Básico y Avanzado En El Trauma Prehospitalario. Edición Militar, 6th ed.; Elsevier Mosby: Maryland Heights, MO, USA, 2011; Volume 7, ISBN 8480865709. [Google Scholar]
- Kelly, J.F.; Ritenour, A.E.; McLaughlin, D.F.; Bagg, K.A.; Apodaca, A.N.; Mallak, C.T.; Pearse, L.; Lawnick, M.M.; Champion, H.R.; Wade, C.E.; et al. Injury Severity and Causes of Death from Operation Iraqi Freedom and Operation Enduring Freedom: 2003-2004 versus 2006. J. Trauma. 2008, 64, S21–S27. [Google Scholar] [CrossRef] [PubMed]
- Gonzalez Alonso, V.; Orbaños Peiro, L.; Gómez Creso, J.; Hossain López, S.; Pérez Escobar, J.; Usero Pérez, C. Estudio Del Torniquete de Dotación Del Ejercito de Tierra. Sanidad. Militar. 2016, 72, 87–94. [Google Scholar]
- Puryear, B.; Roarty, J.; Knight, C. EMS Tactical Combat Casualty Care; StatPearls Publishing: Treasure Island, FL, USA, 2022. [Google Scholar]
- Kheirabadi, B. Evaluation of Topical Hemostatic Agents for Combat Wound Treatment. US Army Med. Dep. J. 2011, 37, 25–37. [Google Scholar]
- Roman, P.; Rodriguez-Alvarez, A.; Bertini-Perez, D.; Ropero-Padilla, C.; Martin-Ibañez, L.; Rodriguez-Arrastia, M. Tourniquets as a Haemorrhage Control Measure in Military and Civilian Care Settings: An Integrative Review. J. Clin. Nurs. 2021. [Google Scholar] [CrossRef]
- Champion, H.R.; Bellamy, R.F.; Roberts, C.P.; Leppaniemi, A. A Profile of Combat Injury. J. Trauma. 2003, 54, S13–S19. [Google Scholar] [CrossRef]
- Sebesta, J. Special Lessons Learned from Iraq. Surg. Clin. North Am. 2006, 86, 711–726. [Google Scholar] [CrossRef]
- Janak, J.; Stockinger, Z.; Mazuchowski, E.; Kotwal, R.; Sosnov, J.; Montgomery, H.; Butler, F.; Shackelford, S.; Gurney, J.; Spott, M.; et al. Military Preventable Death Conceptual Framework: A Systematic Approach for Reducing Battlefield Mortality. Mil. Med. 2018, 183, 15–23. [Google Scholar] [CrossRef]
- Cannon, J.W.; Holena, D.N.; Geng, Z.; Stewart, I.J.; Huang, Y.; Yang, W.; Mayhew, E.R.; Nessen, S.C.; Gross, K.R.; Schwab, C.W. Comprehensive Analysis of Combat Casualty Outcomes in US Service Members from the Beginning of World War II to the End of Operation Enduring Freedom. J. Trauma. Acute Care Surg. 2020, 89, S8–S15. [Google Scholar] [CrossRef]
- Tsur, A.M.; Nadler, R.; Benov, A.; Glassberg, E.; Siman-Tov, M.; Radomislensky, I.; Bodas, M.; Peleg, K.; Thompson, P.; Fink, N.; et al. The Effects of Military-Wide Introduction of Advanced Tourniquets in the Israel Defense Forces. Injury 2020, 51, 1210–1215. [Google Scholar] [CrossRef]
- Mazuchowski, E.L.; Kotwal, R.S.; Janak, J.C.; Howard, J.T.; Harcke, H.T.; Montgomery, H.R.; Butler, F.K.; Holcomb, J.B.; Eastridge, B.J.; Gurney, J.M.; et al. Mortality Review of US Special Operations Command Battle-Injured Fatalities. J. Trauma. Acute Care Surg. 2020, 88, 686–695. [Google Scholar] [CrossRef] [PubMed]
- Lv, M.; Jia, Y.; Zong, Z.; Jiang, R.; Du, W.; Zhang, L.; Ye, Z.; Zhong, X. Method for Teaching Life-Saving Combat First-Aid Skills With Live-Actor Patients Using a Wearable Training Apparatus. Mil. Med. 2022, 187, 757–763. [Google Scholar] [CrossRef] [PubMed]
- Tsur, A.M.; Binyamin, Y.; Koren, L.; Ohayon, S.; Thompson, P.; Glassberg, E. High Tourniquet Failure Rates Among Non-Medical Personnel Do Not Improve with Tourniquet Training, Including Combat Stress Inoculation: A Randomized Controlled Trial. Prehosp. Disaster Med. 2019, 34, 282–287. [Google Scholar] [CrossRef] [PubMed]
- Nichols, R.; Horstman, J. Recommendations for Improving Stop the Bleed: A Systematic Review. Mil. Med. 2022, 187, e1338–e1345. [Google Scholar] [CrossRef]
- Ross, E.M.; Redman, T.T.; Mapp, J.G.; Brown, D.J.; Tanaka, K.; Cooley, C.W.; Kharod, C.U.; Wampler, D.A. Stop the Bleed: The Effect of Hemorrhage Control Education on Laypersons’ Willingness to Respond During a Traumatic Medical Emergency. Prehosp. Disaster Med. 2018, 33, 127–132. [Google Scholar] [CrossRef] [PubMed]
- Valsecchi, D.; Sassi, G.; Tiraboschi, L.; Bonetti, M.; Lagazzi, E.; Michelon, A.M.; Nicolussi, T.; Stevan, A.; Bonasera-Vincenti, N.M.; Guelfi-Pulvano, R.; et al. The Rise of the Stop the Bleed Campaign in Italy. J. Spec. Oper. Med. 2019, 19, 95–99. [Google Scholar] [CrossRef] [PubMed]
- Ramirez, M.L.; Slovis, C.M. Resident Involvement in Civilian Tactical Emergency Medicine. J. Emerg. Med. 2010, 39, 49–56. [Google Scholar] [CrossRef] [PubMed]
- Tactical Combat Casualty Care. Available online: https://www.naemt.org/education/naemt-tccc (accessed on 15 January 2023).
- Jacobs, L.; Keating, J.J.; Hunt, R.C.; Butler, F.K.; Pons, P.T.; Gestring, M.; Bulger, E.; Eastman, A.; Kerby, J.; Hashmi, Z.; et al. Stop the BleedⓇ. Curr. Probl. Surg. 2022, 59, 101193. [Google Scholar] [CrossRef]
- Ministerio de Defensa. Gobierno de España Orden DEF/1153/2020. BOE No 317 2022, 13249, 109332–109337. [Google Scholar]
- Butler, F.K. Two Decades of Saving Lives on the Battlefield: Tactical Combat Casualty Care Turns 20. Mil. Med. 2017, 182, e1563–e1568. [Google Scholar] [CrossRef]
- Ministerio de la Presidencia. G. de E. Real Decreto 944/2001, de 3 de Agosto, Por El Que Se Aprueba El Reglamento Para La Determinación de La Aptitud Psicofísica Del Personal de Las Fuerzas Armadas; Ministerio de la Presidencia: Marid, Spain, 2001; Volume 186, p. 37. [Google Scholar]
- Cuentas, M.; Domínguez, J.L.; Mendoza, M.C.; Montoya, J.G.; Mori, N.; Perez, D.S.; Larrabure, G.; Córdova, D. Estado Nutricional de La Gestante Según Los Índices de Quetelet, Quetelet Modificado y Monograma de Rosso. CIMEL Cienc. E Investig. Médica Estud. Latinoam. 2002, 7, 30–34. [Google Scholar]
- Obesity and Overweight. Available online: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 27 January 2023).
- Usero-Pérez, M.D.C.; Jiménez-Rodríguez, M.L.; González-Aguña, A.; González-Alonso, V.; Orbañanos-Peiro, L.; Santamaría-García, J.M.; Gómez-González, J.L. Validation of an Evaluation Instrument for Responders in Tactical Casualty Care Simulations. Rev. Lat. Am. Enferm. 2020, 28, e3251. [Google Scholar] [CrossRef]
- Crichton, N. Visual Analog Scale (VAS). J. Clin. Nurs. 2001, 10, 697–706. [Google Scholar]
- Chambers, J.A.; Seastedt, K.; Krell, R.; Caterson, E.; Levy, M.; Turner, N. “Stop the Bleed”: A U.S. Military Installation’s Model for Implementation of a Rapid Hemorrhage Control Program. Mil. Med. 2019, 184, 67–71. [Google Scholar] [CrossRef] [PubMed]
- STOP THE BLEED—Save a Life|Stop The Bleed. Available online: https://www.stopthebleed.org/ (accessed on 15 January 2023).
- Zwislewski, A.; Nanassy, A.D.; Meyer, L.K.; Scantling, D.; Jankowski, M.A.; Blinstrub, G.; Grewal, H. Practice Makes Perfect: The Impact of Stop the Bleed Training on Hemorrhage Control Knowledge, Wound Packing, and Tourniquet Application in the Workplace. Injury 2019, 50, 864–868. [Google Scholar] [CrossRef]
- Planchon, J.; Vacher, A.; Comblet, J.; Rabatel, E.; Darses, F.; Mignon, A.; Pasquier, P. Serious Game Training Improves Performance in Combat Life-Saving Interventions. Injury 2018, 49, 86–92. [Google Scholar] [CrossRef]
- Schreckengaust, R.; Littlejohn, L.; Zarow, G.J. Effects of Training and Simulated Combat Stress on Leg Tourniquet Application Accuracy, Time, and Effectiveness. Mil. Med. 2014, 179, 114–120. [Google Scholar] [CrossRef]
- Heldenberg, E.; Aharony, S.; Wolf, T.; Vishne, T. Evaluating New Types of Tourniquets by the Israeli Naval Special Warfare Unit. Disaster Mil. Med. 2015, 1, 1. [Google Scholar] [CrossRef]
- Scott, S.M.; Carman, M.J.; Zychowicz, M.E.; Shapiro, M.L.; True, N.A. Implementation and Evaluation of Tactical Combat Casualty Care for Army Aviators. Mil. Med. 2020, 185, E1271–E1276. [Google Scholar] [CrossRef]
- Gurney, J.M.; Stern, C.A.; Kotwal, R.S.; Cunningham, C.W.; Burelison, D.R.; Gross, K.R.; Montgomery, H.R.; Whitt, E.H.; Murray, C.K.; Stockinger, Z.T.; et al. Tactical Combat Casualty Care Training, Knowledge, and Utilization in the US Army. Mil. Med. 2020, 185, 500–507. [Google Scholar] [CrossRef] [Green Version]
| Variable | Mean | DT | Max | Min |
|---|---|---|---|---|
| Time of application UL pre-course (seconds) | 76.68 | 31.25 | 196.00 | 26.97 |
| Time of application UL post-course (seconds) | 58.06 | 18.46 | 138.00 | 26.99 |
| VAS UL pre-course (score) | 4.48 | 2.15 | 9 | 0 |
| VAS UL post-course (score) | 5.31 | 2.13 | 9 | 0 |
| Time of application LL pre-course (seconds) | 43.33 | 13.12 | 84.18 | 15.91 |
| Time of application LL post-course (seconds) | 47.30 | 12.86 | 98.00 | 22.00 |
| VAS LL pre-course (score) | 5.68 | 2.45 | 9 | 0 |
| VAS LL post-course (score) | 6.24 | 2.01 | 9 | 0 |
| Puntuation pre-course (score) | 6.21 | 1.92 | 9.50 | 1 |
| Puntuation post-course (score) | 8.95 | 1.43 | 10 | 2 |
| Variable (Chi-Square) | Sex (p-Value) | Employment (p-Value) | BMI (p-Value) |
|---|---|---|---|
| Correct place of application UL pretest | 0.159 | 0.189 | 0.215 |
| Correct application of UL pretest | 0.606 | 0.260 | 0.563 |
| Pretest UL Doppler reading | 0.128 | 0.356 | 0.686 |
| Correct application UL pretest | 0.417 | 0.656 | 0.605 |
| Pretest UL Doppler reading | 0.460 | 0.330 | 0.374 |
| Doppler reading UL post-test | 0.159 | 0.226 | 0.416 |
| Correct place LL post-test | 0.938 | 0.990 | 0.669 |
| Correct application LL post-test | 0.938 | 0.079 | 0.516 |
| Doppler reading LL post-test | 0.025 | 0.007 | 0.705 |
| Correct place LL pretest | 0.463 | 0.596 | 0.497 |
| Correct place UL post-test | 0.938 | 0.990 | 0.669 |
| Correct application UL post-test | 0.824 | 0.742 | 0.705 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
González-Alonso, V.; Usero-Pérez, M.d.C.; Seguido Chacón, R.; Gómez de la Fuente, A.; Cortés-Martín, J.; Rodríguez-Blanque, R.; Sánchez-García, J.C. Evaluation of the Impact of a Tourniquet Training Program: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2023, 20, 2742. https://doi.org/10.3390/ijerph20032742
González-Alonso V, Usero-Pérez MdC, Seguido Chacón R, Gómez de la Fuente A, Cortés-Martín J, Rodríguez-Blanque R, Sánchez-García JC. Evaluation of the Impact of a Tourniquet Training Program: A Cross-Sectional Study. International Journal of Environmental Research and Public Health. 2023; 20(3):2742. https://doi.org/10.3390/ijerph20032742
Chicago/Turabian StyleGonzález-Alonso, Valentín, María del Carmen Usero-Pérez, Raquel Seguido Chacón, Alicia Gómez de la Fuente, Jonathan Cortés-Martín, Raquel Rodríguez-Blanque, and Juan Carlos Sánchez-García. 2023. "Evaluation of the Impact of a Tourniquet Training Program: A Cross-Sectional Study" International Journal of Environmental Research and Public Health 20, no. 3: 2742. https://doi.org/10.3390/ijerph20032742
APA StyleGonzález-Alonso, V., Usero-Pérez, M. d. C., Seguido Chacón, R., Gómez de la Fuente, A., Cortés-Martín, J., Rodríguez-Blanque, R., & Sánchez-García, J. C. (2023). Evaluation of the Impact of a Tourniquet Training Program: A Cross-Sectional Study. International Journal of Environmental Research and Public Health, 20(3), 2742. https://doi.org/10.3390/ijerph20032742








