The Impact of Childhood Trauma on Problematic Alcohol and Drug Use Trajectories and the Moderating Role of Social Support
Abstract
1. Introduction
Study Aims
2. Materials and Methods
2.1. Participants and Procedures
2.2. Measures—Dependent Variables
2.3. Measures—Independent Variables
2.4. Measures—Moderator
2.5. Measures—Covariates
2.6. Statistical Analysis
3. Results
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- US Department of Health Human Services the Health Consequences of Smoking—50 Years of Progress: A Report of the Surgeon General. Available online: https://www.cdc.gov/tobacco/data_statistics/sgr/50th-anniversary/index.htm (accessed on 15 November 2022).
- Centers for Disease Control and Prevention Excessive Drinking is Draining the U.S. Economy. Available online: https://www.cdc.gov/alcohol/features/excessive-drinking.html?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Ffeatures%2Fcostsofdrinking%2Findex.html (accessed on 28 August 2021).
- National Institute on Drug Abuse Costs of Substance Abuse. Available online: https://archives.drugabuse.gov/trends-statistics/costs-substance-abuse (accessed on 28 August 2021).
- Hser, Y.; Longshore, D.; Anglin, M.D. The life course perspective on drug use. Eval. Rev. 2007, 31, 515–547. [Google Scholar] [CrossRef] [PubMed]
- Sussman, S.; Ames, S.L. Drug Abuse: Concepts, Prevention, and Cessation; Cambridge University Press: Cambridge, UK, 2008. [Google Scholar]
- Grigsby, T.J.; Forster, M.; Unger, J.B.; Sussman, S. Predictors of alcohol-related negative consequences in adolescents: A systematic review of the literature and implications for future research. J. Adolesc. 2016, 48, 18–35. [Google Scholar] [CrossRef] [PubMed]
- Pedersen, E.R.; Hummer, J.F.; Rinker, D.V.; Traylor, Z.K.; Neighbors, C. Measuring protective behavioral strategies for marijuana use among young adults. J. Stud. Alcohol Drugs 2016, 77, 441–450. [Google Scholar] [CrossRef] [PubMed]
- Palmer, R.S.; McMahon, T.J.; Moreggi, D.I.; Rounsaville, B.J.; Ball, S.A. College student drug use: Patterns, concerns, consequences, and interest in intervention. J. Coll. Stud. Dev. 2012, 53, 3856915. [Google Scholar] [CrossRef]
- Blanchard, K.A.; Morgenstern, J.; Morgan, T.J.; Lobouvie, E.W.; Bux, D.A. Assessing consequences of substance use: Psychometric properties of the inventory of drug use consequences. Psychol. Addict. Behav. 2003, 17, 328. [Google Scholar] [CrossRef]
- White, H.R.; Labouvie, E.W. Towards the assessment of adolescent problem drinking. J. Stud. Alcohol 1989, 50, 30–37. [Google Scholar] [CrossRef]
- Sussman, S.; Lisha, N.; Griffiths, M. Prevalence of the addictions: A problem of the majority or the minority? Eval. Health Prof. 2011, 34, 3–56. [Google Scholar] [CrossRef]
- Sussman, S.; Arpawong, T.E.; Sun, P.; Tsai, J.; Rohrbach, L.A.; Spruijt-Metz, D. Prevalence and co-occurrence of addictive behaviors among former alternative high school youth. J. Behav. Addict. 2014, 3, 33–40. [Google Scholar] [CrossRef] [PubMed]
- Felitti, V.J.; Anda, R.F.; Nordenberg, D.; Williamson, D.F.; Spitz, A.M.; Edwards, V.; Koss, M.P.; Marks, J.S. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: The Adverse Childhood Experiences (ACE) Study. Am. J. Prev. Med. 1998, 14, 245–258. [Google Scholar] [CrossRef] [PubMed]
- Hughes, K.; Bellis, M.A.; Hardcastle, K.A.; Sethi, D.; Butchart, A.; Mikton, C.; Jones, L.; Dunne, M.P. The effect of multiple adverse childhood experiences on health: A systematic review and meta-analysis. Lancet Public Health 2017, 2, e356–e366. [Google Scholar] [CrossRef] [PubMed]
- Forster, M.; Rogers, C.; Sussman, S.Y.; Yu, S.; Rahman, T.; Zeledon, H.; Benjamin, S.M. Adverse childhood experiences and problematic smartphone use among college students: Findings from a pilot study. Addict. Behav. 2021, 117, 106869. [Google Scholar] [CrossRef]
- Forster, M.; Rogers, C.J.; Sussman, S.; Watts, J.; Rahman, T.; Yu, S.; Benjamin, S.M. Can Adverse Childhood Experiences Heighten Risk for Problematic Internet and Smartphone Use? Findings from a College Sample. Int. J. Environ. Res. Public Health 2021, 18, 5978. [Google Scholar] [CrossRef]
- Sharma, A.; Sacco, P. Adverse childhood experiences and gambling: Results from a national survey. J. Soc. Work Pract. Addict. 2015, 15, 25–43. [Google Scholar] [CrossRef]
- Ng, B.D.; Wiemer-Hastings, P. Addiction to the internet and online gaming. Cyberpsychology Behav. 2005, 8, 110–113. [Google Scholar] [CrossRef]
- Danese, A.; McEwen, B.S. Adverse childhood experiences, allostasis, allostatic load, and age-related disease. Physiol. Behav. 2012, 106, 29–39. [Google Scholar] [CrossRef] [PubMed]
- Pechtel, P.; Pizzagalli, D.A. Effects of early life stress on cognitive and affective function: An integrated review of human literature. Psychopharmacology 2011, 214, 55–70. [Google Scholar] [CrossRef] [PubMed]
- Albott, C.S.; Forbes, M.K.; Anker, J.J. Association of childhood adversity with differential susceptibility of transdiagnostic psychopathology to environmental stress in adulthood. JAMA Netw. Open 2018, 1, e185354. [Google Scholar] [CrossRef]
- Felitti, V.J.; Anda, R.F. The relationship of adverse childhood experiences to adult medical disease, psychiatric disorders, and sexual behavior: Implications for healthcare. In The Impact of Early Life Trauma on Health and Disease: The Hidden Epidemic; Cambridge University Press: Cambridge, UK, 2010; pp. 77–87. [Google Scholar]
- Forster, M.; Gower, A.L.; Borowsky, I.W.; McMorris, B.J. Associations between adverse childhood experiences, student-teacher relationships, and non-medical use of prescription medications among adolescents. Addict. Behav. 2017, 68, 30–34. [Google Scholar] [CrossRef]
- Gilbert, P. Introducing compassion-focused therapy. Adv. Psychiatr. Treat. 2009, 15, 199–208. [Google Scholar] [CrossRef]
- Pollak, S.D.; Cicchetti, D.; Hornung, K.; Reed, A. Recognizing emotion in faces: Developmental effects of child abuse and neglect. Dev. Psychol. 2000, 36, 679. [Google Scholar] [CrossRef]
- Grant, J.E.; Chamberlain, S.R. Expanding the definition of addiction: DSM-5 vs. ICD-11. CNS Spectr. 2016, 21, 300–303. [Google Scholar] [CrossRef] [PubMed]
- Espeleta, H.C.; Brett, E.I.; Ridings, L.E.; Leavens, E.L.; Mullins, L.L. Childhood adversity and adult health-risk behaviors: Examining the roles of emotion dysregulation and urgency. Child Abus. Negl. 2018, 82, 92–101. [Google Scholar] [CrossRef]
- Goldstein, A.L.; Flett, G.L.; Wekerle, C. Child maltreatment, alcohol use and drinking consequences among male and female college students: An examination of drinking motives as mediators. Addict. Behav. 2010, 35, 636–639. [Google Scholar] [CrossRef] [PubMed]
- Rogers, C.J.; Pakdaman, S.; Forster, M.; Sussman, S.; Grigsby, T.J.; Victoria, J.; Unger, J.B. Effects of multiple adverse childhood experiences on substance use in young adults: A review of the literature. Drug Alcohol Depend. 2022, 234, 109407. [Google Scholar] [CrossRef] [PubMed]
- Shin, S.H.; McDonald, S.E.; Conley, D. Patterns of adverse childhood experiences and substance use among young adults: A latent class analysis. Addict. Behav. 2018, 78, 187–192. [Google Scholar] [CrossRef]
- Vilhena-Churchill, N.; Goldstein, A.L. Child maltreatment and marijuana problems in young adults: Examining the role of motives and emotion dysregulation. Child Abus. Negl. 2014, 38, 962–972. [Google Scholar] [CrossRef]
- Rogers, C.J.; Forster, M.; Grigsby, T.J.; Albers, L.; Morales, C.; Unger, J.B. The impact of childhood trauma on substance use trajectories from adolescence to adulthood: Findings from a longitudinal Hispanic cohort study. Child Abus. Negl. 2021, 120, 105200. [Google Scholar] [CrossRef] [PubMed]
- Forster, M.; Rogers, C.; Tinoco, S.; Benjamin, S.; Lust, K.; Grigsby, T. Adverse childhood experiences and alcohol related negative consequence among college student drinkers. Addict. Behav. 2023, 136, 107484. [Google Scholar] [CrossRef] [PubMed]
- Enoch, M.-A. The role of early life stress as a predictor for alcohol and drug dependence. Psychopharmacology 2011, 214, 17–31. [Google Scholar] [CrossRef]
- Cohen, S. Social relationships and health. Am. Psychol. 2004, 59, 676. [Google Scholar] [CrossRef]
- Hendrick, C.E.; Hendrick, S.S. Close Relationships: A Sourcebook; Sage Publications, Inc.: Thousand Oaks, CA, USA, 2000. [Google Scholar]
- Harandi, T.F.; Taghinasab, M.M.; Nayeri, T.D. The correlation of social support with mental health: A meta-analysis. Electron. Physician 2017, 9, 5212. [Google Scholar] [CrossRef] [PubMed]
- Taylor, S.E. Social support. In Foundations of Health Psychology; Oxford University Press: Oxford, UK, 2007; pp. 145–171. [Google Scholar]
- Sippel, L.M.; Pietrzak, R.H.; Charney, D.S.; Mayes, L.C.; Southwick, S.M. How does social support enhance resilience in the trauma-exposed individual? Ecol. Soc. 2015, 20, 10. [Google Scholar] [CrossRef]
- Wang, J.; Mann, F.; Lloyd-Evans, B.; Ma, R.; Johnson, S. Associations between loneliness and perceived social support and outcomes of mental health problems: A systematic review. BMC Psychiatry 2018, 18, 156. [Google Scholar] [CrossRef] [PubMed]
- Galaif, E.R.; Sussman, S.; Chou, C.-P.; Wills, T.A. Longitudinal relations among depression, stress, and coping in high risk youth. J. Youth Adolesc. 2003, 32, 243–258. [Google Scholar] [CrossRef]
- Ozbay, F.; Fitterling, H.; Charney, D.; Southwick, S. Social support and resilience to stress across the life span: A neurobiologic framework. Curr. Psychiatry Rep. 2008, 10, 304. [Google Scholar] [CrossRef] [PubMed]
- Forster, M.; Grigsby, T.J.; Gower, A.L.; Mehus, C.J.; McMorris, B.J. The role of social support in the association between childhood adversity and adolescent self-injury and suicide: Findings from a statewide sample of high school students. J. Youth Adolesc. 2020, 49, 1195–1208. [Google Scholar] [CrossRef]
- Taylor, S.E. Social support: A review. In The Oxford Handbook of Health Psychology; Oxford University Press: Oxford, UK, 2011; pp. 189–214. [Google Scholar]
- Wang, Y.; Chung, M.C.; Wang, N.; Yu, X.; Kenardy, J. Social support and posttraumatic stress disorder: A meta-analysis of longitudinal studies. Clin. Psychol. Rev. 2021, 85, 101998. [Google Scholar] [CrossRef]
- Maymon, R.; Hall, N.C. A Review of First-Year Student Stress and Social Support. Soc. Sci. 2021, 10, 472. [Google Scholar] [CrossRef]
- Cohen, S.; Wills, T.A. Stress, social support, and the buffering hypothesis. Psychol. Bull. 1985, 98, 310. [Google Scholar] [CrossRef]
- Caravaca-Sánchez, F.; Wolff, N. Predictors of substance use among male prisoners in Spain: The role of childhood abuse and social support. J. Soc. Soc. Work Res. 2020, 11, 313–337. [Google Scholar] [CrossRef]
- Gros, D.F.; Flanagan, J.C.; Korte, K.J.; Mills, A.C.; Brady, K.T.; Back, S.E. Relations among social support, PTSD symptoms, and substance use in veterans. Psychol. Addict. Behav. 2016, 30, 764. [Google Scholar] [CrossRef] [PubMed]
- Unger, J. Drug Use and Cultural Factors Among Hispanic Adolescents and Emerging Adults, Los Angeles, 2006–2016. Inter-university Consortium for Political and Social Research [Distributor]: 2018. Available online: https://www.icpsr.umich.edu/web/NAHDAP/studies/36765 (accessed on 15 November 2022).
- Unger, J.B.; Ritt-Olson, A.; Wagner, K.D.; Soto, D.W.; Baezconde-Garbanati, L. Parent–child acculturation patterns and substance use among Hispanic adolescents: A longitudinal analysis. J. Prim. Prev. 2009, 30, 293–313. [Google Scholar] [CrossRef]
- Ginzler, J.A.; Garrett, S.B.; Baer, J.S.; Peterson, P.L. Measurement of negative consequences of substance use in street youth: An expanded use of the Rutgers Alcohol Problem Index. Addict. Behav. 2007, 32, 1519–1525. [Google Scholar] [CrossRef]
- Grigsby, T.J.; Forster, M.; Baezconde-Garbanati, L.; Soto, D.W.; Unger, J.B. Do adolescent drug use consequences predict externalizing and internalizing problems in emerging adulthood as well as traditional drug use measures in a Hispanic sample? Addict. Behav. 2014, 39, 644–651. [Google Scholar] [CrossRef] [PubMed]
- Zimet, G.D.; Dahlem, N.W.; Zimet, S.G.; Farley, G.K. The multidimensional scale of perceived social support. J. Personal. Assess. 1988, 52, 30–41. [Google Scholar] [CrossRef]
- Unger, J.B.; Schwartz, S.J.; Huh, J.; Soto, D.W.; Baezconde-Garbanati, L. Acculturation and perceived discrimination: Predictors of substance use trajectories from adolescence to emerging adulthood among Hispanics. Addict. Behav. 2014, 39, 1293–1296. [Google Scholar] [CrossRef] [PubMed]
- Allison, P.D. Handling missing data by maximum likelihood. In SAS Global Forum; Statistical Horizons: Haverford, PA, USA, 2012; p. 1038-21. [Google Scholar]
- Molenberghs, G.; Kenward, M. Missing Data in Clinical Studies; John Wiley & Sons: Hoboken, NJ, USA, 2007; Volume 61. [Google Scholar]
- Palmer, R.; Young, S.; Hopfer, C.; Corley, R.; Stallings, M.; Crowley, T.; Hewitt, J. Developmental epidemiology of drug use and abuse in adolescence and young adulthood: Evidence of generalized risk. Drug Alcohol Depend. 2009, 102, 78–87. [Google Scholar] [CrossRef]
- Squeglia, L.M.; Gray, K.M. Alcohol and drug use and the developing brain. Curr. Psychiatry Rep. 2016, 18, 46. [Google Scholar] [CrossRef]
- Robertson, A.A.; Xu, X.; Stripling, A. Adverse events and substance use among female adolescent offenders: Effects of coping and family support. Subst. Use Misuse 2010, 45, 451–472. [Google Scholar] [CrossRef]
- Karatekin, C.; Ahluwalia, R. Effects of adverse childhood experiences, stress, and social support on the health of college students. J. Interpers. Violence 2020, 35, 150–172. [Google Scholar] [CrossRef]
- Brown, S.M.; Shillington, A.M. Childhood adversity and the risk of substance use and delinquency: The role of protective adult relationships. Child Abus. Negl. 2017, 63, 211–221. [Google Scholar] [CrossRef] [PubMed]
- Chatterjee, D.; McMorris, B.; Gower, A.L.; Forster, M.; Borowsky, I.W.; Eisenberg, M.E. Adverse childhood experiences and early initiation of marijuana and alcohol use: The potential moderating effects of internal assets. Subst. Use Misuse 2018, 53, 1624–1632. [Google Scholar] [CrossRef] [PubMed]
- Forster, M.; Davis, L.; Grigsby, T.J.; Rogers, C.J.; Vetrone, S.F.; Unger, J.B. The role of familial incarceration and ethnic identity in suicidal ideation and suicide attempt: Findings from a longitudinal study of Latinx young adults in California. Am. J. Community Psychol. 2019, 64, 191–202. [Google Scholar] [CrossRef] [PubMed]
- Harrison, L.; Hughes, A. The Validity of Self-Reported Drug Use: Improving the Accuracy of Survey Estimates; NIH Publication No. 97-4147, NIDA Research Monograph 167; National Institute on Drug Abuse: Rockville, MD, USA, 1997.
- Reuben, A.; Moffitt, T.E.; Caspi, A.; Belsky, D.W.; Harrington, H.; Schroeder, F.; Hogan, S.; Ramrakha, S.; Poulton, R.; Danese, A. Lest we forget: Comparing retrospective and prospective assessments of adverse childhood experiences in the prediction of adult health. J. Child Psychol. Psychiatry 2016, 57, 1103–1112. [Google Scholar] [CrossRef]
| Variable | Frequency | Percent |
|---|---|---|
| Nativity | ||
| U.S. Born | 1228 | 87.78% |
| Not U.S. Born | 171 | 12.22% |
| Sex | ||
| Male | 570 | 40.60% |
| Female | 834 | 59.40% |
| Variable | Mean | Std Dev |
| Adverse Childhood Experiences | 2.75 | 2.19 |
| Perceived Social Support (in adolescence) | 26.02 | 4.01 |
| Socioeconomic Status (in adolescence) | −0.28 | 3.70 |
| MODEL 1 Problematic Alcohol and Drug Use—ACE × Time Interaction Model | MODEL 2 Problematic Alcohol and Drug Use—ACE × Time × Support Model | |
|---|---|---|
| Variance Components | Parameter Estimate (SE) | Parameter Estimate (SE) |
| UN1,1 | 1.830 *** (0.1678) | 1.803 *** (0.167) |
| UN2,1 | −0.1483 ** (0.0513) | −0.141 ** (0.051) |
| UN2,2 | 0.1521 *** (0.023) | 0.151 *** (0.023) |
| Time | 3.357 *** (0.080) | 3.359 *** (0.081) |
| Fixed Effects | Parameter Estimate (SE) | Parameter Estimate (SE) |
| Intercept | 7.995 ** (0.353) | 6.6568 (0.623) |
| Time | −0.044 (0.032) | 0.309 (0.216) |
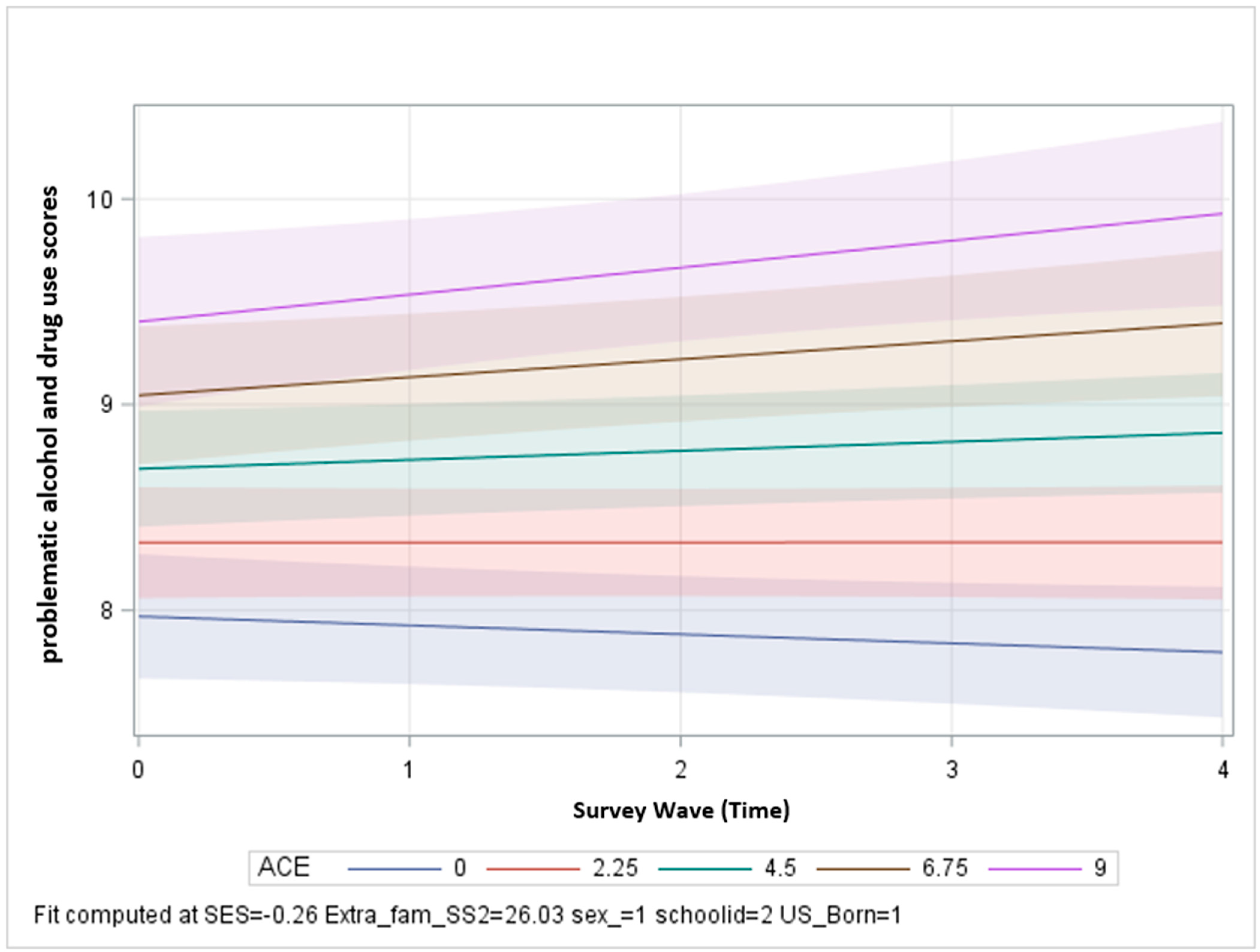
| ACE | 0.159 *** (0.026) | 0.637 *** (0.173) |
| Support | −0.025 * (0.011) | 0.025 (0.226) |
| Sex | 0.514 *** (0.092) | 0.513 *** (0.092) |
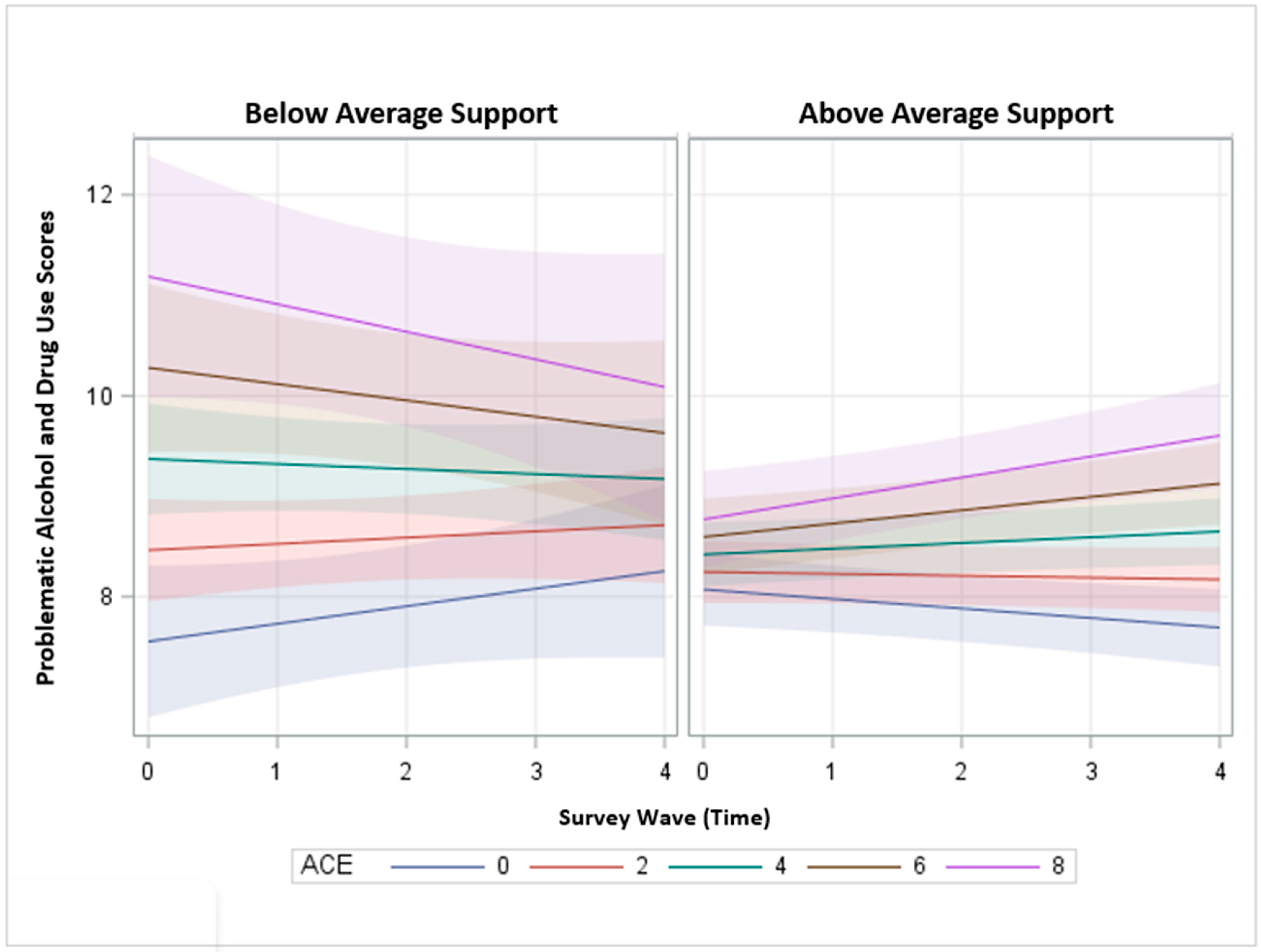
| Time × ACE | 0.019 * (0.009) | −0.103 (0.061) |
| Time × Support | −0.018 (0.008) | |
| ACE × Support | −0.018 ** (0.006) | |
| Time × ACE × Support | 0.005 * (0.002) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rogers, C.J.; Forster, M.; Sussman, S.; Steinberg, J.; Barrington-Trimis, J.L.; Grigsby, T.J.; Unger, J.B. The Impact of Childhood Trauma on Problematic Alcohol and Drug Use Trajectories and the Moderating Role of Social Support. Int. J. Environ. Res. Public Health 2023, 20, 2829. https://doi.org/10.3390/ijerph20042829
Rogers CJ, Forster M, Sussman S, Steinberg J, Barrington-Trimis JL, Grigsby TJ, Unger JB. The Impact of Childhood Trauma on Problematic Alcohol and Drug Use Trajectories and the Moderating Role of Social Support. International Journal of Environmental Research and Public Health. 2023; 20(4):2829. https://doi.org/10.3390/ijerph20042829
Chicago/Turabian StyleRogers, Christopher J., Myriam Forster, Steven Sussman, Jane Steinberg, Jessica L. Barrington-Trimis, Timothy J. Grigsby, and Jennifer B. Unger. 2023. "The Impact of Childhood Trauma on Problematic Alcohol and Drug Use Trajectories and the Moderating Role of Social Support" International Journal of Environmental Research and Public Health 20, no. 4: 2829. https://doi.org/10.3390/ijerph20042829
APA StyleRogers, C. J., Forster, M., Sussman, S., Steinberg, J., Barrington-Trimis, J. L., Grigsby, T. J., & Unger, J. B. (2023). The Impact of Childhood Trauma on Problematic Alcohol and Drug Use Trajectories and the Moderating Role of Social Support. International Journal of Environmental Research and Public Health, 20(4), 2829. https://doi.org/10.3390/ijerph20042829










