‘COVID Is Coming, and I’m Bloody Scared’: How Adults with Co-Morbidities’ Threat Perceptions of COVID-19 Shape Their Vaccination Decisions
Abstract
1. Introduction
1.1. Literature Review and Background
1.2. The Western Australian Pandemic and Vaccination Policy Context
2. Materials and Methods
3. Results
3.1. Perceiving the Threat: Severity Perceptions of COVID-19
“I’m fully vaccinated and boosted at this stage, but I also suffer from asthma and have done for a long time. So, I knew that if I didn’t get vaccinated and I caught it, it would have killed me.”
“I would say that I’ve been pretty cautious about the virus… I know what it’s like to get sick and not fully recover, and then I also I don’t think my body is a as equipped to fight the virus as perhaps another person my age.”
“The research on long COVID isn’t clear, is it? I don’t think they’re in a position yet because there aren’t any longitudinal studies to be clear about long COVID. So I have no concerns for long COVID more than I do for any other infectious disease.”
3.2. Perceiving the Threat: Susceptibility Perceptions of COVID-19
“I think that I’ve got a higher chance of getting COVID than I do flu and pneumonia because I don’t really hang around a lot of people who are sick with the flu. But, COVID is another thing altogether.”
3.3. Responding to the Threat with Vaccination: Response Efficacy
“I did actually speak to my endocrinologist and say, ‘Look, you know, again that thing of knowing what immunity … autoimmune stuff is triggered by viruses. What is the chance that this is gonna trigger something?’ And she said, ‘Oh, it’s possible, but it’s that risk versus, you know, which risk is higher kind of thing’ … But, you know, I’m very vaccine positive so, you know, I’m willing to trust the experts on that.”
3.4. Responding to the Threat with Vaccination: Self-Efficacy
3.5. Vaccination Journeys: How Responses to Fear and Vaccine Beliefs Shape Decisions
- Polly—a quintessential vaccine acceptance story
- Molly—a quintessential vaccine refusal story
- Charlie—a story of external coercion shaping vaccine decisions
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Centre for Disease and Control Prevention. Underlying Medical Conditions Associated with Higher Risk for Severe COVID-19: Information for Healthcare Professionals. Available online: https://www.cdc.gov/coronavirus/2019-ncov/hcp/clinical-care/underlyingconditions.html (accessed on 18 November 2022).
- Department of Health and Aged Care. Protecting older Australians: COVID-19 Update 12 March 2021. Available online: https://www.health.gov.au/news/newsletters/protecting-older-australians-covid-19-update-12-march-2021 (accessed on 10 January 2023).
- Seale, H.; McFadden, K.; Dyda, A.; Kaufman, J.; Heywood, A. The pendulum has swung: How do we ensure a life course approach to immunisation in Australia? Front. Public Health 2021, 9, 801176. [Google Scholar] [CrossRef] [PubMed]
- Department of Health and Aged Care. AstraZeneca ChAdOx1-S COVID-19 Vaccine. Available online: https://www.tga.gov.au/news/media-releases/astrazeneca-chadox1-s-covid-19-vaccine (accessed on 10 January 2023).
- Department of Health and Aged Care. ATAGI Statement on Revised Recommendations on the Use of COVID-19 Vaccine AstraZeneca, 17 June 2021. Available online: https://www.health.gov.au/news/atagi-statement-on-revised-recommendations-on-the-use-of-covid-19-vaccine-astrazeneca-17-june-2021 (accessed on 10 January 2023).
- Department of Health and Aged Care. ATAGI Statement on the Use of a 3rd Primary Dose of COVID-19 Vaccine in Individuals Who Are Severely Immunocompromised. 2021. Available online: https://www.health.gov.au/resources/publications/atagi-recommendations-on-the-use-of-a-third-primary-dose-of-covid-19-vaccine-in-individuals-who-are-severely-immunocompromised?language=en (accessed on 10 January 2023).
- Department of Health and Aged Care. TGA Provisionally Approves Novavax (Biocelect Pty Ltd’s) COVID-19 Vaccine NUVAXOVID. 2022. Available online: https://www.tga.gov.au/news/media-releases/tga-provisionally-approves-novavax-biocelect-pty-ltds-covid-19-vaccine-nuvaxovid (accessed on 10 January 2023).
- Department of Health and Aged Care. Nuvaxovid (Novavax). Available online: https://www.health.gov.au/our-work/covid-19-vaccines/approved-vaccines/novavax#:~:text=Novavax%20is%20approved%20and%20available,booster%20on%209%20June%202022 (accessed on 10 January 2023).
- Oliver, J.; Kaufman, J.; Bagot, K.; Bradfield, Z.; Homer, C.; Gibney, K.B.; Danchin, M. Drivers of COVID-19 vaccine hesitancy among women of childbearing age in Victoria, Australia: A descriptive qualitative study. Vaccine X 2022, 12, 100240. [Google Scholar] [CrossRef]
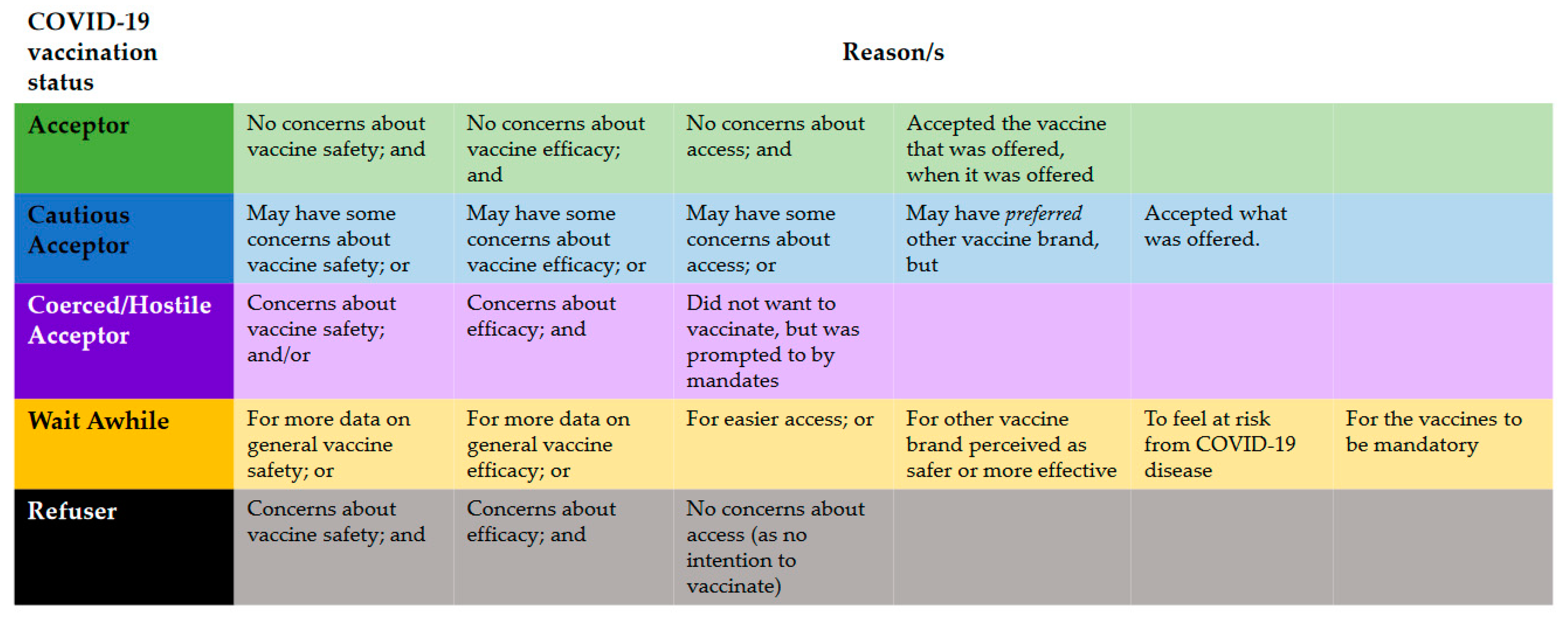
- Bedford, H.; Attwell, K.; Danchin, M.; Marshall, H.; Corben, P.; Leask, J. Vaccine hesitancy, refusal and access barriers: The need for clarity in terminology. Vaccine 2018, 36, 6556–6558. [Google Scholar] [CrossRef] [PubMed]
- World Health Organisation. Ten Threats to Global Health in 2019; World Health Organisation: Geneva, Switzerland, 2019.
- Bussink-Voorend, D.; Hautvast, J.L.A.; Vandeberg, L.; Visser, O.; Hulscher, M.E.J.L. A systematic literature review to clarify the concept of vaccine hesitancy. Nat. Hum. Behav. 2022, 6, 1634–1648. [Google Scholar] [CrossRef] [PubMed]
- Deml, M.J.; Buhl, A.; Notter, J.; Kliem, P.; Huber, B.M.; Pfeiffer, C.; Burton-Jeangros, C.; Tarr, P.E. ‘Problem patients and physicians’ failures’: What it means for doctors to counsel vaccine hesitant patients in Switzerland. Soc. Sci. Med. 2020, 255, 112946. [Google Scholar] [CrossRef] [PubMed]
- Larson, H.J.; Jarrett, C.; Eckersberger, E.; Smith, D.M.; Paterson, P. Understanding vaccine hesitancy around vaccines and vaccination from a global perspective: A systematic review of published literature, 2007–2012. Vaccine 2014, 32, 2150–2159. [Google Scholar] [CrossRef] [PubMed]
- Carlson, S.J.; McKenzie, L.; Roberts, L.; Blyth, C.C.; Attwell, K. Does a major change to a COVID-19 vaccine program alter vaccine intention? A qualitative investigation. Vaccine 2022, 40, 594–600. [Google Scholar] [CrossRef]
- Department of Health and Aged Care. Vaccination Numbers and Statistics. Available online: https://www.health.gov.au/our-work/covid-19-vaccines/vaccination-numbers-and-statistics (accessed on 10 January 2023).
- Wiley, K.E.; Leask, J.; Attwell, K.; Helps, C.; Degeling, C.; Ward, P.; Carter, S.M. Parenting and the vaccine refusal process: A new explanation of the relationship between lifestyle and vaccination trajectories. Soc. Sci. Med. 2020, 263, 113259. [Google Scholar] [CrossRef]
- Robb, C.E.; De Jager, C.A.; Ahmadi-Abhari, S.; Giannakopoulou, P.; Udeh-Momoh, C.; McKeand, J.; Price, G.; Car, J.; Majeed, A.; Ward, H. Associations of social isolation with anxiety and depression during the early COVID-19 pandemic: A survey of older adults in London, UK. Front. Psychiatry 2020, 11, 591120. [Google Scholar] [CrossRef]
- Mello, S.; Fitzhenry, D.; Pierpoint, R.; Collins, R. Experiences and priorities of older adults during the COVID-19 pandemic. Ir. J. Med. Sci. (1971-) 2022, 191, 2253–2256. [Google Scholar] [CrossRef]
- Michaud, K.; Wipfler, K.; Shaw, Y.; Simon, T.A.; Cornish, A.; England, B.R.; Ogdie, A.; Katz, P. Experiences of patients with rheumatic diseases in the United States during early days of the COVID-19 pandemic. ACR Open Rheumatol. 2020, 2, 335–343. [Google Scholar] [CrossRef]
- Wolf, M.S.; Serper, M.; Opsasnick, L.; O’Conor, R.M.; Curtis, L.; Benavente, J.Y.; Wismer, G.; Batio, S.; Eifler, M.; Zheng, P. Awareness, attitudes, and actions related to COVID-19 among adults with chronic conditions at the onset of the US outbreak: A cross-sectional survey. Ann. Intern. Med. 2020, 173, 100–109. [Google Scholar] [CrossRef]
- Singh, K.; Kondal, D.; Mohan, S.; Jaganathan, S.; Deepa, M.; Venkateshmurthy, N.S.; Jarhyan, P.; Anjana, R.M.; Narayan, K.M.; Mohan, V. Health, psychosocial, and economic impacts of the COVID-19 pandemic on people with chronic conditions in India: A mixed methods study. BMC Public Health 2021, 21, 685. [Google Scholar] [CrossRef]
- Reno, C.; Maietti, E.; Fantini, M.P.; Savoia, E.; Manzoli, L.; Montalti, M.; Gori, D. Enhancing COVID-19 vaccines acceptance: Results from a survey on vaccine hesitancy in Northern Italy. Vaccines 2021, 9, 378. [Google Scholar] [CrossRef]
- Yan, A.F.; Sun, X.; Zheng, J.; Mi, B.; Zuo, H.; Ruan, G.; Hussain, A.; Wang, Y.; Shi, Z. Perceived risk, behavior changes and Health-related outcomes during COVID-19 pandemic: Findings among adults with and without diabetes in China. Diabetes Res. Clin. Pract. 2020, 167, 108350. [Google Scholar] [CrossRef]
- Kaufman, J.; Bagot, K.L.; Tuckerman, J.; Biezen, R.; Oliver, J.; Jos, C.; Ong, D.S.; Manski-Nankervis, J.-A.; Seale, H.; Sanci, L.; et al. Qualitative exploration of intentions, concerns and information needs of vaccine-hesitant adults initially prioritised to receive COVID-19 vaccines in Australia. Aust. N. Z. J. Public Health 2022, 46, 16–24. [Google Scholar] [CrossRef]
- Attwell, K. The politics of picking: Selective vaccinators and population-level policy. SSM-Popul. Health 2019, 7, 100342. [Google Scholar] [CrossRef]
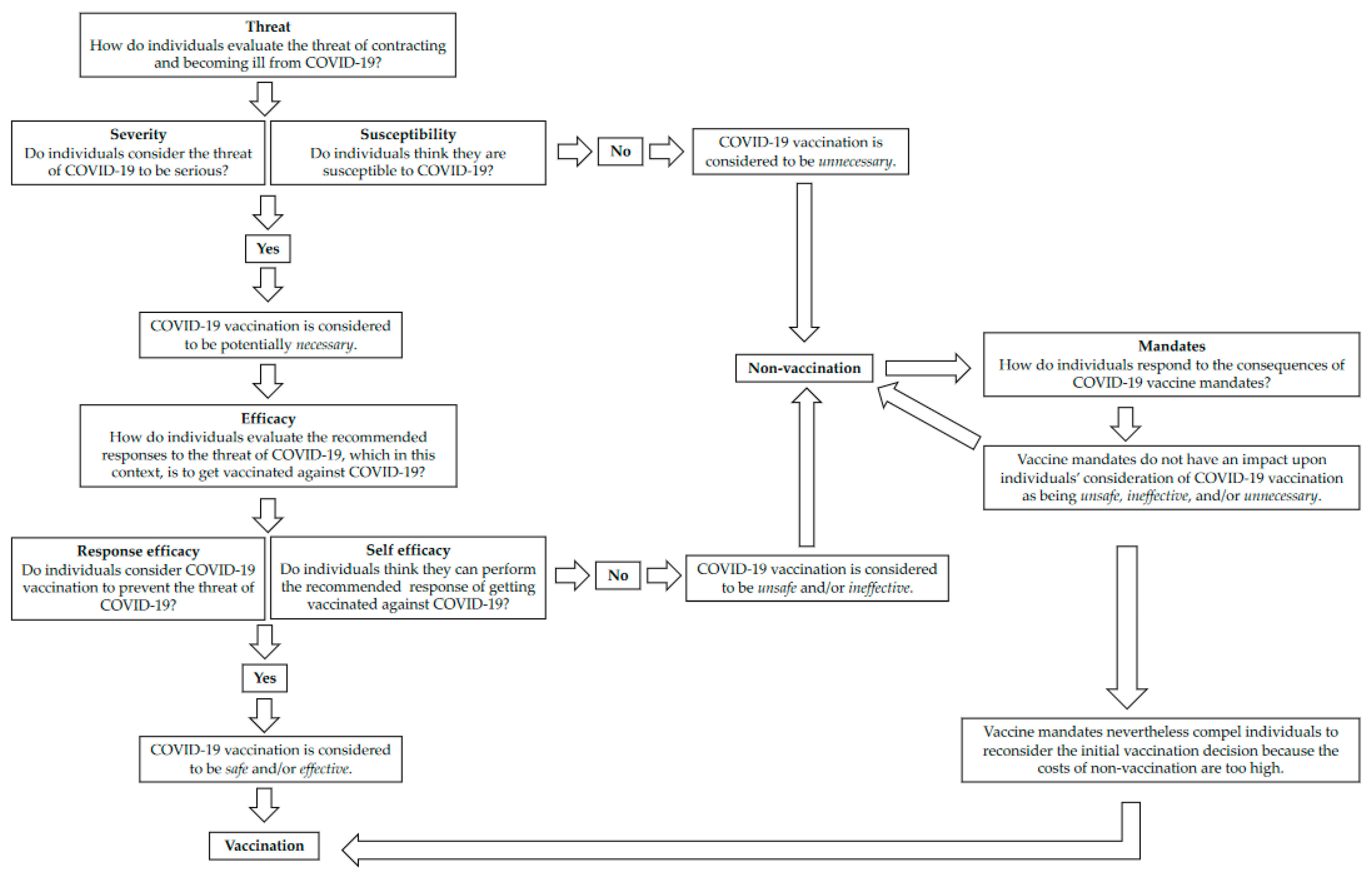
- Domosławska-Żylińska, K.; Krysińska-Pisarek, M.; Czabanowska, K.; Sesa, G. Vaccinated and unvaccinated risk perceptions and motivations for COVID-19 preventive measures based on EPPM—A Polish qualitative pilot study. Int. J. Environ. Res. Public Health 2022, 19, 13473. [Google Scholar] [CrossRef]
- Roberto, A.J.; Zhou, X. Predicting college students’ COVID-19 vaccination behavior: An application of the extended parallel process model. J. Behav. Med. 2022, 1–12. [Google Scholar] [CrossRef]
- Chu, H.; Liu, S. Integrating health behavior theories to predict American’s intention to receive a COVID-19 vaccine. Patient Educ. Couns. 2021, 104, 1878–1886. [Google Scholar] [CrossRef]
- Slonim, A.B.; Roberto, A.J.; Downing, C.R.; Adams, I.F.; Fasano, N.J.; Davis-Satterla, L.; Miller, M.A. Adolescents’ knowledge, beliefs, and behaviors regarding hepatitis B: Insights and implications for programs targeting vaccine-preventable diseases. J. Adolesc. Health 2005, 36, 178–186. [Google Scholar] [CrossRef]
- Kaufman, J.; Tuckerman, J.; Bonner, C.; Durrheim, D.N.; Costa, D.; Trevena, L.; Thomas, S.; Danchin, M. Parent-level barriers to uptake of childhood vaccination: A global overview of systematic reviews. BMJ Glob. Health 2021, 6, e006860. [Google Scholar] [CrossRef] [PubMed]
- Wiley, K.E.; Levy, D.; Shapiro, G.K.; Dube, E.; SteelFisher, G.K.; Sevdalis, N.; Ganter-Restrepo, F.; Menning, L.; Leask, J. A user-centered approach to developing a new tool measuring the behavioural and social drivers of vaccination. Vaccine 2021, 39, 6283–6290. [Google Scholar] [CrossRef] [PubMed]
- Betsch, C.; Schmid, P.; Heinemeier, D.; Korn, L.; Holtmann, C.; Böhm, R. Beyond confidence: Development of a measure assessing the 5C psychological antecedents of vaccination. PLoS ONE 2018, 13, e0208601. [Google Scholar] [CrossRef]
- Leask, J.; Quinn, H.E.; Macartney, K.; Trent, M.; Massey, P.; Carr, C.; Turahui, J. Immunisation attitudes, knowledge and practices of health professionals in regional NSW. Aust. N. Z. J. Public Health 2008, 32, 224–229. [Google Scholar] [CrossRef] [PubMed]
- Larson, H.J.; de Figueiredo, A.; Xiahong, Z.; Schulz, W.S.; Verger, P.; Johnston, I.G.; Cook, A.R.; Jones, N.S. The state of vaccine confidence 2016: Global insights through a 67-country survey. EBioMedicine 2016, 12, 295–301. [Google Scholar] [CrossRef]
- Smith, D.T.; Attwell, K.; Evers, U. Majority acceptance of vaccination and mandates across the political spectrum in Australia. Politics 2019, 40, 189–206. [Google Scholar] [CrossRef]
- Attwell, K.; Roberts, L.; Ji, J. COVID-19 vaccine mandates: Attitudes and effects on holdouts in a large Australian university population. Int. J. Environ. Res. Public Health 2022, 19, 10130. [Google Scholar] [CrossRef]
- Government of Western Australia: Department of Health. Coronavirus COVID-19 in Western Australia. Available online: https://experience.arcgis.com/experience/359bca83a1264e3fb8d3b6f0a028d768 (accessed on 29 April 2022).
- Towie, N. Western Australia to Reopen Border on 5 February after Almost Two Years Sealed Off from the World. Available online: https://www.theguardian.com/australia-news/2021/dec/13/western-australia-to-reopen-border-on-5-february-after-almost-two-years-sealed-off-from-the-world (accessed on 10 January 2023).
- Cook, R. COVID-19 Vaccination to Become Mandatory for Western Australian Health Care Workers. 2021. Available online: https://www.mediastatements.wa.gov.au/Pages/McGowan/2021/09/COVID-19-vaccination-to-become-mandatory-for-Western-Australian-health-care-workers.aspx#:~:text=These%20workers%20will%20need%20to%20be%20fully%20vaccinated%20by%20January,on%20placement%3B%20and%20ambulance%20officers (accessed on 2 September 2021).
- McGowan, M. COVID-19 Vaccine Required for Workers in the RESOURCES industry. 2021. Available online: https://www.mediastatements.wa.gov.au/Pages/McGowan/2021/10/COVID-19-vaccine-required-for-workers-in-the-resources-industry.aspx (accessed on 5 October 2021).
- McGowan, M. Mandatory COVID-19 Vaccination Policy to Further Protect WA. 2021. Available online: https://www.mediastatements.wa.gov.au/Pages/McGowan/2021/10/Mandatory-COVID-19-vaccination-policy-to-further-protect-WA.aspx (accessed on 20 October 2021).
- McGowan, M. COVID-19 Vaccination Third Dose NOW mandatory to Keep WA Safe. 2021. Available online: https://www.mediastatements.wa.gov.au/Pages/McGowan/2021/12/COVID-19-vaccination-third-dose-now-mandatory-to-keep-WA-safe.aspx (accessed on 22 December 2021).
- McGowan, M. WA to proceed with Safe Transition Plan from February 5, 2022. 2022. Available online: https://www.wa.gov.au/government/announcements/wa-proceed-safe-transition-plan-february-5-2022 (accessed on 13 December 2021).
- Harris, P.A.; Taylor, R.; Thielke, R.; Payne, J.; Gonzalez, N.; Conde, J.G. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inform. 2009, 42, 377–381. [Google Scholar] [CrossRef]
- Harris, P.A.; Taylor, R.; Minor, B.L.; Elliott, V.; Fernandez, M.; O’Neal, L.; McLeod, L.; Delacqua, G.; Delacqua, F.; Kirby, J. The REDCap consortium: Building an international community of software platform partners. J. Biomed. Inform. 2019, 95, 103208. [Google Scholar] [CrossRef]
- Attwell, K.; Carlson, S.; Tchilingirian, J.; Harper, T.; McKenzie, L.; Roberts, L.; Rizzi, M.; Westphal, D.; Effler, P.; Hughes, C.; et al. Coronavax: Preparing community and government for COVID-19 vaccination: A research protocol for a mixed methods social research project. BMJ Open 2021, 11, e049356. [Google Scholar] [CrossRef]
- Braun, V.; Clarke, V. Thematic analysis. In APA Handbook of Research Methods in Psychology: Vol. 2 Research Designs; Cooper, H., Ed.; American Psychological Association: Washington, DC, USA, 2012; Volume 2, pp. 57–71. [Google Scholar]
- Witte, K. Putting the fear back into fear appeals: The extended parallel process model. Commun. Monogr. 1992, 59, 329–349. [Google Scholar] [CrossRef]
- Hornsey, M.J.; Harris, E.A.; Fielding, K.S. The psychological roots of anti-vaccination attitudes: A 24-nation investigation. Health Psychol. 2018, 37, 307–315. [Google Scholar] [CrossRef]
- Omer, S.B.; Betsch, C.; Leask, J. Mandate vaccination with care. Nature 2019, 571, 469. [Google Scholar] [CrossRef]
- McGowan, M. Further Public Health Measures to be Phased Out. Available online: https://www.facebook.com/photo/?fbid=568794841276032&set=a.263657845123068 (accessed on 8 June 2022).

| Vaccination Status and Intention | Pseudonym | Comorbidity (Self-Identified) | Gender | Age |
|---|---|---|---|---|
| Acceptor, Triple dosed | Anna | High blood pressure, obesity | F | 24 |
| Acceptor, Triple dosed | Redgum | MADD (multiple acyl-CoA dehydrogenase deficiency—rare disease) | M | 21 |
| Acceptor, Triple dosed | Joan | Did not disclose specific comorbidity | Prefer not to say | 34 |
| Acceptor, Triple dosed | Jess | Autoimmune condition | F | 22 |
| Acceptor, Triple dosed | Dawn | Asthma | F | 59 |
| Acceptor, Triple dosed | Phoenix | Did not disclose specific comorbidity | F | 45 |
| Acceptor, Triple dosed | Polly | Type 2 Diabetes | F | 55 |
| Cautious acceptor, Triple dosed | Liz | Type 1 Diabetes | F | 46 |
| Cautious acceptor, Triple dosed | Boris | Asthma | M | 33 |
| Wait Awhile, Triple dosed | Gillian | Type 1 Diabetes | F | 23 |
| Coerced acceptor, One dose | Stewart | Obesity | M | 60 |
| Coerced acceptor, One dose, second dose booked | Charlie | Chronic neurological conditions | M | 30 |
| Refuser, No doses | Molly | Autoimmune disorder | F | 49 |
| Refuser, No doses | Sophie | Lupus and other conditions | F | 43 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Roberts, L.; Deml, M.J.; Attwell, K. ‘COVID Is Coming, and I’m Bloody Scared’: How Adults with Co-Morbidities’ Threat Perceptions of COVID-19 Shape Their Vaccination Decisions. Int. J. Environ. Res. Public Health 2023, 20, 2953. https://doi.org/10.3390/ijerph20042953
Roberts L, Deml MJ, Attwell K. ‘COVID Is Coming, and I’m Bloody Scared’: How Adults with Co-Morbidities’ Threat Perceptions of COVID-19 Shape Their Vaccination Decisions. International Journal of Environmental Research and Public Health. 2023; 20(4):2953. https://doi.org/10.3390/ijerph20042953
Chicago/Turabian StyleRoberts, Leah, Michael J. Deml, and Katie Attwell. 2023. "‘COVID Is Coming, and I’m Bloody Scared’: How Adults with Co-Morbidities’ Threat Perceptions of COVID-19 Shape Their Vaccination Decisions" International Journal of Environmental Research and Public Health 20, no. 4: 2953. https://doi.org/10.3390/ijerph20042953
APA StyleRoberts, L., Deml, M. J., & Attwell, K. (2023). ‘COVID Is Coming, and I’m Bloody Scared’: How Adults with Co-Morbidities’ Threat Perceptions of COVID-19 Shape Their Vaccination Decisions. International Journal of Environmental Research and Public Health, 20(4), 2953. https://doi.org/10.3390/ijerph20042953






