Association between Feelings of Trust and Security with Subjective Health among Mexican Migrants in the New York City Area
Abstract
:1. Introduction
2. Methods
2.1. Study Design and Sample
2.2. Study Variables
2.2.1. Subjective Health Status
2.2.2. Measures of Subjective Perceptions of Trust and Safety
2.2.3. Sociodemographic Characteristics
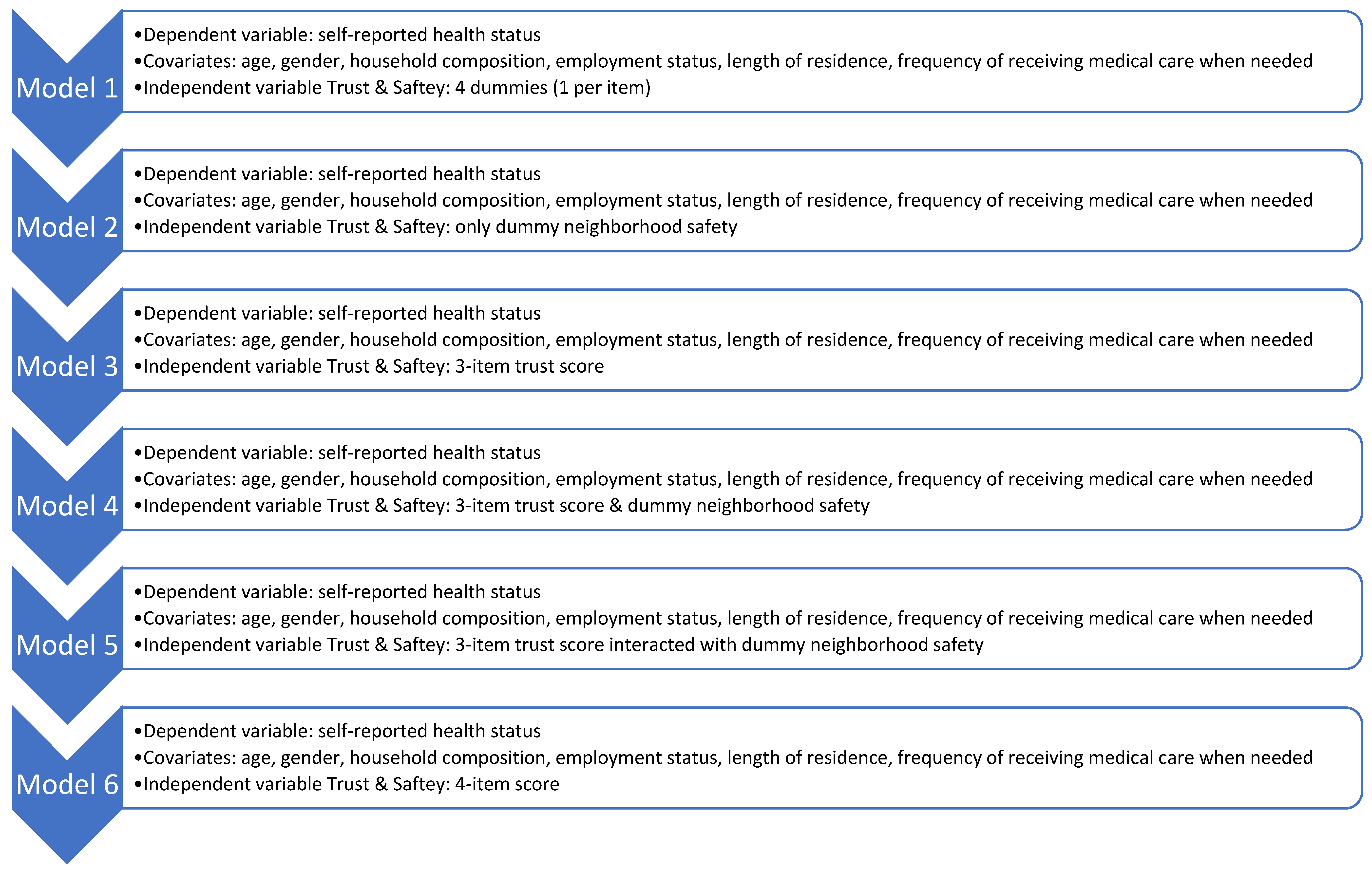
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Noe-Bustamante, L.; Flores, A.; Shah, S. Facts on Hispanics of Mexican Origin in the United States, 2017; Pew Research Center: Washington, DC, USA, 2019; Available online: https://www.pewresearch.org/hispanic/fact-sheet/u-s-hispanics-facts-on-mexican-origin-latinos/ (accessed on 14 December 2022).
- Gonzalez-Barrera, A.; Manuel Krogstad, J. What We Know about Illegal Immigration from Mexico; Pew Research Center: Washington, DC, USA, 2019; Available online: https://www.pewresearch.org/fact-tank/2019/06/28/what-we-know-about-illegal-immigration-from-mexico/ (accessed on 14 December 2022).
- Gómez de León, J.; Tuirán, R. Patrones de continuidad y cambio de la migración hacia Estados Unidos. In Migración México-Estados Unidos, Presente y Futuro; Tuirán, R., Ed.; Consejo Nacional de Población: Mexico City, Mexico, 2000; pp. 19–28. Available online: http://www.omi.gob.mx/work/models/OMI/Resource/481/ppyfuturo.pdf (accessed on 14 December 2022).
- Baker, B. Population Estimates. Illegal Alien Population Residing in the United States; Office of Immigration Statistics, Department of Homeland Security: Washington, DC, USA, 2018. Available online: https://www.dhs.gov/sites/default/files/publications/18_1214_PLCY_pops-est-report.pdf (accessed on 14 December 2022).
- Department of City Planning. NYC’s Foreign-Born, 2000–2015. New York City. 2017. Available online: https://www1.nyc.gov/assets/planning/download/pdf/about/dcp-priorities/data-expertise/nyc-foreign-born-info-brief.pdf?r=1 (accessed on 14 December 2022).
- Vilar-Compte, M.; Vargas Bustamante, A.; López-Olmedo, N.; Gaitán-Rossi, P.; Torres, J.; Peterson, K.E.; Teruel, G.; Pérez-Escamilla, R. Migration as a determinant of childhood obesity in the United States and Latin America. Obes. Rev. 2021, 3, E13240. [Google Scholar] [CrossRef] [PubMed]
- Teruya, S.A.; Bazargan-Hejazi, S. The Immigrant and Hispanic Paradoxes: A Systematic Review of Their Predictions and Effects. Hisp. J. Behav. Sci. 2013, 35, 486–509. [Google Scholar] [CrossRef] [PubMed]
- Allen, J.D.; Caspi, C.; Yang, M.; Leyva, B.; Stoddard, A.M.; Tamers, S.; Tucker-Seeley, R.D.; Sorensen, G.C. Pathways between acculturation and health behaviors among residents of low-income housing: The mediating role of social and contextual factors. Soc. Sci. Med. 2014, 123, 26–36. [Google Scholar] [CrossRef] [PubMed]
- Abraído-Lanza, A.F.; Chao, M.T.; Flórez, K.R. Do healthy behaviors decline with greater acculturation? Implications for the Latino mortality paradox. Soc. Sci. Med. 2005, 61, 1243–1255. [Google Scholar] [CrossRef]
- Abraído-Lanza, A.F.; Echeverría, S.E.; Flórez, K.R. Latino Immigrants, Acculturation, and Health: Promising New Directions in Research. Annu. Rev. Public Health 2016, 37, 219–236. [Google Scholar] [CrossRef]
- Eskenazi, B.; Fahey, C.A.; Kogut, K.; Gunier, R.; Torres, J.; Gonzales, N.A.; Holland, N.; Deardorff, J. Association of Perceived Immigration Policy Vulnerability With Mental and Physical Health Among US-Born Latino Adolescents in California. JAMA Pediatr. 2019, 173, 744–753. [Google Scholar] [CrossRef]
- Torres, J.M.; Deardorff, J.; Gunier, R.B.; Harley, K.G.; Alkon, A.; Kogut, K.; Eskenazi, B. Worry About Deportation and Cardiovascular Disease Risk Factors Among Adult Women: The Center for the Health Assessment of Mothers and Children of Salinas Study. Ann. Behav. Med. 2018, 52, 186–193. [Google Scholar] [CrossRef]
- Henry, J.; Keiser Family Foundation. Community Health Centers Prepare for Funding Uncertainty. 2019. Available online: https://www.kff.org/medicaid/issue-brief/community-health-centers-prepare-for-funding-uncertainty/ (accessed on 14 December 2022).
- Vargas Bustamante, A.; Chen, J. Health expenditure dynamics and years of US residence: Analyzing spending disparities among Latinos by citizenship/nativity status. Health Serv. Res. 2012, 47, 794–818. [Google Scholar] [CrossRef]
- Vargas Bustamante, A.; Fang, H.; Garza, J.; Carter-Pokras, O.; Wallace, S.P.; Rizzo, J.A.; Ortega, A.N. Variations in healthcare access and utilization among Mexican immigrants: The role of documentation status. J. Immigr. Minor. Health 2012, 14, 146–155. [Google Scholar] [CrossRef]
- Bustamante, A.V.; McKenna, R.M.; Viana, J.; Ortega, A.N.; Chen, J. Access-to-care differences between Mexican-heritage and other latinos in California after the Affordable Care Act. Health Aff. 2018, 37, 1400–1408. [Google Scholar] [CrossRef]
- Wallace, S.P.; Torres, J.; Sadegh-Nobari, T.; Pourat, N.; Brown, E.R. Undocumented Immigrants and Health Care Reform; UCLA Center for Health Policy Research: Los Angeles, CA, USA, 2012; pp. 1–48. Available online: https://healthpolicy.ucla.edu/publications/Documents/PDF/undocumentedreport-aug2013.pdf (accessed on 14 December 2022).
- Hacker, K.; Anies, M.; Folb, B.L.; Zallman, L. Barriers to health care for undocumented immigrants: A literature review. Risk Manag. Healthc. Policy 2015, 8, 175. [Google Scholar] [CrossRef] [PubMed]
- Morey, B.N.; García, S.J.; Nieri, T.; Bruckner, T.A.; Link, B.G. Symbolic disempowerment and Donald Trump’s 2016 presidential election: Mental health responses among Latinx and white populations. Soc. Sci. Med. 2021, 289, 114417. [Google Scholar] [CrossRef] [PubMed]
- Bernstein, H.; Gonzalez, D.; Karpman, M.; Zuckerman, S. One in Seven Adults in Immigrant Families Reported avoiding Public Benefit Programs in 2018; Urban Institute: Washington, DC, USA, 2019; Available online: https://www.immigrationresearch.org/node/2676 (accessed on 14 December 2022).
- Hesson, T. Exclusive: Visa Denials to Poor Mexicans Skyrocket under Trump’s State Department: POLITICO. 2019. Available online: https://www.politico.com/story/2019/08/06/visa-denials-poor-mexicans-trump-1637094 (accessed on 14 December 2022).
- Changes to “Public Charge” Inadmissibility Rule: Implications for Health and Health Coverage [Press Release]. KAISER FAMILY FOUNDATION (KFF). 2019. Available online: https://www.kff.org/racial-equity-and-health-policy/fact-sheet/public-charge-policies-for-immigrants-implications-for-health-coverage/ (accessed on 14 December 2022).
- Artiga, S.; Ubri, P. Living in an Immigrant Family in America: How Fear and Toxic Stress Are Affecting Daily Life, Well-Being, & Health; Kaiser Family Foundation: Menlo Park, CA, USA, 2017. Available online: http://resource.nlm.nih.gov/101727557 (accessed on 14 December 2022).
- Waxman, E. By Targeging SNAP, the Expanded “Public Charge” Rule Could Worsen Food Insecurity. 2018. Available online: https://www.urban.org/urban-wire/targeting-snap-expanded-public-charge-rule-could-worsen-food-insecurity (accessed on 14 December 2022).
- Artiga, S.; Lyons, B. Family Consequences of Detention/Deportation: Effects on Finances, Health, and Well-Being. 2018. Available online: https://www.kff.org/disparities-policy/issue-brief/family-consequences-of-detention-deportation-effects-on-finances-health-and-well-being/ (accessed on 14 December 2022).
- Morey, B.N. Mechanisms by Which Anti-Immigrant Stigma Exacerbates Racial/Ethnic Health Disparities. Am. J. Public Health 2018, 108, 460–463. [Google Scholar] [CrossRef] [PubMed]
- Caballero, E.; Gutierrez, R.; Schmitt, E.; Castenada, J.; Torres-Cacho, N.; Rodriguez, R.M. Impact of anti-immigrant rhetoric on Latinx families’ perceptions of child safety and health care access. J. Emerg. Med. 2022, 62, 264–274. [Google Scholar] [CrossRef]
- Wilson, K.; Elliott, S.; Law, M.; Eyles, J.; Jerrett, M.; Keller-Olaman, S. Linking perceptions of neighbourhood to health in Hamilton, Canada. J. Epidemiol. Community Health 2004, 58, 192–198. [Google Scholar] [CrossRef]
- Cain, C.L.; Wallace, S.P.; Ponce, N.A. Helpfulness, trust, and safety of neighborhoods: Social capital, household income, and self-reported health of older adults. Gerontol. 2018, 58, 4–14. [Google Scholar] [CrossRef]
- Bjornstrom, E.E. The neighborhood context of relative position, trust, and self-rated health. Soc. Sci. Med. 2011, 73, 42–49. [Google Scholar] [CrossRef]
- Appiah, D.; Luitel, S.; Fuentes, N.; Nwabuo, C.C. Perceived neighborhood social cohesion and the 10-year risk of cardiovascular disease in low-and middle-income countries: The World Health Organization Study on Global Aging and Adult Health. Health Place 2022, 77, 102895. [Google Scholar] [CrossRef]
- Miilunpalo, S.; Vuori, I.; Oja, P.; Pasanen, M.; Urponen, H. Self-rated health status as a health measure: The predictive value of self-reported health status on the use of physician services and on mortality in the working-age population. J. Clin. Epidemiol. 1997, 50, 517–528. [Google Scholar] [CrossRef]
- Burström, B.; Fredlund, P. Self rated health: Is it as good a predictor of subsequent mortality among adults in lower as well as in higher social classes? J. Epidemiol. Community Health 2001, 55, 836–840. [Google Scholar] [CrossRef] [Green Version]
- Stenholm, S.; Kivimäki, M.; Jylhä, M.; Kawachi, I.; Westerlund, H.; Pentti, J.; Goldberg, M.; Zins, M.; Vahtera, J. Trajectories of self-rated health in the last 15 years of life by cause of death. Eur. J. Epidemiol. 2016, 31, 177–185. [Google Scholar] [CrossRef] [PubMed]
- Hoffman, E.E.; Mair, T.T.; Hunter, B.A.; Prince, D.M.; Tebes, J.K. Neighborhood sexual violence moderates women’s perceived safety in urban neighborhoods. J. Community Psychol. 2018, 46, 79–94. [Google Scholar] [CrossRef]
- Assari, S.; Caldwell, C.H.; Zimmerman, M.A. Perceived neighborhood safety during adolescence predicts subsequent deterioration of subjective health two decades later; gender differences in a racially-diverse sample. Int. J. Prev. Med. 2015, 24, 117. [Google Scholar] [CrossRef] [PubMed]
- Stokes, J.E. Trajectories of perceived neighborhood quality across the life course: Sociodemographic determinants and implications for well-being. Soc. Sci. Res. 2019, 79, 181–193. [Google Scholar] [CrossRef]
- Beyer, K.M.; Malecki, K.M.; Hoormann, K.A.; Szabo, A.; Nattinger, A.B. Perceived neighborhood quality and cancer screening behavior: Evidence from the Survey of the Health of Wisconsin. J. Community Health 2016, 41, 134–137. [Google Scholar] [CrossRef]
- Greer, S.; Naidoo, M.; Archer, A.; Hinterland, K.; Gould, H.; De La Cruz, N.L.; Crossa, A.; Allison, K. Health of Latinos in New York City; NYC government: New York City, NY, USA, 2017; pp. 1–32. Available online: https://www1.nyc.gov/assets/doh/downloads/pdf/episrv/2017-latino-health-sp.pdf (accessed on 14 December 2022).
- Sommers, B.D.; Maylone, B.; Blendon, R.J.; Orav, E.J.; Epstein, A.M. Three-year impacts of the Affordable Care Act: Improved medical care and health among low-income adults. Health Aff. 2017, 36, 1119–1128. [Google Scholar] [CrossRef]
- Sommers, B.D.; Gawande, A.A.; Baicker, K. Health insurance coverage and health—What the recent evidence tells us. Mass. Med. Soc. 2017, 377, 586–593. [Google Scholar] [CrossRef]
- Hayes, S.L.; Riley, P.; Radley, D.C.; McCarthy, D. Reducing racial and ethnic disparities in access to care: Has the Affordable Care Act made a difference? Issue Brief 2017, 2017, 1–14. Available online: https://pubmed.ncbi.nlm.nih.gov/28836751/ (accessed on 14 December 2022).
- Lüdecke, D. sjPlot: Data Visualization for Statistics in Social Science, R package version 2.8.12. 2022. Available online: https://CRAN.R-project.org/package=sjPlot(accessed on 14 December 2022).
- QGIS Development Team. QGIS Geographic Information System. Open Source Geospatial Foundation. 2009. Available online: http://qgis.org (accessed on 14 December 2022).
- America’s Health Rankings. United Health Foundation. Annual Report. 2019. Available online: https://www.americashealthrankings.org/explore/annual/measure/Diabetes/state/NY (accessed on 14 December 2022).
- Asad, A.L.; Garip, F. Mexico-US Migration in Time: From Economic to Social Mechanisms. ANNALS Am. Acad. Political Soc. Sci. 2019, 684, 60–84. [Google Scholar] [CrossRef]
- Delva, J.; Horner, P.; Martinez, R.; Sanders, L.; Lopez, W.D.; Doering-White, J. Mental health problems of children of undocumented parents in the United States: A hidden crisis. J. Community Posit. Pract. 2013, 13, 25–35. Available online: http://jppc.ro/en/index.php/jppc/article/view/203/180 (accessed on 14 December 2022).
- Vargas, E.D.; Ybarra, V.D. US citizen children of undocumented parents: The link between state immigration policy and the health of Latino children. J. Immigr. Minor. Health 2017, 19, 913–920. [Google Scholar] [CrossRef] [PubMed]
- Vilar-Compte, M.; Macinko, J.; Weitzman, B.C.; Avendaño-Villela, C.M. Short relative leg length is associated with overweight and obesity in Mexican immigrant women. Int. J. Equity Health 2019, 18, 103. [Google Scholar] [CrossRef] [PubMed] [Green Version]


| Total (N = 266) | ||
|---|---|---|
| Variable | % (N) | p-Value |
| Age, years (mean, SD) | 39.14 (10.78) | |
| Sex (%, n) | 0.030 * | |
| Male | 43.30% (113) | |
| Female | 56.70% (148) | |
| Household composition (%, n) | <0.000 * | |
| With children | 65.5% (169) | |
| Without children | 34.5% (89) | |
| Employment status (%, n) | <0.000 * | |
| Not working | 24.43% (64) | |
| Working | 75.57% (198) | |
| Length of residence in the US (mean, SD) | 17.33 (8.18) | |
| Diagnosed comorbidities | 0.010 * | |
| One or more diagnosed comorbidities | 42.11% (112) | |
| Without diagnosed comorbidities | 57.89% (154) | |
| Has valid health insurance in the US (%, n) | 37.6% (97) | |
| How frequently has received medical care when needed (%, n) | 0.0403 * | |
| Never or Sometimes | 56.37% (146) | |
| Usually or Always | 43.63% (113) | |
| Self-reported health status (%, n) | 0.753 | |
| Fair or bad | 50.99% (129) | |
| Excellent, very good, and good | 49.01% (124) | |
| Subjective measures of trust and safety | ||
| I can trust most people in my community (%, n) | 0.001 * | |
| Disagree or Strongly disagree | 39.29% (99) | |
| Agree or Strongly agree | 60.71% (153) | |
| I can get help from my neighbors whenever I need it (%, n) | <0.000 * | |
| Disagree or Strongly disagree | 25.82% (63) | |
| Agree or Strongly agree | 74.18% (181) | |
| I feel safe when I walk alone at night in my community (%, n) | <0.000 * | |
| Disagree or Strongly disagree | 18.11% (46) | |
| Agree or Strongly agree | 81.89% (208) | |
| Rating of neighborhood safety (%, n) | <0.000 * | |
| Insecure or Very insecure | 13.73% (35) | |
| Secure or Very secure | 86.27% (220) | |
| Three-item measure of trust (mean, SD) | 2.17 (0.99) | |
| Four-item composite measure of trust and safety (mean, SD) | 3.04 (1.16) | |
| Variable | Self-Reported Health Status (%, n) | p-Value | |
|---|---|---|---|
| Poor Health (n = 129) | Good Health (n = 124) | ||
| Age, years (mean ± SD) | 40.0 ± 11.2 | 38.7 ± 10.3 | 0.348 |
| Sex (%, n) | 0.429 | ||
| Male | 46.9% (60) | 41.1% (51) | |
| Female | 53.1% (68) | 58.9% (73) | |
| Household composition (%, n) | 0.253 | ||
| With children | 61.7% (79) | 69.4% (84) | |
| Without children | 38.3% (49) | 30.6% (37) | |
| Employment status (%, n) | 0.196 | ||
| Not working | 27.9% (36) | 20.2% (25) | |
| Working | 72.1% (93) | 79.8% (99) | |
| Length of residence in the US (mean, SD) | 18.0 ± 7.6 | 16.9 ± 8.8 | 0.273 |
| Diagnosed comorbidities | <0.001 * | ||
| One or more diagnosed comorbidities | 55% (71) | 32.3% (40) | |
| Without diagnosed comorbidities | 45% (58) | 67.7% (84) | |
| Health insurance (%, n) | 0.523 | ||
| Does not have a valid health insurance in the US | 64.1% (82) | 59.3% (73) | |
| Has valid health insurance in the US | 35.9% (46) | 40.7% (50) | |
| How frequently has received medical care when needed (%, n) | 0.465 | ||
| Never or Sometimes | 58.6% (75) | 53.2% (66) | |
| Usually or Always | 41.4% (53) | 46.8% (58) | |
| Subjective measures of trust and safety | |||
| I can trust most people in my community (%, n) | 0.961 | ||
| Disagree or Strongly disagree | 39.4% (50) | 39.7% (48) | |
| Agree or Strongly agree | 60.6% (77) | 60.3% (73) | |
| I can get help from my neighbors whenever I need it (%, n) | 0.099 | ||
| Disagree or Strongly disagree | 30.6% (38) | 20.5% (24) | |
| Agree or Strongly agree | 69.4% (86) | 79.5% (93) | |
| I feel safe when I walk alone at night in my community (%, n) | 0.018 * | ||
| Disagree or Strongly disagree | 24.4% (31) | 12.1% (15) | |
| Agree or Strongly agree | 75.6% (96) | 87.9% (109) | |
| Rating of neighborhood safety (%, n) | 0.002 * | ||
| Insecure or Very insecure | 21.1% (27) | 6.5% (8) | |
| Secure or Very secure | 78.9% (101) | 93.5% (115) | |
| Three-item measure of trust (mean, SD) | 2.1 ± 1.1 | 2.3 ± 0.9 | 0.123 |
| Four-item composite measure of trust and safety (mean, SD) | 2.9 ± 1.3 | 3.2 ± 1.0 | 0.019 * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gaitán-Rossi, P.; Vilar-Compte, M.; Ferré-Eguiluz, I.; Ortiz, L.; Garcia, E. Association between Feelings of Trust and Security with Subjective Health among Mexican Migrants in the New York City Area. Int. J. Environ. Res. Public Health 2023, 20, 2981. https://doi.org/10.3390/ijerph20042981
Gaitán-Rossi P, Vilar-Compte M, Ferré-Eguiluz I, Ortiz L, Garcia E. Association between Feelings of Trust and Security with Subjective Health among Mexican Migrants in the New York City Area. International Journal of Environmental Research and Public Health. 2023; 20(4):2981. https://doi.org/10.3390/ijerph20042981
Chicago/Turabian StyleGaitán-Rossi, Pablo, Mireya Vilar-Compte, Isabel Ferré-Eguiluz, Luis Ortiz, and Erika Garcia. 2023. "Association between Feelings of Trust and Security with Subjective Health among Mexican Migrants in the New York City Area" International Journal of Environmental Research and Public Health 20, no. 4: 2981. https://doi.org/10.3390/ijerph20042981
APA StyleGaitán-Rossi, P., Vilar-Compte, M., Ferré-Eguiluz, I., Ortiz, L., & Garcia, E. (2023). Association between Feelings of Trust and Security with Subjective Health among Mexican Migrants in the New York City Area. International Journal of Environmental Research and Public Health, 20(4), 2981. https://doi.org/10.3390/ijerph20042981







