Hope Buffers the Effect of Fear of COVID-19 on Depression among College Students: Insomnia as a Mediator
Abstract
:1. Introduction
1.1. The Relationship between Fear of COVID-19 and Depression
1.2. Hope Moderates the Relationship between Fear of COVID-19 and Depression
1.3. Insomnia Mediates the Relationship between Fear of COVID-19 and Depression
1.4. Hope Buffers the Relationship between Fear of COVID-19 and Insomnia
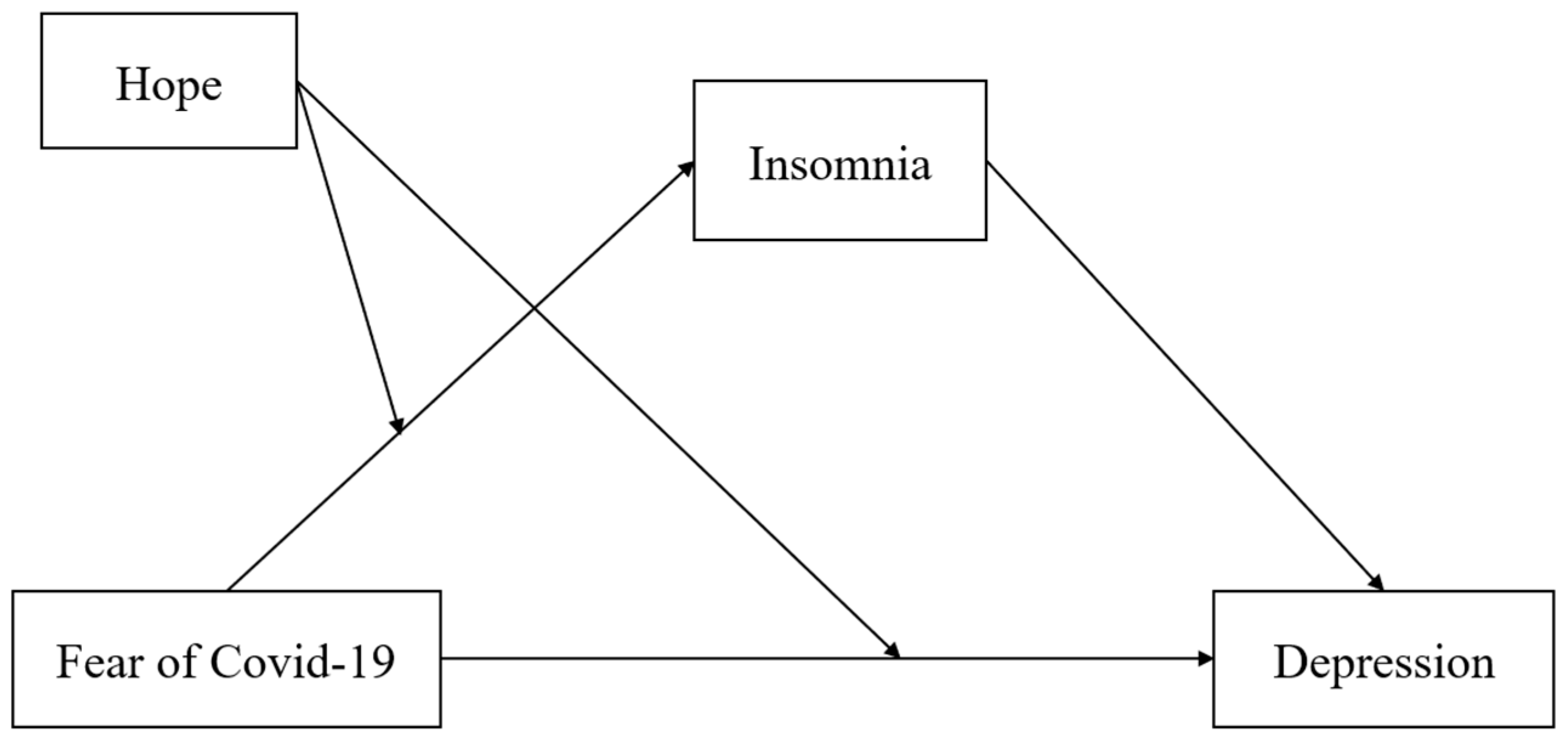
1.5. The Present Study
2. Materials and Methods
2.1. Participants and Sampling
2.2. Measures
2.2.1. Fear of COVID-19 Scale
2.2.2. Athens Insomnia Scale
2.2.3. Adult Dispositional Hope Scale
2.2.4. The Patient Health Questionnaire
2.3. Data Analysis
3. Results
3.1. Common Method Bias
3.2. Descriptive Statistics
3.3. The Mediated Moderation Model Test
4. Discussion
4.1. Significance of the Study
4.2. Fear of COVID-19 and Depression
4.3. Hope as a Moderator on the Relationship between Fear of COVID-19 and Depression
4.4. Discussion on the Mediated Moderation Model
4.5. Implications for Practice
5. Limitations and Implications for Future Research
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Durmuş, M.; Öztürk, Z.; Şener, N.; Eren, S.Y. The Relationship between the Fear of Covid-19, Depression, and Spiritual Well-Being in Pregnant Women. J. Relig. Health 2021, 61, 798–810. [Google Scholar] [CrossRef] [PubMed]
- Liu, Q.W.; Zhao, G.Z.; Ji, B.; Liu, Y.T.; Zhang, J.Y.; Mou, Q.J.; Shi, T.Y. Analysis of the influence of the psychology changes of fear induced by the COVID-19 epidemic on the body. World J. Acupunct-Mox. 2020, 30, 85–89. [Google Scholar] [CrossRef] [PubMed]
- Wieteska-Miłek, M.; Szmit, S.; Florczyk, M.; Kuśmierczyk-Droszcz, B.; Ryczek, R.; Dzienisiewicz, M.; Torbicki, A.; Kurzyna, M. Fear of COVID-19, Anxiety and Depression in Patients with Pulmonary Arterial Hypertension and Chronic Thromboembolic Pulmonary Hypertension during the Pandemic. J. Clin. Med. 2021, 10, 4195. [Google Scholar] [CrossRef] [PubMed]
- Cikrikci, O.; Cikrikci, N.; Griffiths, M. Fear of COVID-19, stress and depression: A meta-analytic test of the mediating role of anxiety. Psychol. Psychother.-T. Res. Pract. 2022, 95, 853–874. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Hidalgo, A.J.; Pantaleón, Y.; Dios, I.; Falla, D. Fear of COVID-19, Stress, and Anxiety in University Undergraduate Students: A Predictive Model for Depression. Front. Psychol. 2020, 11, 591797. [Google Scholar] [CrossRef]
- Ma, Y.-F.; Li, W.; Deng, H.-B.; Wang, L.; Wang, Y.; Wang, P.-H.; Bo, H.-X.; Cao, J.; Wang, Y.; Zhu, L.-Y.; et al. Prevalence of depression and its association with quality of life in clinically stable patients with COVID-19. J. Affect. Disord. 2020, 275, 145–148. [Google Scholar] [CrossRef]
- Liu, X.; Luo, W.-T.; Li, Y.; Li, C.-N.; Hong, Z.-S.; Chen, H.-L.; Xiao, F.; Xia, J.-Y. Psychological status and behavior changes of the public during the COVID-19 epidemic in China. Infect. Dis. Poverty 2020, 9, 1–11. [Google Scholar] [CrossRef]
- Ettman, C.K.; Abdalla, S.M.; Cohen, G.H.; Sampson, L.; Vivier, P.M.; Galea, S. Prevalence of Depression Symptoms in US Adults Before and During the COVID-19 Pandemic. JAMA Netw. Open 2020, 3, e2019686. [Google Scholar] [CrossRef]
- Karakose, T. Assessing the Relationships between Internet Addiction, Depression, COVID-19-Related Fear, Anxiety, and Suspicion among Graduate Students in Educational Administration: A Structural Equation Modeling Analysis. Sustainability 2022, 14, 5356. [Google Scholar] [CrossRef]
- Rehman, T.; Singh, T.; Sharma, S.; Kumar, J.; Govindan, D.; Singh, S.M. Prevalence of Depression and Anxiety during the COVID-19 Pandemic among the Residents of an Urban Slum in North India. J. Neurosci. Rural. Pract. 2021, 12, 153–158. [Google Scholar] [CrossRef]
- Feldman, D.B. Hope and Fear in the Midst of Coronavirus: What Accounts for COVID-19 Preparedness? Am. Behav. Sci. 2021, 65, 1929–1950. [Google Scholar] [CrossRef]
- Stolte, O. Hope in the age of anxiety. Scioli, A., and Biller, H.B. (2009). New York: Oxford University Press. ISBN 978-0-19-4, 440 pages. J. Community Appl. Soc. Psychol. 2010, 20, 331–332. [Google Scholar] [CrossRef]
- Visser, P.L.; Loess, P.; Jeglic, E.L.; Hirsch, J.K. Hope as a Moderator of Negative Life Events and Depressive Symptoms in a Diverse Sample. Stress Health 2012, 29, 82–88. [Google Scholar] [CrossRef] [PubMed]
- Di Corrado, D.; Muzii, B.; Magnano, P.; Coco, M.; La Paglia, R.; Maldonato, N.M. The Moderated Mediating Effect of Hope, Self-Efficacy and Resilience in the Relationship between Post-Traumatic Growth and Mental Health during the COVID-19 Pandemic. Healthcare 2022, 10, 1091. [Google Scholar] [CrossRef] [PubMed]
- Laslo-Roth, R.; George-Levi, S.; Margalit, M. Social participation and posttraumatic growth: The serial mediation of hope, social support, and reappraisal. J. Community Psychol. 2020, 50, 47–63. [Google Scholar] [CrossRef]
- Snyder, C.R. Reality Negotiation: From Excuses to Hope and Beyond. J. Soc. Clin. Psychol. 1989, 8, 130–157. [Google Scholar] [CrossRef]
- Rasmussen, H.N.; Wrosch, C.; Scheier, M.F.; Carver, C. Self-Regulation Processes and Health: The Importance of Optimism and Goal Adjustment. J. Pers. 2006, 74, 1721–1748. [Google Scholar] [CrossRef]
- Speed, T.J.; Hanks, L.; Turner, G.; Gurule, E.; Kearson, A.; Buenaver, L.; Smith, M.T.; Antoine, D. A comparison of cognitive behavioral therapy for insomnia to standard of care in an outpatient substance use disorder clinic embedded within a therapeutic community: A RE-AIM framework evaluation. Trials 2022, 23, 1–15. [Google Scholar] [CrossRef]
- Ahorsu, D.K.; Lin, C.-Y.; Imani, V.; Saffari, M.; Griffiths, M.D.; Pakpour, A.H. The Fear of COVID-19 Scale: Development and Initial Validation. Int. J. Ment. Health Addict. 2020, 20, 1537–1545. [Google Scholar] [CrossRef]
- Hirsch, J.K.; Ma, P.L.V.; Chang, E.C.; Jeglic, E.L. Race and Ethnic Differences in Hope and Hopelessness as Moderators of the Association Between Depressive Symptoms and Suicidal Behavior. J. Am. Coll. Health 2012, 60, 115–125. [Google Scholar] [CrossRef]
- Muyan-Yılık, M.; Demir, A. A Pathway Towards Subjective Well-Being for Turkish University Students: The Roles of Dispositional Hope, Cognitive Flexibility, and Coping Strategies. J. Happiness Stud. 2019, 21, 1945–1963. [Google Scholar] [CrossRef]
- Long, L.J.; Bistricky, S.L.; Phillips, C.A.; D’Souza, J.M.; Richardson, A.L.; Lai, B.S.; Short, M.; Gallagher, M.W. The Potential Unique Impacts of Hope and Resilience on Mental Health and Well-Being in the Wake of Hurricane Harvey. J. Trauma. Stress 2020, 33, 962–972. [Google Scholar] [CrossRef]
- Waynor, W.R.; Gao, N.; Dolce, J.N.; Haytas, L.A.; Reilly, A. The relationship between hope and symptoms. Psychiatr. Rehabil. J. 2012, 35, 345–348. [Google Scholar] [CrossRef]
- Yuan, K.; Zheng, Y.-B.; Wang, Y.-J.; Sun, Y.-K.; Gong, Y.-M.; Huang, Y.-T.; Chen, X.; Liu, X.-X.; Zhong, Y.; Su, S.-Z.; et al. A systematic review and meta-analysis on prevalence of and risk factors associated with depression, anxiety and insomnia in infectious diseases, including COVID-19: A call to action. Mol. Psychiatry 2022, 27, 3214–3222. [Google Scholar] [CrossRef] [PubMed]
- Cheng, P.; Kalmbach, D.A.; Castelan, A.C.; Murugan, N.; Drake, C.L. Depression prevention in digital cognitive behavioral therapy for insomnia: Is rumination a mediator? J. Affect. Disord. 2020, 273, 434–441. [Google Scholar] [CrossRef] [PubMed]
- Kalmbach, A.D. The emerging role of prenatal insomnia therapy in the prevention of perinatal depression and anxiety. Sleep 2022, 45, 1–3. [Google Scholar] [CrossRef] [PubMed]
- van Mill, J.G.; Hoogendijk, W.J.G.; Vogelzangs, N.; van Dyck, R.; Penninx, B.W.J.H. Insomnia and Sleep Duration in a Large Cohort of Patients with Major Depressive Disorder and Anxiety Disorders. J. Clin. Psychiatry 2010, 71, 239–246. [Google Scholar] [CrossRef] [PubMed]
- Cheng, P.; Kalmbach, A.D.; Tallent, G.; Joseph, C.L.; Espie, A.C.; Drake, C.L. Depression prevention via digital cognitive behavioral therapy for insomnia: A randomized controlled trial. Sleep 2019, 42, 1–9. [Google Scholar] [CrossRef]
- Baglioni, C.; Battagliese, G.; Feige, B.; Spiegelhalder, K.; Nissen, C.; Voderholzer, U.; Lombardo, C.; Riemann, D. Insomnia as a predictor of depression: A meta-analytic evaluation of longitudinal epidemiological studies. J. Affect. Disord. 2011, 135, 10–19. [Google Scholar] [CrossRef]
- Shanahan, L.; Copeland, W.E.; Angold, A.; Bondy, C.L.; Costello, E.J. Sleep Problems Predict and Are Predicted by Generalized Anxiety/Depression and Oppositional Defiant Disorder. J. Am. Acad. Child Adolesc. Psychiatry 2014, 53, 550–558. [Google Scholar] [CrossRef] [Green Version]
- Smith, K.E.; Pollak, S.D. Early life stress and development: Potential mechanisms for adverse outcomes. J. Neurodev. Disord. 2020, 12, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Drake, C.L.; Cheng, P.; Almeida, D.M.; Roth, T. Familial Risk for Insomnia Is Associated With Abnormal Cortisol Response to Stress. Sleep 2017, 40, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Kalmbach, D.A.; Anderson, J.R.; Drake, C.L. The impact of stress on sleep: Pathogenic sleep reactivity as a vulnerability to insomnia and circadian disorders. J. Sleep Res. 2018, 27, e12710. [Google Scholar] [CrossRef] [PubMed]
- LeMoult, J.; Humphreys, K.L.; Tracy, A.; Hoffmeister, J.-A.; Ip, E.; Gotlib, I.H. Meta-analysis: Exposure to Early Life Stress and Risk for Depression in Childhood and Adolescence. J. Am. Acad. Child Adolesc. Psychiatry 2019, 59, 842–855. [Google Scholar] [CrossRef]
- Hamilton, J.L.; Buysse, D.J. Reducing Suicidality Through Insomnia Treatment: Critical Next Steps in Suicide Prevention. Am. J. Psychiatry 2019, 176, 897–899. [Google Scholar] [CrossRef]
- Hertenstein, E.; Feige, B.; Gmeiner, T.; Kienzler, C.; Spiegelhalder, K.; Johann, A.; Jansson-Fröjmark, M.; Palagini, L.; Rücker, G.; Riemann, D.; et al. Insomnia as a predictor of mental disorders: A systematic review and meta-analysis. Sleep Med. Rev. 2019, 43, 96–105. [Google Scholar] [CrossRef]
- Al-Otaibi, T.; Abbas, A.; Nagib, A.M.; Gheith, O.A.; Nair, P.; Farid, M.M.; Albader, M.A.S. COVID-somnia: Anxiety, insomnia, and poor sleep among second-line healthcare workers during COVID-19 pandemic. Egypt. J. Bronchol. 2022, 16, 1–10. [Google Scholar] [CrossRef]
- Cai, H.; Zhao, Y.-J.; Xing, X.; Tian, T.; Qian, W.; Liang, S.; Wang, Z.; Cheung, T.; Su, Z.; Tang, Y.-L.; et al. Network Analysis of Comorbid Anxiety and Insomnia Among Clinicians with Depressive Symptoms During the Late Stage of the COVID-19 Pandemic: A Cross-Sectional Study. Nat. Sci. Sleep 2022, 14, 1351–1362. [Google Scholar] [CrossRef]
- Okajima, I.; Honda, Y.; Semba, O.; Kiyota, Y.; Tani, Y. Effects of COVID-19-Related Anxiety and Sleep Problems on Loneliness and Feelings of School Refusal in Adolescents. Front. Psychiatry 2022, 13, 1–7. [Google Scholar] [CrossRef]
- Li, Y.I.; Starr, L.R.; Wray-Lake, L. Insomnia mediates the longitudinal relationship between anxiety and depressive symptoms in a nationally representative sample of adolescents. Depress. Anxiety 2018, 35, 583–591. [Google Scholar] [CrossRef]
- Smith, M.B. Hope and despair: Keys to the socio-psychodynamics of youth. Am. J. Orthopsychiatr. 1983, 53, 388–399. [Google Scholar] [CrossRef] [PubMed]
- Gupta, R.; Mahajan, R.; Bakhshi, A.; Gupta, K.; Singh, D.; Kaur, B. Fear vs. hope in India: Finding the silver lining amid the dark clouds of COVID-19. Pers. Individ. Differ. 2021, 181, 111017. [Google Scholar] [CrossRef] [PubMed]
- Xiao, S.; Liu, S.; Zhang, P.; Yu, J.; A, H.; Wu, H.; Zhang, F.; Xiao, Y.; Ma, N.; Zhang, X.; et al. The Association Between Depressive Symptoms and Insomnia in College Students in Qinghai Province: The Mediating Effect of Rumination. Front. Psychiatry 2021, 12, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Frojd, L.A.; Papageorgiou, C.; Munkhaugen, J.; Moum, T.; Sverre, E.; Nordhus, I.H.; Dammen, T. Worry and rumination predict insomnia in patients with coronary heart disease: A cross-sectional study with long-term follow-up. J. Clin. Sleep Med. 2022, 18, 779–787. [Google Scholar] [CrossRef]
- Amra, B.; Ghadiry, F.; Vaezi, A.; Nematollahy, A.; Radfar, N.; Haghjoo, S.; Penzel, T.; Morin, C.M. Effect of one-shot cognitive behavioral therapy on insomnia and heart rate variability of health care workers at the time of COVID-19 pandemic: A randomized controlled trial. Sleep Breath. 2022, 26, 1–8. [Google Scholar] [CrossRef]
- Soldatos, C.R.; Dikeos, D.G.; Paparrigopoulos, T.J. Athens Insomnia Scale: Validation of an instrument based on ICD-10 criteria. J. Psychosom. Res. 2000, 48, 555–560. [Google Scholar] [CrossRef]
- Snyder, C.R.; Harris, C.; Anderson, J.R.; Holleran, S.A.; Irving, L.M.; Sigmon, S.T.; Yoshinobu, L.; Gibb, J.; Langelle, C.; Harney, P. The will and the ways: Development and validation of an individual-differences measure of hope. J. Personal. Soc. Psychol. 1991, 60, 570–585. [Google Scholar] [CrossRef]
- Kroenke, K.; Spitzer, R.L. The PHQ-9: A New Depression Diagnostic and Severity Measure. Psychiatr. Ann. 2002, 32, 509–515. [Google Scholar] [CrossRef]
- Podsakoff, P.M.; MacKenzie, S.B.; Lee, J.-Y.; Podsakoff, N.P. Common method biases in behavioral research: A critical review of the literature and recommended remedies. J. Appl. Psychol. 2003, 88, 879–903. [Google Scholar] [CrossRef]
- Yalçın, I.; Can, N.; Çalışır, M.; Yalçın, S.; Çolak, B. Latent profile analysis of COVID-19 fear, depression, anxiety, stress, mindfulness, and resilience. Curr. Psychol. 2021, 41, 459–469. [Google Scholar] [CrossRef]
- Yao, Y.; Chen, J.; Dong, D.; Feng, Y.; Qiao, Z. The Relationship between Exercise and Mental Health Outcomes during the COVID-19 Pandemic: From the Perspective of Hope. Int. J. Environ. Res. Public Health 2022, 19, 4090. [Google Scholar] [CrossRef]
- Ni, M.Y.; Yang, L.; Leung, C.M.C.; Li, N.; Yao, X.I.; Wang, Y.; Leung, G.M.; Cowling, B.J.; Liao, Q. Mental Health, Risk Factors, and Social Media Use During the COVID-19 Epidemic and Cordon Sanitaire Among the Community and Health Professionals in Wuhan, China: Cross-Sectional Survey. JMIR Ment. Health 2020, 7, e19009. [Google Scholar] [CrossRef] [PubMed]
- Sorge, A.; Bassanini, F.; Zucca, J.; Saita, E. “Fear can hold you, hope can set you free”. Analysis of Italian prisoner narrative experience of the COVID-19 pandemic. Int. J. Prison. Health 2021, 17, 406–423. [Google Scholar] [CrossRef] [PubMed]
- Ding, Y.; Xu, J.; Huang, S.; Li, P.; Lu, C.; Xie, S. Risk Perception and Depression in Public Health Crises: Evidence from the COVID-19 Crisis in China. Int. J. Environ. Res. Public Health 2020, 17, 5728. [Google Scholar] [CrossRef] [PubMed]
- Ariyo, J.O.; Akinnawo, E.O.; Akpunne, B.C.; Kumuyi, D.O.; Onisile, D.F. An Investigation of Associations and Incidence of Anxiety, Depression, Perceived Vulnerability to Diseases, and Fear of COVID-19 Among Nigerian Health Care Workers. Arch. Pediatr. Infect. Dis. 2021, 10, e114746. [Google Scholar] [CrossRef]
- Huynh, G.; Nguyen, H.V.; Vo, L.Y.; Le, N.T.; Nguyen, H.T.N. Assessment of Insomnia and Associated Factors Among Patients Who Have Recovered from COVID-19 in Vietnam. Patient Prefer. Adher. 2022, 16, 1637–1647. [Google Scholar] [CrossRef]
- Holloway, K.; Bhullar, N.; Schutte, N.S. A latent profile analysis of dispositional hope and defense styles. Pers. Individ. Differ. 2017, 114, 151–154. [Google Scholar] [CrossRef]
- Snyder, C.R.; Ilardi, S.S.; Cheavens, J.; Michael, S.T.; Yamhure, L.; Sympson, S. The Role of Hope in Cognitive-Behavior Therapies. Cogn. Ther. Res. 2000, 24, 747–762. [Google Scholar] [CrossRef]
- Sekizawa, Y.; Hashimoto, S.; Denda, K.; Ochi, S.; So, M. Association between COVID-19 vaccine hesitancy and generalized trust, depression, generalized anxiety, and fear of COVID-19. BMC Public Health 2022, 22, 1–17. [Google Scholar] [CrossRef]
- Irwin, M.R.; Piber, D. Insomnia and inflammation: A two hit model of depression risk and prevention. World Psychiatry 2018, 17, 359–361. [Google Scholar] [CrossRef]
- Leerssen, J.; Foster-Dingley, J.C.; Lakbila-Kamal, O.; Dekkers, L.M.S.; Albers, A.C.W.; Ikelaar, S.L.C.; Maksimovic, T.; Wassing, R.; Houtman, S.J.; Bresser, T.; et al. Internet-guided cognitive, behavioral and chronobiological interventions in depression-prone insomnia subtypes: Protocol of a randomized controlled prevention trial. BMC Psychiatry 2020, 20, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Papagiouvanni, I.; Kotoulas, S.; Vettas, C.; Sourla, E.; Pataka, A. Sleep During the COVID-19 Pandemic. Curr. Psychiatry Rep. 2022, 24, 635–643. [Google Scholar] [CrossRef] [PubMed]
- Lindsay, J.A.B.; McGowan, N.M.; King, N.; Rivera, D.; Li, M.; Byun, J.; Cunningham, S.; Saunders, K.E.A.; Duffy, A. Psychological predictors of insomnia, anxiety and depression in university students: Potential prevention targets. BJPsych Open 2022, 8, e86. [Google Scholar] [CrossRef] [PubMed]
- Chadwick, A.E.; Zoccola, P.M.; Figueroa, W.S.; Rabideau, E.M. Communication and Stress: Effects of Hope Evocation and Rumination Messages on Heart Rate, Anxiety, and Emotions After a Stressor. Health Commun. 2016, 31, 1447–1459. [Google Scholar] [CrossRef] [PubMed]
- Lauridsen, S.; Nielsen, M.B.D.; Kusier, A.O.; Cloos, C.; Jensen, M.P.; Andersen, S.; Thygesen, L.C.; Folker, A.P. Implementing a peer-to-peer, self-management intervention for young people with depression and anxiety in Denmark. BMC Psychol. 2022, 10, 1–13. [Google Scholar] [CrossRef]
- Bakioğlu, F.; Korkmaz, O.; Ercan, H. Fear of COVID-19 and Positivity: Mediating Role of Intolerance of Uncertainty, Depression, Anxiety, and Stress. Int. J. Ment. Health Addict. 2020, 19, 2369–2382. [Google Scholar] [CrossRef]
- Yıldırım, M.; Güler, A. Coronavirus anxiety, fear of COVID-19, hope and resilience in healthcare workers: A moderated mediation model study. Health Psychol. Rep. 2021, 9, 388–397. [Google Scholar] [CrossRef]


| Variables | With Depressive Symptoms (n = 1061) | Without Depressive Symptoms (n = 1392) | t |
|---|---|---|---|
| Fear of COVID-19 | 17.19 ±6.22 | 14.62 ± 5.85 | −10.47 *** |
| Insomnia | 7.06 ± 3.48 | 3.64 ± 2.56 | −26.95 *** |
| Hope | 2.62 ± 0.46 | 2.97 ± 0.48 | 18.38 *** |
| M ± SD | 1 | 2 | 3 | 4 | 5 | 6 | |
|---|---|---|---|---|---|---|---|
| 1 Gender | —— | —— | |||||
| 2 Age | 18.13 ± 0.774 | −0.050 * | —— | ||||
| 3 Fear of COVID-19 | 15.73 ± 6.14 | 0.155 ** | 0.000 | 0.883 | |||
| 4 Insomnia | 5.12 ± 3.44 | 0.068 ** | 0.001 | 0.170 ** | 0.800 | ||
| 5 Hope | 2.82 ± 0.50 | −0.024 | 0.045 * | −0.153 ** | −0.339 ** | 0.883 | |
| 6 Depression | 4.61 ±4.22 | 0.075 ** | −0.012 | 0.246 ** | 0.601 ** | −0.458 ** | 0.875 |
| Depression (First Step) | Insomnia (Second Step) | Depression (Third Step) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| β | t | 95% CI | β | T | 95% CI | β | t | 95% CI | |
| Gender | 0.240 | 1.562 | [−0.061, 0.540] | 0.284 | 2.160 | [0.026, 0.541] | 0.059 | 0.461 | [−0.193, 0.312] |
| Age | 0.042 | 0.429 | [−0.150, 0.234] | 0.111 | 1.319 | [−0.054, 0.275] | −0.028 | −0.344 | [−0.190, 0.133] |
| Fear of COVID-19 | 0.365 | 5.553 | [0.236, 0.494] | 0.333 | 5.906 | [0.222, 0.443] | 0.154 | 2.769 | [0.045, 0.263] |
| Hope | −2.288 | −6.296 | [−3.001, −1.576] | −0.707 | −2.272 | [−1.318, −0.097] | −1.839 | −6.023 | [−2.438, −1.240] |
| Insomnia | 0.635 | 32.067 | [0.596, 0.674] | ||||||
| Fear of COVID-19 *Hope | −0.093 | −4.066 | [−0.137, −0.048] | −0.095 | −4.841 | [−0.133, −0.056] | −0.033 | −1.699 | [−0.070, 0.005] |
| R2 | 0.233 | 0.130 | 0.460 | ||||||
| F | 148.544 | 72.995 | 347.130 | ||||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yao, Y.; Lin, M.; Ni, J.; Ni, J. Hope Buffers the Effect of Fear of COVID-19 on Depression among College Students: Insomnia as a Mediator. Int. J. Environ. Res. Public Health 2023, 20, 3245. https://doi.org/10.3390/ijerph20043245
Yao Y, Lin M, Ni J, Ni J. Hope Buffers the Effect of Fear of COVID-19 on Depression among College Students: Insomnia as a Mediator. International Journal of Environmental Research and Public Health. 2023; 20(4):3245. https://doi.org/10.3390/ijerph20043245
Chicago/Turabian StyleYao, Yingying, Min Lin, Jianchao Ni, and Jing Ni. 2023. "Hope Buffers the Effect of Fear of COVID-19 on Depression among College Students: Insomnia as a Mediator" International Journal of Environmental Research and Public Health 20, no. 4: 3245. https://doi.org/10.3390/ijerph20043245
APA StyleYao, Y., Lin, M., Ni, J., & Ni, J. (2023). Hope Buffers the Effect of Fear of COVID-19 on Depression among College Students: Insomnia as a Mediator. International Journal of Environmental Research and Public Health, 20(4), 3245. https://doi.org/10.3390/ijerph20043245






