Effects of Live Music on the Perception of Noise in the SICU/PICU: A Patient, Caregiver, and Medical Staff Environmental Study
Abstract
1. Introduction
1.1. Background
1.2. Environments
1.3. Working Definition of Noise
1.4. Music in the PICU and SICU
1.5. Pain
1.6. Music Therapy
1.7. Environmental Music Therapy
1.8. Current Study
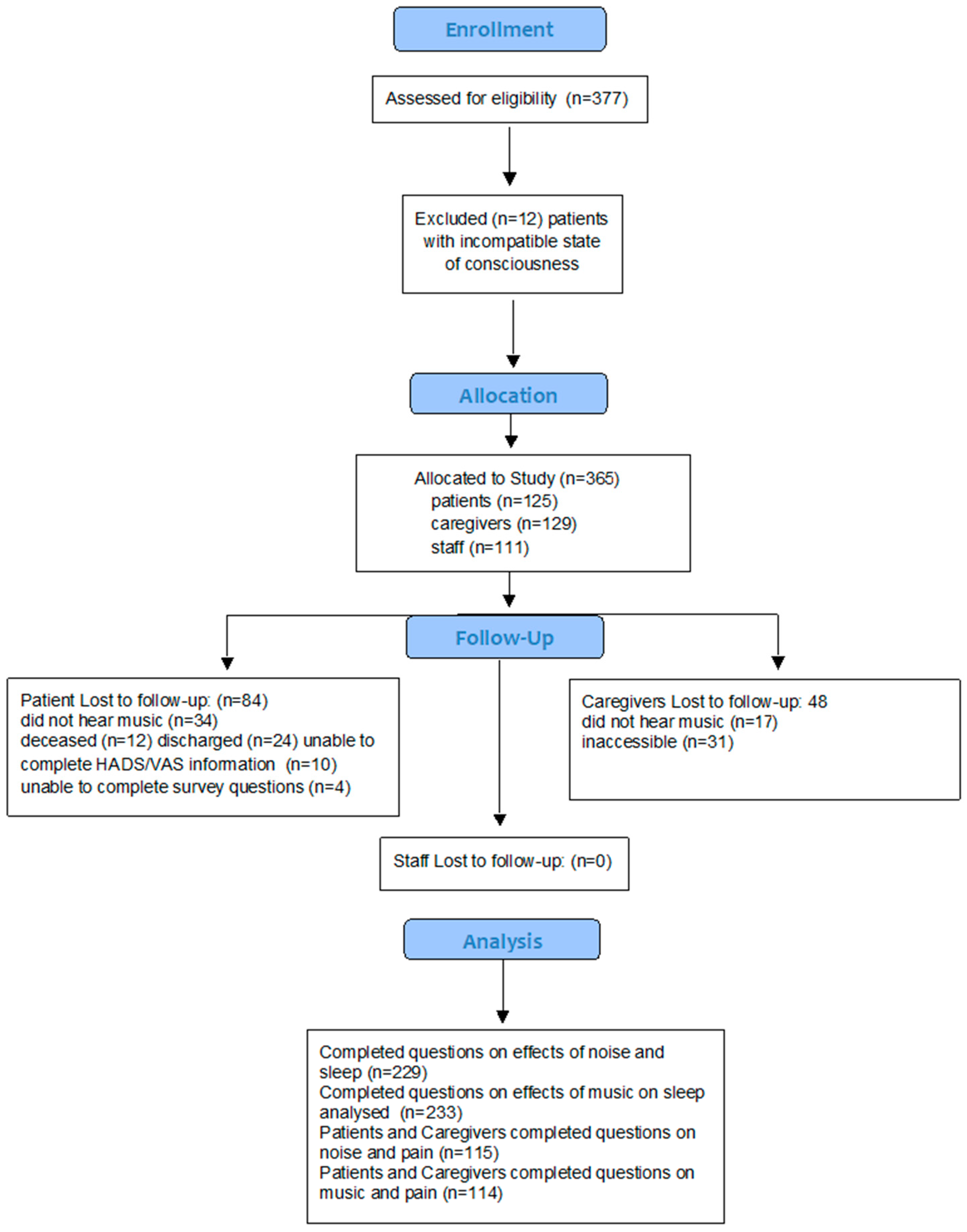
2. Methodology
2.1. Patient and Caregiver Population
2.2. Staff Population
2.3. Statistical Methods
2.4. Results
2.5. Effects of Noise and Music on Sleep and Pain
3. Discussion: Music’s Effect
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| PATIENTS | CAREGIVERS |
|---|---|
| Does noise in the SICU interfere with rest? 1–10 | Question 1: Does noise in the SICU interfere with rest? 1–10 |
| Does noise in the SICU interfere with sleep? 1–10 | Question 2: Does noise in the SICU interfere with sleep? |
| Does noise interfere with family and other support interactions? 1–10 | Question 3: Does noise interfere with family interactions and other supportive interactions? 1–10 |
| Does the noise in the unit impact your impression of the care you receive? 1–10 | Question 4: Does the noise in the unit impact your impression of the care the patient receives? of the general care? of the medical care? |
| Does the noise in the unit impact your impression of the general care? 1–10 | |
| Does the noise in the unit impact your impression of the medical care? 1–10 | |
| Who is the least considerate of the impact of voice noise on you? Open text | Question 5: Who is the least considerate of the impact of voice noise on you? Open text |
| Are the staff responsive to your requests to try and decrease noise? 1–10 | Question 6: Are staff responsive to your requests to try and decrease noise? 1–10 |
| Does the loudness of the noise affect your perception of staff? 1–10 | Question 7: Does the loudness of the noise affect your perception of staff? 1–10 |
| How bothered are you by the sound of the vents? 1–10 | Question 8: How bothered are you by the sound of the Vents, IVACS, Monitor Alarms, Voice Noise, Adjacent Patient Noise (Voice, Music or TV), Sound of Procedure Noise? 1–10 |
| How bothered are you by the sound of the IVACS? 1–10 | |
| How bothered are you by the sound of the Monitor alarms? 1–10 | |
| How bothered are you by the sound of Voice noise? 1–10 | |
| How bothered are you by Adjacent patient noise (music or tv)? 1–10 | |
| How bothered are you by the sound of Procedure noise? 1–10 | |
| Does noise in the SICU affect your level of tiredness? 1–10 | |
| Has noise ever interfered with your willingness to sign a consent form for a procedure? 1–10 | Question 9: Has noise ever interfered with your willingness to sign a consent form for a procedure? 1–10 |
| How much does tiredness impact pain of minor procedures? 1–10 | Question 10: How much do you think noise impacts the pain of minor procedures (IV lines and blood draws) 1–10/Open text |
| How much does tiredness impact the pain of the following major procedures: | |
| Central Lines 1–10 | Question 11: How much do you think noise impacts pain of the following major procedures: Central lines, Chest tubes, Procedure involving the staff sterile prepping and draping? 1–10/Open text |
| Chest tubes 1–10 | |
| Procedures involving the staff (sterile prepping and draping) 1–10 | |
| Were you taught any relaxation techniques before your SICU stay? If yes, which technique? Open text | Question 12: Were you taught any relaxation techniques before you SICU stay? Yes-no/open text |
| Question 13: Were you taught any relaxation techniques during your SICU stay? Yes-no/open text | |
| Have you or family members developed any relaxation technique on your own during your SICU stay? If yes, name of technique; Open text | Question 14: Have you or your family members developed any relaxation techniques on your own during your SICU stay? Yes-no/open text |
| What are your ideas for noise reduction and improved relaxation in the SICU? Open text | Question 15: What are your ideas for noise reduction and improved relaxation in the SICU? Open text |
| STAFF | |
| What percent of patients complain about the noise in the SICU? 0–100% | Do patients seem more restless or combative when the SICU is noisy? 0–10 (never–always) |
| What percent of family members complain about the noise in the SICU? 0–100% | Do you notice any influences upon treatment due to noise? 0–10 (never–always) |
| How often do patients and families request attempts at noise reduction? 0–10 (never–endlessly) | Is there any increased refusal to sign consents when the unit is noisy? 0–10 (never–always) |
| Please rate the following according to levels of complaints 0–10 (never-sometimes-often-always) | Do you think noise reduction affects outcome in the SICU? 0–10 (never–always) |
| Vents IVACS | Do you think it affects patient and family interaction with staff? 0–10 (never–always) |
| Monitor Alarms Voice Noise | Do you think noise reduction affects outcome in the SICU? 0–10 (never–always) |
| Adjacent patient noise Procedure noise | Do you think noise affects patient and family interaction with staff? 0–10 (never–always) |
References
- Oleksy, A.J.; Schlesinger, J.J. What’s all that noise—Improving the hospital soundscape. J. Clin. Monit. Comput. 2018, 33, 557–562. [Google Scholar] [CrossRef]
- Elliott, R.; McKinley, S.; Cistulli, P. The quality and duration of sleep in the intensive care setting: An integrative review. Int. J. Nurs. Stud. 2011, 48, 384–400. [Google Scholar] [CrossRef]
- Waye, K.P.; Elmenhorst, E.-M.; Croy, I.; Pedersen, E. Improvement of intensive care unit sound environment and analyses of consequences on sleep: An experimental study. Sleep Med. 2013, 14, 1334–1340. [Google Scholar] [CrossRef]
- Tembo, A.C.; Parker, V.; Higgins, I. The experience of sleep deprivation in intensive care patients: Findings from a larger hermeneutic phenomenological study. Intensive Crit. Care Nurs. 2013, 29, 310–316. [Google Scholar] [CrossRef]
- Honarmand, K.; Rafay, H.; Le, J.; Mohan, S.; Rochwerg, B.; Devlin, J.W.; Skrobik, Y.; Weinhouse, G.L.; Drouot, X.; Watson, P.L.; et al. A Systematic Review of Risk Factors for Sleep Disruption in Critically Ill Adults. Crit. Care Med. 2020, 48, 1066–1074. [Google Scholar] [CrossRef]
- Delaney, L.; Litton, E.; Van Haren, F. The effectiveness of noise interventions in the ICU. Curr. Opin. Anaesthesiol. 2019, 32, 144–149. [Google Scholar] [CrossRef]
- Johansson, L.; Bergbom, I.; Waye, K.P.; Ryherd, E.; Lindahl, B. The sound environment in an ICU patient room—A content analysis of sound levels and patient experiences. Intensive Crit. Care Nurs. 2012, 28, 269–279. [Google Scholar] [CrossRef]
- Kebapcı, A.; Güner, P. “Noise Factory”: A qualitative study exploring healthcare providers’ perceptions of noise in the intensive care unit. Intensive Crit. Care Nurs. 2020, 63, 102975. [Google Scholar] [CrossRef]
- Berglund, B. Guidelines for Community Noise; Institute of Environmental Epidemiology, Ministry of the Environment: New York, NY, USA, 2000. [Google Scholar]
- Khademi, G.; Roudi, M.; Farhat, A.S.; Shahabian, M. Noise Pollution in Intensive Care Units and Emergency Wards. Iran J. Otorhinolaryngol. 2011, 23, 141–148. [Google Scholar] [CrossRef]
- Lawson, N.; Thompson, K.; Saunders, G.; Saiz, J.; Richardson, J.; Brown, D.; Ince, N.; Caldwell, M.; Pope, D. Sound Intensity and Noise Evaluation in a Critical Care Unit. Am. J. Crit. Care 2010, 19, e88–e98. [Google Scholar] [CrossRef]
- Pugh, R.; Jones, C.; Griffiths, R.D. The impact of noise in the intensive care unit. In Intensive Care Medicine; Vincent, J.L., Ed.; Springer Science: New York, NY, USA, 2007; pp. 942–949. [Google Scholar]
- Churchill, W. London England, House of Lords Speech to Parliament October 28, 1943. Available online: https://www.forbes.com/quotes/10298/ (accessed on 10 December 2022).
- Hsu, T.E.; Ryherd, K.; Waye, P.; Ackerman, J. Noise pollution in hospitals: Impacts on patients. J. Clin. Out. Mgmt. 2012, 19, 301–309. [Google Scholar]
- McGain, F.; Naylor, C. Environmental sustainability in hospitals–a systematic review and research agenda. J. Health Serv. Res. Policy 2014, 19, 245–252. [Google Scholar] [CrossRef]
- Shield, B.; Shiers, N.; Glanville, R. The acoustic environment of inpatient hospital wards in the United Kingdom. J. Acoust. Soc. Am. 2016, 140, 2213–2224. [Google Scholar] [CrossRef]
- Walker, L.; Karl, C.A. The Hospital (Not So) Quiet Zone: Creating an Environment for Patient Satisfaction Through Noise Reduction Strategies. HERD Health Environ. Res. Des. J. 2019, 12, 197–202. [Google Scholar] [CrossRef] [PubMed]
- Nightingale, F. Nightingale, Notes on Nursing: What It Is, and What It Is Not; Lippincott, Williams & Wilkins: Philadelphia, PA, USA, 1992; ISBN 0-397-55007. [Google Scholar]
- Craik, K.H. The lived day of an individual: A person–environment perspective. In Person–Environment Psychology: New Directions and Perspectives; Walsh, W.B., Craik, K.H., Price, R.H., Eds.; Lawrence Erlbaum Associates Publishers: Mahwah, NJ, USA, 2000; pp. 233–266. [Google Scholar]
- Schneider, B.A.; Pichora-Fuller, K.M. Implications of perceptual deterioration for cognitive aging research. In The Handbook of Aging and Cognition; Craik, F.I.M., Salthouse, T.A., Eds.; Lawrence Erlbaum: Mahwah, NJ, USA, 2000; pp. 155–220. [Google Scholar]
- Gibson, J. Chapter XIV: The causes of deficient perception. In The Senses Considered as Perceptual Systems; Gibsonpp, J.J., Ed.; Houghton Mifflin: Boston, MA, USA, 1996; pp. 287–318. [Google Scholar]
- Hilton, B.A. Noise in acute patient care areas. Res. Nurs. Health 1985, 8, 283–291. [Google Scholar] [CrossRef]
- Belojevic, G.; Jakovljevic, B.; Slepcevic, V. Noise and mental performance: Personality attributes and noise sensitivity. Noise Health 2004, 6, 77–89. [Google Scholar]
- Löf, L.; Berggren, L.; Ahlström, G. Severely ill ICU patients recall of factual events and unreal experiences of hospital admission and ICU stay—3 and 12 months after discharge. Intensive Crit. Care Nurs. 2006, 22, 154–166. [Google Scholar] [CrossRef]
- Akansel, N.; Kaymakçi, S. Effects of intensive care unit noise on patients: A study on coronary artery bypass graft surgery patients. J. Clin. Nurs. 2008, 17, 1581–1590. [Google Scholar] [CrossRef]
- Granberg, A.; Engberg, I.B.; Lundberg, D. Patients’ experience of being critically ill or severely injured and cared for in an intensive care unit in relation to the ICU syndrome. Part I. Intensive Crit. Care Nurs. 1998, 14, 294–307. [Google Scholar] [CrossRef]
- Hohmann, L.; Bradt, J.; Stegemann, T.; Koelsch, S. Effects of music therapy and music-based interventions in the treatment of substance use disorders: A systematic review. PLoS ONE 2017, 12, e0187363. [Google Scholar] [CrossRef]
- Peng, C.S.; Baxter, K.; Lally, K.M. Music Intervention as a Tool in Improving Patient Experience in Palliative Care. Am. J. Hosp. Palliat. Med. 2018, 36, 45–49. [Google Scholar] [CrossRef] [PubMed]
- Chan, J.C.-H.; Chan, L.P.; Yeung, C.P.; Tang, T.W.; Mang, O.Y.; Lam, W.C. Effect of Music on Patient Experience during Intravitreal Injection. J. Ophthalmol. 2020, 2020, 9120235. [Google Scholar] [CrossRef] [PubMed]
- Music and Health. Harvard Health. Available online: https://www.health.harvard.edu/newsletter_article/music-and-health (accessed on 5 November 2022).
- Richard-Lalonde, M.; Gélinas, C.; Boitor, M.; Gosselin, E.; Feeley, N.; Cossette, S.; Chlan, L.L. The Effect of Music on Pain in the Adult Intensive Care Unit: A Systematic Review of Randomized Controlled Trials. J. Pain Symptom Manag. 2019, 59, 1304–1319.e6. [Google Scholar] [CrossRef]
- Guerra, G.G.; Joffe, A.; Sheppard, C.; Hewson, K.; Dinu, I.A.; De Caen, A.; Jou, H.; Hartling, L.; Vohra, S. The Canadian Critical Care Trials Group Music Use for Sedation in Critically ill Children (MUSiCC trial): Study protocol for a pilot randomized controlled trial. Pilot Feasibility Stud. 2020, 6, 31–38. [Google Scholar] [CrossRef] [PubMed]
- Bush, M.H.I.; LaGasse, A.B.; Collier, L.E.H.; Gettis, D.M.A.; Walson, K. Effect of Live Versus Recorded Music on Children Receiving Mechanical Ventilation and Sedation. Am. J. Crit. Care 2021, 30, 343–349. [Google Scholar] [CrossRef] [PubMed]
- Cousin, V.L.; Colau, H.; Barcos-Munoz, F.; Rimensberger, P.C.; Polito, A. Parents’ Views with Music Therapy in the Pediatric Intensive Care Unit: A Retrospective Cohort Study. Children 2022, 9, 958. [Google Scholar] [CrossRef]
- Umbrello, M.; Sorrenti, T.; Mistraletti, G.; Formenti, P.; Chiumello, D.; Terzoni, S. Music therapy reduces stress and anxiety in critically ill patients: A systematic review of randomized clinical trials. Minerva Anestesiol. 2019, 85, 886–898. [Google Scholar] [CrossRef]
- Kakar, E.; Billar, R.J.; van Rosmalen, J.; Klimek, M.; Takkenberg, J.J.M.; Jeekel, J. Music intervention to relieve anxiety and pain in adults undergoing cardiac surgery: A systematic review and meta-analysis. Open Heart 2021, 8, e001474. [Google Scholar] [CrossRef]
- So, H.M.; Chan, D.S.K. Perception of stressors by patients and nurses of critical care units in Hong Kong. Int. J. Nurs. Stud. 2004, 41, 77–84. [Google Scholar] [CrossRef]
- Maidl-Putz, C.; McAndrew, N.S.; Leske, J.S. Noise in the ICU. Nurs. Crit. Care 2014, 9, 29–35. [Google Scholar] [CrossRef]
- Gabor, J.Y.; Cooper, A.B.; Crombach, S.A.; Lee, B.; Kadikar, N.; Bettger, H.E.; Hanly, P.J. Contribution of the Intensive Care Unit Environment to Sleep Disruption in Mechanically Ventilated Patients and Healthy Subjects. Am. J. Respir. Crit. Care Med. 2003, 167, 708–715. [Google Scholar] [CrossRef] [PubMed]
- Russell, S. An exploratory study of patients’ perceptions, memories and experiences of an intensive care unit. J. Adv. Nurs. 1999, 29, 783–791. [Google Scholar] [CrossRef] [PubMed]
- Green, A. An exploratory study of patients’ memory recall of their stay in an adult intensive therapy unit. Intensive Crit. Care Nurs. 1996, 12, 131–137. [Google Scholar] [CrossRef] [PubMed]
- Horsten, S.; Reinke, L.; Absalom, A.; Tulleken, J. Systematic review of the effects of intensive-care-unit noise on sleep of healthy subjects and the critically ill. Br. J. Anaesth. 2018, 120, 443–452. [Google Scholar] [CrossRef] [PubMed]
- Novaes, M.A.F.P.; Knobel, E.; Bork, A.M.; Pavão, O.F.; Nogueira-Martins, L.A.; Ferraz, M.B. Stressors in ICU: Perception of the patient, relatives and health care team. Intensive Care Med. 1999, 25, 1421–1426. [Google Scholar] [CrossRef]
- Cochran, J.; Ganong, L.H. A comparison of nurses’ and patients’ perceptions of intensive care unit stressors. J. Adv. Nurs. 1989, 14, 1038–1043. [Google Scholar] [CrossRef]
- Cornock, M.A. Stress and the intensive care patient: Perceptions of patients and nurses. J. Adv. Nurs. 1998, 27, 518–527. [Google Scholar] [CrossRef]
- O’Callaghan, C.; Magill, L. Effect of music therapy on oncologic staff bystanders: A substantive grounded theory. Palliat. Support. Care 2009, 7, 219–228. [Google Scholar] [CrossRef]
- Wang, Z.; Downs, B.; Farell, A.; Cook, K.; Hourihan, P.; McCreery, S. Role of a Service Corridor in ICU Noise Control, Staff Stress, and Staff Satisfaction: Environmental Research of an Academic Medical Center. HERD Health Environ. Res. Des. J. 2013, 6, 80–94. [Google Scholar] [CrossRef]
- Rossetti, A. Environmental Music Therapy (EMT): Music’s Contribution to Changing Hospital Atmospheres and Perceptions of Environments. Music Med. 2020, 12, 130–141. [Google Scholar] [CrossRef]
- Shertzer, K.E.; Keck, J.F. Music and the PACU environment. J. PeriAnesthesia Nurs. 2001, 16, 90–102. [Google Scholar] [CrossRef] [PubMed]
- Loewy, J.V. Efficacy of Pain Management: Integration versus Distraction. Music Med. 2019, 11, 55–63. [Google Scholar] [CrossRef]
- Loewy, J.; MacGregor, B.; Richards, K.; Rodriguez, J. Music therapy in pediatric pain management: Assessing and attending to the sounds of hurt, fear and anxiety. In Music Therapy and Pediatric Pain; Loewy, J., Ed.; Jeffrey Books: Malvern, NJ, USA, 1997. [Google Scholar]
- Chetta, H.D. The Effect of Music and Desensitization on Preoperative Anxiety in Children. J. Music Ther. 1981, 18, 74–87. [Google Scholar] [CrossRef] [PubMed]
- Robb, S.; Nichols, R.J.; Rutan, R.L.; Bishop, B.L.; Parker, J.C. The Effects of Music Assisted Relaxation on Preoperative Anxiety. J. Music Ther. 1995, 32, 2–21. [Google Scholar] [CrossRef]
- Edwards, J. Music Therapy for Children with Severe Burn Injury. Music Ther. Perspect. 1998, 16, 21–26. [Google Scholar] [CrossRef]
- Rossetti, A. Towards Prescribed Music in Clinical Contexts: More Than Words. Music Med. 2014, 6, 70–77. [Google Scholar] [CrossRef]
- Joint Commission–Health Equity. Available online: https://www.jointcommission.org/resources/patient-safety-topics/health-equity#t=_Tab_StandardsFAQs&sort=relevancy (accessed on 13 December 2021).
- Conrad, C.; Niess, H.; Jauch, K.-W.; Bruns, C.J.; Hartl, W.H.; Welker, L. Overture for growth hormone: Requiem for interleukin-6? Crit. Care Med. 2007, 35, 2709–2713. [Google Scholar] [CrossRef]
- Loewy, J.; Hallan, C.; Friedman, E.; Martinez, C. Sleep/Sedation in Children Undergoing EEG Testing: A Comparison of Chloral Hydrate and Music Therapy. J. PeriAnesthesia Nurs. 2005, 20, 323–331. [Google Scholar] [CrossRef]
- Loewy, J. NICU music therapy: Song of kin as critical lullaby in research and practice. Ann. N. Y. Acad. Sci. 2015, 1337, 178–185. [Google Scholar] [CrossRef]
- Chlan, L.L.; Weinert, C.R.; Heiderscheit, A.; Tracy, M.F.; Skaar, D.J.; Guttormson, J.L.; Savik, K. Effects of Patient-Directed Music Intervention on Anxiety and Sedative Exposure in Critically Ill Patients Receiving Mechanical Ventilatory Support. JAMA 2013, 309, 2335–2344. [Google Scholar] [CrossRef]
- Good, M.; Anderson, G.C.; Ahn, S.; Cong, X.; Stanton-Hicks, M. Relaxation and music reduce pain following intestinal surgery. Res. Nurs. Health 2005, 28, 240–251. [Google Scholar] [CrossRef] [PubMed]
- Golino, A.J.; Leone, R.; Gollenberg, A.; Christopher, C.; Stanger, D.; Davis, T.M.; Meadows, A.; Zhang, Z.; Friesen, M.A. Impact of an Active Music Therapy Intervention on Intensive Care Patients. Am. J. Crit. Care 2019, 28, 48–55. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.; Choi, D.; Yeo, M.S.; Yoo, G.E.; Kim, S.J.; Na, S. Effects of Patient-Directed Interactive Music Therapy on Sleep Quality in Postoperative Elderly Patients: A Randomized-Controlled Trial. Nat. Sci. Sleep 2020, 12, 791–800. [Google Scholar] [CrossRef] [PubMed]
- Bradt, J.; Dileo, C.; Myers-Coffman, K.; Biondo, J. Music interventions for improving psychological and physical outcomes in people with cancer. Cochrane Database Syst. Rev. 2021, 10, 15–16. [Google Scholar] [CrossRef]
- Rossetti, A.; Chadha, M.; Torres, B.N.; Lee, J.K.; Hylton, D.; Loewy, J.V.; Harrison, L.B. The Impact of Music Therapy on Anxiety in Cancer Patients Undergoing Simulation for Radiation Therapy. Int. J. Radiat. Oncol. 2017, 99, 103–110. [Google Scholar] [CrossRef]
- Rodziewicz, T.L.; Houseman, B.; Hipskind, J.E. Medical Error Reduction and Prevention. [Updated 4 January 2022]. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2022. [Google Scholar]
- Stewart, K.; Schneider, S. E MT: The effects of music therapy on the sound environment in the NICU: A pilot study. In Music Therapy in the Neonatal Intensive Care Unit; Loewy, J.V., Ed.; Satchnote Press: New York, NY, USA, 2000; pp. 85–100. [Google Scholar]
- Schneider, S. Environmental Music Therapy: Life, death and the ICU. In Music Therapy at the End of Life; Dileo, C., Loewy, J.V., Eds.; Jeffrey Books: Cherry Hill, NJ, USA, 2005; pp. 219–225. [Google Scholar]
- Chestnut, M.; Duncan, M.; Gagnon, S.; Schreck, B. Music Meditation in the ICU. In Music Therapy at the End of Life; Dileo, C., Loewy, J.V., Eds.; Jeffrey Books: Cherry Hill, NJ, USA, 2005; pp. 219–228. [Google Scholar]
- Zhang, J.W.; Doherty, M.A.; Mahoney, J.F. Environmental Music in a Hospital Setting: Considerations of Music Therapists and Performing Musicians. Music Med. 2018, 10, 71. [Google Scholar] [CrossRef]
- Van Dokkum, H.; Rossetti, A.; Loewy, J. Music in the lobby: Listener and performer perspectives of a hospital Visiting Artists Series (VAS). Music Med. 2022, 14, 205–212. [Google Scholar] [CrossRef]
- Sutari, M.M.A.; Abdalrahim, M.S.; Hamdan-Mansour, A.M.; Ayasrah, S.M. Pain among mechanically ventilated patients in critical care units. J. Res. Med. Sci. 2014, 19, 726–732. [Google Scholar]
- Herr, K.; Coyne, P.J.; McCaffery, M.; Manworren, R.; Merkel, S. Pain Assessment in the Patient Unable to Self-Report: Position Statement with Clinical Practice Recommendations. Pain Manag. Nurs. 2011, 12, 230–250. [Google Scholar] [CrossRef]
| Entire Cohort (N = 233) | |||
|---|---|---|---|
| Participant Characteristics | |||
| Participant Age | Participant Gender | ||
| Patient Median (Range) | 58 (14–89) | Male 80 (34.3%) | Female 153 (65.7%) |
| PT Age Groups+ % | STF Age Groups+ % | CG Age Groups+ % | |
| 14–25 y | 5 (12.19%) | 4 (3.6%) | 7 (8.64%) |
| 26–48 y | 9 (21.95%) | 64 (57.65%) | 17 (20.98%) |
| 49–58 y | 7 (17.1%) | 37 (33.3%) | 47 (58%) |
| 59–64 y | 7 (17.1%) | 6 (5.4%) | 10 (12.34%) |
| 65–89 y | 13 (31.7%) | 0 (0%) | 0 (0%) |
| Patient Diagnosis | |||
| Oncology n = 9 Respiratory n =9 Hepatic n = 2 Circulatory n= 3 | Neurological n = 4 Gastrointestinal n = 10 | Surgical complications n = 2 Infectious n = 2 | |
| Patient place of origin | NYC Area 27 | Extended US 10 | Outside US 4 |
| Staff Characteristics | number n (%) | Staff Gender | |
| Male | Female | ||
| Physicians | n = 28 (25.2%) | 21 (81.1%) | 9 (18.9%) |
| Nurses | n = 57 (51.4%) | 8 (14.03%) | 49 (85.96%) |
| Nurse Managers | n = 2 (1.8%) | 0 (0%) | 2 (100%) |
| Physician Assistants | n = 3 (2.7%) | 2 (66.6%) | 1 (33.3%) |
| Support Staff | n = 17 (15.3%) | 6 (35.3%) | 11 (64.7%) |
| Students | n = 4 (3.6%) | 1 (25%) | 3 (75%) |
| Sleep | ||||
|---|---|---|---|---|
| No Music: Median (Interquartile Range) | Music: Median (Interquartile Range) | p-Value | Effect Size | |
| Total | 5.5 (4.5) | 7.0 (3.5) | <0.001 | 0.25 |
| Patients | 4.3 (5.0) | 6.0 (5.2) | 0.28 | 0.24 |
| Caregivers | 5.0 (5.5) | 5.0 (7.0) | 0.93 | 0.03 |
| Staff members | 6.0 (4.0) | 7.0 (2.0) | <0.001 | 0.76 |
| Pain | ||||
| No Music: Median (Interquartile range) | Music: Median (Interquartile range) | p-value | Effect size | |
| Total | 3.0 (5.0) | 4.7 (3.5) | 0.037 | 0.05 |
| Patients | 3.3 (4.9) | 4.7 (3.8) | 0.70 | 0.06 |
| Caregivers | 3.0 (5.0) | 5.0 (3.3) | 0.022 | 0.35 |
| Entries n = 112 Patients Identifying 1 Genre n = 4 (9.75%) Patient Preferred Music Genre n = 41 Patients Identifying Multiple Genres as Favorite Music n = 37 (90.25%) | |||||
|---|---|---|---|---|---|
| Classic rock | n = 9 | (8.03%) | Opera | n = 2 | (1.78%) |
| Blues | n= 3 | (2.68%) | 40′s big band | n = 2 | (1.78%) |
| Broadway | n = 2 | (1.78%) | Chinese pop | n = 1 | (1.12%) |
| Folk | n = 4 | (3.5%) | Asian Classical | n = 2 | (1.78%) |
| Country | n = 3 | (2.68%) | Kletzmer | n = 1 | (1.12%) |
| Soca | n = 1 | (1.12%) | Gospel | n = 5 | (4.46%) |
| Salsa | n = 5 | (4.46%) | Contemporary Devotional | n = 5 | (4.46%) |
| Latin | n =4 | (3.5%) | Reggae | n = 5 | (4.46%) |
| R&B | n = 3 | (3.5%) | New Age | n = 8 | (7.14%) |
| Jazz | n= 15 | (13.39%) | Classical | n = 17 | (15.2%) |
| Freestyle | n = 1 | (1.12%) | Freestyle | n = 1 | (1.12%) |
| Classic pop | n = 7 | (6.25%) | Current Pop | n = 4 | (3.5%) |
| Rap | n = 1 | (1.12%) | Hip Hop | n = 1 | (1.12%) |
| House | n = 1 | (1.12%) | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rossetti, A.; Loewy, J.; Chang-Lit, W.; van Dokkum, N.H.; Baumann, E.; Bouissou, G.; Mondanaro, J.; O’Connor, T.; Asch-Ortiz, G.; Mitaka, H. Effects of Live Music on the Perception of Noise in the SICU/PICU: A Patient, Caregiver, and Medical Staff Environmental Study. Int. J. Environ. Res. Public Health 2023, 20, 3499. https://doi.org/10.3390/ijerph20043499
Rossetti A, Loewy J, Chang-Lit W, van Dokkum NH, Baumann E, Bouissou G, Mondanaro J, O’Connor T, Asch-Ortiz G, Mitaka H. Effects of Live Music on the Perception of Noise in the SICU/PICU: A Patient, Caregiver, and Medical Staff Environmental Study. International Journal of Environmental Research and Public Health. 2023; 20(4):3499. https://doi.org/10.3390/ijerph20043499
Chicago/Turabian StyleRossetti, Andrew, Joanne Loewy, Wen Chang-Lit, Nienke H. van Dokkum, Erik Baumann, Gabrielle Bouissou, John Mondanaro, Todd O’Connor, Gabriela Asch-Ortiz, and Hayato Mitaka. 2023. "Effects of Live Music on the Perception of Noise in the SICU/PICU: A Patient, Caregiver, and Medical Staff Environmental Study" International Journal of Environmental Research and Public Health 20, no. 4: 3499. https://doi.org/10.3390/ijerph20043499
APA StyleRossetti, A., Loewy, J., Chang-Lit, W., van Dokkum, N. H., Baumann, E., Bouissou, G., Mondanaro, J., O’Connor, T., Asch-Ortiz, G., & Mitaka, H. (2023). Effects of Live Music on the Perception of Noise in the SICU/PICU: A Patient, Caregiver, and Medical Staff Environmental Study. International Journal of Environmental Research and Public Health, 20(4), 3499. https://doi.org/10.3390/ijerph20043499








