International Music Therapists’ Perceptions and Experiences in Telehealth Music Therapy Provision
Abstract
1. Introduction
Literature Review
2. Method
2.1. Purpose of Study
2.2. Research Questions
- What are the perceptions and clinical practice experiences of music therapy professionals from around the globe in providing Telehealth Music Therapy (TMT) services?
- What are the benefits and challenges of TMT, and what is needed to advance this practice?
- Does a music therapists’ primary theoretical orientation and work setting contribute to perceptions and trends associated with the successful implementation of TMT services?
2.3. Participants
2.4. Recruitment
2.5. Data
2.6. Data Analysis
2.6.1. The Wilcoxon Signed-Rank Test
2.6.2. Chi-Square Test of Independence
2.6.3. Correlation Analysis
2.6.4. Qualitative Analysis
3. Results
3.1. Participants
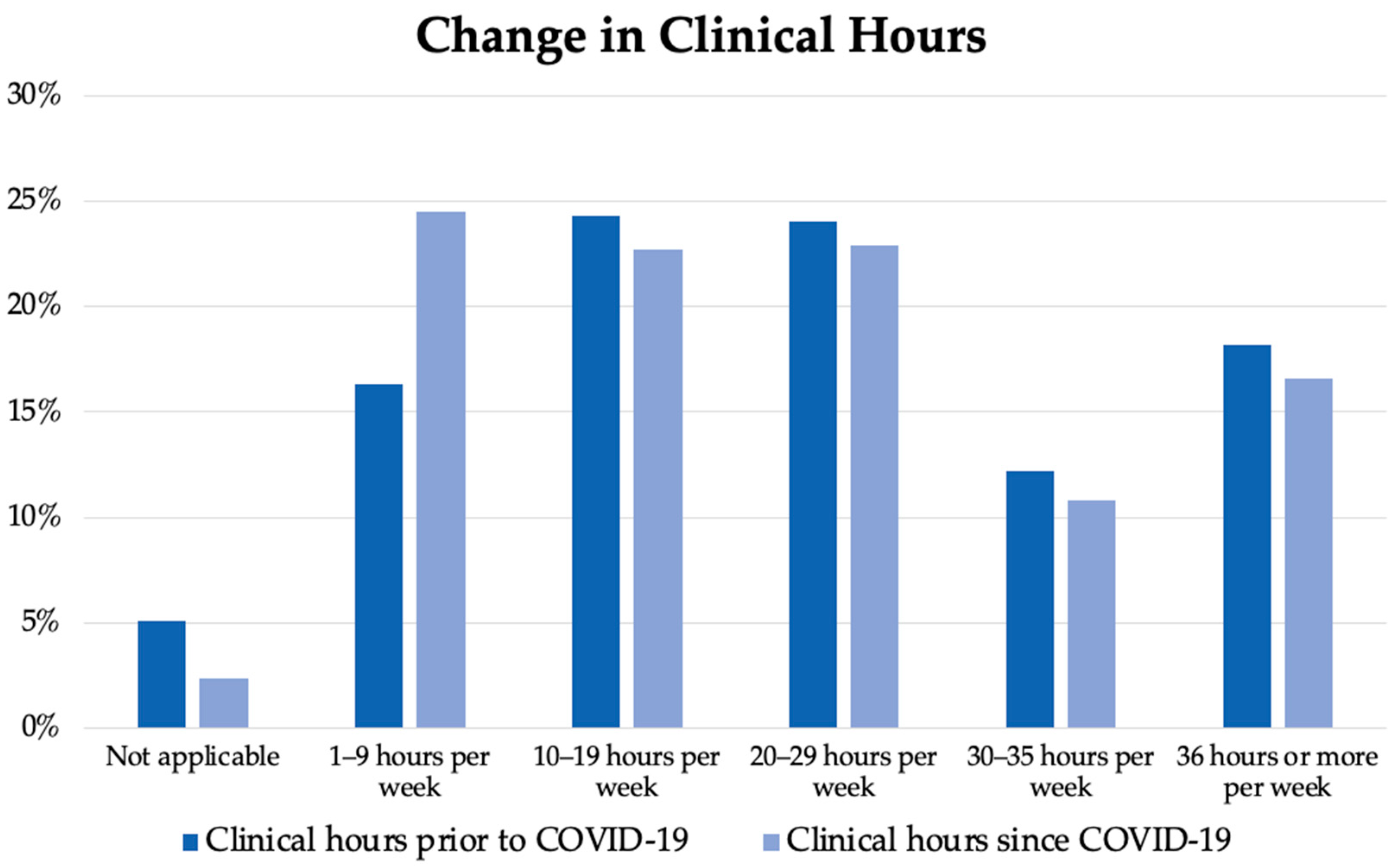
3.2. Clinical Practice
3.3. Telehealth Provision
3.3.1. Influence of Primary Theoretical Orientation and Work Setting
3.3.2. Telehealth Perceptions
3.4. Correlation Analysis
3.5. Qualitative Analysis
3.5.1. Training Taken by Music Therapists to Prepare for TMT Delivery
3.5.2. Benefits and Challenges for Clients/Consumers Engaging in a TMT Session
3.5.3. Benefits and Challenges for Music Therapists Engaging in TMT
4. Discussion
4.1. Limitations
4.2. Recommendations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- United States Department of Health Information Technology. What Is Telehealth? Frequently Asked Questions. 2023. Available online: https://www.healthit.gov/faq/what-telehealth-how-telehealth-different-telemedicine (accessed on 10 February 2023).
- Hyder, M.A.; Razzak, J. Telemedicine in the United States: An introduction for students and residents. J. Med. Internet Res. 2020, 22, e20839. [Google Scholar] [CrossRef] [PubMed]
- Peretti, A.; Amenta, F.; Tayebati, S.K.; Nittari, G.; Mahdi, S.S. Telerehabilitation: Review of the state-of-the-art and areas of application. JMIR Rehabil. Assist. Technol. 2017, 4, e7. [Google Scholar] [CrossRef] [PubMed]
- National Centre for Hearing Assessment and Management. Telehealth and EHDI Systems. 2023. Available online: https://www.infanthearing.org/telehealth/index.html (accessed on 20 February 2023).
- New England Journal of Medicine. What Is Telehealth? NEJM Catal. 2018, 4. Available online: https://catalyst.nejm.org/doi/full/10.1056/CAT.18.0268 (accessed on 10 February 2023).
- U.S. Department of Health and Human Services. What Is Telehealth? Information for Patients. 2022. Available online: https://telehealth.hhs.gov/patients/understanding-telehealth/ (accessed on 10 February 2023).
- Levy, C.E.; Spooner, H.; Lee, J.B.; Sonke, J.; Myers, K.; Snow, E. Telehealth-based creative arts therapy: Transforming mental health and rehabilitation care for rural veterans. Arts Psychother. 2018, 57, 20–26. [Google Scholar] [CrossRef]
- Spooner, H.; Lee, J.B.; Langston, D.G.; Sonke, J.; Myers, K.J.; Levy, C.E. Using distance technology to deliver the creative arts therapies to veterans: Case studies in art, dance/movement and music therapy. Arts Psychother. 2019, 62, 12–18. [Google Scholar] [CrossRef]
- Vaudreuil, R.; Langston, D.G.; Magee, W.; Betts, D.; Kass, S.; Levy, C. Implementing music therapy through telehealth: Considerations for military populations. Disabil. Rehabil. Assist. Technol. 2020, 17, 201–210. [Google Scholar] [CrossRef]
- Lightstone, A.J.; Bailey, S.K.; Voros, P. Collaborative music therapy via remote video technology to reduce a veteran’s symptoms of severe, chronic PTSD. Arts Health 2015, 7, 123–136. [Google Scholar] [CrossRef]
- Gooding, L.F.; Trainor, B. Working with parents in the neonatal intensive care unit: An analysis of music therapy practice in the United States of America. Arts Psychother. 2018, 59, 1–6. [Google Scholar] [CrossRef]
- Baker, F.; Krout, R. Songwriting via skype: An online music therapy intervention to enhance social skills in an adolescent diagnosed with Asperger’s Syndrome. Br. J. Music. Ther. 2009, 23, 3–14. [Google Scholar] [CrossRef]
- Baker, F.; Krout, R.E.; Magee, W. Therapeutic songwriting with clients/consumers in an e-health environment. In Music Technology in Therapeutic and Health Settings; Jessica Kingsley Publishers: London, UK, 2014; pp. 299–310. [Google Scholar]
- Fuller, A.M.; McLeod, R.G. The connected music therapy teleintervention approach (CoMTTA) and its application to family-centered programs for young children with hearing loss. Aust. J. Music Ther. 2019, 30, 12–30. [Google Scholar]
- Carvajal, M.A. Telehealth Music Therapy: Considerations and Changes During the COVID-19 Crisis. Ph.D. Thesis, The Florida State University, Tallahassee, FL, USA, 2020. [Google Scholar]
- American Music Therapy Association. AMTA Telehealth/Therapy Statement. 2020. Available online: https://www.musictherapy.org/music_therapy_in_telehealth/ (accessed on 16 April 2020).
- American Music Therapy Association. Telehealth Considerations and Resources. COVID-19 Resources. 2023. Available online: https://www.musictherapy.org/about/covid19_resources_telehealth_considerations_and_resources/ (accessed on 17 December 2022).
- Australian Music Therapy Association Inc. COVID 19 Member Resources. 2023. Available online: https://www.austmta.org.au/members-resources/covid-19/ (accessed on 15 January 2023).
- British Association for Music Therapy. Online & Phone Therapy. 2023. Available online: https://www.bamt.org/resources/covid-19-useful-information/online-and-phone-therapy (accessed on 15 January 2023).
- Gaddy, S.; Gallardo, R.; McCluskey, S.; Moore, L.; Peuser, A.; Rotert, R.; Stypulkoski, C.; LaGasse, A.B. COVID-19 and music therapists’ employment, service delivery, perceived stress, and hope: A descriptive study. Music Ther. Perspect. 2020, 38, 157–166. [Google Scholar] [CrossRef]
- Fay, M.; Register, D.; Sena Moore, K.; Simpson, J. Music Therapy during the COVID-19 Pandemic: Advocacy Highlights and Recommendations. 2020. Available online: https://www.musictherapy.org/music_therapy_during_the_covid-19_pandemic_advocacy_highlights_and_recommendations/ (accessed on 5 February 2023).
- Cole, L.P.; Henechowicz, T.L.; Kang, K.; Pranjić, M.; Richard, N.M.; Tian, G.L.; Hurt-Thaut, C. Neurologic music therapy via telehealth: A survey of clinician experiences, trends, and recommendations during the COVID-19 Pandemic. Front. Neurosci. 2021, 15, 347. [Google Scholar] [CrossRef] [PubMed]
- Agres, K.R.; Foubert, K.; Sridhar, S. Music therapy during COVID-19: Changes to the practice, use of technology, and what to carry forward in the future. Front. Psychol. 2021, 21, 143–161. [Google Scholar] [CrossRef] [PubMed]
- Baker, F.A.; Tamplin, J. Music therapy service provision via telehealth in response to COVID-19 restrictions: A survey of Australian practitioners and consumers. Aust. J. Music Ther. 2021, 32, 1–24. [Google Scholar]
- Wilhelm, L.; Wilhelm, K. Telehealth music therapy services in the United States with older adults: A descriptive study. Music Ther. Perspect. 2022, 40, 84–93. [Google Scholar] [CrossRef]
- Kantorová, L.; Kantor, J.; Hořejší, B.; Gilboa, A.; Svobodová, Z.; Lipský, M.; Marečková, J.; Klugar, M. Adaptation of music therapists’ practice to the outset of the COVID-19 pandemic—going virtual: A scoping review. Int. J. Environ. Res. Public Health 2021, 18, 5138. [Google Scholar] [CrossRef]
- Knott, D.; Block, S. Virtual music therapy: Developing new approaches to service delivery. Music Ther. Perspect. 2020, 38, 151–156. [Google Scholar] [CrossRef]
- Lam, K.; Lu, A.D.; Shi, Y.; Covinsky, K.E. Assessing telemedicine unreadiness among older adults in the United States during the COVID-19 pandemic. JAMA Intern. Med. 2020, 180, 1389–1391. [Google Scholar] [CrossRef]
- Clements-Cortés, A.; Mercadal-Brotons, M.; Alcântara Silva, T.R.; Vianna Moreira, S. Telehealth music therapy for persons with dementia and/or caregivers. Music Med. 2021, 13, 206–210. [Google Scholar] [CrossRef]
- Dassa, A.; Ray, K.; Clements-Cortés, A. Reflections on telehealth music therapy for persons with dementia in response to COVID-19. Music Med. 2021, 13, 201–205. [Google Scholar] [CrossRef]
- Cephas, A.S.; Sofield, S.; Millstein, A. Embracing technological possibilities in the telehealth delivery of interactive music therapy. Nord. J. Music Ther. 2022, 31, 214–227. [Google Scholar] [CrossRef] [PubMed]
- Devlin, K. Shaping the digital space: Exploring relationships in online music therapy session delivery. Nord. J. Music Ther. 2022, 31, 203–213. [Google Scholar] [CrossRef]
- Kern, P.; Tague, D.B. Students’ perception of online learning during COVID-19: A US-based music therapy survey. J. Music Ther. 2022, 59, 127–155. [Google Scholar] [CrossRef] [PubMed]
- Gooding, L.F.; Rushing, J.L. Clinical teletraining in music therapy: Two educators’ perspectives. Nord. J. Music Ther. 2022, 31, 244–258. [Google Scholar] [CrossRef]
- Curtis, S. Survey research. In Music Therapy Research, 3rd ed.; Wheeler, B., Murphy, K., Eds.; Barcelona Publishers: New Braunfels, TX, USA, 2016; pp. 322–330. [Google Scholar]
- Mehta, C.R.; Patel, N.R. IBM SPSS Exact Tests; IBM Corporation: Armonk, NY, USA, 2011. [Google Scholar]
- Bland, J.M.; Altman, D.G. Multiple significance tests: The Bonferroni method. BMJ 1995, 310, 170. [Google Scholar] [CrossRef]
- Zar, J.H. Spearman rank correlation. In Encyclopedia of Biostatistics; John Wiley & Sons: Hoboken, NJ, USA, 2005; Volume 7. [Google Scholar]
- Braun, V.; Clarke, V. Using thematic analysis in psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef]
- Williams, N.M.R.; Hurt-Thaut, C.; Thaut, M.H. Novel Screening Tool and Considerations for Music Therapists Serving Autistic Individuals via Telehealth: Qualitative Results from a Survey of Clinicians’ Experiences. J. Music. Ther. 2023, 59, 368–393. [Google Scholar] [CrossRef]
- Certification Board for Music Therapists. For Convenience & Safety, Music Therapists Indicate Telepractice Is Here to Stay. Available online: https://www.cbmt.org/for-convenience-safety-music-therapists-indicate-telepractice-is-here-to-stay/ (accessed on 25 June 2021).



| Variables | Mean (SD)/n (%) |
|---|---|
| Age | 41.3 (±12.8) |
| Gender | |
| Female | 473 (82.7%) |
| Male | 80 (14%) |
| Non-binary/non-conforming | 10 (1.7%) |
| Prefer not to say | 7 (1.2%) |
| Other | 2 (0.3%) |
| Country | |
| United States | 386 (67.5%) |
| Canada | 60 (10.5%) |
| Australia | 52 (9.1%) |
| Other | 74 (12.9%) |
| Country per region | |
| North America | 446 (78%) |
| Oceania | 57 (10%) |
| Europa | 33 (5.8%) |
| Asia | 26 (4.5%) |
| South America | 10 (1.7%) |
| Education level | |
| Bachelor’s degree | 186 (32.5%) |
| Master’s degree | 307 (53.7%) |
| Doctorate | 54 (9.4%) |
| Graduate Certificate | 12 (2.1%) |
| Other | 12 (2.1%) |
| Years practicing as a music therapist | |
| Less than 5 years | 146 (25.5%) |
| 5–10 years | 152 (26.6%) |
| 10–15 years | 93 (16.3%) |
| 15–20 years | 52 (9.1%) |
| More than 20 years | 129 (22.6%) |
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | |
|---|---|---|---|---|---|---|---|
| 1 | ||||||
| 0.138 ** <0.001 | 1 | |||||
| 0.211 ** <0.001 | 0.077 0.066 | 1 | ||||
| −0.101 * 0.016 | −0.122 ** 0.003 | −0.069 0.100 | 1 | |||
| −0.017 0.679 | 0.332 ** <0.001 | 0.089 * 0.034 | −0.188 ** <0.001 | 1 | ||
| 0.109 ** 0.009 | 0.428 ** <0.001 | 0.168 ** <0.001 | −0.148 ** <0.001 | 0.399 ** <0.001 | 1 | |
| −0.021 0.615 | 0.095 * 0.023 | −0.068 0.104 | 0.091 * 0.030 | −0.027 0.522 | −0.037 0.381 | 1 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Clements-Cortés, A.; Pranjić, M.; Knott, D.; Mercadal-Brotons, M.; Fuller, A.; Kelly, L.; Selvarajah, I.; Vaudreuil, R. International Music Therapists’ Perceptions and Experiences in Telehealth Music Therapy Provision. Int. J. Environ. Res. Public Health 2023, 20, 5580. https://doi.org/10.3390/ijerph20085580
Clements-Cortés A, Pranjić M, Knott D, Mercadal-Brotons M, Fuller A, Kelly L, Selvarajah I, Vaudreuil R. International Music Therapists’ Perceptions and Experiences in Telehealth Music Therapy Provision. International Journal of Environmental Research and Public Health. 2023; 20(8):5580. https://doi.org/10.3390/ijerph20085580
Chicago/Turabian StyleClements-Cortés, Amy, Marija Pranjić, David Knott, Melissa Mercadal-Brotons, Allison Fuller, Lisa Kelly, Indra Selvarajah, and Rebecca Vaudreuil. 2023. "International Music Therapists’ Perceptions and Experiences in Telehealth Music Therapy Provision" International Journal of Environmental Research and Public Health 20, no. 8: 5580. https://doi.org/10.3390/ijerph20085580
APA StyleClements-Cortés, A., Pranjić, M., Knott, D., Mercadal-Brotons, M., Fuller, A., Kelly, L., Selvarajah, I., & Vaudreuil, R. (2023). International Music Therapists’ Perceptions and Experiences in Telehealth Music Therapy Provision. International Journal of Environmental Research and Public Health, 20(8), 5580. https://doi.org/10.3390/ijerph20085580






