The Effect of Vinyasa Yoga Practice on the Well-Being of Breast-Cancer Patients during COVID-19 Pandemic
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patients Recruitment
2.2. Questionary Form
2.3. Intervention and Yoga Exercise Protocol
2.4. Statistic
2.5. Analysis of Multiple Answer Questions
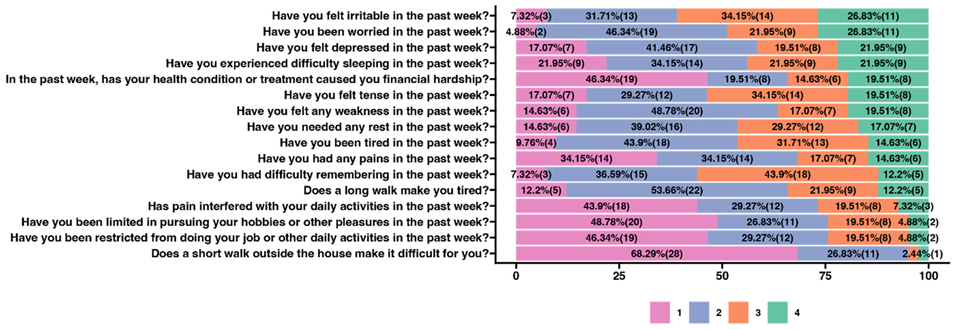
3. Results
4. Discussion
Limitations of the Study
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Rajarajeswaran, P.; Vishnupriya, R. Exercise in cancer. Indian J. Med. Paediatr. Oncol. 2009, 30, 61–70. [Google Scholar] [CrossRef] [PubMed]
- Cormie, P.; Atkinson, M.; Bucci, L.; Cust, A.; Eakin, E.; Hayes, S.; McCarthy, A.L.; Murnane, A.; Patchell, S.; Adams, D. Clinical Oncology Society of Australia position statement on exercise in cancer care. Med. J. Aust. 2018, 209, 184–187. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dighe, S.G.; Yan, L.; Mukherjee, S.; McGillicuddy, C.S.; Hulme, K.L.; Hochwald, S.N.; Yendamuri, S.; Bain, A.J.; Robillard, K.T.; Moysich, K.B.; et al. Clinical and Lifestyle-Related Prognostic Indicators among Esophageal Adenocarcinoma Patients Receiving Treatment at a Comprehensive Cancer Center. Cancers 2021, 13, 4653. [Google Scholar] [CrossRef] [PubMed]
- Danhauer, S.C.; Addington, E.L.; Sohl, S.; Chaoul, A.; Cohen, L. Review of yoga therapy during cancer treatment. Support. Care Cancer 2017, 25, 1357–1372. [Google Scholar] [CrossRef]
- Rock, C.L.; Thomson, C.A.; Sullivan, K.R.; Howe, C.L.; Kushi, L.H.; Caan, B.J.; Neuhouser, M.L.; Bandera, E.V.; Wang, Y.; Robien, K.; et al. American Cancer Society nutrition and physical activity guideline for cancer survivors. CA Cancer J. Clin. 2022, 72, 230–262. [Google Scholar] [CrossRef]
- Patel, A.V.; Friedenreich, C.M.; Moore, S.C.; Hayes, S.C.; Silver, J.K.; Campbell, K.L.; Winters-Stone, K.; Gerber, L.H.; George, S.M.; Fulton, J.E.; et al. American College of Sports Medicine Roundtable Report on Physical Activity, Sedentary Behavior, and Cancer Prevention and Control. Med. Sci. Sports Exerc. 2019, 51, 2391–2402. [Google Scholar] [CrossRef] [Green Version]
- Pedersen, B.K.; Saltin, B. Exercise as medicine–Evidence for prescribing exercise as therapy in 26 different chronic diseases. Scand. J. Med. Sci. Sports 2015, 25 (Suppl. 3), 1–72. [Google Scholar] [CrossRef] [Green Version]
- Avancini, A.; Sartori, G.; Gkountakos, A.; Casali, M.; Trestini, I.; Tregnago, D.; Bria, E.; Jones, L.W.; Milella, M.; Lanza, M.; et al. Physical Activity and Exercise in Lung Cancer Care: Will Promises Be Fulfilled? Oncologist 2020, 25, e555–e569. [Google Scholar] [CrossRef] [Green Version]
- Pudkasam, S.; Polman, R.; Pitcher, M.; Fisher, M.; Chinlumprasert, N.; Stojanovska, L.; Apostolopoulos, V. Physical activity and breast cancer survivors: Importance of adherence, motivational interviewing and psychological health. Maturitas 2018, 116, 66–72. [Google Scholar] [CrossRef] [Green Version]
- Mehnert, A.; Koranyi, S.; Philipp, R.; Scheffold, K.; Kriston, L.; Lehmann-Laue, A.; Engelmann, D.; Vehling, S.; Eisenecker, C.; Oechsle, K.; et al. Efficacy of the Managing Cancer and Living Meaningfully (CALM) individual psychotherapy for patients with advanced cancer: A single-blind randomized controlled trial. Psycho-Oncology 2020, 29, 1895–1904. [Google Scholar] [CrossRef]
- Mustian, K.M.; Alfano, C.M.; Heckler, C.; Kleckner, A.S.; Kleckner, I.R.; Leach, C.R.; Mohr, D.; Palesh, O.G.; Peppone, L.J.; Piper, B.F.; et al. Comparison of Pharmaceutical, Psychological, and Exercise Treatments for Cancer-Related Fatigue: A Meta-analysis. JAMA Oncol. 2017, 3, 961–968. [Google Scholar] [CrossRef]
- Breitbart, W.; Pessin, H.; Rosenfeld, B.; Applebaum, A.J.; Lichtenthal, W.G.; Li, Y.; Saracino, R.M.; Marziliano, A.M.; Ma, M.M.; Tobias, K.; et al. Individual meaning-centered psychotherapy for the treatment of psychological and existential distress: A randomized controlled trial in patients with advanced cancer. Cancer 2018, 124, 3231–3239. [Google Scholar] [CrossRef] [Green Version]
- Hilfiker, R.; Meichtry, A.; Eicher, M.; Balfe, L.N.; Knols, R.H.; Verra, M.L.; Taeymans, J. Exercise and other non-pharmaceutical interventions for cancer-related fatigue in patients during or after cancer treatment: A systematic review incorporating an indirect-comparisons meta-analysis. Br. J. Sports Med. 2017, 52, 651–658. [Google Scholar] [CrossRef] [Green Version]
- Charalambous, A.; Giannakopoulou, M.; Bozas, E.; Marcou, Y.; Kitsios, P.; Paikousis, L. Guided Imagery and Progressive Muscle Relaxation as a Cluster of Symptoms Management Intervention in Patients Receiving Chemotherapy: A Randomized Control Trial. PLoS ONE 2016, 11, e0156911. [Google Scholar] [CrossRef] [Green Version]
- Rossetti, A.; Chadha, M.; Torres, B.N.; Lee, J.K.; Hylton, D.; Loewy, J.V.; Harrison, L.B. The Impact of Music Therapy on Anxiety in Cancer Patients Undergoing Simulation for Radiation Therapy. Int. J. Radiat. Oncol. Biol. Phys. 2017, 99, 103–110. [Google Scholar] [CrossRef] [Green Version]
- Nardone, V.; Vinciguerra, C.; Correale, P.; Guida, C.; Tini, P.; Reginelli, A.; Cappabianca, S. Music therapy and radiation oncology: State of art and future directions. Complement. Ther. Clin. Pract. 2020, 39, 101124. [Google Scholar] [CrossRef]
- Pergolotti, M.; Ms, A.M.D.; Williams, G.R.; Bryant, A.L.; Ms, L.M.; Nyrop, K.A.; Ms, K.R.C.; Reeve, B.B.; Basch, E.; Muss, H.B. Older Adults with Cancer: A Randomized Controlled Trial of Occupational and Physical Therapy. J. Am. Geriatr. Soc. 2019, 67, 953–960. [Google Scholar] [CrossRef]
- Petruševičienė, D.; Surmaitiene, D.; Baltaduonienė, D.; Lendraitienė, E. Effect of Community-Based Occupational Therapy on Health-Related Quality of Life and Engagement in Meaningful Activities of Women with Breast Cancer. Occup. Ther. Int. 2018, 2018, 6798697. [Google Scholar] [CrossRef] [Green Version]
- Pergolotti, M.; Williams, G.; Campbell, C.; Munoz, L.A.; Muss, H.B. Occupational Therapy for Adults with Cancer: Why It Matters. Oncologist 2016, 21, 314–319. [Google Scholar] [CrossRef] [Green Version]
- Chakrabarty, J.; Vidyasagar, M.S.; Fernandes, D.; Mayya, S. Emotional aspects and pranayama in breast cancer patients undergoing radiation therapy: A randomized controlled trial. Asia-Pacific J. Oncol. Nurs. 2016, 3, 199–204. [Google Scholar] [CrossRef]
- Dhruva, A.; Miaskowski, C.; Abrams, D.; Acree, M.; Cooper, B.; Goodman, S.; Hecht, F. Yoga Breathing for Cancer Chemotherapy–Associated Symptoms and Quality of Life: Results of a Pilot Randomized Controlled Trial. J. Altern. Complement. Med. 2012, 18, 473–479. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- DiStasio, S.A. Integrating Yoga into Cancer Care. Clin. J. Oncol. Nurs. 2008, 12, 125–130. [Google Scholar] [CrossRef] [PubMed]
- Hanghøj, S.; Pappot, N.; Hjerming, M.; Taarnhøj, G.A.; Boisen, K.A.; Pappot, H. Experiences of Social Isolation During the COVID-19 Lockdown Among Adolescents and Young Adult Cancer Patients and Survivors. J. Adolesc. Young-Adult Oncol. 2021, 10, 142–147. [Google Scholar] [CrossRef] [PubMed]
- Lesser, I.A.; Nienhuis, C.P. The Impact of COVID-19 on Physical Activity Behavior and Well-Being of Canadians. Int. J. Environ. Res. Public Health 2020, 17, 3899. [Google Scholar] [CrossRef]
- Sallis, R.; Young, D.R.; Tartof, S.Y.; Sallis, J.F.; Sall, J.; Li, Q.; Smith, G.N.; Cohen, D.A. Physical inactivity is associated with a higher risk for severe COVID-19 outcomes: A study in 48 440 adult patients. Br. J. Sports Med. 2021, 55, 1099–1105. [Google Scholar] [CrossRef]
- Rzymski, P.; Rzymski, P.; Burzynski, B.; Jurys, T.; Knapik, M.; Rzymska, I. The effect of the COVID-19 pandemic on pro and advanced cycling athletes: A cross-sectional study in Poland. Arch. Med. Sci. 2022. [Google Scholar] [CrossRef]
- Liang, W.; Guan, W.; Chen, R.; Wang, W.; Li, J.; Xu, K.; Li, C.; Ai, Q.; Lu, W.; Liang, H.; et al. Cancer patients in SARS-CoV-2 infection: A nationwide analysis in China. Lancet Oncol. 2020, 21, 335–337. [Google Scholar] [CrossRef]
- Rezende, L.F.M.; Lee, D.H.; Ferrari, G.; Eluf-Neto, J.; Giovannucci, E.L. Physical activity for cancer patients during COVID-19 pandemic: A call to action. Cancer Causes Control 2021, 32, 1–3. [Google Scholar] [CrossRef]
- Schauberger, P.; Walker, A. openxlsx: Read, Write and Edit xlsx Files. R Package Version 4.2.5.1. 2022. Available online: https://CRAN.R-project.org/package=openxlsx (accessed on 10 January 2023).
- Wickham, H. ggplot2: Elegant Graphics for Data Analysis; Springer: Berlin/Heidelberg, Germany, 2009. [Google Scholar] [CrossRef]
- Peters, G. User Friendly Science: Quantitative Analysis Made Accessible. R Package Version 0.7.2. 2018. Available online: https://userfriendlyscience.com (accessed on 10 January 2023).
- Sanchez, G. arcdiagram: Plot Prettyarc Diagrams. Rpackage Version 0.1.12. Available online: https://github.com/gastonstat/arcdiagram (accessed on 10 January 2023).
- Gu, Z.; Eils, R.; Schlesner, M. Complex heatmaps reveal patterns and correlations in multidimensional genomic data. Bioinformatics 2016, 32, 2847–2849. [Google Scholar] [CrossRef] [Green Version]
- Tang, D.; Comish, P.; Kang, R. The hallmarks of COVID-19 disease. PLoS Pathog. 2020, 16, e1008536. [Google Scholar] [CrossRef]
- Maugeri, G.; Castrogiovanni, P.; Battaglia, G.; Pippi, R.; D’Agata, V.; Palma, A.; Di Rosa, M.; Musumeci, G. The impact of physical activity on psychological health during COVID-19 pandemic in Italy. Heliyon 2020, 6, e04315. [Google Scholar] [CrossRef]
- Warburton, D.E.R.; Nicol, C.W.; Bredin, S.S.D. Health benefits of physical activity: The evidence. CMAJ 2006, 174, 801–809. [Google Scholar] [CrossRef] [Green Version]
- Grazioli, E.; Cerulli, C.; Dimauro, I.; Moretti, E.; Murri, A.; Parisi, A. New Strategy of Home-Based Exercise during Pandemic COVID-19 in Breast Cancer Patients: A Case Study. Sustainability 2020, 12, 6940. [Google Scholar] [CrossRef]
- Jamka, M.; Makarewicz-Bukowska, A.; Bokayeva, K.; Śmidowicz, A.; Geltz, J.; Kokot, M.; Kaczmarek, N.; Żok, A.; Kononets, V.; Cielecka-Piontek, J.; et al. Comparison of the Effect of Endurance, Strength and Endurance-Strength Training on Glucose and Insulin Homeostasis and the Lipid Profile of Overweight and Obese Subjects: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2022, 19, 14928. [Google Scholar] [CrossRef]
- Natalucci, V.; Marini, C.; Flori, M.; Pietropaolo, F.; Lucertini, F.; Annibalini, G.; Vallorani, L.; Sisti, D.; Saltarelli, R.; Villarini, A.; et al. Effects of a Home-Based Lifestyle Intervention Program on Cardiometabolic Health in Breast Cancer Survivors during the COVID-19 Lockdown. J. Clin. Med. 2021, 10, 2678. [Google Scholar] [CrossRef]
- Campbell, K.L.; Winters-Stone, K.M.; Wiskemann, J.; May, A.M.; Schwartz, A.L.; Courneya, K.S.; Zucker, D.S.; Matthews, C.E.; Ligibel, J.A.; Gerber, L.H.; et al. Exercise Guidelines for Cancer Survivors: Consensus Statement from International Multidisciplinary Roundtable. Med. Sci. Sports Exerc. 2019, 51, 2375–2390. [Google Scholar] [CrossRef] [Green Version]
- Friedenreich, C.M.; Stone, C.R.; Cheung, W.Y.; Hayes, S.C. Physical Activity and Mortality in Cancer Survivors: A Systematic Review and Meta-Analysis. JNCI Cancer Spectr. 2019, 4, pkz080. [Google Scholar] [CrossRef]
- Ibrahim, E.M.; Al-Homaidh, A. Physical activity and survival after breast cancer diagnosis: Meta-analysis of published studies. Med. Oncol. 2010, 28, 753–765. [Google Scholar] [CrossRef]
- Prathikanti, S.; Rivera, R.; Cochran, A.; Tungol, J.G.; Fayazmanesh, N.; Weinmann, E. Treating major depression with yoga: A prospective, randomized, controlled pilot trial. PLoS ONE 2017, 12, e0173869. [Google Scholar] [CrossRef] [Green Version]
- Sorkin, D.; Rook, K.S.; Lu, J.L. Loneliness, lack of emotional support, lack of companionship, and the likelihood of having a heart condition in an elderly sample. Ann. Behav. Med. 2002, 24, 290–298. [Google Scholar] [CrossRef]
- Pelczyńska, M.; Burak, W.; Królak, S.; Geppert, A.; Lipczyński, M.; Grzybołowska, J.; Kociubiński, P. The role of the dietary patterns in the cardiovascular disease risk prevention. J. Med. Sci. 2022, 91, e704. [Google Scholar] [CrossRef]
- Hawkley, L.C.; Thisted, R.A.; Masi, C.M.; Cacioppo, J.T. Loneliness predicts increased blood pressure: 5-year cross-lagged analyses in middle-aged and older adults. Psychol. Aging 2010, 25, 132–141. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yamada, K.; Wakaizumi, K.; Kubota, Y.; Murayama, H.; Tabuchi, T. Loneliness, social isolation, and pain following the COVID-19 outbreak: Data from a nationwide internet survey in Japan. Sci. Rep. 2021, 11, 18643. [Google Scholar] [CrossRef] [PubMed]
- Holt-Lunstad, J.; Smith, T.B.; Baker, M.; Harris, T.; Stephenson, D. Loneliness and Social Isolation as Risk Factors for Mortality. Perspect. Psychol. Sci. 2015, 10, 227–237. [Google Scholar] [CrossRef] [Green Version]
- Hawkley, L.C.; Cacioppo, J.T. Loneliness and pathways to disease. Brain Behav. Immun. 2003, 17, 98–105. [Google Scholar] [CrossRef]
- Holt-Lunstad, J.; Smith, T.B.; Layton, J.B. Social Relationships and Mortality Risk: A Meta-analytic Review. PLoS Med. 2010, 7, e1000316. [Google Scholar] [CrossRef]
- Hawkley, L.C.; Thisted, R.A.; Cacioppo, J.T. Loneliness predicts reduced physical activity: Cross-sectional & longitudinal analyses. Health Psychol. 2009, 28, 354–363. [Google Scholar] [CrossRef] [Green Version]
- Anderson, E.S.; Wojcik, J.R.; Winett, R.A.; Williams, D.M. Social-cognitive determinants of physical activity: The influence of social support, self-efficacy, outcome expectations, and self-regulation among participants in a church-based health promotion study. Health Psychol. 2006, 25, 510–520. [Google Scholar] [CrossRef]
- Hawkley, L.C.; Burleson, M.H.; Berntson, G.G.; Cacioppo, J.T. Loneliness in everyday life: Cardiovascular activity, psychosocial context, and health behaviors. J. Pers. Soc. Psychol. 2003, 85, 105–120. [Google Scholar] [CrossRef]
- Zapała, J.; Matecka, M.; Zok, A.; Baum, E. The needs of cancer patients during the COVID-19 pandemic—Psychosocial, ethical and spiritual aspects—Systematic review. PeerJ 2022, 10, e13480. [Google Scholar] [CrossRef]
- Hardoerfer, K.; Jentschke, E. Effect of Yoga Therapy on Symptoms of Anxiety in Cancer Patients. Oncol. Res. Treat. 2018, 41, 526–532. [Google Scholar] [CrossRef]
- Żok, A.; Zapała, J.; Baum, E. Activities based on yoga techniques in psychiatric treatment in Poland in a historical context. Psychiatr. Polska 2022, 56, 1405–1416. [Google Scholar] [CrossRef]
- Bower, J.E.; Garet, D.; Sternlieb, B.; Ganz, P.A.; Irwin, M.; Olmstead, R.A.; Greendale, G. Yoga for persistent fatigue in breast cancer survivors: A randomized controlled trial. Cancer 2012, 118, 3766–3775. [Google Scholar] [CrossRef] [Green Version]
- Lundt, A.; Jentschke, E. Long-Term Changes of Symptoms of Anxiety, Depression, and Fatigue in Cancer Patients 6 Months After the End of Yoga Therapy. Integr. Cancer Ther. 2019, 18, 1534735418822096. [Google Scholar] [CrossRef] [Green Version]
- Greenlee, H.; DuPont-Reyes, M.J.; Rn, L.G.B.; Carlson, L.E.; Cohen, M.R.; Deng, G.; Johnson, J.A.; Mumber, M.; Seely, D.; Zick, S.M.; et al. Clinical practice guidelines on the evidence-based use of integrative therapies during and after breast cancer treatment. CA Cancer J. Clin. 2017, 67, 194–232. [Google Scholar] [CrossRef]
- Kaminsky, D.A.; Guntupalli, K.K.; Lippmann, J.; Burns, S.M.; Brock, M.A.; Skelly, J.; DeSarno, M.; Pecott-Grimm, H.; Mohsin, A.; LaRock-McMahon, C.; et al. Effect of Yoga Breathing (Pranayama) on Exercise Tolerance in Patients with Chronic Obstructive Pulmonary Disease: A Randomized, Controlled Trial. J. Altern. Complement. Med. 2017, 23, 696–704. [Google Scholar] [CrossRef]
- Cramer, H.; Lauche, R.; Klose, P.; Lange, S.; Langhorst, J.; Dobos, G.J. Yoga for improving health-related quality of life, mental health and cancer-related symptoms in women diagnosed with breast cancer. Cochrane Database Syst. Rev. 2017, 1, CD010802. [Google Scholar] [CrossRef] [Green Version]
- Gosain, R.; Gage-Bouchard, E.; Ambrosone, C.; Repasky, E.; Gandhi, S. Stress reduction strategies in breast cancer: Review of pharmacologic and non-pharmacologic based strategies. Semin. Immunopathol. 2020, 42, 719–734. [Google Scholar] [CrossRef]
- Sephton, S.; Spiegel, D. Circadian disruption in cancer: A neuroendocrine-immune pathway from stress to disease? Brain Behav. Immun. 2003, 17, 321–328. [Google Scholar] [CrossRef]
- Kach, J.; Conzen, S.D.; Szmulewitz, R.Z. Targeting the glucocorticoid receptor in breast and prostate cancers. Sci. Transl. Med. 2015, 7, 305ps19. [Google Scholar] [CrossRef] [Green Version]
- Heffner, K.L.; Loving, T.J.; Robles, T.F.; Kiecolt-Glaser, J.K. Examining psychosocial factors related to cancer incidence and progression: In search of the silver lining. Brain Behav. Immun. 2003, 17, 109–111. [Google Scholar] [CrossRef] [PubMed]
- Voss, M.J.; Entschladen, F. Tumor interactions with soluble factors and the nervous system. Cell Commun. Signal. 2010, 8, 21. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chalaye, P.; Goffaux, P.; Lafrenaye, S.; Marchand, S. Respiratory Effects on Experimental Heat Pain and Cardiac Activity. Pain Med. 2009, 10, 1334–1340. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Busch, V.; Magerl, W.; Kern, U.; Haas, J.; Hajak, G.; Eichhammer, P. The Effect of Deep and Slow Breathing on Pain Perception, Autonomic Activity, and Mood Processing—An Experimental Study. Pain Med. 2012, 13, 215–228. [Google Scholar] [CrossRef] [PubMed]
- Li, J.X.; Hong, Y.; Chan, K.M. Tai chi: Physiological characteristics and beneficial effects on health. Br. J. Sports Med. 2001, 35, 148–156. [Google Scholar] [CrossRef] [PubMed]
- Sovik, R. The science of breathing—The yogic view. Prog. Brain Res. 2000, 122, 491–505. [Google Scholar] [CrossRef]
- Bai, Z.; Guan, Z.; Fan, Y.; Liu, C.; Yang, K.; Ma, B.; Wu, B. The Effects of Qigong for Adults with Chronic Pain: Systematic Review and Meta-Analysis. Am. J. Chin. Med. 2015, 43, 1525–1539. [Google Scholar] [CrossRef]
- Scott, T.M.; Gerbarg, P.L.; Silveri, M.M.; Nielsen, G.H.; Owen, L.; Nyer, M.; Brown, R.P.; Streeter, C.C. Psychological Function, Iyengar Yoga, and Coherent Breathing: A Randomized Controlled Dosing Study. J. Psychiatr. Pract. 2019, 25, 437–450. [Google Scholar] [CrossRef]
- Nyer, M.; Gerbarg, P.L.; Silveri, M.M.; Johnston, J.; Scott, T.M.; Nauphal, M.; Owen, L.; Nielsen, G.H.; Mischoulon, D.; Brown, R.P.; et al. A randomized controlled dosing study of Iyengar yoga and coherent breathing for the treatment of major depressive disorder: Impact on suicidal ideation and safety findings. Complement. Ther. Med. 2018, 37, 136–142. [Google Scholar] [CrossRef] [Green Version]
- Streeter, C.C.; Gerbarg, P.L.; Whitfield, T.H.; Owen, L.; Johnston, J.; Silveri, M.M.; Gensler, M.; Faulkner, C.L.; Mann, C.; Wixted, M.; et al. Treatment of Major Depressive Disorder with Iyengar Yoga and Coherent Breathing: A Randomized Controlled Dosing Study. J. Altern. Complement. Med. 2017, 23, 201–207. [Google Scholar] [CrossRef] [Green Version]
- Streeter, C.C.; Whitfield, T.H.; Owen, L.; Rein, T.; Karri, S.K.; Yakhkind, A.; Perlmutter, R.; Prescot, A.; Renshaw, P.F.; Ciraulo, D.; et al. Effects of Yoga Versus Walking on Mood, Anxiety, and Brain GABA Levels: A Randomized Controlled MRS Study. J. Altern. Complement. Med. 2010, 16, 1145–1152. [Google Scholar] [CrossRef]
- Tsopanidou, A.; Venetsanou, F.D.; Stavridis, I.S.; Paradisis, G.P.; Zacharogiannis, E.G. Energy expenditure during a Vinyasa yoga session. J. Sports Med. Phys. Fit. 2020, 60, 1110–1117. [Google Scholar] [CrossRef]
- Piña, A.A.; Shadiow, J.; Fadeyi, A.T.; Chavez, A.; Hunter, S.D. The acute effects of vinyasa flow yoga on vascular function, lipid and glucose concentrations, and mood. Complement. Ther. Med. 2021, 56, 102585. [Google Scholar] [CrossRef]
- Sherman, S.A.; Rogers, R.J.; Davis, K.K.; Minster, R.; Creasy, S.A.; Mullarkey, N.C.; O’Dell, M.; Donahue, P.; Jakicic, J.M. Energy Expenditure in Vinyasa Yoga Versus Walking. J. Phys. Act. Health 2017, 14, 597–605. [Google Scholar] [CrossRef]
- Lemay, V.; Hoolahan, J.; Buchanan, A. Impact of a Yoga and Meditation Intervention on Students’ Stress and Anxiety Levels. Am. J. Pharm. Educ. 2019, 83, 7001. [Google Scholar] [CrossRef]
- Pierce, D.R.; Doma, K.; Leicht, A.S. Acute Effects of Exercise Mode on Arterial Stiffness and Wave Reflection in Healthy Young Adults: A Systematic Review and Meta-Analysis. Front. Physiol. 2018, 9, 73. [Google Scholar] [CrossRef] [Green Version]
- Kwak, A.; Jacobs, J.; Haggett, D.; Jimenez, R.; Peppercorn, J. Evaluation and management of insomnia in women with breast cancer. Breast Cancer Res. Treat. 2020, 181, 269–277. [Google Scholar] [CrossRef]
- Olfson, M.; Wall, M.; Liu, S.-M.; Morin, C.M.; Blanco, C. Insomnia and Impaired Quality of Life in the United States. J. Clin. Psychiatry 2018, 79, 9151. [Google Scholar] [CrossRef]
- Dirksen, S.R.; Epstein, D.R. Efficacy of an insomnia intervention on fatigue, mood and quality of life in breast cancer survivors. J. Adv. Nurs. 2008, 61, 664–675. [Google Scholar] [CrossRef]
- Bolge, S.C.; Doan, J.F.; Kannan, H.; Baran, R.W. Association of insomnia with quality of life, work productivity, and activity impairment. Qual. Life Res. 2009, 18, 415–422. [Google Scholar] [CrossRef]
- Büttner-Teleagă, A.; Kim, Y.-T.; Osel, T.; Richter, K. Sleep Disorders in Cancer—A Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 11696. [Google Scholar] [CrossRef] [PubMed]
- Fleming, L.; Randell, K.; Stewart, E.; Espie, C.A.; Morrison, D.; Lawless, C.; Paul, J. Insomnia in breast cancer: A prospective observational study. Sleep 2019, 42, zsy245. [Google Scholar] [CrossRef] [PubMed]
- Savard, J.; Simard, S.; Blanchet, J.; Ivers, H.; Morin, C.M. Prevalence, Clinical Characteristics, and Risk Factors for Insomnia in the Context of Breast Cancer. Sleep 2001, 24, 583–590. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schieber, K.; Niecke, A.; Geiser, F.; Erim, Y.; Bergelt, C.; Büttner-Teleaga, A.; Maatouk, I.; Stein, B.; Teufel, M.; Wickert, M.; et al. The course of cancer-related insomnia: Don’t expect it to disappear after cancer treatment. Sleep Med. 2019, 58, 107–113. [Google Scholar] [CrossRef]
- Torales, J.; O’Higgins, M.; Castaldelli-Maia, J.M.; Ventriglio, A. The outbreak of COVID-19 coronavirus and its impact on global mental health. Int. J. Soc. Psychiatry 2020, 66, 317–320. [Google Scholar] [CrossRef] [Green Version]
- Taporoski, T.P.; Beijamini, F.; Gómez, L.M.; Ruiz, F.S.; Ahmed, S.S.; von Schantz, M.; Pereira, A.C.; Knutson, K.L. Subjective sleep quality before and during the COVID-19 pandemic in a Brazilian rural population. Sleep Health 2022, 8, 167–174. [Google Scholar] [CrossRef]
- Jiang, Z.; Zhu, P.; Wang, L.; Hu, Y.; Pang, M.; Ma, S.; Tang, X. Psychological distress and sleep quality of COVID-19 patients in Wuhan, a lockdown city as the epicenter of COVID-19. J. Psychiatr. Res. 2021, 136, 595–602. [Google Scholar] [CrossRef]
- Goyal, N.; Levine, B.J.; Crawford, S.L.; Avis, N.E. Sleep disturbance among breast cancer survivors and controls from midlife to early older adulthood: Pink SWAN. J. Cancer Surviv. 2022, 1–10. [Google Scholar] [CrossRef]
- Zeichner, S.B.; Zeichner, R.L.; Gogineni, K.; Shatil, S.; Ioachimescu, O. Cognitive Behavioral Therapy for Insomnia, Mindfulness, and Yoga in Patients With Breast Cancer with Sleep Disturbance: A Literature Review. Breast Cancer Basic Clin. Res. 2017, 11, 1178223417745564. [Google Scholar] [CrossRef] [Green Version]
- Wang, W.-L.; Chen, K.-H.; Pan, Y.-C.; Yang, S.-N.; Chan, Y.-Y. The effect of yoga on sleep quality and insomnia in women with sleep problems: A systematic review and meta-analysis. BMC Psychiatry 2020, 20, 195. [Google Scholar] [CrossRef]
- Mason, H.; Vandoni, M.; DeBarbieri, G.; Codrons, E.; Ugargol, V.; Bernardi, L. Cardiovascular and Respiratory Effect of Yogic Slow Breathing in the Yoga Beginner: What Is the Best Approach? Evid.-Based Complement. Altern. Med. 2013, 2013, 743504. [Google Scholar] [CrossRef] [Green Version]
- Jovanov, E. On Spectral Analysis of Heart Rate Variability during Very Slow Yogic Breathing. In Proceedings of the 2005 IEEE Engineering in Medicine and Biology 27th Annual Conference, Shanghai, China, 31 August–3 September 2005; Volume 3, pp. 2467–2470. [Google Scholar] [CrossRef] [Green Version]
- Kuppusamy, M.; Dilara, K.; Ravishankar, P.; Julius, A. Effect of bhrāmarī Prāṇāyāma practice on pulmonary function in healthy adolescents: A randomized control study. Anc. Sci. Life 2017, 36, 196–199. [Google Scholar] [CrossRef]
- Kuppusamy, M.; Kamaldeen, D.; Pitani, R.; Amaldas, J.; Shanmugam, P. Effects of Bhramari Pranayama on health—A systematic review. J. Tradit. Complement. Med. 2018, 8, 11–16. [Google Scholar] [CrossRef]
- Pasyar, N.; Tashnizi, N.B.; Mansouri, P.; Tahmasebi, S. Effect of yoga exercise on the quality of life and upper extremity volume among women with breast cancer related lymphedema: A pilot study. Eur. J. Oncol. Nurs. 2019, 42, 103–109. [Google Scholar] [CrossRef]
- Zhi, W.I.; Baser, R.E.; Zhi, L.M.; Talukder, D.; Li, Q.S.; Paul, T.; Patterson, C.; Piulson, L.; Seluzicki, C.; Galantino, M.L.; et al. Yoga for cancer survivors with chemotherapy-induced peripheral neuropathy: Health-related quality of life outcomes. Cancer Med. 2021, 10, 5456. [Google Scholar] [CrossRef]
- Duncan, M.; Moschopoulou, E.; Herrington, E.; Deane, J.; Roylance, R.; Jones, L.; Bourke, L.; Morgan, A.; Chalder, T.; Thaha, M.A.; et al. Review of systematic reviews of non-pharmacological interventions to improve quality of life in cancer survivors. BMJ Open 2017, 7, e015860. [Google Scholar] [CrossRef]
- Sahni, P.S.; Singh, K.; Sharma, N.; Garg, R. Yoga an effective strategy for self-management of stress-related problems and wellbeing during COVID19 lockdown: A cross-sectional study. PLoS ONE 2021, 16, e0245214. [Google Scholar] [CrossRef]




| Parameter | N | % |
|---|---|---|
| Age ranges | ||
| 25–30 | 2 | 4.88 |
| 31–36 | 1 | 2.44 |
| 37–45 | 13 | 31.71 |
| 46–51 | 12 | 29.27 |
| 52–60 | 6 | 14.63 |
| 61–69 | 7 | 17.07 |
| Sex | ||
| Women | 41 | 100 |
| I live with | ||
| with the family | 24 | 58.54 |
| with soul mate | 11 | 26.83 |
| alone | 6 | 14.63 |
| Residence | ||
| city with a population of over 100,000 | 20 | 48.78 |
| city of 26,000–100,000 residents | 5 | 12.2 |
| city of 10,000–25,000 residents | 7 | 17.07 |
| city of less than 10,000 inhabitants | 4 | 9.76 |
| village | 5 | 12.2 |
| Education | ||
| higher education | 34 | 82.93 |
| high school education | 7 | 17.07 |
| Do you practice yoga? | ||
| Yes, regularly | 1 | 2.44 |
| Yes, sometimes | 27 | 65.85 |
| I never practiced yoga | 13 | 31.71 |
| Are you receiving treatment with chemo/radiotherapy? | ||
| Finished treatment | 22 | 53.66 |
| I am in the process of treatment | 16 | 39.02 |
| I do not qualify for treatment | 3 | 7.32 |
| Answer | Before (N) | After (N) | Before % | After % |
|---|---|---|---|---|
| I am constantly so sad and unhappy that it is unbearable | 1 | 0 | 7.69 | 0 |
| I am experiencing constant sadness, depression and I cannot free myself from these experiences | 1 | 1 | 7.69 | 7.69 |
| I often feel sad and depressed | 5 | 4 | 38.46 | 30.77 |
| I’m not sad or depressed | 6 | 8 | 46.15 | 61.54 |
| I often worry about the future | 7 | 5 | 53.85 | 38.46 |
| I’m afraid that nothing good awaits me in the future | 2 | 1 | 15.38 | 7.69 |
| I’m not too worried about the future | 4 | 7 | 30.77 | 53.85 |
| I feel self-loathing | 1 | 0 | 7.69 | 0 |
| I’m not satisfied with myself | 5 | 5 | 38.46 | 38.46 |
| I’m satisfied with myself | 7 | 8 | 53.85 | 61.54 |
| I cry more often than I used to | 6 | 1 | 46.15 | 7.69 |
| I don’t cry more than usual | 7 | 12 | 53.85 | 92.31 |
| Everything that used to irritate me has become indifferent | 1 | 0 | 7.69 | 0 |
| I am constantly nervous and irritable | 1 | 1 | 7.69 | 7.69 |
| I’m more nervous and unpleasant than before | 5 | 1 | 38.46 | 7.69 |
| I’m no more nervous than I used to be | 6 | 11 | 46.15 | 84.62 |
| I sleep well, as usual | 2 | 8 | 15.38 | 61.54 |
| I sleep worse than I used to | 7 | 5 | 53.85 | 38.46 |
| I wake up a few hours too early and can’t get to sleep | 1 | 0 | 7.69 | 0 |
| In the morning, I wake up 1–2 h too early and find it difficult to get back to sleep again | 3 | 0 | 23.08 | 0 |
| I’m tiring much faster than before | 11 | 6 | 84.62 | 46.15 |
| I get tired of everything I do | 0 | 1 | 0 | 7.69 |
| Well, I’m getting more tired than before | 2 | 6 | 15.38 | 46.15 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zok, A.; Matecka, M.; Zapala, J.; Izycki, D.; Baum, E. The Effect of Vinyasa Yoga Practice on the Well-Being of Breast-Cancer Patients during COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2023, 20, 3770. https://doi.org/10.3390/ijerph20043770
Zok A, Matecka M, Zapala J, Izycki D, Baum E. The Effect of Vinyasa Yoga Practice on the Well-Being of Breast-Cancer Patients during COVID-19 Pandemic. International Journal of Environmental Research and Public Health. 2023; 20(4):3770. https://doi.org/10.3390/ijerph20043770
Chicago/Turabian StyleZok, Agnieszka, Monika Matecka, Joanna Zapala, Dariusz Izycki, and Ewa Baum. 2023. "The Effect of Vinyasa Yoga Practice on the Well-Being of Breast-Cancer Patients during COVID-19 Pandemic" International Journal of Environmental Research and Public Health 20, no. 4: 3770. https://doi.org/10.3390/ijerph20043770





