Improving Sleep with Far-Infrared-Emitting Pajamas: A Pilot Randomized Controlled Trial
Abstract
1. Introduction
2. Materials and Methods
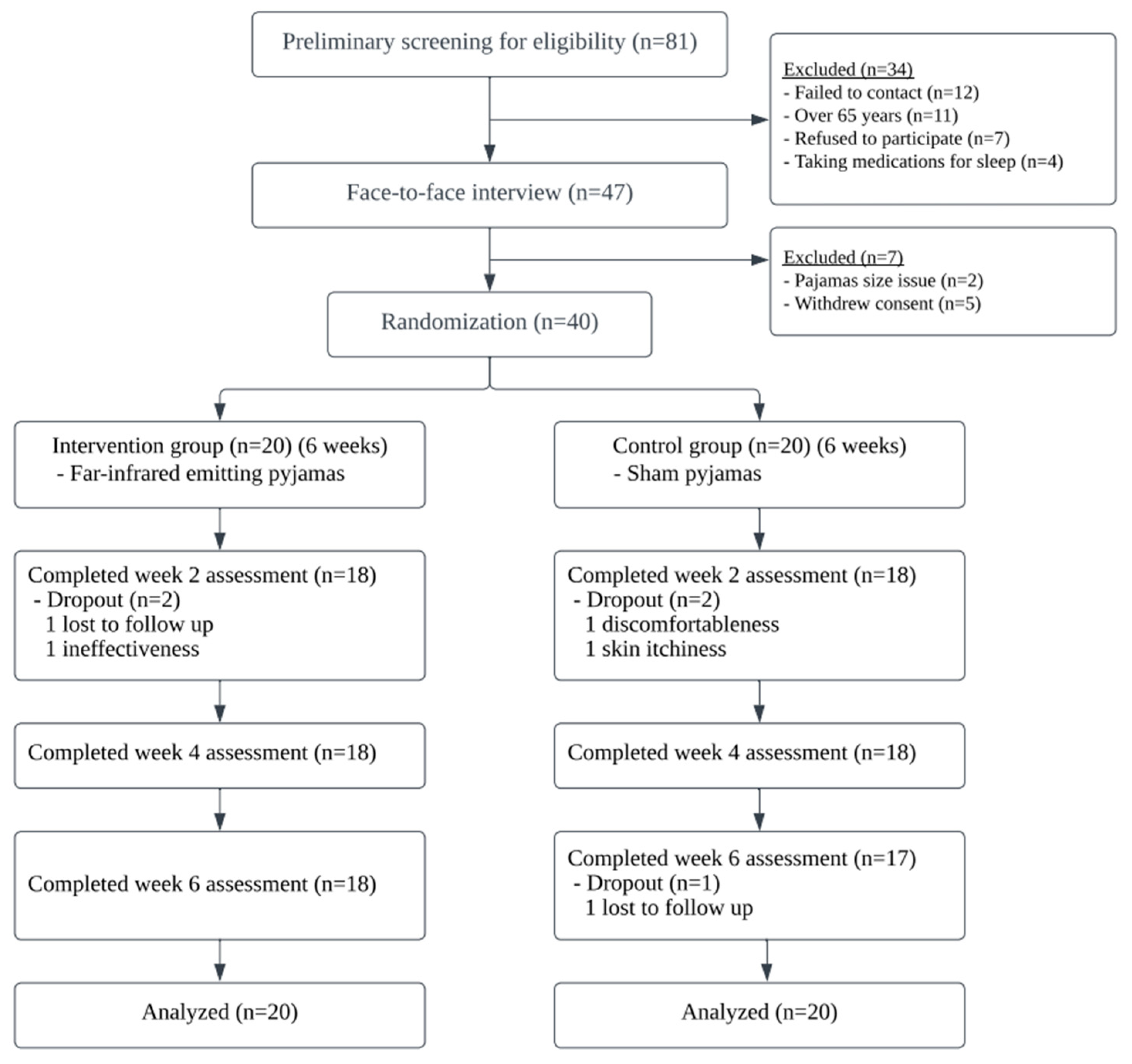
2.1. Study Design
2.2. Subjects and Randomization
2.3. Interventions
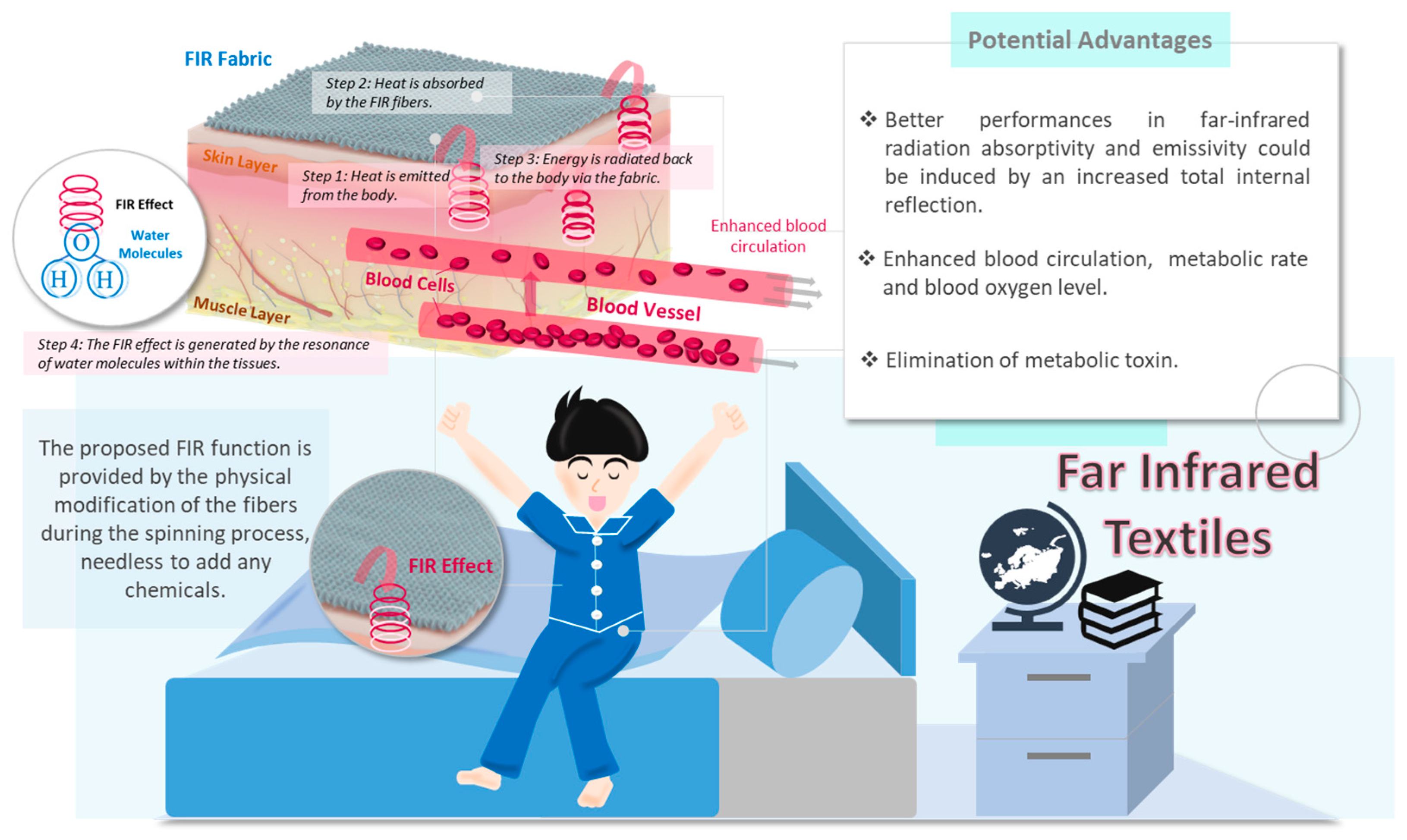
2.3.1. FIR-Emitting-Pajamas Group
2.3.2. Sham-Pajamas Group
2.4. Monitoring of Compliance at Home
2.5. Outcome Assessments
Patient-Centered Outcome Assessment
2.6. Adherence Assessment
2.7. Sample Size Estimation
2.8. Data Management and Analysis
3. Results
3.1. Characteristics of Recruited Subjects
3.2. Intervention Compliance
3.3. Primary Outcome
3.4. Secondary Outcomes
3.4.1. ISI
3.4.2. The Seven-Day Sleep Diary
3.4.3. HADS, MFI, Satisfaction with Life Scale, ESS
3.4.4. Blinding
3.4.5. Adverse Events
3.4.6. Post Hoc Power Analysis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ford, D.E.; Kamerow, D. Epidemiologic study of sleep disturbances and psychiatric disorders: An opportunity for prevention? JAMA 1989, 262, 1479–1484. [Google Scholar] [CrossRef]
- Ohayon, M.M.; Paiva, T. Global sleep dissatisfaction for the assessment of insomnia severity in the general population of Portugal. Sleep Med. 2005, 6, 435–441. [Google Scholar] [CrossRef]
- Ohayon, M.M.; Smirne, S. Prevalence and consequences of insomnia disorders in the general population of Italy. Sleep Med. 2002, 3, 115–120. [Google Scholar] [CrossRef]
- Morin, C.M.; Drake, C.L.; Harvey, A.G.; Krystal, A.D.; Manber, R.; Riemann, D.; Spiegelhalder, K. Insomnia disorder. Nat. Rev. Dis. Primers 2015, 3, 15026. [Google Scholar] [CrossRef]
- Perlis, M.L.; Posner, D.; Riemann, D.; Bastien, C.H.; Teel, J.; Thase, M. Insomnia. Lancet 2022, 24, 1047–1060. [Google Scholar] [CrossRef]
- Cao, X.L.; Wang, S.B.; Zhong, B.L.; Zhang, L.; Ungvari, G.S.; Ng, C.H. The prevalence of insomnia in the general population in China: A meta-analysis. PLoS ONE 2017, 12, e0170772. [Google Scholar] [CrossRef]
- Chung, K.F.; Yeung, W.F.; Ho, F.Y.Y.; Yung, K.P.; Yu, Y.M.; Kwok, C.W. Cross-cultural and comparative epidemiology of insomnia: The Diagnostic and Statistical Manual (DSM), International Classification of Diseases (ICD) and International Classification of Sleep Disorders (ICSD). Sleep Med. 2014, 16, 477–482. [Google Scholar] [CrossRef]
- Lam, C.S.; Yu, B.Y.M.; Cheung, D.S.T.; Cheung, T.; Lam, S.C.; Chung, K.F.; Ho, F.Y.Y.; Yeung, W.F. Sleep and mood disturbances during the COVID-19 outbreak in an urban Chinese population in Hong Kong: A longitudinal study of the second and third waves of the outbreak. Int. J. Environ. Res. Public Health 2021, 18, 8444. [Google Scholar] [CrossRef] [PubMed]
- Wong, W.S.; Fielding, R. Prevalence of insomnia among Chinese adults in Hong Kong: A population-based study. J. Sleep Res. 2011, 20, 117–126. [Google Scholar] [CrossRef]
- Yu, B.Y.M.; Yeung, W.F.; Lam, J.C.S.; Yuen, S.C.S.; Lam, S.C.; Chung, V.C.H.; Chung, K.F.; Lee, P.H.; Ho, F.Y.Y.; Ho, J.Y.S. Prevalence of sleep disturbances during COVID-19 outbreak in an urban Chinese population: A cross-sectional study. Sleep Med. 2020, 74, 18–24. [Google Scholar] [CrossRef]
- Kuppermann, M.; Lubeck, D.P.; Mazonson, P.D.; Patrick, D.L.; Stewart, A.L.; Buesching, D.P.; Filer, S. Sleep problems and their correlates in a working population. J. Gen. Intern. Med. 1995, 10, 25–32. [Google Scholar] [CrossRef]
- Taylor, D.J.; Mallory, L.J.; Lichstein, K.L.; Durrence, H.H.; Riedel, B.W.; Bush, A. Comorbidity of chronic insomnia with medical problems. Sleep 2007, 30, 213–218. [Google Scholar] [CrossRef]
- Yeung, W.F.; Chung, K.F.; Wong, C.Y. Relationship between insomnia and headache in community-based middle-aged Hong Kong Chinese women. J. Headache Pain 2010, 11, 187–195. [Google Scholar] [CrossRef]
- Neckelmann, D.; Mykletun, A.; Dahl, A. Chronic insomnia as a risk factor for developing anxiety and depression. Sleep 2007, 30, 873–880. [Google Scholar] [CrossRef]
- Okamoto-Mizuno, K.; Mizuno, K. Effects of thermal environment on sleep and circadian rhythm. J. Physiol. Anthropol. 2012, 31, 14. [Google Scholar] [CrossRef]
- Vatansever, F.; Hamblin, M. Far infrared radiation (FIR): Its biological effects and medical applications: Ferne Infrarotstrahlung: Biologische Effekte und medizinische Anwendungen. Photonics Lasers Med. 2012, 1, 255–266. [Google Scholar] [CrossRef]
- Leung, T.K.; Chen, C.H.; Tsai, S.Y.; Hsiao, G.; Lee, C.M. Effects of far infrared rays irradiated from ceramic material (BIOCERAMIC) on psychological stress-conditioned elevated heart rate, blood pressure, and oxidative stress-suppressed cardiac contractility. Chin. J. Physiol. 2012, 55, 323–330. [Google Scholar]
- Washington, K.; Wason, J.; Thein, M.S.; Lavery, L.A.; Hamblin, M.R.; Gordon, I.L. Randomized controlled trial comparing the effects of far-infrared emitting ceramic fabric shirts and control polyester shirts on transcutaneous PO2. J. Text. Sci. Eng. 2018, 8, 349. [Google Scholar]
- McCall, W.V.; Letton, A.; Lundeen, J.; Case, D.; Cidral-Filho, F. The effect of far-infrared emitting sheets on sleep. Res. J. Text. Appar. 2018, 22, 247–259. [Google Scholar] [CrossRef]
- Hamilton, M. The Hamilton Depression Scale-accelerator or break on antidepressant drug discovery. J. Neurol. Neurosurg. Psychiatry 1960, 23, 56–62. [Google Scholar] [CrossRef]
- Cheung, D.S.T.; Tiwari, A.; Yeung, W.F.; Yu, D.S.F.; So, M.K.P.; Chau, P.H.; Wang, X.M.; Lum, T.Y.S.; Yuk Fung, H.Y.K.; Ng, B.Y.M.; et al. Self-Administered Acupressure for Caregivers of Older Family Members: A Randomized Controlled Trial. J. Am. Geriatr. Soc. 2020, 68, 1193–1201. [Google Scholar] [CrossRef]
- Cheung, D.S.T.; Yeung, W.F.; Suen, L.K.P.; Chong, T.C.; Ho, Y.S.; Yu, B.Y.M.; Chan, L.Y.T.; Chen, H.Y.; Lao, L.X. Self-administered acupressure for knee osteoarthritis in middle-aged and older adults: A pilot randomized controlled trial. Acupunct. Med. 2020, 38, 75–85. [Google Scholar] [CrossRef]
- Yeung, W.F.; Lai, A.Y.K.; Ho, F.Y.Y.; Suen, L.K.P.; Chung, K.F.; Ho, J.Y.S.; Ho, L.M.; Yu, B.Y.M.; Chan, L.Y.T.; Lam, T.H. Effects of Zero-time Exercise on inactive adults with insomnia disorder: A pilot randomized controlled trial. Sleep Med. 2018, 52, 118–127. [Google Scholar] [CrossRef] [PubMed]
- Yeung, W.F.; Ho, F.Y.Y.; Chung, K.F.; Zhang, Z.J.; Yu, B.Y.M.; Suen, L.K.P.; Chan, L.Y.T.; Chen, H.Y.; Ho, L.M.; Lao, L.X. Self-administered acupressure for insomnia disorder: A pilot randomized controlled trial. J. Sleep Res. 2018, 27, 220–231. [Google Scholar] [CrossRef]
- Yeung, W.F.; Yu, B.Y.M.; Chung, K.F.; Zhang, Z.J.; Lao, L.X.; Ho, F.Y.Y.; Suen, L.K.P.; Ho, L.M. Self-administered acupressure for insomnia disorder: A randomized controlled trial. Phytomedicine 2022, 99, 153993. [Google Scholar] [CrossRef]
- Chen, S.C.; Yu, J.; Wang, H.S.; Wang, D.D.; Sun, Y.; Cheng, H.L.; Suen, L.K.; Yeung, W.F. Parent-administered pediatric Tuina for attention deficit/hyperactivity disorder symptoms in preschool children: A pilot randomized controlled trial embedded with a process evaluation. Phytomedicine 2022, 102, 154191. [Google Scholar] [CrossRef]
- Buysse, D.J.; Reynolds III, C.F.; Monk, T.H.; Berman, S.R.; Kupfer, D.J. The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiartry Res. 1988, 28, 193–213. [Google Scholar] [CrossRef]
- Bastien, C.H.; Vallières, A.; Morin, C.M. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med. 2001, 2, 297–307. [Google Scholar] [CrossRef]
- Zigmond, A.S.; Snaith, R.P. The hospital anxiety and depression scale. Occup. Med. 1983, 67, 361–370. [Google Scholar] [CrossRef]
- Johns, M. A new method for measuring daytime sleepiness: The Epworth sleepiness scale. Sleep 1991, 14, 540–545. [Google Scholar] [CrossRef]
- Pavot, W.; Diener, E. The satisfaction with life scale and the emerging construct of life satisfaction. J. Posit. Psychol. 2008, 3, 137–152. [Google Scholar] [CrossRef]
- Carney, C.E.; Buysse, D.J.; Ancoli-Israel, S.; Edinger, J.D.; Krystal, A.D.; Lichstein, K.L.; Morin, C.M. The consensus sleep diary: Standardizing prospective sleep self-monitoring. Sleep 2012, 35, 287–302. [Google Scholar] [CrossRef]
- Buysse, D.J.; Ancoli-Israel, S.; Edinger, J.D.; Lichstein, K.L.; Morin, C.M. Recommendations for a standard research assessment of insomnia. Sleep 2006, 29, 1155–1173. [Google Scholar] [CrossRef]
- Whitehead, A.L.; Julious, S.A.; Cooper, C.L.; Campbell, M. Estimating the sample size for a pilot randomised trial to minimise the overall trial sample size for the external pilot and main trial for a continuous outcome variable. Stat. Methods Med. Res. 2016, 25, 1057–1073. [Google Scholar] [CrossRef]
- Julious, S.A. Sample size of 12 per group rule of thumb for a pilot study. Pharm. Stat. 2005, 4, 287–291. [Google Scholar] [CrossRef]
- Morris, S.B. Estimating Effect Sizes From Pretest-Posttest-Control Group Designs. Organ. Res. Methods 2008, 11, 364–386. [Google Scholar] [CrossRef]
- Paterson, C.; Dieppe, P. Characteristic and incidental (placebo) effects in complex interventions such as acupuncture. BMJ 2005, 330, 1202–1205. [Google Scholar] [CrossRef]
- Markt, C.; Johnson, M. Transitional objects, pre-sleep rituals, and psychopathology. Child Psychiatry Hum. Dev. 1993, 23, 161–173. [Google Scholar] [CrossRef]
- Jencius, M.J.; Rotter, J.C. Bedtime Rituals and Their Relationship to Childhood Sleep Disturbance. Fam. J. 1998, 6, 94–105. [Google Scholar] [CrossRef]
- Chung, K.F.; Yeung, W.F.; Yu, Y.M.; Ho, F.Y.Y. A population-based 2-year longitudinal study of insomnia disorder in a Chinese population in Hong Kong. Psychol. Health Med. 2018, 23, 505–510. [Google Scholar] [CrossRef]
- Raymann, R.J.; van Someren, E.J.W. Diminished capability to recognize the optimal temperature for sleep initiation may contribute to poor sleep in elderly people. Sleep 2008, 31, 1301–1309. [Google Scholar] [CrossRef]
- Andersen, A.L.; Araujo, P.; Frange, C.; Tufik, S. Sleep Disturbance and Pain: A Tale of Two Common Problems. Contemp. Rev. Sleep Med. 2018, 154, 1249–1259. [Google Scholar]
| Variable a | All Subjects (n = 40) | FIR-Pajamas Group (n = 20) | Sham-Pajamas Group (n = 20) | p-Value b |
|---|---|---|---|---|
| Age (y) | 51.23 (11.212) | 53.10 (10.508) | 49.35 (11.842) | 0.296 |
| Female gender (%) | 0.376 | |||
| Female | 34 (85.0%) | 16 (47.1%) | 18 (52.9%) | |
| Educational level (y) | 0.062 | |||
| Primary education or below | 1 (2.5%) | 0 (0.0%) | 1 (100.0%) | |
| S1–S3 | 4 (10.0%) | 4 (100.0%) | 0 (0.0%) | |
| S4–S7 | 13 (32.5%) | 8 (61.5%) | 5 (38.5%) | |
| Tertiary education or above | 22 (55.0%) | 8 (36.4%) | 14 (63.6%) | |
| Marital status (%) | 0.729 | |||
| Single | 8 (20.0%) | 3 (37.5%) | 5 (62.5%) | |
| Married | 30 (75.0%) | 16 (53.3%) | 14 (46.7%) | |
| Divorced/widowed | 2 (5.0%) | 1 (50.0%) | 1 (50.0%) | |
| Employment status (%) | ||||
| Employed | 22 (55.0%) | 11 (50.0%) | 11 (50.0%) | |
| Unemployed/retired/housework | 18 (45.0%) | 9 (50.0%) | 9 (50.0%) | 1.000 |
| BMI (kg/m2) | 22.361 (4.481) | 21.997 (2.755) | 22.726 (5.774) | 0.613 |
| Hospitalization for physical disease (%) | 12.0 (30.0%) | 7 (58.3%) | 5 (41.7%) | 0.490 |
| Previous intervention for sleep disturbance (%) | 30 (75.0%) | 15 (50.0%) | 15 (50.0%) | 1.000 |
| Western medicine | 3 (7.5%) | 2 (66.7%) | 1 (33.3%) | 0.548 |
| Chinese herbal medicine | 13 (32.5%) | 6 (46.2%) | 7 (53.8%) | 0.736 |
| Acupuncture | 10 (25.0%) | 4 (40.0%) | 6 (60.0%) | 0.465 |
| Massage | 8 (20.0%) | 5 (62.5%) | 3 (37.5%) | 0.429 |
| Sports | 18 (45.0%) | 8 (44.4%) | 10 (55.6%) | 0.525 |
| Psychotherapy | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 1.000 |
| Others | 5 (12.5%) | 3 (6.0.%) | 2 (40.0%) | 0.633 |
| Pittsburgh Sleep Quality Index | 9.33 (3.058) | 9.50 (3.269) | 9.15 (2.907) | 0.722 |
| Insomnia Severity Index | 14.70 (4.490) | 14.30 (4.231) | 15.10 (4.811) | 0.580 |
| Seven-day sleep diary | ||||
| Sleep onset latency | 38.575 (28.241) | 36.614 (26.657) | 40.535 (30.305) | 0.666 |
| Wakefulness after sleep onset | 37.382 (36.551) | 46.858 (44.678) | 27.907 (23.604) | 0.102 |
| Total sleep time | 375.684 (72.231) | 361.617 (78.749) | 389.752 (63.964) | 0.223 |
| Sleep efficiency | 79.558 (12.294) | 77.054 (14.572) | 82.062 (9.205) | 0.202 |
| Hospital Anxiety and Depression Scale | ||||
| Anxiety | 7.65 (3.711) | 7.85 (3.543) | 7.45 (3.953) | 0.738 |
| Depression | 6.85 (3.446) | 6.60 (3.299) | 7.10 (3.655) | 0.652 |
| Epworth Sleepiness Scale | 12.33 (5.264) | 10.40 (4.784) | 14.25 (5.118) | 0.019 |
| Satisfaction with Life Scale | 20.00 (5.875) | 19.55 (6.278) | 20.45 (5.568) | 0.634 |
| Multidimensional Fatigue Inventory | ||||
| MFI-general | 13.17 (3.411) | 13.65 (3.014) | 12.70 (3.785) | 0.385 |
| MFI-physical | 11.88 (1.362) | 12.35 (1.182) | 11.40 (1.392) | 0.025 |
| MFI-mental | 11.70 (3.360) | 11.50 (3.253) | 11.90 (3.538) | 0.712 |
| MFI-activities | 12.20 (3.314) | 12.20 (3.205) | 10.20 (3.503) | 1.000 |
| MFI-motivation | 11.30 (2.366) | 10.70 (2.203) | 11.90 (2.426) | 0.110 |
| MFI-total score | 60.25 (10.744) | 60.40 (10.096) | 60.10 (11.616) | 0.931 |
| Time Points | Time Effect | Time × Group Effect | p-Value d | |||
|---|---|---|---|---|---|---|
| FIR-Pajamas Group (n = 20) | Sham-Pajamas Group (n = 20) | |||||
| Mean (SE) a | Cohen’s d b | Mean (SE) | Cohen’s db | dppc2c | ||
| Pittsburgh Sleep Quality Index | 0.439 | |||||
| Baseline | 9.50 (0.712) | 9.15 (0.634) | ||||
| Week 2 | 8.99 (0.804) | 0.15 | 7.43 (0.536) | 0.655 | −0.393 | 0.112 |
| Week 4 | 8.31 (0.748) | 0.364 | 6.95 (0.628) | 0.78 | −0.328 | 0.273 |
| Week 6 | 8.34 (0.743) | 0.356 | 7.28 (0.461) | 0.754 | −0.231 | 0.255 |
| Insomnia Severity Index | 0.161 | |||||
| Baseline | 14.30 (0.922) | 15.10 (1.049) | ||||
| Week 2 | 13.10 (1.054) | 0.271 | 12.29 (1.053) | 0.598 | −0.357 | 0.167 |
| Week 4 | 11.09 (0.993) | 0.749 | 10.30 (0.993) | 1.051 | −0.353 | 0.254 |
| Week 6 | 10.65 (0.930) | 0.881 | 11.30 (1.332) | 0.709 | −0.033 | 0.917 |
| Seven-Day Sleep Diary | ||||||
| Sleep onset latency | 0.565 | |||||
| Baseline | 36.614 (5.810) | 40.535 (6.605) | ||||
| Week 6 | 31.752 (6.173) | 0.181 | 31.973 (4.273) | 0.344 | −0.13 | 0.565 |
| Wakefulness after sleep onset | 0.176 | |||||
| Baseline | 46.858 (9.737) | 27.907 (5.144) | ||||
| Week 6 | 24.052 (4.727) | 0.666 | 16.715 (3.103) | 0.589 | 0.327 | 0.176 |
| Total sleep time | 0.852 | |||||
| Baseline | 361.617 (17.162) | 389.752 (13.941) | ||||
| Week 6 | 393.220 (18.307) | 0.398 | 418.719 (11.630) | 0.505 | 0.037 | 0.852 |
| Sleep efficiency | 0.648 | |||||
| Baseline | 77.054 (3.175) | 82.062 (2.006) | ||||
| Week 6 | 81.318 (3.004) | 0.308 | 85.219 (1.536) | 0.395 | 0.091 | 0.648 |
| Time Points | Time Effect | Time × Group Effect | p-Value d | |||
|---|---|---|---|---|---|---|
| FIR-Pajamas Group (n = 20) | Sham-Pajamas Group (n = 20) | |||||
| Mean (SE) a | Cohen’s d b | Mean (SE) | Cohen’s d b | dppc2 c | ||
| HADS Anxiety | 0.417 | |||||
| Baseline | 7.85 (0.772) | 7.45 (0.862) | ||||
| Week 2 | 8.32 (0.762) | −0.137 | 7.15 (1.095) | 0.068 | −0.206 | 0.460 |
| Week 4 | 6.99 (0.805) | 0.244 | 7.40 (0.878) | 0.013 | 0.217 | 0.472 |
| Week 6 | 6.92 (0.805) | 0.264 | 6.66 (0.869) | 0.204 | 0.037 | 0.891 |
| HADS Depression | 0.767 | |||||
| Baseline | 6.60 (0.719) | 7.10 (0.797) | ||||
| Week 2 | 7.51 (0.970) | −0.238 | 7.22 (0.833) | −0.033 | −0.228 | 0.435 |
| Week 4 | 7.42 (1.198) | −0.186 | 6.66 (0.926) | 0.114 | −0.364 | 0.306 |
| Week 6 | 7.54 (0.958) | −0.57 | 7.07 (1.050) | 0.007 | −0.280 | 0.391 |
| Epworth Sleepiness Scale | 0.042 | |||||
| Baseline | 10.40 (1.043) | 14.25 (1.116) | ||||
| Week 2 | 10.57 (1.135) | −0.035 | 11.98 (1.224) | 0.433 | −0.495 | 0.046 |
| Week 4 | 9.23 (1.032) | 0.252 | 10.34 (1.267) | 0.732 | −0.556 | 0.041 |
| Week 6 | 7.49 (1.346) | 0.54 | 10.31 (1.139) | 0.781 | −0.209 | 0.532 |
| Satisfaction with Life Scale | 0.364 | |||||
| Baseline | 19.55 (1.368) | 20.45 (1.213) | ||||
| Week 2 | 19.26 (1.392) | −0.047 | 20.60 (1.388) | −0.026 | −0.075 | 0.694 |
| Week 4 | 20.19 (1.690) | 0.093 | 20.04 (1.404) | 0.07 | 0.178 | 0.454 |
| Week 6 | 19.90 (1.549) | 0.054 | 18.94 (1.646) | 0.234 | 0.315 | 0.179 |
| Multidimensional Fatigue Inventory | ||||||
| MFI-general | 0.328 | |||||
| Baseline | 13.65 (0.657) | 12.70 (0.825) | ||||
| Week 2 | 14.25 (0.594) | −0.214 | 12.16 (0.665) | 0.161 | −0.335 | 0.264 |
| Week 4 | 13.20 (0.585) | 0.162 | 12.15 (0.577) | 0.173 | −0.029 | 0.908 |
| Week 6 | 13.31 (0.603) | 0.121 | 12.94 (0.690) | −0.071 | 0.17 | 0.635 |
| MFI-physical | 0.106 | |||||
| Baseline | 12.35 (0.258) | 11.40 (0.303) | ||||
| Week 2 | 11.83 (0.361) | 0.371 | 12.11 (0.312) | −0.516 | 0.958 | 0.031 |
| Week 4 | 12.21 (0.398) | 0.093 | 12.34 (0.372) | −0.62 | 0.841 | 0.075 |
| Week 6 | 12.11 (0.504) | 0.134 | 12.31 (0.350) | −0.622 | 0.896 | 0.123 |
| MFI-mental | 0.906 | |||||
| Baseline | 11.50 (0.709) | 11.90 (0.771) | ||||
| Week 2 | 12.27 (0.677) | −0.248 | 12.44 (0.778) | −0.156 | −0.068 | 0.816 |
| Week 4 | 11.47 (0.661) | 0.01 | 11.35 (0.726) | 0.164 | −0.154 | 0.476 |
| Week 6 | 12.07 (0.786) | −0.17 | 12.39 (0.805) | −0.139 | −0.024 | 0.947 |
| MFI-activities | 0.715 | |||||
| Baseline | 12.20 (0.699) | 12.20 (0.764) | ||||
| Week 2 | 12.84 (0.716) | −0.202 | 12.28 (0.591) | −0.026 | −0.168 | 0.408 |
| Week 4 | 12.31 (0.789) | −0.033 | 12.38 (0.644) | −0.057 | 0.021 | 0.901 |
| Week 6 | 12.85 (0.695) | −0.209 | 13.45 (0.695) | −0.383 | 0.18 | 0.548 |
| MFI-motivation | 0.671 | |||||
| Baseline | 10.70 (0.480) | 11.90 (0.529) | ||||
| Week 2 | 11.61 (0.586) | −0.38 | 12.20 (0.546) | −0.125 | −0.265 | 0.447 |
| Week 4 | 11.38 (0.562) | −0.291 | 11.85 (0.450) | 0.023 | −0.317 | 0.287 |
| Week 6 | 11.77 (0.711) | −0.394 | 12.20 (0.511) | −0.129 | −0.334 | 0.372 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, S.-C.; Cheung, T.-W.; Yu, B.Y.-M.; Chan, M.-Y.; Yeung, W.-F.; Li, L. Improving Sleep with Far-Infrared-Emitting Pajamas: A Pilot Randomized Controlled Trial. Int. J. Environ. Res. Public Health 2023, 20, 3870. https://doi.org/10.3390/ijerph20053870
Chen S-C, Cheung T-W, Yu BY-M, Chan M-Y, Yeung W-F, Li L. Improving Sleep with Far-Infrared-Emitting Pajamas: A Pilot Randomized Controlled Trial. International Journal of Environmental Research and Public Health. 2023; 20(5):3870. https://doi.org/10.3390/ijerph20053870
Chicago/Turabian StyleChen, Shu-Cheng, Tin-Wai Cheung, Branda Yee-Man Yu, Mei-Yan Chan, Wing-Fai Yeung, and Li Li. 2023. "Improving Sleep with Far-Infrared-Emitting Pajamas: A Pilot Randomized Controlled Trial" International Journal of Environmental Research and Public Health 20, no. 5: 3870. https://doi.org/10.3390/ijerph20053870
APA StyleChen, S.-C., Cheung, T.-W., Yu, B. Y.-M., Chan, M.-Y., Yeung, W.-F., & Li, L. (2023). Improving Sleep with Far-Infrared-Emitting Pajamas: A Pilot Randomized Controlled Trial. International Journal of Environmental Research and Public Health, 20(5), 3870. https://doi.org/10.3390/ijerph20053870







