Kinesio Taping as a Therapeutic Tool for Masticatory Myofascial Pain Syndrome—An Insight View
Abstract
1. Introduction
2. Search Study and Selection Criteria
3. Kinesio Taping
3.1. Background of Kinesio Taping
3.2. Characters of Kinesio Taping
3.3. Types of Kinesio Taping
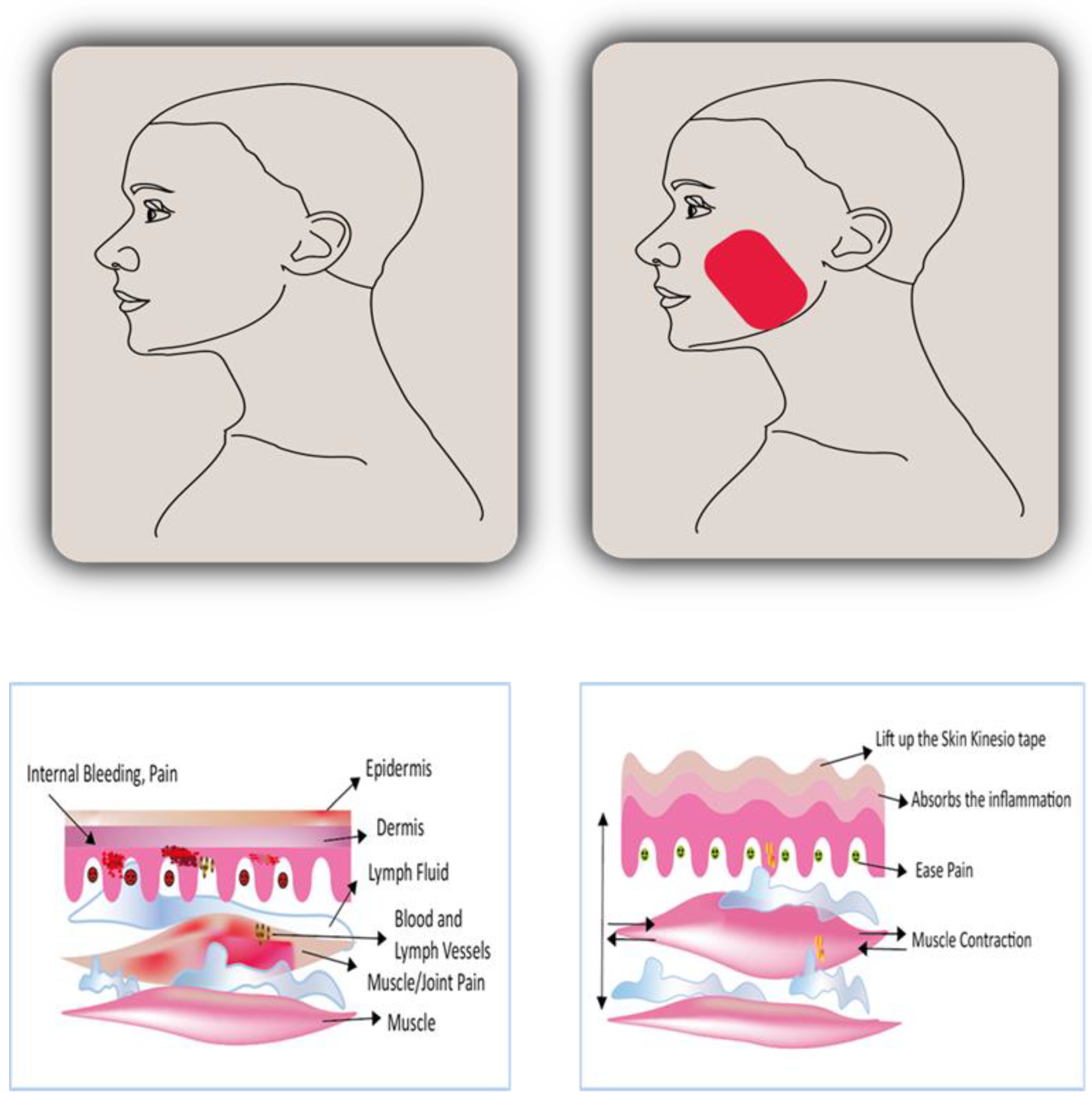
4. Mechanism of Action of Kinesio Taping
5. Clinical Application of Kinesio Taping for Myofascial Pain Syndrome
6. Limitations and Research Gap
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Giamberardino, M.A.; Affaitati, G.; Fabrizio, A.; Costantini, R. Myofascial pain syndromes and their evaluation. Best Pract. Res. Clin. Rheumatol. 2011, 25, 185–198. [Google Scholar] [CrossRef]
- Montes-Carmona, J.-F.; Gonzalez-Perez, L.-M.; Infante-Cossio, P. Treatment of Localized and Referred Masticatory Myofascial Pain with Botulinum Toxin Injection. Toxins 2020, 13, 6. [Google Scholar] [CrossRef]
- Schiffman, E.; Ohrbach, R.; Truelove, E.; Look, J.; Anderson, G.; Goulet, J.-P.; List, T.; Svensson, P.; Gonzalez, Y.; Lobbezoo, F.; et al. Diagnostic Criteria for Temporomandibular Disorders (DC/TMD) for Clinical and Research Applications: Recommendations of the International RDC/TMD Consortium Network* and Orofacial Pain Special Interest Group. J. Oral Facial Pain Headache 2014, 28, 6–27. [Google Scholar] [CrossRef]
- Afrashtehfar, K.I.; Belser, U.C. Prevention and Management of Cheek and/or Tongue Biting Related to Posterior Implant-Supported Fixed Dental Prostheses (ISFDPs). J. Prosthodont. 2019, 28, 837–839. [Google Scholar] [CrossRef]
- Bathi, R.J.; Taneja, N.; Parveen, S. Rheumatoid Arthritis of TMJ—A Diagnostic Dilemma? Dent. Update 2004, 31, 167–174. [Google Scholar] [CrossRef]
- Saxena, A.; Chansoria, M.; Tomar, G.; Kumar, A. Myofascial pain syndrome: An overview. J. Pain Palliat. Care Pharmacother. 2015, 29, 16–21. [Google Scholar] [CrossRef]
- Gerwin, R.D. Diagnosis of myofascial pain syndrome. Phys. Med. Rehabilitation Clin. N. Am. 2014, 25, 341–355. [Google Scholar] [CrossRef]
- Elbarbary, M.; Goldberg, M.; Tenenbaum, H.C.; Lam, D.K.; Freeman, B.V.; Pustaka, D.J.; Mock, D.; Beyene, J.; Azarpazhooh, A. Assessment of Concordance between Chairside Ultrasonography and Digital Palpation in Detecting Myofascial Trigger Points in Masticatory Myofascial Pain Syndrome. J. Endod. 2023, 49, 129–136. [Google Scholar] [CrossRef]
- Ferrillo, M.; Giudice, A.; Marotta, N.; Fortunato, F.; Di Venere, D.; Ammendolia, A.; Fiore, P.; de Sire, A. Pain Management and Rehabilitation for Central Sensitization in Temporomandibular Disorders: A Comprehensive Review. Int. J. Mol. Sci. 2022, 23, 12164. [Google Scholar] [CrossRef]
- Kanhachon, W.; Boonprakob, Y. The correlation between scapulocostal syndrome and masticatory myofascial pain on selected pain and functional parameters- an observational study. J. Bodyw. Mov. Ther. 2022, 29, 198–205. [Google Scholar] [CrossRef]
- Kurt, A.; Guner-Onur, S.; Bilmenoglu, C.; Memisoglu, G.; Cilingir, A.A. Efficacy of different treatment methods in patients with myofascial pain syndrome. Lasers Dent. Sci. 2020, 4, 181–186. [Google Scholar] [CrossRef]
- Afrashtehfar, K.I.; Schimmel, M. Muscular activity may improve in edentulous patients after implant treatment. Evid. Based Dent. 2016, 17, 119–120. [Google Scholar] [CrossRef]
- Lavelle, E.D.; Lavelle, W.; Smith, H.S. Myofascial trigger points. Anesthesiol. Clin. 2007, 25, 841–851, vii–iii. [Google Scholar] [CrossRef]
- Elbarbary, M.; Oren, A.; Goldberg, M.; Freeman, B.V.; Mock, D.; Tenenbaum, H.C.; Azarpazhooh, A. Masticatory Myofascial Pain Syndrome: Implications for Endodontists. J. Endod. 2022, 48, 55–69. [Google Scholar] [CrossRef]
- de-la-Hoz, J.L.; de-Pedro, M.; Martín-Fontelles, I.; Mesa-Jimenez, J.; Chivato, T.; Bagües, A. Efficacy of botulinum toxin type A in the management of masticatory myofascial pain: A retrospective clinical study. J. Am. Dent. Assoc. 2022, 153, 683–691. [Google Scholar] [CrossRef]
- Borg-Stein, J.; Iaccarino, M.A. Myofascial pain syndrome treatments. Phys. Med. Rehabil. Clin. N. Am. 2014, 25, 357–374. [Google Scholar] [CrossRef]
- Afrashtehfar, K.I.; Huynh, N. Five Things to Know About Sleep Bruxism. J. N. J. Dent. Assoc. 2016, 87, 14. [Google Scholar]
- Arrebola, L.S.; Teixeira de Carvalho, R.; Lam Wun, P.Y.; Rizzi de Oliveira, P.; Firmo dos Santos, J.; Coutinho de Oliveira, V.G.; Pinfildi, C.E. Investigation of different application techniques for Kinesio Taping® with an accompanying exercise protocol for improvement of pain and functionality in patients with patellofemoral pain syndrome: A pilot study. J. Bodyw. Mov. Ther. 2020, 24, 47–55. [Google Scholar] [CrossRef]
- Brockmann, R.; Klein, H.-M. Pain-diminishing effects of Kinesio® taping after median sternotomy. Physiother. Theory Pract. 2018, 34, 433–441. [Google Scholar] [CrossRef]
- Tantawy, S.A.; Abdelbasset, W.K.; Nambi, G.; Kamel, D.M. Comparative Study Between the Effects of Kinesio Taping and Pressure Garment on Secondary Upper Extremity Lymphedema and Quality of Life Following Mastectomy: A Randomized Controlled Trial. Integr. Cancer Ther. 2019, 18, 1534735419847276. [Google Scholar] [CrossRef]
- Donec, V.; Kubilius, R. The effectiveness of Kinesio Taping® for pain management in knee osteoarthritis: A randomized, double-blind, controlled clinical trial. Ther. Adv. Musculoskelet. Dis. 2019, 11, 1759720X19869135. [Google Scholar] [CrossRef]
- Thelen, M.D.; Dauber, J.A.; Stoneman, P.D. The clinical efficacy of kinesio tape for shoulder pain: A randomized, double-blinded, clinical trial. J. Orthop. Sports Phys. Ther. 2008, 38, 389–395. [Google Scholar] [CrossRef]
- Cho, H.; Kim, E.-H.; Kim, J.; Yoon, Y.W. Kinesio taping improves pain, range of motion, and proprioception in older patients with knee osteoarthritis: A randomized controlled trial. Am. J. Phys. Med. Rehabil. 2015, 94, 192–200. [Google Scholar] [CrossRef]
- Bae, Y. Change the Myofascial Pain and Range of Motion of the Temporomandibular Joint Following Kinesio Taping of Latent Myofascial Trigger Points in the Sternocleidomastoid Muscle. J. Phys. Ther. Sci. 2014, 26, 1321–1324. [Google Scholar] [CrossRef]
- Cheshmi, B.; Keyhan, S.O.; Rayegani, S.M.; Kim, S.-G.; Ozunlu Pekyavas, N.; Ramezanzade, S. A literature review of applications of Kinesio Taping® in the craniomaxillofacial region. CRANIO® 2021, 1–8. [Google Scholar] [CrossRef]
- Sharma, J.; Jamali, S.; Rao, S.K. A comparative analysis of efficacy of Kinesio taping versus conventional therapy in Bell’s palsy by using House-Brackmann grading system. Int. J. Recent Sci. Res. 2019, 10, 31177–31179. [Google Scholar]
- Afrashtehfar, K.I.; Afrashtehfar, C.D.M.; Huynh, N. Managing a patient with sleep bruxism. J. Can. Dent. Assoc. 2014, 80, e48. [Google Scholar]
- Lietz-Kijak, D.; Kopacz, Ł.; Ardan, R.; Grzegocka, M.; Kijak, E. Assessment of the Short-Term Effectiveness of Kinesiotaping and Trigger Points Release Used in Functional Disorders of the Masticatory Muscles. Pain Res. Manag. 2018, 2018, 5464985. [Google Scholar] [CrossRef]
- Wu, W.-T.; Hong, C.-Z.; Chou, L.-W. The Kinesio Taping Method for Myofascial Pain Control. Evid. Based Complement Altern. Med. 2015, 2015, 950519. [Google Scholar] [CrossRef]
- Jaroń, A.; Jedliński, M.; Grzywacz, E.; Mazur, M.; Trybek, G. Kinesiology Taping as an Innovative Measure against Post-Operative Complications after Third Molar Extraction-Systematic Review. J. Clin. Med. 2020, 9, 3988. [Google Scholar] [CrossRef]
- Yun, H.; Lee, J.-H.; Choi, I.-R. Effects of Kinesiology Taping on Shoulder Posture and Peak Torque in Junior Baseball Players with Rounded Shoulder Posture: A Pilot Study. Life 2020, 10, 139. [Google Scholar] [CrossRef]
- Pihut, M.; Kulesa-Mrowiecka, M. The Emergencies in the Group of Patients with Temporomandibular Disorders. J. Clin. Med. 2022, 12, 298. [Google Scholar] [CrossRef]
- El-Tallawy, S.N.; Nalamasu, R.; Salem, G.I.; LeQuang, J.A.K.; Pergolizzi, J.V.; Christo, P.J. Management of Musculoskeletal Pain: An Update with Emphasis on Chronic Musculoskeletal Pain. Pain Ther. 2021, 10, 181–209. [Google Scholar] [CrossRef]
- Mao, H.-Y.; Hu, M.-T.; Yen, Y.-Y.; Lan, S.-J.; Lee, S.-D. Kinesio Taping Relieves Pain and Improves Isokinetic Not Isometric Muscle Strength in Patients with Knee Osteoarthritis—A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2021, 18, 10440. [Google Scholar] [CrossRef]
- Tusharbhai, D.M.; Baliga, M.; Mishra, A. Versatility of Kinesio-Taping in Postoperative Swelling, Pain, and Trismus After Surgical Removal of Impacted Lower Third Molars. J. Orofac. Sci. 2020, 12, 126. [Google Scholar] [CrossRef]
- Banerjee, G.; Briggs, M.; Johnson, M.I. The immediate effects of kinesiology taping on cutaneous blood flow in healthy humans under resting conditions: A randomised controlled repeated-measures laboratory study. PLoS ONE 2020, 15, e0229386. [Google Scholar] [CrossRef]
- Dilek, B.; Batmaz, İ.; Akif Sarıyıldız, M.; Şahin, E.; Bulut, D.; Akalın, E.; Çevik, R.; Nas, K. Effectiveness of training about kinesiotaping in myofascial pain syndrome: A prospective, single-blind, randomized-controlled study. Turk. J. Phys. Med. Rehabil. 2021, 67, 17–24. [Google Scholar] [CrossRef]
- Chao, Y.W.; Lin, J.J.; Yang, J.L.; Wang, W.T.-J. Kinesio taping and manual pressure release: Short-term effects in subjects with myofasical trigger point. J. Hand Ther. 2016, 29, 23–29. [Google Scholar] [CrossRef]
- Erpala, F.; Ozturk, T.; Zengin, E.C.; Bakir, U. Early Results of Kinesio Taping and Steroid Injections in Elbow Lateral Epicondylitis: A Randomized, Controlled Study. Medicina 2021, 57, 306. [Google Scholar] [CrossRef]
- Cupler, Z.A.; Alrwaily, M.; Polakowski, E.; Mathers, K.S.; Schneider, M.J. Taping for conditions of the musculoskeletal system: An evidence map review. Chiropr. Man. Ther. 2020, 28, 52. [Google Scholar] [CrossRef]
- Lemos, T.V.; Pereira, K.C.; Protássio, C.C.; Lucas, L.B.; Matheus, J.P.C. The effect of Kinesio Taping on handgrip strength. J. Phys. Ther. Sci. 2015, 27, 567–570. [Google Scholar] [CrossRef]
- Liu, K.; Yin, L.; Ma, Z.; Yu, B.; Ma, Y.; Huang, L. Effect of Different Kinesio Taping Interventions on the Local Thresholds of Current Perception and Pressure Pain in Healthy Adults. Front. Physiol. 2020, 11, 596159. [Google Scholar] [CrossRef]
- Ristow, O.; Hohlweg-Majert, B.; Kehl, V.; Koerdt, S.; Hahnefeld, L.; Pautke, C. Does elastic therapeutic tape reduce postoperative swelling, pain, and trismus after open reduction and internal fixation of mandibular fractures? J. Oral Maxillofac. Surg. 2013, 71, 1387–1396. [Google Scholar] [CrossRef]
- Artioli, D.P.; Bertolini, G.R.F. Kinesio taping: Application and results on pain: Systematic review. Fisioter. Pesqui. 2014, 21, 94–99. [Google Scholar] [CrossRef]
- Paoloni, M.; Bernetti, A.; Fratocchi, G.; Mangone, M.; Parrinello, L.; Del Pilar Cooper, M.; Sesto, L.; Di Sante, L.; Santilli, V. Kinesio Taping applied to lumbar muscles influences clinical and electromyographic characteristics in chronic low back pain patients. Eur. J. Phys. Rehabil. Med. 2011, 47, 237–244. [Google Scholar]
- Abdelfattah, A.; Kattabei, O.; Nasef, S.; Semaya, A. Effect of kinesio tape in myofascial pain syndrome ‘Randomized Control Trial’. Physiotherapy 2016, 102, e140. [Google Scholar] [CrossRef]
- Lumbroso, D.; Ziv, E.; Vered, E.; Kalichman, L. The effect of kinesio tape application on hamstring and gastrocnemius muscles in healthy young adults. J. Bodyw. Mov. Ther. 2014, 18, 130–138. [Google Scholar] [CrossRef]
- Selva, F.; Pardo, A.; Aguado, X.; Montava, I.; Gil-Santos, L.; Barrios, C. A study of reproducibility of kinesiology tape applications: Review, reliability and validity. BMC Musculoskelet. Disord. 2019, 20, 153. Available online: https://bmcmusculoskeletdisord.biomedcentral.com/articles/10.1186/s12891-019-2533-0 (accessed on 12 October 2022). [CrossRef]
- Akbaş, E.; Atay, A.O.; Yüksel, I. The effects of additional kinesio taping over exercise in the treatment of patellofemoral pain syndrome. Acta Orthop. Traumatol. Turc. 2011, 45, 335–341. [Google Scholar] [CrossRef]
- Kaya, E.; Zinnuroglu, M.; Tugcu, I. Kinesio taping compared to physical therapy modalities for the treatment of shoulder impingement syndrome. Clin. Rheumatol. 2011, 30, 201–207. [Google Scholar] [CrossRef]
- Emérito, T.M.; Silva, J.A.S.; Furlan, R.M.M.M. O uso da bandagem elástica adesiva para alívio da dor no tratamento das disfunções temporomandibulares: Revisão sistemática com metanálise. Audiol. Commun. Res. 2022, 27, e2631. [Google Scholar] [CrossRef]
- Coskun Benlidayi, I.; Salimov, F.; Kurkcu, M.; Guzel, R. Kinesio Taping for temporomandibular disorders: Single-blind, randomized, controlled trial of effectiveness. J. Back Musculoskelet. Rehabil. 2016, 29, 373–380. [Google Scholar] [CrossRef]
- Keskinruzgar, A.; Kucuk, A.O.; Yavuz, G.Y.; Koparal, M.; Caliskan, Z.G.; Utkun, M. Comparison of kinesio taping and occlusal splint in the management of myofascial pain in patients with sleep bruxism. J. Back Musculoskelet. Rehabil. 2019, 32, 1–6. [Google Scholar] [CrossRef]
- Guarda-Nardini, L.; Olivo, M.; Ferronato, G.; Salmaso, L.; Bonnini, S.; Manfredini, D. Treatment effectiveness of arthrocentesis plus hyaluronic acid injections in different age groups of patients with temporomandibular joint osteoarthritis. J. Oral Maxillofac. Surg. 2012, 70, 2048–2056. [Google Scholar] [CrossRef]
- Yılmaz, N.; Erdal, A.; Demir, O. A comparison of dry needling and kinesiotaping therapies in myofascial pain syndrome: A randomized clinical study. Turk. J. Phys. Med. Rehabil. 2020, 66, 351–359. [Google Scholar] [CrossRef]
- Yasar, M.F.; Yaksi, E.; Kurul, R.; Alisik, T.; Seker, Z. Comparison of dry needling and kinesio taping methods in the treatment of myofascial pain syndrome: A single blinded randomised controlled study. Int. J. Clin. Pract. 2021, 75, e14561. [Google Scholar] [CrossRef]
- Dec-Ćwiek, M.; Porębska, K.; Sawczyńska, K.; Kubala, M.; Witkowska, M.; Zmijewska, K.; Antczak, J.; Pera, J. KinesioTaping after botulinum toxin type A for cervical dystonia in adult patients. Brain Behav. 2022, 12, e2541. [Google Scholar] [CrossRef]

| S. No. | Types of Kinesio Taping | Features | Reference |
|---|---|---|---|
| 1. | KinesioTex Classic | Universal and best option since it can be used in any situation and is most suited for healthy skin. | [23] |
| 2. | KinesioTex Performance+ | Polyester and cotton blends are excellent for delicate skin when more significant tape tensions are needed. | [21] |
| 3. | KinesioTex Gold | For low-tension applications and uses a specific distribution of glue accessible exclusively to qualified specialists that provide high adhesion without needing an enormous surface area. | [23] |
| 4. | KinesioTex Gold Light Touch Plus | used for short-term treatments and is often used on youngsters and the elderly with sensitive skin. | [21] |
| 5. | Kinesio Equine | It can be applied straight to horsehair and has a flavor that animals would not eat. | [33] |
| 6. | Kinesio Canine | For dogs, it works nicely with their hair. | [33] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alqahtani, A.S.; Parveen, S. Kinesio Taping as a Therapeutic Tool for Masticatory Myofascial Pain Syndrome—An Insight View. Int. J. Environ. Res. Public Health 2023, 20, 3872. https://doi.org/10.3390/ijerph20053872
Alqahtani AS, Parveen S. Kinesio Taping as a Therapeutic Tool for Masticatory Myofascial Pain Syndrome—An Insight View. International Journal of Environmental Research and Public Health. 2023; 20(5):3872. https://doi.org/10.3390/ijerph20053872
Chicago/Turabian StyleAlqahtani, Ahmed Shaher, and Sameena Parveen. 2023. "Kinesio Taping as a Therapeutic Tool for Masticatory Myofascial Pain Syndrome—An Insight View" International Journal of Environmental Research and Public Health 20, no. 5: 3872. https://doi.org/10.3390/ijerph20053872
APA StyleAlqahtani, A. S., & Parveen, S. (2023). Kinesio Taping as a Therapeutic Tool for Masticatory Myofascial Pain Syndrome—An Insight View. International Journal of Environmental Research and Public Health, 20(5), 3872. https://doi.org/10.3390/ijerph20053872







