Understanding Post-Adoption Behavioral Intentions of Mobile Health Service Users: An Empirical Study during COVID-19
Abstract
:1. Introduction
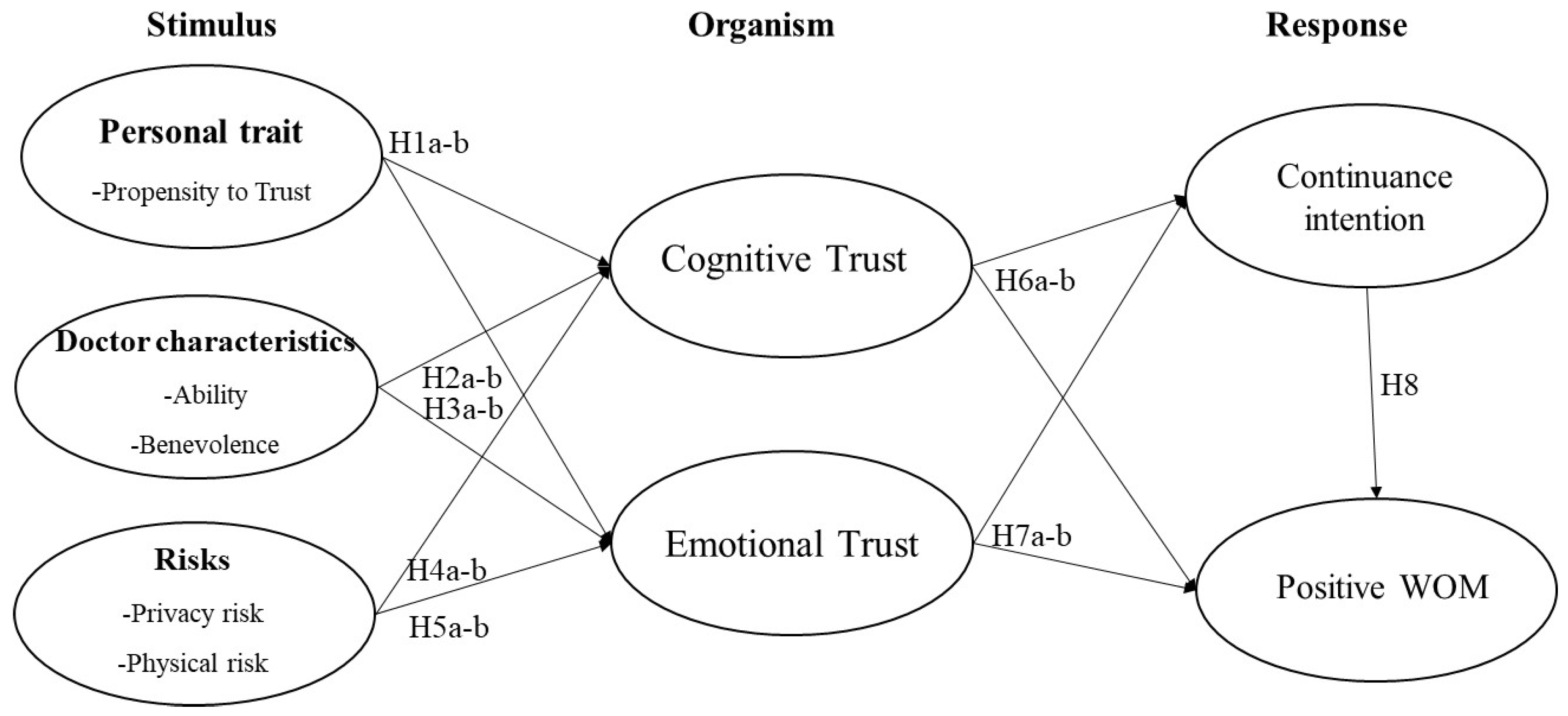
What effects do user personality traits, doctor characteristics, and perceived risks have on user post-adoption behavioral intentions via cognitive trust and emotional trust in the m-Health service context?
2. Conceptual Framework
2.1. S-O-R Framework
2.2. Cognitive Trust and Emotional Trust
3. Research Model and Hypotheses
3.1. Antecedents of Cognitive and Emotional Trust in the m-Health Platform
3.2. Roles of Cognitive and Emotional Trust in m-Health Platforms
3.3. Relationship between Continuance Intention and Positive WOM
4. Methodology
4.1. Research Approach
4.2. Research Context
4.3. Measurements
4.4. Survey Design and Data Collection
4.5. Sample Profiles
5. Results
5.1. Measurement Model
5.2. Common Method Bias Assessment
5.3. Structural Model
5.3.1. Goodness of Fit
5.3.2. Path Coefficient
5.3.3. Coefficient of Determination (R2)
5.3.4. Effect Size (f2)
5.3.5. Prediction Relevance (Q2)
6. Discussion
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Istepanian, R.S.H. Mobile Health (m-Health) in Retrospect: The Known Unknowns. Int. J. Environ. Res. Public Health 2022, 19, 3747. [Google Scholar] [CrossRef] [PubMed]
- Sujarwoto, S.; Augia, T.; Dahlan, H.; Sahputri, R.A.M.; Holipah, H.; Maharani, A. COVID-19 Mobile Health Apps: An Overview of Mobile Applications in Indonesia. Front. Public Health 2022, 10, 879695. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.; Xie, X.; Yang, L.; Xu, X.; Cai, Y.; Wang, T.; Xie, X. Mobile health technology combats COVID-19 in China. J. Infect. 2021, 82, 159–198. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.-W.; Chiou, C.-C.; Su, C.-H.; Wu, C.-C.; Tsai, S.-C.; Lin, T.-K.; Hsu, C.-N. Measuring Mobile Phone Application Usability for Anticoagulation from the Perspective of Patients, Caregivers, and Healthcare Professionals. Int. J. Environ. Res. Public Health 2022, 19, 10136. [Google Scholar] [CrossRef]
- Varshney, U. Pervasive Healthcare Computing: EMR/EHR, Wireless and Health Monitoring; Springer Science & Business Media: New York, NY, USA, 2009. [Google Scholar]
- Asadzadeh, A.; Kalankesh, L.R. A scope of mobile health solutions in COVID-19 pandemics. Inform. Med. Unlocked 2021, 23, 100558. [Google Scholar] [CrossRef]
- Salehinejad, S.; Kalhori, S.R.N.; Gohari, S.H.; Bahaadinbeigy, K.; Fatehi, F. A review and content analysis of national apps for COVID-19 management using Mobile Application Rating Scale (MARS). Inform. Health Soc. Care 2020, 46, 42–55. [Google Scholar] [CrossRef]
- Yuduang, N.; Ong, A.K.S.; Vista, N.B.; Prasetyo, Y.T.; Nadlifatin, R.; Persada, S.F.; Gumasing, M.J.J.; German, J.D.; Robas, K.P.E.; Chuenyindee, T.; et al. Utilizing Structural Equation Modeling–Artificial Neural Network Hybrid Approach in Determining Factors Affecting Perceived Usability of Mobile Mental Health Application in the Philippines. Int. J. Environ. Res. Public Health 2022, 19, 6732. [Google Scholar] [CrossRef]
- Zhang, X.; Liu, S.; Wang, L.; Zhang, Y.; Wang, J. Mobile health service adoption in China: Integration of theory of planned behavior, protection motivation theory and personal health differences. Online Inf. Rev. 2019, 44, 1–23. [Google Scholar] [CrossRef]
- Wan, Y.; Zhang, Y.; Yan, M. What influences patients’ willingness to choose in online health consultation? An empirical study with PLS–SEM. Ind. Manag. Data Syst. 2020, 120, 2423–2446. [Google Scholar] [CrossRef]
- Wang, H.; Liang, L.; Du, C.; Wu, Y. Implementation of Online Hospitals and Factors Influencing the Adoption of Mobile Medical Services in China: Cross-Sectional Survey Study. JMIR mHealth uHealth 2021, 9, e25960. [Google Scholar] [CrossRef]
- Zhao, Y.; Ni, Q.; Zhou, R. What factors influence the mobile health service adoption? A meta-analysis and the moderating role of age. Int. J. Inf. Manag. 2018, 43, 342–350. [Google Scholar] [CrossRef]
- Shareef, M.A.; Kumar, V.; Kumar, U. Predicting mobile health adoption behaviour: A demand side perspective. J. Cust. Behav. 2014, 13, 187–205. [Google Scholar] [CrossRef] [Green Version]
- Yan, M.; Filieri, R.; Raguseo, E.; Gorton, M. Mobile apps for healthy living: Factors influencing continuance intention for health apps. Technol. Forecast. Soc. Chang. 2021, 166, 120644. [Google Scholar] [CrossRef]
- Meng, F.; Guo, X.; Peng, Z.; Ye, Q.; Lai, K.-H. Trust and elderly users’ continuance intention regarding mobile health services: The contingent role of health and technology anxieties. Inf. Technol. People 2021, 35, 259–280. [Google Scholar] [CrossRef]
- Hong, Z.; Deng, Z.; Zhang, W. Examining factors affecting patients trust in online healthcare services in China: The moderating role of the purpose of use. Health Inform. J. 2018, 25, 1647–1660. [Google Scholar] [CrossRef] [PubMed]
- Oppong, E.; Hinson, R.E.; Adeola, O.; Muritala, O.; Kosiba, J.P. The effect of mobile health service quality on user satisfaction and continual usage. Total. Qual. Manag. Bus. Excell. 2021, 32, 177–198. [Google Scholar] [CrossRef]
- Luo, Y.; Wang, G.; Li, Y.; Ye, Q. Examining Protection Motivation and Network Externality Perspective Regarding the Continued Intention to Use M-Health Apps. Int. J. Environ. Res. Public Health 2021, 18, 5684. [Google Scholar] [CrossRef]
- Gountas, J.; Gountas, S. Personality orientations, emotional states, customer satisfaction, and intention to repurchase. J. Bus. Res. 2007, 60, 72–75. [Google Scholar] [CrossRef]
- Jiang, Y.; Lau, A.K. Roles of consumer trust and risks on continuance intention in the sharing economy: An empirical investigation. Electron. Commer. Res. Appl. 2021, 47, 101050. [Google Scholar] [CrossRef]
- Guo, X.; Zhang, X.; Sun, Y. The privacy–personalization paradox in mHealth services acceptance of different age groups. Electron. Commer. Res. Appl. 2016, 16, 55–65. [Google Scholar] [CrossRef]
- Cao, L.; Chongsuvivatwong, V.; McNeil, E.B. The Association between mHealth App Use and Healthcare Satisfaction among Clients at Outpatient Clinics: A Cross-Sectional Study in Inner Mongolia, China. Int. J. Environ. Res. Public Health 2022, 19, 6916. [Google Scholar] [CrossRef] [PubMed]
- Cocosila, M. Role of user a priori attitude in the acceptance of mobile health: An empirical investigation. Electron. Mark. 2012, 23, 15–27. [Google Scholar] [CrossRef]
- Torous, J.; Keshavan, M. COVID-19, mobile health and serious mental illness. Schizophr. Res. 2020, 218, 36–37. [Google Scholar] [CrossRef] [PubMed]
- Xu, X.; Cai, Y.; Wu, S.; Guo, J.; Yang, L.; Lan, J.; Sun, Y.; Wang, B.; Wu, J.; Wang, T.; et al. Assessment of Internet Hospitals in China During the COVID-19 Pandemic: National Cross-Sectional Data Analysis Study. J. Med. Internet Res. 2021, 23, e21825. [Google Scholar] [CrossRef] [PubMed]
- Casaló, L.V.; Flavián, C.; Guinalíu, M. The role of satisfaction and website usability in developing customer loyalty and positive word-of-mouth in the e-banking services. Int. J. Bank Mark. 2008, 26, 399–417. [Google Scholar] [CrossRef]
- Gu, D.; Yang, X.; Li, X.; Jain, H.K.; Liang, C. Understanding the Role of Mobile Internet-Based Health Services on Patient Satisfaction and Word-of-Mouth. Int. J. Environ. Res. Public Health 2018, 15, 1972. [Google Scholar] [CrossRef] [Green Version]
- Li, H.; Liu, Y. Understanding post-adoption behaviors of e-service users in the context of online travel services. Inf. Manag. 2014, 51, 1043–1052. [Google Scholar] [CrossRef]
- Mehrabian, A.; Russell, J.A. An Approach to Environmental Psychology; MIT Press: Cambridge, MA, USA, 1974. [Google Scholar]
- Jacoby, J. Stimulus-Organism-Response Reconsidered: An Evolutionary Step in Modeling (Consumer) Behavior. J. Consum. Psychol. 2002, 12, 51–57. [Google Scholar] [CrossRef]
- Bleier, A.; Eisenbeiss, M. The Importance of Trust for Personalized Online Advertising. J. Retail. 2015, 91, 390–409. [Google Scholar] [CrossRef]
- Wu, Y.-L.; Li, E.Y. Marketing mix, customer value, and customer loyalty in social commerce: A stimulus-organism-response perspective. Internet Res. 2018, 28, 74–104. [Google Scholar] [CrossRef] [Green Version]
- Yang, S.; Zhou, S.; Cheng, X. Why do college students continue to use mobile learning? Learning involvement and self-determination theory. Br. J. Educ. Technol. 2019, 50, 626–637. [Google Scholar] [CrossRef]
- Chopdar, P.K.; Balakrishnan, J. Consumers response towards mobile commerce applications: S-O-R approach. Int. J. Inf. Manag. 2020, 53, 102106. [Google Scholar] [CrossRef]
- Cho, W.-C.; Lee, K.Y.; Yang, S.-B. What makes you feel attached to smartwatches? The stimulus–organism–response (S–O–R) perspectives. Inf. Technol. People 2019, 32, 319–343. [Google Scholar] [CrossRef]
- Brewer, P.; Sebby, A.G. The effect of online restaurant menus on consumers’ purchase intentions during the COVID-19 pandemic. Int. J. Hosp. Manag. 2021, 94, 102777. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Jiang, F.; Lin, P. Influence Mechanism of the Affordances of Chronic Disease Management Apps on Continuance Intention: Questionnaire Study. JMIR mHealth uHealth 2021, 9, e21831. [Google Scholar] [CrossRef] [PubMed]
- Elsotouhy, M.M.; Ghonim, M.A.; Alasker, T.H.; Khashan, M.A. Investigating health and fitness app users’ stickiness, WOM, and continuance intention using SOR model: The moderating role of health consciousness. Int. J. Hum. Comput. Interact. 2022, 1–16. [Google Scholar] [CrossRef]
- Chudhery, M.A.Z.; Safdar, S.; Huo, J.; Rehman, H.U.; Rafique, R. Proposing and empirically investigating a mo-bile-based outpatient healthcare service delivery framework using stimulus–organism–response theory. IEEE Trans. Eng. Manag. 2021, 1–14. [Google Scholar] [CrossRef]
- Wang, T.; Wang, W.; Liang, J.; Nuo, M.; Wen, Q.; Wei, W.; Han, H.; Lei, J. Identifying major impact factors affecting the continuance intention of mHealth: A systematic review and multi-subgroup meta-analysis. NPJ Digit. Med. 2022, 5, 145. [Google Scholar] [CrossRef]
- Song, T.; Deng, N.; Cui, T.; Qian, S.; Liu, F.; Guan, Y.; Yu, P. Measuring Success of Patients’ Continuous Use of Mobile Health Services for Self-management of Chronic Conditions: Model Development and Validation. J. Med. Internet Res. 2021, 23, e26670. [Google Scholar] [CrossRef]
- Kaium, M.A.; Bao, Y.; Alam, M.Z.; Hoque, M.R. Understanding continuance usage intention of mHealth in a developing country: An empirical investigation. Int. J. Pharm. Healthc. Mark. 2020, 14, 251–272. [Google Scholar] [CrossRef]
- Guo, X.; Chen, S.; Zhang, X.; Ju, X.; Wang, X. Exploring Patients’ Intentions for Continuous Usage of mHealth Services: Elaboration-Likelihood Perspective Study. JMIR mHealth uHealth 2020, 8, e17258. [Google Scholar] [CrossRef] [PubMed]
- Hsiao, J.L.; Chen, R.F. Understanding determinants of health care professionals’ perspectives on mobile health con-tinuance and performance. JMIR Med. Inform. 2019, 7, e12350. [Google Scholar] [CrossRef] [PubMed]
- Kim, K.H.; Kim, K.J.; Lee, D.H.; Kim, M.G. Identification of critical quality dimensions for continuance intention in mHealth services: Case study of onecare service. Int. J. Inf. Manag. 2019, 46, 187–197. [Google Scholar] [CrossRef]
- Kim, E.; Han, S. Determinants of Continuance Intention to Use Health Apps among Users over 60: A Test of Social Cognitive Model. Int. J. Environ. Res. Public Health 2021, 18, 10367. [Google Scholar] [CrossRef] [PubMed]
- Birkmeyer, S.; Wirtz, B.W.; Langer, P.F. Determinants of mHealth success: An empirical investigation of the user perspective. Int. J. Inf. Manag. 2021, 59, 102351. [Google Scholar] [CrossRef]
- Wu, C.; Zhou, Y.; Wang, R.; Huang, S.; Yuan, Q. Understanding the Mechanism Between IT Identity, IT Mindfulness and Mobile Health Technology Continuance Intention: An Extended Expectation Confirmation Model. Technol. Forecast. Soc. Chang. 2022, 176, 121449. [Google Scholar] [CrossRef]
- McAllister, D. Affect- and Cognition-Based Trust as Foundations for Interpersonal Cooperation in Organizations. Acad. Manag. J. 1995, 38, 24–59. [Google Scholar] [CrossRef]
- Oliveira, T.; Alhinho, M.; Rita, P.; Dhillon, G. Modelling and testing consumer trust dimensions in e-commerce. Comput. Hum. Behav. 2017, 71, 153–164. [Google Scholar] [CrossRef] [Green Version]
- McKnight, D.H.; Chervany, N.L. What Trust Means in E-Commerce Customer Relationships: An Interdisciplinary Conceptual Typology. Int. J. Electron. Commer. 2001, 6, 35–59. [Google Scholar] [CrossRef] [Green Version]
- Johnson, D.; Grayson, K. Cognitive and affective trust in service relationships. J. Bus. Res. 2005, 58, 500–507. [Google Scholar] [CrossRef]
- Lu, C.; Hu, Y.; Xie, J.; Fu, Q.; Leigh, I.; Governor, S.; Wang, G. The Use of Mobile Health Applications to Improve Patient Experience: Cross-Sectional Study in Chinese Public Hospitals. JMIR mHealth uHealth 2018, 6, e126. [Google Scholar] [CrossRef] [PubMed]
- Gefen, D. E-commerce: The role of familiarity and trust. Omega 2000, 28, 725–737. [Google Scholar] [CrossRef] [Green Version]
- Gefen, D.; Karahanna, E.; Straub, D.W. Trust and TAM in Online Shopping: An Integrated Model. MIS Q. 2003, 27, 51–90. [Google Scholar] [CrossRef]
- Chen, D.; Lai, F.; Lin, Z. A trust model for online peer-to-peer lending: A lender’s perspective. Inf. Technol. Manag. 2014, 15, 239–254. [Google Scholar] [CrossRef]
- Kim, G.; Shin, B.; Lee, H.G. Understanding dynamics between initial trust and usage intentions of mobile banking. Inf. Syst. J. 2009, 19, 283–311. [Google Scholar] [CrossRef]
- Liang, T.-P.; Wu, S.P.-J.; Huang, C.-C. Why funders invest in crowdfunding projects: Role of trust from the dual-process perspective. Inf. Manag. 2019, 56, 70–84. [Google Scholar] [CrossRef]
- McKnight, D.H.; Choudhury, V.; Kacmar, C. The impact of initial consumer trust on intentions to transact with a web site: A trust building model. J. Strat. Inf. Syst. 2002, 11, 297–323. [Google Scholar] [CrossRef]
- Bélanger, F.; Carter, L. Trust and risk in e-government adoption. J. Strat. Inf. Syst. 2008, 17, 165–176. [Google Scholar] [CrossRef] [Green Version]
- Park, S.; Tussyadiah, I.P. How Guests Develop Trust in Hosts: An Investigation of Trust Formation in P2P Accommodation. J. Travel Res. 2020, 59, 1402–1412. [Google Scholar] [CrossRef]
- Xie, Y.; Peng, S. How to repair customer trust after negative publicity: The roles of competence, integrity, benevolence, and forgiveness. Psychol. Mark. 2009, 26, 572–589. [Google Scholar] [CrossRef]
- Moudud-Ul-Huq, S.; Swarna, R.S.; Sultana, M. Elderly and middle-aged intention to use m-health services: An empirical evidence from a developing country. J. Enabling Technol. 2021, 15, 23–39. [Google Scholar] [CrossRef]
- Mayer, R.C.; Davis, J.H.; Schoorman, F.D. An Integrative Model of Organizational Trust. Acad. Manag. Rev. 1995, 20, 709. [Google Scholar] [CrossRef]
- Qiu, Y.; Liu, Y.; Ren, W.; Qiu, Y.; Ren, J. Internet-Based and Mobile-Based General Practice: Cross-Sectional Survey. J. Med. Internet Res. 2018, 20, e266. [Google Scholar] [CrossRef]
- Du, L.; Xu, J.; Chen, X.; Zhu, X.; Zhang, Y.; Wu, R.; Ji, H.; Zhou, L. Rebuild doctor–patient trust in medical service delivery in China. Sci. Rep. 2020, 10, 21956. [Google Scholar] [CrossRef]
- Qi, M.; Cui, J.; Li, X.; Han, Y. Perceived Factors Influencing the Public Intention to Use E-Consultation: Analysis of Web-Based Survey Data. J. Med. Internet Res. 2021, 23, e21834. [Google Scholar] [CrossRef]
- Tandon, U.; Kiran, R.; Sah, A.N. The influence of website functionality, drivers and perceived risk on customer satisfaction in online shopping: An emerging economy case. Inf. Syst. e-Bus. Manag. 2017, 16, 57–91. [Google Scholar] [CrossRef]
- Yang, Q.; Pang, C.; Liu, L.; Yen, D.C.; Tarn, J.M. Exploring consumer perceived risk and trust for online payments: An empirical study in China’s younger generation. Comput. Hum. Behav. 2015, 50, 9–24. [Google Scholar] [CrossRef]
- Featherman, M.S.; Pavlou, P.A. Predicting e-services adoption: A perceived risk facets perspective. Int. J. Hum. Comput. Stud. 2003, 59, 451–474. [Google Scholar] [CrossRef] [Green Version]
- Stone, R.N.; Grønhaug, K. Perceived Risk: Further Considerations for the Marketing Discipline. Eur. J. Mark. 1993, 27, 39–50. [Google Scholar] [CrossRef]
- Yi, M.Y.; Yoon, J.J.; Davis, J.M.; Lee, T. Untangling the antecedents of initial trust in Web-based health information: The roles of argument quality, source expertise, and user perceptions of information quality and risk. Decis. Support Syst. 2013, 55, 284–295. [Google Scholar] [CrossRef]
- Tang, Y.; Yang, Y.-T.; Shao, Y.-F. Acceptance of Online Medical Websites: An Empirical Study in China. Int. J. Environ. Res. Public Health 2019, 16, 943. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Filieri, R.; Alguezaui, S.; McLeay, F. Why do travelers trust TripAdvisor? Antecedents of trust towards consumer-generated media and its influence on recommendation adoption and word of mouth. Tour. Manag. 2015, 51, 174–185. [Google Scholar] [CrossRef] [Green Version]
- Liang, L.J.; Choi, H.C.; Joppe, M. Exploring the relationship between satisfaction, trust and switching intention, repurchase intention in the context of Airbnb. Int. J. Hosp. Manag. 2018, 69, 41–48. [Google Scholar] [CrossRef]
- Lien, C.H.; Cao, Y. Examining WeChat users’ motivations, trust, attitudes, and positive word-of-mouth: Evidence from China. Comput. Hum. Behav. 2014, 41, 104–111. [Google Scholar] [CrossRef]
- Deng, Z.; Lu, Y.; Wei, K.K.; Zhang, J. Understanding customer satisfaction and loyalty: An empirical study of mobile instant messages in China. Int. J. Inf. Manag. 2010, 30, 289–300. [Google Scholar] [CrossRef]
- Ha, H.; Janda, S.; Muthaly, S.K. A new understanding of satisfaction model in e-re-purchase situation. Eur. J. Mark. 2010, 44, 997–1016. [Google Scholar] [CrossRef] [Green Version]
- de Matos, C.A.; Rossi, C.A.V. Word-of-mouth communications in marketing: A meta-analytic review of the antecedents and moderators. J. Acad. Mark. Sci. 2008, 36, 578–596. [Google Scholar] [CrossRef]
- Xiong, J.; Zuo, M. Understanding factors influencing the adoption of a mobile platform of medical and senior care in China. Technol. Forecast. Soc. Chang. 2022, 179, 121621. [Google Scholar] [CrossRef]
- Hair, J.F., Jr.; Hult, G.T.M.; Ringle, C.M.; Sarstedt, M. A Primer on Partial Least Squares Structural Equation Modeling (PLS-SEM); Sage Publications: New York, NY, USA, 2021. [Google Scholar]
- iResearch. 2020. Available online: https://report.iresearch.cn/report/202009/3645.shtml (accessed on 1 January 2023).
- Cheng, T.C.; Fu, H.; Xu, D.; Yip, W. Technology platforms are revolutionizing health care service delivery in China. NEJM Catal. Innov. Care Deliv. 2022, 3, 1–11. [Google Scholar] [CrossRef]
- McKnight, D.H.; Choudhury, V.; Kacmar, C. Developing and Validating Trust Measures for e-Commerce: An Integrative Typology. Inf. Syst. Res. 2002, 13, 334–359. [Google Scholar] [CrossRef] [Green Version]
- Chopdar, P.K.; Korfiatis, N.; Sivakumar, V.; Lytras, M.D. Mobile shopping apps adoption and perceived risks: A cross-country perspective utilizing the Unified Theory of Acceptance and Use of Technology. Comput. Hum. Behav. 2018, 86, 109–128. [Google Scholar] [CrossRef] [Green Version]
- Bhattacherjee, A. Understanding Information Systems Continuance: An Expectation-Confirmation Model. MIS Q. 2001, 25, 351–370. [Google Scholar] [CrossRef]
- Venkatesh, V.; Thong, J.Y.L.; Xu, X. Consumer Acceptance and Use of Information Technology: Extending the Unified Theory of Acceptance and Use of Technology. MIS Q. 2012, 36, 157–178. [Google Scholar] [CrossRef] [Green Version]
- Goyette, I.; Ricard, L.; Bergeron, J.; Marticotte, F. e-WOM Scale: Word-of-mouth measurement scale for e-services context. Can. J. Adm. Sci. Rev. Can. Sci. l’Adm. 2010, 27, 5–23. [Google Scholar] [CrossRef]
- van Dolen, W.M.; Dabholkar, P.A.; de Ruyter, K. Satisfaction with Online Commercial Group Chat: The Influence of Perceived Technology Attributes, Chat Group Characteristics, and Advisor Communication Style. J. Retail. 2007, 83, 339–358. [Google Scholar] [CrossRef]
- Wang, Y.; Yu, C. Social interaction-based consumer decision-making model in social commerce: The role of word of mouth and observational learning. Int. J. Inf. Manag. 2017, 37, 179–189. [Google Scholar] [CrossRef]
- Wenjuanxing. Available online: https://www.wjx.cn/sample/service.aspx (accessed on 1 January 2020).
- Khan, M.J.; Chelliah, S.; Ahmed, S. Factors influencing destination image and visit intention among young women travelers: Role of travel motivation, perceived risks, and travel constraints. Asia Pac. J. Tour. Res. 2017, 22, 1139–1155. [Google Scholar] [CrossRef]
- Danielsoper.com. Free Statistical Calculators. 2016. Available online: http://www.danielsoper.com/statcalc/default.asp (accessed on 8 February 2023).
- Cohen, J. Statistical power analysis. Curr. Dir. Psychol. Sci. 1992, 1, 98–101. [Google Scholar] [CrossRef]
- Tian, X.-F.; Wu, R.-Z. Determinants of the Mobile Health Continuance Intention of Elders with Chronic Diseases: An Integrated Framework of ECM-ISC and UTAUT. Int. J. Environ. Res. Public Health 2022, 19, 9980. [Google Scholar] [CrossRef]
- Churchill, G.A., Jr. A Paradigm for Developing Better Measures of Marketing Constructs. J. Mark. Res. 1979, 16, 64–73. [Google Scholar] [CrossRef]
- Rahimnia, F.; Hassanzadeh, J.F. The impact of website content dimension and e-trust on e-marketing effectiveness: The case of Iranian commercial saffron corporations. Inf. Manag. 2013, 50, 240–247. [Google Scholar] [CrossRef]
- Henseler, J.; Ringle, C.M.; Sarstedt, M. A new criterion for assessing discriminant validity in variance-based structural equation modeling. J. Acad. Mark. Sci. 2015, 43, 115–135. [Google Scholar] [CrossRef] [Green Version]
- Krey, N.; Chuah, S.H.-W.; Ramayah, T.; Rauschnabel, P.A. How functional and emotional ads drive smartwatch adoption: The moderating role of consumer innovativeness and extraversion. Internet Res. 2019, 29, 578–602. [Google Scholar] [CrossRef]
- Kock, N.; Lynn, G.S. Stevens Institute of Technology Lateral Collinearity and Misleading Results in Variance-Based SEM: An Illustration and Recommendations. J. Assoc. Inf. Syst. 2012, 13, 546–580. [Google Scholar] [CrossRef] [Green Version]
- Sarstedt, M.; Hair, J.F.; Pick, M.; Liengaard, B.D.; Radomir, L.; Ringle, C.M. Progress in partial least squares structural equation modeling use in marketing research in the last decade. Psychol. Mark. 2022, 39, 1035–1064. [Google Scholar] [CrossRef]
- Lohmöller, J.B. Predictive vs. structural modeling: PLS vs. ML. In Latent Variable Path Modeling with Partial Least Squares; Physica: Heidelberg, Germany, 1989; pp. 199–226. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences; Lawrence Erlbaum: Mahwah, NJ, USA, 1988. [Google Scholar]
- Fan, H.; Lederman, R. Online health communities: How do community members build the trust required to adopt information and form close relationships? Eur. J. Inf. Syst. 2018, 27, 62–89. [Google Scholar] [CrossRef]
- Akter, S.; D’Ambra, J.; Ray, J.P. Trustworthiness in mHealth information services: An assessment of a hierarchical model with mediating and moderating effects using partial least squares (PLS). J. Am. Soc. Inf. Sci. Technol. 2011, 62, 100–116. [Google Scholar] [CrossRef] [Green Version]
- Chen, Y.; Yang, L.; Zhang, M.; Yang, J. Central or peripheral? Cognition elaboration cues’ effect on users’ continuance intention of mobile health applications in the developing markets. Int. J. Med. Inform. 2018, 116, 33–45. [Google Scholar] [CrossRef]
- Serva, M.A.; Benamati, J.; Fuller, M.A. Trustworthiness in B2C e-commerce: An examination of alternative models. ACM SIGMIS Database Database Adv. Inf. Syst. 2005, 36, 89–108. [Google Scholar] [CrossRef]
- Sang, H.; Cheng, J. Effects of Perceived Risk and Patient Anxiety on Intention to Use Community Healthcare Services in a Big Modern City. SAGE Open 2020, 10, 2158244020933604. [Google Scholar] [CrossRef]
- Hajli, N.; Lin, X. Exploring the Security of Information Sharing on Social Networking Sites: The Role of Perceived Control of Information. J. Bus. Ethic 2014, 133, 111–123. [Google Scholar] [CrossRef]
- Karwatzki, S.; Dytynko, O.; Trenz, M.; Veit, D. Beyond the Personalization–Privacy Paradox: Privacy Valuation, Transparency Features, and Service Personalization. J. Manag. Inf. Syst. 2017, 34, 369–400. [Google Scholar] [CrossRef]
- Alalwan, A.A. Mobile food ordering apps: An empirical study of the factors affecting customer e-satisfaction and continued intention to reuse. Int. J. Inf. Manag. 2020, 50, 28–44. [Google Scholar] [CrossRef]
- Tam, C.; Oliveira, T. Understanding the impact of m-banking on individual performance: DeLone & McLean and TTF perspective. Comput. Hum. Behav. 2016, 61, 233–244. [Google Scholar] [CrossRef]
- Meng, F.; Guo, X.; Peng, Z.; Zhang, X.; Vogel, D. The routine use of mobile health services in the presence of health consciousness. Electron. Commer. Res. Appl. 2019, 35, 100847. [Google Scholar] [CrossRef]
| Platforms | Haodf.com | WeDoctor | Chunyu Doctor | Ping An Good Doctor | AliHealth | JD Health |
|---|---|---|---|---|---|---|
| Headquarters | Beijing | Hangzhou | Beijing | Shanghai | Beijing | Beijing |
| Year founded | 2006 | 2010 | 2011 | 2014 | 2004 | 2017 |
| Ownership | Private | Private | Private | Publicly listed | Publicly listed | Publicly listed |
| Main functionalities | Online consultation, Sales of medicines | Online consultation, Sales of medicines and insurance | Online consultation, Sales of medicines | Online consultation, Sales of medicines Health management programs | Online consultation, Sales of medicines, health products and insurance Health management programs | Online consultation, Sales of medicines, health products and insurance Health management programs |
| Variables | Level | Frequency | Percent |
|---|---|---|---|
| Gender | Female | 379 | 55.8 |
| Male | 300 | 44.2 | |
| Age | 18–25 | 120 | 17.7 |
| 26–30 | 175 | 25.8 | |
| 31–40 | 305 | 44.9 | |
| 41–50 | 59 | 8.7 | |
| >50 | 20 | 2.9 | |
| Marital status | Single | 162 | 23.9 |
| Married | 517 | 76.1 | |
| Salary | Less than RMB 3000 | 37 | 5.4 |
| RMB 3000~RMB 4999 | 60 | 8.8 | |
| RMB 5000~RMB 7999 | 196 | 28.9 | |
| RMB 8000~RMB 9999 | 186 | 27.4 | |
| More than RMB 10,000 | 200 | 29.5 | |
| Education | Less than high school degree | 11 | 1.6 |
| College graduate or student | 54 | 8.0 | |
| Undergraduate or student | 533 | 78.5 | |
| Masters postgraduate degree or above | 81 | 11.9 | |
| Apps | Ping An Good Doctor | 308 | 45.4 |
| Good Doctor | 143 | 21.1 | |
| Wei Mai | 3 | 0.4 | |
| Wei Yi | 32 | 4.7 | |
| Spring Rain Doctor | 55 | 8.1 | |
| Ding Xiang Doctor | 137 | 20.2 | |
| Others | 1 | 0.1 | |
| Frequency | ≤1 time | 97 | 14.3 |
| 2 times–3 times | 392 | 57.7 | |
| 4 times–5 times | 135 | 19.9 | |
| ≥6 times | 55 | 8.1 |
| Constructs | Items | Factor Loadings | Cronbach’s Alpha | CR | AVE |
|---|---|---|---|---|---|
| Propensity to trust | DispositionToTrust1 | 0.869 *** | 0.883 | 0.919 | 0.74 |
| DispositionToTrust2 | 0.89 *** | ||||
| DispositionToTrust3 | 0.874 *** | ||||
| DispositionToTrust4 | 0.806 *** | ||||
| Doctor’s ability | Ability1 | 0.737 *** | 0.693 | 0.813 | 0.521 |
| Ability2 | 0.666 *** | ||||
| Ability3 | 0.718 *** | ||||
| Ability4 | 0.762 *** | ||||
| Doctor’s benevolence | Benevolence1 | 0.733 *** | 0.758 | 0.846 | 0.579 |
| Benevolence2 | 0.807 *** | ||||
| Benevolence3 | 0.766 *** | ||||
| Benevolence4 | 0.735 *** | ||||
| Privacy risk | PrivacyRisk1 | 0.924 *** | 0.916 | 0.947 | 0.856 |
| PrivacyRisk2 | 0.917 *** | ||||
| PrivacyRisk3 | 0.934 *** | ||||
| Physical risk | PhysicalRisk1 | 0.77 *** | 0.81 | 0.875 | 0.638 |
| PhysicalRisk2 | 0.856 *** | ||||
| PhysicalRisk3 | 0.794 *** | ||||
| PhysicalRisk4 | 0.77 *** | ||||
| Cognitive trust | CognitionbasedTrust1 | 0.707 *** | 0.691 | 0.812 | 0.519 |
| CognitionbasedTrust2 | 0.697*** | ||||
| CognitionbasedTrust3 | 0.713 *** | ||||
| CognitionbasedTrust4 | 0.763 *** | ||||
| Emotional trust | AffectbasedTrust1 | 0.691 *** | 0.734 | 0.834 | 0.556 |
| AffectbasedTrust2 | 0.761 *** | ||||
| AffectbasedTrust3 | 0.74 *** | ||||
| AffectbasedTrust4 | 0.789 *** | ||||
| Continuance intention | ContinuanceIntention1 | 0.732 *** | 0.704 | 0.818 | 0.529 |
| ContinuanceIntention2 | 0.707 *** | ||||
| ContinuanceIntention3 | 0.729 *** | ||||
| ContinuanceIntention4 | 0.741 *** | ||||
| Positive WOM | PositiveWOM1 | 0.796 *** | 0.79 | 0.864 | 0.615 |
| PositiveWOM2 | 0.82 *** | ||||
| PositiveWOM3 | 0.707 *** | ||||
| PositiveWOM4 | 0.81 *** |
| Propensity to Trust | Ability | Benevolence | Privacy Risk | Physical Risk | Cognitive Trust | Emotional Trust | Continuance Intention | Positive WOM | |
|---|---|---|---|---|---|---|---|---|---|
| DispositionToTrust1 | 0.869 | 0.124 | 0.192 | −0.119 | −0.112 | 0.216 | 0.216 | 0.112 | 0.192 |
| DispositionToTrust2 | 0.89 | 0.161 | 0.201 | −0.101 | −0.159 | 0.263 | 0.228 | 0.186 | 0.214 |
| DispositionToTrust3 | 0.874 | 0.161 | 0.186 | −0.149 | −0.164 | 0.293 | 0.251 | 0.167 | 0.201 |
| DispositionToTrust4 | 0.806 | 0.178 | 0.134 | −0.071 | −0.148 | 0.218 | 0.227 | 0.212 | 0.217 |
| Ability1 | 0.127 | 0.737 | 0.458 | −0.172 | −0.262 | 0.455 | 0.357 | 0.397 | 0.353 |
| Ability2 | 0.178 | 0.666 | 0.448 | −0.213 | −0.295 | 0.348 | 0.322 | 0.299 | 0.296 |
| Ability3 | 0.094 | 0.718 | 0.373 | −0.196 | −0.243 | 0.428 | 0.349 | 0.391 | 0.391 |
| Ability4 | 0.134 | 0.762 | 0.47 | −0.225 | −0.256 | 0.456 | 0.365 | 0.351 | 0.381 |
| Benevolence1 | 0.149 | 0.397 | 0.733 | −0.221 | −0.222 | 0.401 | 0.421 | 0.302 | 0.351 |
| Benevolence2 | 0.172 | 0.488 | 0.807 | −0.251 | −0.243 | 0.486 | 0.449 | 0.305 | 0.385 |
| Benevolence3 | 0.156 | 0.455 | 0.766 | −0.226 | −0.269 | 0.491 | 0.457 | 0.295 | 0.406 |
| Benevolence4 | 0.155 | 0.502 | 0.735 | −0.215 | −0.238 | 0.422 | 0.383 | 0.28 | 0.324 |
| PrivacyRisk1 | −0.134 | −0.257 | −0.274 | 0.924 | 0.465 | −0.332 | −0.357 | −0.338 | −0.343 |
| PrivacyRisk2 | −0.117 | −0.266 | −0.293 | 0.917 | 0.457 | −0.338 | −0.4 | −0.313 | −0.358 |
| PrivacyRisk3 | −0.11 | −0.248 | −0.268 | 0.934 | 0.44 | −0.351 | −0.396 | −0.331 | −0.366 |
| PhysicalRisk1 | −0.148 | −0.215 | −0.211 | 0.441 | 0.77 | −0.292 | −0.289 | −0.285 | −0.302 |
| PhysicalRisk2 | −0.157 | −0.362 | −0.317 | 0.431 | 0.856 | −0.387 | −0.339 | −0.395 | −0.408 |
| PhysicalRisk3 | −0.15 | −0.289 | −0.26 | 0.339 | 0.794 | −0.373 | −0.319 | −0.378 | −0.318 |
| PhysicalRisk4 | −0.085 | −0.279 | −0.222 | 0.362 | 0.77 | −0.308 | −0.274 | −0.352 | −0.299 |
| CognitionbasedTrust1 | 0.226 | 0.464 | 0.494 | −0.26 | −0.288 | 0.707 | 0.471 | 0.398 | 0.439 |
| CognitionbasedTrust2 | 0.226 | 0.416 | 0.415 | −0.275 | −0.313 | 0.697 | 0.459 | 0.364 | 0.4 |
| CognitionbasedTrust3 | 0.206 | 0.404 | 0.392 | −0.253 | −0.31 | 0.713 | 0.449 | 0.368 | 0.437 |
| CognitionbasedTrust4 | 0.184 | 0.411 | 0.41 | −0.274 | −0.328 | 0.763 | 0.431 | 0.448 | 0.523 |
| AffectbasedTrust1 | 0.146 | 0.337 | 0.401 | −0.271 | −0.293 | 0.47 | 0.691 | 0.319 | 0.416 |
| AffectbasedTrust2 | 0.23 | 0.294 | 0.381 | −0.388 | −0.295 | 0.443 | 0.761 | 0.369 | 0.463 |
| AffectbasedTrust3 | 0.205 | 0.44 | 0.5 | −0.278 | −0.254 | 0.467 | 0.74 | 0.392 | 0.486 |
| AffectbasedTrust4 | 0.217 | 0.363 | 0.394 | −0.306 | −0.307 | 0.492 | 0.789 | 0.388 | 0.503 |
| ContinuanceIntention1 | 0.149 | 0.419 | 0.305 | −0.23 | −0.323 | 0.436 | 0.377 | 0.732 | 0.435 |
| ContinuanceIntention2 | 0.115 | 0.341 | 0.232 | −0.189 | −0.257 | 0.343 | 0.294 | 0.707 | 0.359 |
| ContinuanceIntention3 | 0.192 | 0.346 | 0.315 | −0.283 | −0.31 | 0.429 | 0.4 | 0.729 | 0.405 |
| ContinuanceIntention4 | 0.111 | 0.342 | 0.267 | −0.322 | −0.399 | 0.379 | 0.355 | 0.741 | 0.376 |
| PositiveWOM1 | 0.18 | 0.365 | 0.383 | −0.289 | −0.332 | 0.498 | 0.523 | 0.453 | 0.796 |
| PositiveWOM2 | 0.204 | 0.403 | 0.411 | −0.317 | −0.329 | 0.498 | 0.524 | 0.398 | 0.82 |
| PositiveWOM3 | 0.15 | 0.397 | 0.347 | −0.287 | −0.303 | 0.475 | 0.415 | 0.423 | 0.707 |
| PositiveWOM4 | 0.214 | 0.387 | 0.375 | −0.314 | −0.349 | 0.495 | 0.502 | 0.433 | 0.81 |
| Doctor’s Ability | Doctor’s Benevolence | Cognitive Trust | Continuance Intention | Emotional Trust | Physical Risk | Positive WOM | Privacy Risk | Propensity to Trust | |
|---|---|---|---|---|---|---|---|---|---|
| Doctor’s ability | 0.722 | ||||||||
| Doctor’s benevolence | 0.605 | 0.761 | |||||||
| Cognitive trust | 0.588 | 0.594 | 0.721 | ||||||
| Continuance intention | 0.5 | 0.388 | 0.55 | 0.727 | |||||
| Emotional trust | 0.483 | 0.563 | 0.627 | 0.494 | 0.746 | ||||
| Physical risk | −0.363 | −0.32 | −0.43 | −0.444 | −0.384 | 0.798 | |||
| Positive WOM | 0.494 | 0.484 | 0.627 | 0.544 | 0.628 | −0.419 | 0.784 | ||
| Privacy risk | −0.278 | −0.301 | −0.368 | −0.354 | −0.416 | 0.49 | −0.385 | 0.925 | |
| Propensity to trust | 0.182 | 0.208 | 0.291 | 0.198 | 0.269 | −0.171 | 0.239 | −0.13 | 0.86 |
| Doctor’s Ability | Doctor’s Benevolence | Cognitive Trust | Continuance Intention | Emotional Trust | Physical Risk | Positive WOM | Privacy Risk | Propensity to Trust | |
|---|---|---|---|---|---|---|---|---|---|
| Doctor’s ability | |||||||||
| Doctor’s benevolence | 0.837 | ||||||||
| Cognitive trust | 0.845 | 0.817 | |||||||
| Continuance intention | 0.709 | 0.527 | 0.778 | ||||||
| Emotional trust | 0.674 | 0.751 | 0.883 | 0.679 | |||||
| Physical risk | 0.482 | 0.403 | 0.57 | 0.581 | 0.497 | ||||
| Positive WOM | 0.667 | 0.623 | 0.846 | 0.726 | 0.821 | 0.519 | |||
| Privacy risk | 0.351 | 0.36 | 0.463 | 0.438 | 0.507 | 0.572 | 0.453 | ||
| Propensity to trust | 0.235 | 0.253 | 0.37 | 0.246 | 0.331 | 0.198 | 0.286 | 0.143 |
| β | STDEV | T Values | p Values | Status | |
|---|---|---|---|---|---|
| H1a Propensity to trust -> Cognitive trust | 0.134 | 0.029 | 4.637 | 0.000 | Accepted |
| H1b Propensity to trust -> Emotional trust | 0.125 | 0.034 | 3.693 | 0.000 | Accepted |
| H2a Doctor’s ability -> Cognitive trust | 0.293 | 0.04 | 7.258 | 0.000 | Accepted |
| H2b Doctor’s ability -> Emotional trust | 0.158 | 0.041 | 3.838 | 0.000 | Accepted |
| H3a Doctor’s benevolence -> Cognitive trust | 0.31 | 0.039 | 7.904 | 0.000 | Accepted |
| H3b Doctor’s benevolence -> Emotional trust | 0.351 | 0.042 | 8.371 | 0.000 | Accepted |
| H4a Privacy risk -> Cognitive trust | −0.102 | 0.032 | 3.212 | 0.001 | Accepted |
| H4b Privacy risk -> Emotional trust | −0.206 | 0.035 | 5.869 | 0.000 | Accepted |
| H5a Physical risk -> Cognitive trust | −0.151 | 0.034 | 4.431 | 0.000 | Accepted |
| H5b Physical risk -> Emotional trust | −0.092 | 0.039 | 2.366 | 0.018 | Accepted |
| H6a Cognitive trust -> Continuance intention | 0.395 | 0.042 | 9.471 | 0.000 | Accepted |
| H6b Cognitive trust -> Positive WOM | 0.299 | 0.042 | 7.111 | 0.000 | Accepted |
| H7a Emotional trust -> Continuance intention | 0.246 | 0.041 | 5.989 | 0.000 | Accepted |
| H7b Emotional trust -> Positive WOM | 0.334 | 0.043 | 7.794 | 0.000 | Accepted |
| H8 Continuance intention -> Positive WOM | 0.214 | 0.044 | 4.919 | 0.000 | Accepted |
| R Square | R Square Adjusted | |
|---|---|---|
| Cognitive trust | 0.498 | 0.494 |
| Emotional trust | 0.428 | 0.424 |
| Continuance intention | 0.339 | 0.337 |
| Positive WOM | 0.514 | 0.512 |
| Cognitive Trust | Emotional Trust | Continuance Intention | Positive WOM | |
|---|---|---|---|---|
| Propensity to trust | 0.034 | 0.026 | ||
| Ability | 0.102 | 0.026 | ||
| Benevolence | 0.116 | 0.13 | ||
| Cognitive trust | 0.143 | 0.098 | ||
| Emotional trust | 0.056 | 0.132 | ||
| Privacy risk | 0.015 | 0.054 | ||
| Physical risk | 0.032 | 0.01 | ||
| Continuance intention | 0.062 | |||
| Positive WOM |
| SSO | SSE | Q2 (=1-SSE/SSO) | |
|---|---|---|---|
| Propensity to trust | 2716 | 2716 | |
| Ability | 2716 | 2716 | |
| Benevolence | 2716 | 2716 | |
| Privacy risk | 2037 | 2037 | |
| Physical risk | 2716 | 2716 | |
| Cognitive trust | 2716 | 2027.111 | 0.254 |
| Emotional trust | 2716 | 2084.539 | 0.232 |
| Continuance intention | 2716 | 2240.208 | 0.175 |
| Positive WOM | 2716 | 1868.289 | 0.312 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jiang, Y.; Lau, A.K.W. Understanding Post-Adoption Behavioral Intentions of Mobile Health Service Users: An Empirical Study during COVID-19. Int. J. Environ. Res. Public Health 2023, 20, 3907. https://doi.org/10.3390/ijerph20053907
Jiang Y, Lau AKW. Understanding Post-Adoption Behavioral Intentions of Mobile Health Service Users: An Empirical Study during COVID-19. International Journal of Environmental Research and Public Health. 2023; 20(5):3907. https://doi.org/10.3390/ijerph20053907
Chicago/Turabian StyleJiang, Yanmei, and Antonio K. W. Lau. 2023. "Understanding Post-Adoption Behavioral Intentions of Mobile Health Service Users: An Empirical Study during COVID-19" International Journal of Environmental Research and Public Health 20, no. 5: 3907. https://doi.org/10.3390/ijerph20053907
APA StyleJiang, Y., & Lau, A. K. W. (2023). Understanding Post-Adoption Behavioral Intentions of Mobile Health Service Users: An Empirical Study during COVID-19. International Journal of Environmental Research and Public Health, 20(5), 3907. https://doi.org/10.3390/ijerph20053907






