Twelve Tips for Inclusive Practice in Healthcare Settings
Abstract
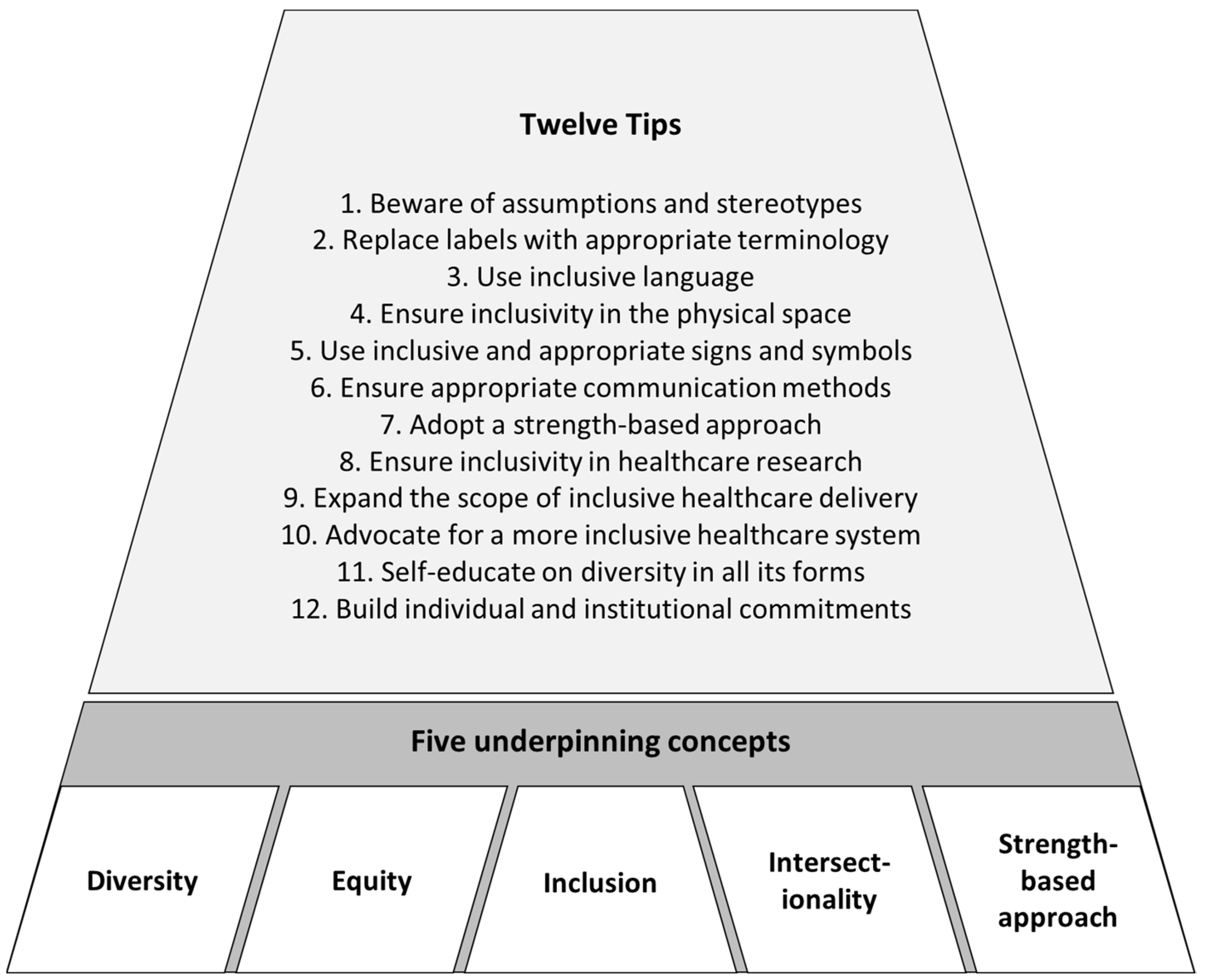
:1. Introduction
2. The Twelve Tips and Discussion
2.1. Tip 1: Beware of Assumptions and Stereotypes
2.2. Tip 2: Replace Labels with Appropriate Terminology
2.3. Tip 3: Use Inclusive Language
2.4. Tip 4: Ensure Inclusivity in Physical Spaces
2.5. Tip 5: Use Inclusive and Appropriate Signage and Symbols
2.6. Tip 6: Ensure Appropriate Communication Methods
2.7. Tip 7: Adopt a Strength-Based Approach
2.8. Tip 8: Ensure Inclusivity in Healthcare Service Research
2.9. Tip 9: Expand the Scope of Inclusive Healthcare Delivery
2.10. Tip 10: Advocate for a More Inclusive Healthcare System
2.11. Tip 11: Self-Educate on Diversity in All Its Forms
2.12. Tip 12: Build Individual and Institutional Commitments
3. Conclusions
4. Future Direction
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. Constitution of the World Health Organization 1946. Bull. World Health Organ. 2002, 80, 983. [Google Scholar]
- Dowling, A.; Enticott, J.; Kunin, M.; Russell, G. The association of migration experiences on the self-rated health status among adult humanitarian refugees to Australia: An analysis of a longitudinal cohort study. Int. J. Equity Health 2019, 18, 130. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tan, K.K.; Ellis, S.J.; Schmidt, J.M.; Byrne, J.L.; Veale, J.F. Mental health inequities among transgender people in Aotearoa New Zealand: Findings from the Counting Ourselves Survey. Int. J. Environ. Res. Public Health 2020, 17, 2862. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schultz, R. Closing the gap and the sustainable development goals: Listening to Aboriginal and Torres Strait Islander people. Aust. N. Z. J. Public Health 2020, 44, 11–13. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Commission on the Social Determinants of Health. Closing the Gap in a Generation: Health Equity Through Action on the Social Determinants of Health. Final Report of the Commission on Social Determinants of Health; World Health Organization: Geneva, Switzerland, 2008.
- Minnican, C.; O’Toole, G. Exploring the incidence of culturally responsive communication in Australian healthcare: The first rapid review on this concept. BMC Health Serv. Res. 2020, 20, 20. [Google Scholar] [CrossRef] [PubMed]
- Baker, K.; Adams, J.; Steel, A. Experiences, perceptions and expectations of health services amongst marginalized populations in urban Australia: A meta-ethnographic review of the literature. Health Expect. 2021, 25, 2166–2187. [Google Scholar] [CrossRef] [PubMed]
- Richardson, F. An introduction to inclusive practice. In Inclusive Practice for Health Professionals; Birks, M., Davis, J., Richardson, F., Eds.; Oxford University Press: Oxford, UK, 2015; pp. 2–22. [Google Scholar]
- McGlynn, N.; Browne, K.; Sherriff, N.; Zeeman, L.; Mirandola, M.; Gios, L.; Davis, R.; Donisi, V.; Farinella, F.; Rosińska, M. Healthcare professionals’ assumptions as barriers to LGBTI healthcare. Cult. Health Sex. 2020, 22, 954–970. [Google Scholar] [CrossRef]
- Mengesha, Z.B.; Perz, J.; Dune, T.; Ussher, J. Refugee and migrant women’s engagement with sexual and reproductive health care in Australia: A socio-ecological analysis of health care professional perspectives. PLoS ONE 2017, 12, e0181421. [Google Scholar] [CrossRef] [Green Version]
- Dickinson, J.K.; Guzman, S.J.; Maryniuk, M.D.; O’Brian, C.A.; Kadohiro, J.K.; Jackson, R.A.; D’Hondt, N.; Montgomery, B.; Close, K.L.; Funnell, M.M. The use of language in diabetes care and education. Diabetes Care 2017, 40, 1790–1799. [Google Scholar] [CrossRef] [Green Version]
- Tylka, T.L.; Annunziato, R.A.; Burgard, D.; Daníelsdóttir, S.; Shuman, E.; Davis, C.; Calogero, R.M. The weight-inclusive versus weight-normative approach to health: Evaluating the evidence for prioritizing well-being over weight loss. J. Obes. 2014, 2014, 983495. [Google Scholar] [CrossRef]
- Diabetes Australia. Position Statement: A New Language for Diabetes. Available online: https://www.diabetesaustralia.com.au/wp-content/uploads/Language-position-statement-2016.pdf (accessed on 18 April 2022).
- Brunton, S. I have never liked the term “Compliance”. Clin. Diabetes 2017, 35, 76–77. [Google Scholar] [CrossRef] [Green Version]
- Kyle, T.K.; Puhl, R.M. Putting people first in obesity. Obesity 2014, 22, 1211. [Google Scholar] [CrossRef]
- Public Health Association of Australia. Aboriginal and Torres Strait Islander Guide to Terminology. Available online: https://www.phaa.net.au/documents/item/2292 (accessed on 18 April 2022).
- Grove, N.J.; Zwi, A.B. Our health and theirs: Forced migration, othering, and public health. Soc. Sci. Med. 2006, 62, 1931–1942. [Google Scholar] [CrossRef] [PubMed]
- Oliver, M. The social model of disability: Thirty years on. Disabil. Soc. 2013, 28, 1024–1026. [Google Scholar] [CrossRef]
- MacDonald, T.; Noel-Weiss, J.; West, D.; Walks, M.; Biener, M.; Kibbe, A.; Myler, E. Transmasculine individuals’ experiences with lactation, chestfeeding, and gender identity: A qualitative study. BMC Pregnancy Childbirth 2016, 16, 106. [Google Scholar] [CrossRef] [Green Version]
- Dwyer, P. Stigma, incommensurability, or both? Pathology-first, person-first, and identity-first language and the challenges of discourse in divided autism communities. J. Dev. Behav. Pediatr. 2022, 43, 111–113. [Google Scholar] [CrossRef] [PubMed]
- Dunn, D.S.; Andrews, E.E. Person-first and identity-first language: Developing psychologists’ cultural competence using disability language. Am. Psychol. 2015, 70, 255. [Google Scholar] [CrossRef] [PubMed]
- Dunning, T.; Speight, J.; Bennett, C. Language, the “Diabetes Restricted Code/Dialect,” and what it means for people with diabetes and clinicians. Diabetes Educ. 2017, 43, 18–26. [Google Scholar] [CrossRef]
- Haelle, T. Identity-First vs. Person-First Language Is an Important Distinction. Available online: https://healthjournalism.org/blog/2019/07/identity-first-vs-person-first-language-is-an-important-distinction/ (accessed on 20 April 2022).
- Gernsbacher, M.A. The use of person-first language in scholarly writing may accentuate stigma. J. Child Psychol. Psychiatry 2017, 58, 859–861. [Google Scholar] [CrossRef] [Green Version]
- Australian Government. Style Manual: People with Disability. Available online: https://www.stylemanual.gov.au/accessible-and-inclusive-content/inclusive-language/people-disability (accessed on 18 April 2022).
- Crenshaw, K.W. Demarginalizing the Intersection of Race and Sex: A Black Feminist Critique of Antidiscrimination Doctrine, Feminist Theory and Antiracist Politics. Univ. Chic. Leg. Forum 1989, 1989, 139–167. [Google Scholar]
- Barnes, S.; Gott, M.; Payne, S.; Seamark, D.; Parker, C.; Gariballa, S.; Small, N. Communication in heart failure: Perspectives from older people and primary care professionals. Health Soc. Care Community 2006, 14, 482–490. [Google Scholar] [CrossRef]
- Myerson, J.; West, J. Make It Better: How universal design principles can have an impact on healthcare services to improve the patient experience. In Proceedings of the Universal Design in Education Conference, Dublin, Ireland, 12–13 November 2015. [Google Scholar]
- World Health Organization. Disability-Inclusive Health Services Toolkit: A Resource for Health Facilities in the Western Pacific Region. Available online: https://apps.who.int/iris/bitstream/handle/10665/336857/9789290618928-eng.pdf?sequence=1&isAllowed=y (accessed on 20 April 2022).
- Waller, S.; Masterson, A. Designing dementia-friendly hospital environments. Future Healthc. J. 2015, 2, 63–68. [Google Scholar] [CrossRef]
- Dimer, L.; Dowling, T.; Jones, J.; Cheetham, C.; Thomas, T.; Smith, J.; McManus, A.; Maiorana, A.J. Build it and they will come: Outcomes from a successful cardiac rehabilitation program at an Aboriginal Medical Service. Aust. Health Rev. 2012, 37, 79–82. [Google Scholar] [CrossRef] [Green Version]
- Government of South Australia. Accessible Wayfinding and Signage. Available online: https://inclusive.sa.gov.au/__data/assets/pdf_file/0003/124635/Accessible-wayfinding-and-signage-toolkit.pdf (accessed on 18 April 2022).
- Tasmanian Government Department of Health. Signage that Makes Sense. Available online: https://www.health.tas.gov.au/professionals/health-literacy/health-literacy-workplace-toolkit/improving-health-literacy-environment/signage-makes-sense (accessed on 18 April 2022).
- Iezzoni, L.I. Make no assumptions: Communication between persons with disabilities and clinicians. Assist. Technol. 2006, 18, 212–219. [Google Scholar] [CrossRef]
- Cummins, C.; Pellicano, E.; Crane, L. Autistic adults’ views of their communication skills and needs. Int. J. Lang. Commun. Disord. 2020, 55, 678–689. [Google Scholar] [CrossRef] [PubMed]
- Javanparast, S.; Naqvi, S.K.A.; Mwanri, L. Health service access and utilisation amongst culturally and linguistically diverse populations in regional South Australia: A qualitative study. Rural Remote Health 2020, 20, 5694. [Google Scholar] [CrossRef] [PubMed]
- Australian Government Department of Health. Fact Sheet: Mental Health Services for People of Culturally and Linguistically Diverse (CALD) Backgrounds. Available online: https://www.health.gov.au/sites/default/files/documents/2020/11/mental-health-services-for-people-of-culturally-and-linguistically-diverse-cald-backgrounds.pdf (accessed on 20 April 2022).
- Mengesha, Z.B.; Perz, J.; Dune, T.; Ussher, J. Talking about sexual and reproductive health through interpreters: The experiences of health care professionals consulting refugee and migrant women. Sex. Reprod. Healthc. 2018, 16, 199–205. [Google Scholar] [CrossRef]
- Fogarty, W.; Lovell, M.; Langenberg, J.; Heron, M.-J. Deficit Discourse and Strengths-Based Approaches: Changing the Narrative of Aboriginal and Torres Strait Islander Health and Wellbeing; The Lowitja Institute: Melbourne, VIC, Australia, 2018. [Google Scholar]
- Wolf, N. Forget everything you thought you knew: How your assumptions are impacting the health outcomes of your patients. Aust. Med. Stud. J. 2016, 7, 60–62. [Google Scholar]
- Steering Committee for the Review of Government Service Provision. Overcoming Indigenous Disadvantage: Key Indicators 2020; Productivity Commission: Canberra, ACT, Australia, 2020. [Google Scholar]
- Autistica. Action Briefing: Strengths Based Approaches. Available online: https://www.autistica.org.uk/downloads/files/FINAL-Strengths-Based-Approaches-ActionBriefing.pdf (accessed on 20 April 2022).
- Drahm-Butler, T. Decolonising identity stories: Narrative practice through Aboriginal eyes. In Aboriginal Narrative Practice: Honouring Storylines of Pride, Strength and Creativity; Wingard, B., Johnson, C., Drahm-Butler, T., Eds.; Dulwich Centre: Adelaide, SA, Australia, 2015. [Google Scholar]
- Muthusamy, A.; Long, D.; Underhill, C.R. Improving recruitment to clinical trials for regional and rural cancer patients through a regionally based clinical trials network. Med. J. Aust. 2021, 214, 453–454. [Google Scholar] [CrossRef]
- Ekezie, W.; Czyznikowska, B.M.; Rohit, S.; Harrison, J.; Miah, N.; Campbell-Morris, P.; Khunti, K. The views of ethnic minority and vulnerable communities towards participation in COVID-19 vaccine trials. J. Public Health 2021, 43, e258–e260. [Google Scholar] [CrossRef]
- Schmotzer, G.L. Barriers and facilitators to participation of minorities in clinical trials. Ethn. Dis. 2012, 22, 226–230. [Google Scholar]
- Baum, F.; MacDougall, C.; Smith, D. Participatory action research. J. Epidemiol. Community Health 2006, 60, 854–857. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Etti, M.; Fofie, H.; Razai, M.; Crawshaw, A.F.; Hargreaves, S.; Goldsmith, L.P. Ethnic minority and migrant underrepresentation in COVID-19 research: Causes and solutions. eClinicalMedicine 2021, 36, 100903. [Google Scholar] [CrossRef] [PubMed]
- Luchenski, S.; Maguire, N.; Aldridge, R.; Hayward, A.; Story, A.; Perri, P.; Withers, J.; Clint, S.; Fitzpatrick, S.; Hewett, N. What works in inclusion health: Overview of effective interventions for marginalised and excluded populations. Lancet 2018, 391, 266–280. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Disability and Health. Available online: https://www.who.int/news-room/fact-sheets/detail/disability-and-health (accessed on 20 April 2022).
- Nkhoma, G.; Lim, C.X.; Kennedy, G.A.; Stupans, I. Reducing health inequities for asylum seekers with chronic non-communicable diseases: Australian context. Aust. J. Prim. Health 2021, 27, 130–135. [Google Scholar] [CrossRef]
- Tippens, K.M.; Chao, M.T.; Connelly, E.; Locke, A. Patient perspectives on care received at community acupuncture clinics: A qualitative thematic analysis. BMC Complement. Altern. Med. 2013, 13, 293. [Google Scholar] [CrossRef] [Green Version]
- Victorian Government Department of Health. A Whole-of-Journey Approach: A Resource Kit for Health Services that Care for Rural Consumers Who Travel for Health Care. 2010. Available online: https://content.health.vic.gov.au/sites/default/files/migrated/files/collections/policies-and-guidelines/r/resource-kit-ruralconsumers---pdf.pdf (accessed on 20 April 2022).
- Javanparast, S.; Windle, A.; Freeman, T.; Baum, F. Community health worker programs to improve healthcare access and equity: Are they only relevant to low-and middle-income countries? Int. J. Health Policy Manag. 2018, 7, 943. [Google Scholar] [CrossRef] [Green Version]
- De Beer, J.; Engels, J.; Heerkens, Y.; van der Klink, J. Factors influencing work participation of adults with developmental dyslexia: A systematic review. BMC Public Health 2014, 14, 77. [Google Scholar] [CrossRef] [Green Version]
- Salsberg, E.; Richwine, C.; Westergaard, S.; Martinez, M.P.; Oyeyemi, T.; Vichare, A.; Chen, C.P. Estimation and comparison of current and future racial/ethnic representation in the US health care workforce. JAMA Netw. Open 2021, 4, e213789. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Marjadi, B.; Flavel, J.; Baker, K.; Glenister, K.; Morns, M.; Triantafyllou, M.; Strauss, P.; Wolff, B.; Procter, A.M.; Mengesha, Z.; et al. Twelve Tips for Inclusive Practice in Healthcare Settings. Int. J. Environ. Res. Public Health 2023, 20, 4657. https://doi.org/10.3390/ijerph20054657
Marjadi B, Flavel J, Baker K, Glenister K, Morns M, Triantafyllou M, Strauss P, Wolff B, Procter AM, Mengesha Z, et al. Twelve Tips for Inclusive Practice in Healthcare Settings. International Journal of Environmental Research and Public Health. 2023; 20(5):4657. https://doi.org/10.3390/ijerph20054657
Chicago/Turabian StyleMarjadi, Brahmaputra, Joanne Flavel, Kirsten Baker, Kristen Glenister, Melissa Morns, Mel Triantafyllou, Penelope Strauss, Brittany Wolff, Alexandra Marie Procter, Zelalem Mengesha, and et al. 2023. "Twelve Tips for Inclusive Practice in Healthcare Settings" International Journal of Environmental Research and Public Health 20, no. 5: 4657. https://doi.org/10.3390/ijerph20054657
APA StyleMarjadi, B., Flavel, J., Baker, K., Glenister, K., Morns, M., Triantafyllou, M., Strauss, P., Wolff, B., Procter, A. M., Mengesha, Z., Walsberger, S., Qiao, X., & Gardiner, P. A. (2023). Twelve Tips for Inclusive Practice in Healthcare Settings. International Journal of Environmental Research and Public Health, 20(5), 4657. https://doi.org/10.3390/ijerph20054657







