Environmental Quality, Extreme Heat, and Healthcare Expenditures
Abstract
:1. Introduction
1.1. The Environmental Quality Index
1.2. The Current Study
2. Methods
2.1. Study Design
2.2. Data
2.3. Covariates
2.4. Statistical Analysis
3. Results
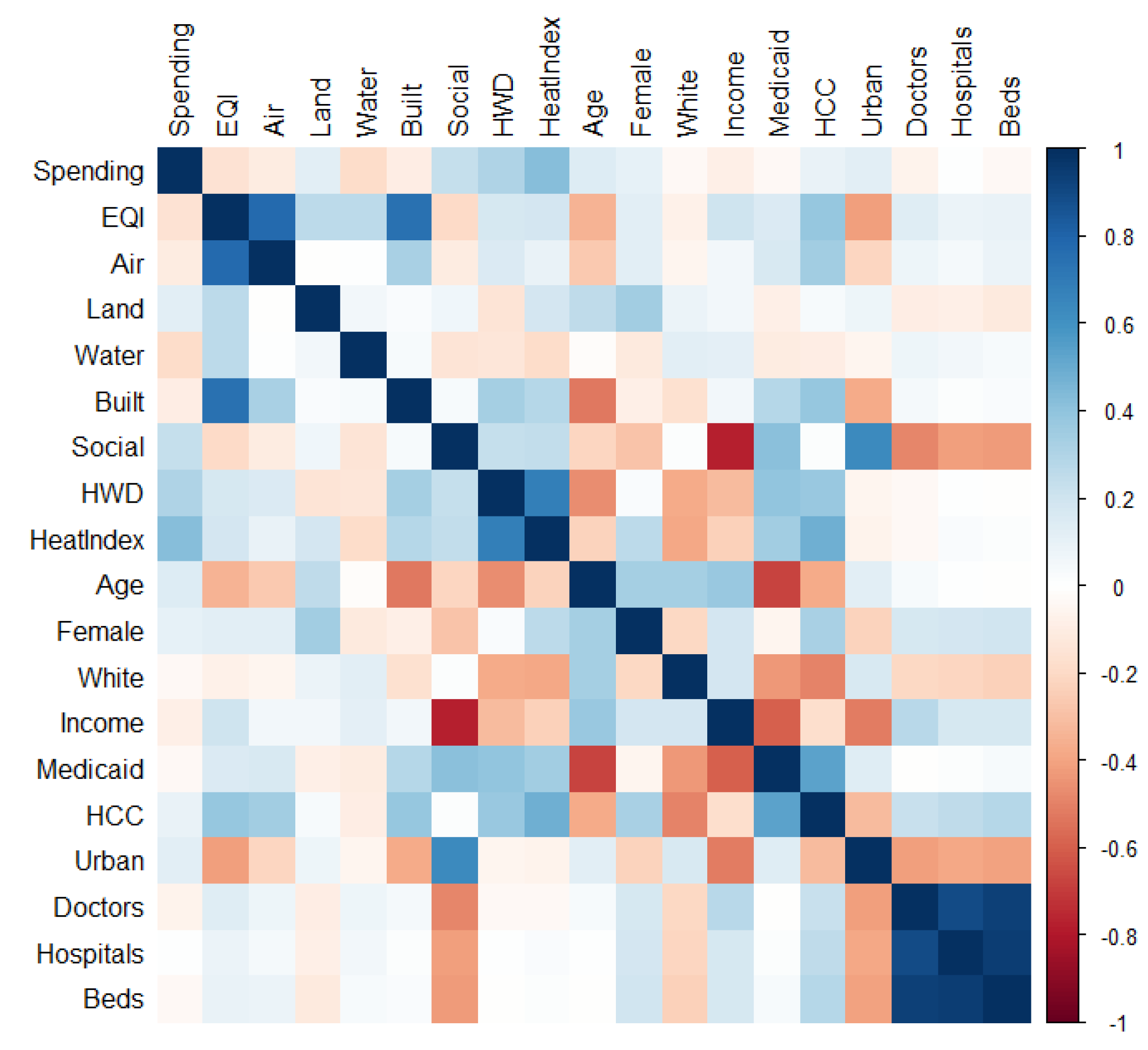
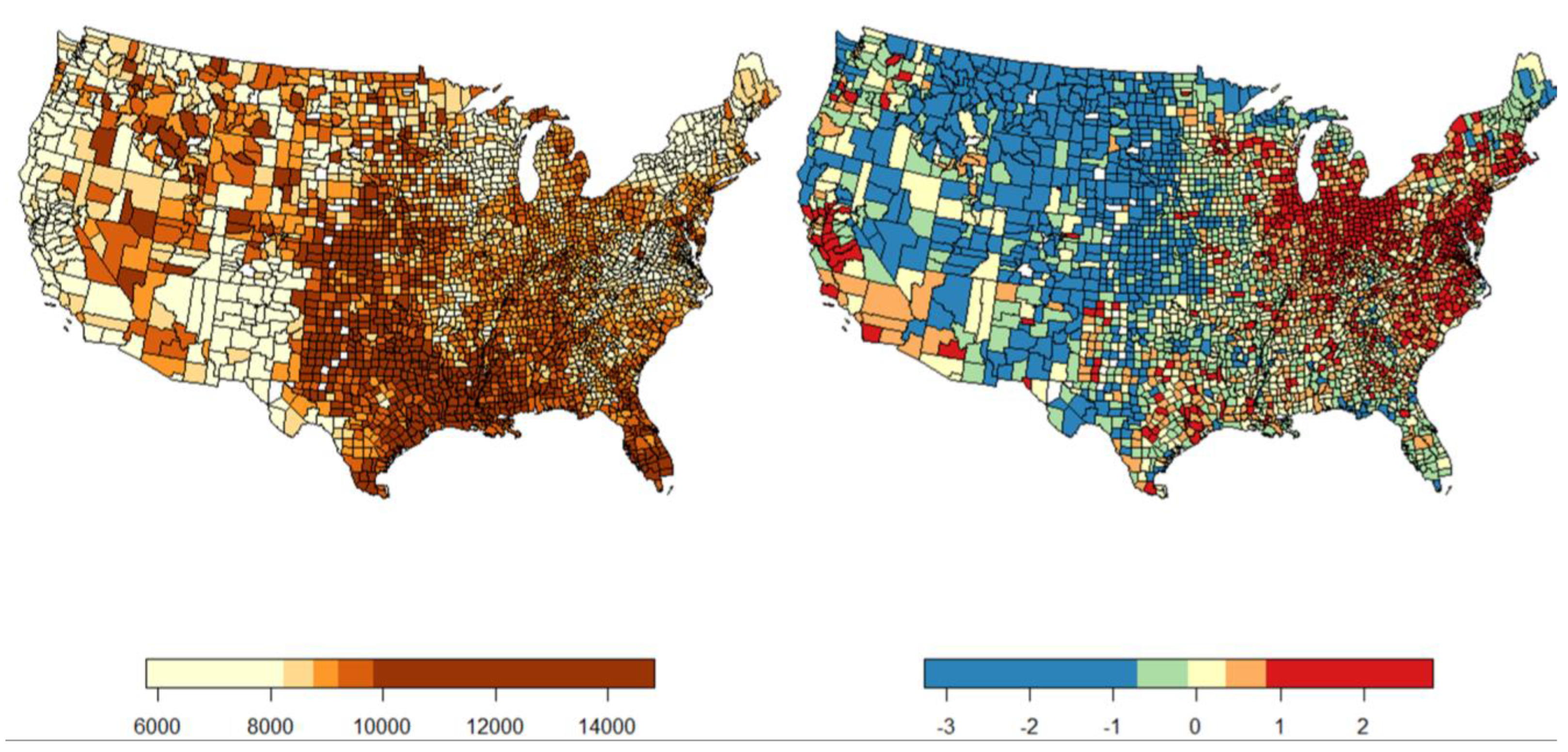
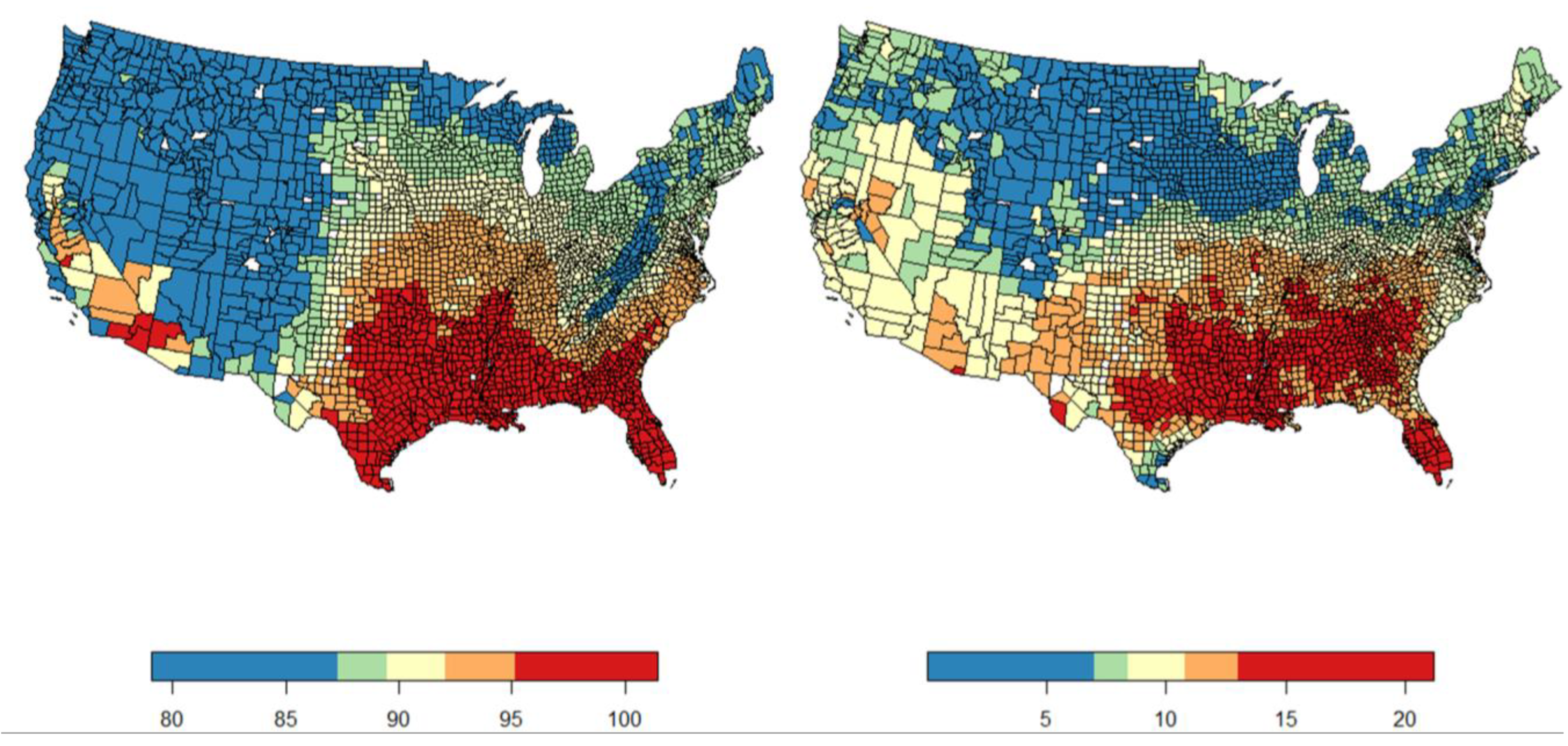
3.1. Exploratory Analysis
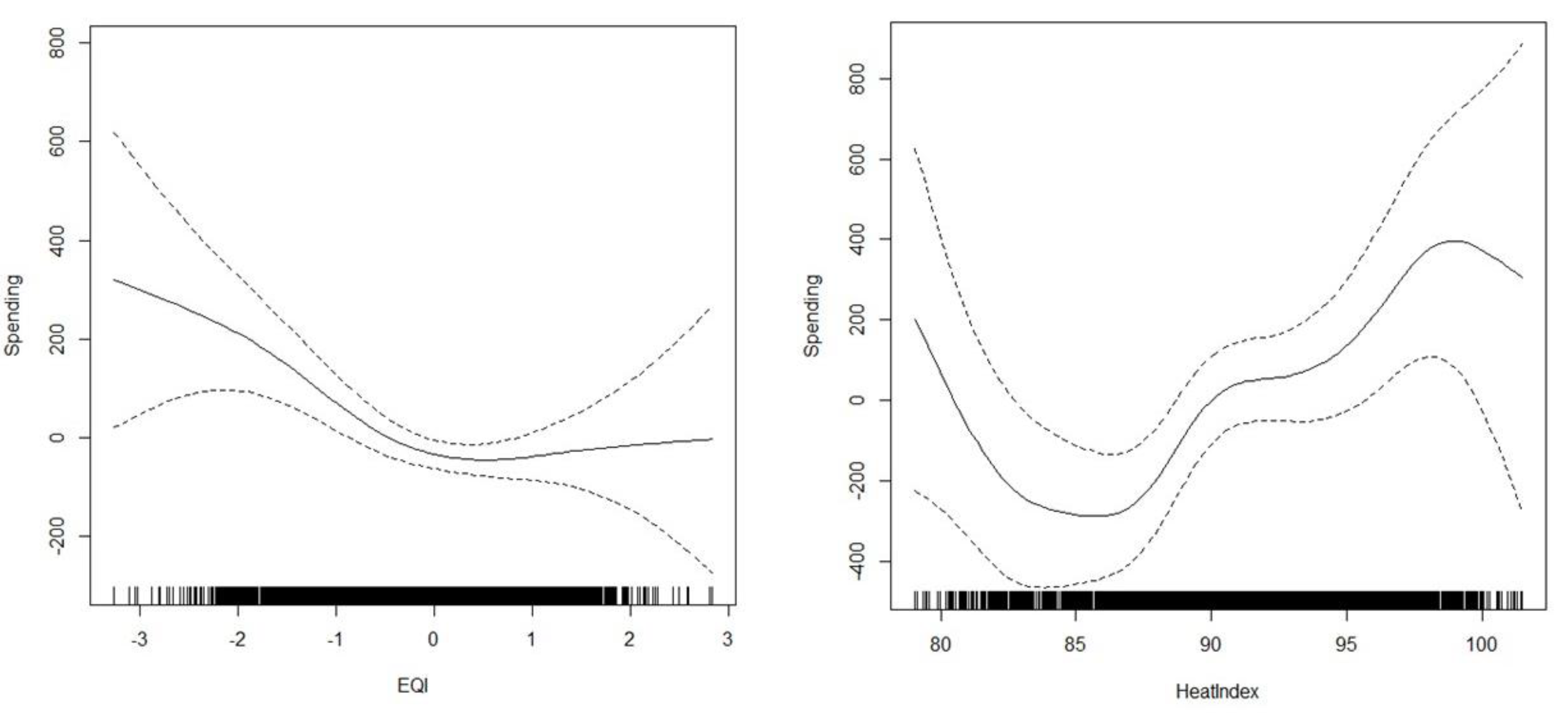
3.2. Main Results
4. Discussion
Strengths and Limitations
5. Conclusions
Supplementary Materials
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Brender, J.D.; Maantay, J.A.; Chakraborty, J. Residential proximity to environmental hazards and adverse health outcomes. Am. J. Public Health 2011, 101 (Suppl. S1), S37–S52. [Google Scholar] [CrossRef] [PubMed]
- Kim, K.H.; Kabir, E.; Kabir, S. A review on the human health impact of airborne particulate matter. Environ. Int. 2015, 74, 136–143. [Google Scholar] [CrossRef]
- Jian, Y.; Messer, L.C.; Jagai, J.S.; Rappazzo, K.M.; Gray, C.L.; Grabich, S.C.; Lobdell, D.T. Associations between environmental quality and mortality in the contiguous United States, 2000–2005. Environ. Health Perspect. 2017, 125, 355–362. [Google Scholar] [CrossRef]
- Remoundou, K.; Koundouri, P. Environmental effects on public health: An economic perspective. Int. J. Environ. Res. Public Health 2009, 6, 2160–2178. [Google Scholar] [CrossRef]
- Sætterstrøm, B.; Kruse, M.; Brønnum-Hansen, H.; Bønløkke, J.H.; Meulengracht Flachs, E.; Sørensen, J. A method to assess the potential effects of air pollution mitigation on healthcare costs. J. Environ. Public Health 2012, 2012, 935825. [Google Scholar] [CrossRef] [PubMed]
- Roy, A.; Sheffield, P.; Wong, K.; Trasande, L. The effects of outdoor air pollutants on the costs of pediatric asthma hospitalizations in the United States, 1999–2007. Med. Care 2011, 49, 810. [Google Scholar] [CrossRef]
- Lightwood, J.; Glantz, S.A. Smoking behavior and healthcare expenditure in the United States, 1992–2009: Panel data estimates. PLoS Med. 2016, 13, e1002020. [Google Scholar] [CrossRef] [PubMed]
- Yao, T.; Sung, H.Y.; Wang, Y.; Lightwood, J.; Max, W. Healthcare costs attributable to secondhand smoke exposure at home for US adults. Prev. Med. 2018, 108, 41–46. [Google Scholar] [CrossRef]
- Huovinen, E.; Laine, J.; Virtanen, M.J.; Snellman, M.; Hujanen, T.; Kiiskinen, U.; Kujansuu, E.; Lumio, J.; Ruutu, P.; Kuusi, M. Excess healthcare costs of a large waterborne outbreak in Finland. Scand. J. Public Health 2013, 41, 761–766. [Google Scholar] [CrossRef]
- Corso, P.S.; Kramer, M.H.; Blair, K.A.; Addiss, D.G.; Davis, J.P.; Haddix, A.C. Costs of illness in the 1993 waterborne Cryptosporidium outbreak, Milwaukee, Wisconsin. Emerg. Infect. Dis. 2003, 9, 426. [Google Scholar] [CrossRef]
- DeFlorio-Barker, S.; Wing, C.; Jones, R.M.; Dorevitch, S. Estimate of incidence and cost of recreational waterborne illness on United States surface waters. Environ. Health 2018, 17, 3. [Google Scholar] [CrossRef] [PubMed]
- Alzahrani, F.; Collins, A.R.; Erfanian, E. Drinking water quality impacts on health care expenditures in the United States. Water Resour. Econ. 2020, 32, 100162. [Google Scholar] [CrossRef]
- Noe, R.S.; Jin, J.O.; Wolkin, A.F. Exposure to natural cold and heat: Hypothermia and hyperthermia Medicare claims, United States, 2004–2005. Am. J. Public Health 2012, 102, e11–e18. [Google Scholar] [CrossRef] [PubMed]
- Wondmagegn, B.Y.; Xiang, J.; Williams, S.; Pisaniello, D.; Bi, P. What do we know about the healthcare costs of extreme heat exposure? A comprehensive literature review. Sci. Total Environ. 2019, 657, 608–618. [Google Scholar] [CrossRef]
- Abdullah, H.; Azam, M.; Zakariya, S.K. The impact of environmental quality on public health expenditure in Malaysia. Asia Pac. J. Adv. Bus. Soc. Stud. 2016, 2, 365–379. [Google Scholar]
- Alimi, O.Y.; Ajide, K.B.; Isola, W.A. Environmental quality and health expenditure in ECOWAS. Environ. Dev. Sustain. 2019, 22, 5105–5127. [Google Scholar] [CrossRef]
- Ibukun, C.O.; Osinubi, T.T. Environmental Quality, Economic Growth, and Health Expenditure: Empirical Evidence from a Panel of African Countries. Afr. J. Econ. Rev. 2020, 8, 119–140. [Google Scholar]
- Marsh, K.; Ganz, M.; Nørtoft, E.; Lund, N.; Graff-Zivin, J. Incorporating environmental outcomes into a health economic model. Int. J. Technol. Assess. Health Care 2016, 32, 400–406. [Google Scholar] [CrossRef]
- Patel, A.P.; Jagai, J.S.; Messer, L.C.; Gray, C.L.; Rappazzo, K.M.; Deflorio-Barker, S.A.; Lobdell, D.T. Associations between environmental quality and infant mortality in the United States, 2000–2005. Arch. Public Health 2018, 76, 60. [Google Scholar] [CrossRef]
- Gray, C.L.; Lobdell, D.T.; Rappazzo, K.M.; Jian, Y.; Jagai, J.S.; Messer, L.C.; Patel, A.P.; De Florio-Barker, S.A.; Lyttle, C.; Solway, J.; et al. Associations between environmental quality and adult asthma prevalence in medical claims data. Environ. Res. 2018, 166, 529–536. [Google Scholar] [CrossRef]
- Jagai, J.S.; Krajewski, A.K.; Shaikh, S.; Lobdell, D.T.; Sargis, R.M. Association between environmental quality and diabetes in the USA. J. Diabetes Investig. 2020, 11, 315–324. [Google Scholar] [CrossRef] [PubMed]
- Bunker, A.; Wildenhain, J.; Vandenbergh, A.; Henschke, N.; Rocklöv, J.; Hajat, S.; Sauerborn, R. Effects of air temperature on climate-sensitive mortality and morbidity outcomes in the elderly; a systematic review and meta-analysis of epidemiological evidence. eBioMedicine 2016, 6, 258–268. [Google Scholar] [CrossRef] [PubMed]
- Hadley, J.; Waidmann, T. Health insurance and health at age 65: Implications for medical care spending on new Medicare beneficiaries. Health Serv. Res. 2006, 41, 429–451. [Google Scholar] [CrossRef]
- Charron-Chénier, R.; Mueller, C.W. Racial disparities in medical spending: Healthcare expenditures for black and white households (2013–2015). Race Soc. Probl. 2018, 10, 113–133. [Google Scholar] [CrossRef]
- Thornton, J.A.; Rice, J.L. Determinants of healthcare spending: A state level analysis. Appl. Econ. 2008, 40, 2873–2889. [Google Scholar] [CrossRef]
- United State Census Bureau. County Population Totals; 2010–2019. 2019. Available online: https://www.census.gov/data/tables/time-series/demo/popest/2010s-counties-total.html (accessed on 1 September 2020).
- Centers for Medicare Medicaid Services. Rural–Urban Disparities in Health Care in Medicare; Centers for Medicare Medicaid Services: Baltimore, MD, USA, 2019. [Google Scholar]
- National Climate Assessment. Extreme Heat Events: Heat Wave Days in May—September for years 1981–2010 on CDC WONDER Online Database, Released 2015. 2022. Available online: http://wonder.cdc.gov/NCA-heatwavedays-historic.html (accessed on 1 September 2022).
- Zuckerman, S.; Waidmann, T.; Berenson, R.; Hadley, J. Clarifying sources of geographic differences in Medicare spending. N. Engl. J. Med. 2010, 363, 54–62. [Google Scholar] [CrossRef] [PubMed]
- United States Census Bureau. US Census. 2022. Available online: https://www.census.gov/en.html (accessed on 1 September 2022).
- Kelley, A.S.; Ettner, S.L.; Morrison, R.S.; Du, Q.; Wenger, N.S.; Sarkisian, C.A. Determinants of medical expenditures in the last 6 months of life. Ann. Intern. Med. 2011, 154, 235–242. [Google Scholar] [CrossRef]
- Health Resources and Services Administration. Area Health Resource Files. 2018. Available online: https://datawarehouse.hrsa.gov/topics/ahrf.aspx (accessed on 1 September 2020).
- Mansfield, E.R.; Helms, B.P. Detecting multicollinearity. Am. Stat. 1982, 36, 158–160. [Google Scholar]
- Moran, P.A. A test for the serial independence of residuals. Biometrika 1950, 37, 178–181. [Google Scholar] [CrossRef]
- Akaike, H. A new look at the statistical model identification. IEEE Trans. Autom. Control 1974, 19, 716–723. [Google Scholar] [CrossRef]
- Wood, S.N. Fast stable restricted maximum likelihood and marginal likelihood estimation of semiparametric generalized linear models. J. R. Stat. Soc. B 2011, 73, 3–36. [Google Scholar] [CrossRef]
- Bivand, R.; Wong, D.W.S. Comparing implementations of global and local indicators of spatial association. TEST 2018, 27, 716–748. [Google Scholar] [CrossRef]
- Trubka, R.; Newman, P.; Bilsborough, D. The costs of urban sprawl–Infrastructure and transportation. Environ. Des. Guide 2010, 83, 1–6. [Google Scholar]
- Yancey, A.K.; Fielding, J.E.; Flores, G.R.; Sallis, J.F.; McCarthy, W.J.; Breslow, L. Creating a robust public health infrastructure for physical activity promotion. Am. J. Prev. Med. 2007, 32, 68–78. [Google Scholar] [CrossRef] [PubMed]
- Garrido, M.M.; Deb, P.; Burgess, J.F., Jr.; Penrod, J.D. Choosing models for health care cost analyses: Issues of nonlinearity and endogeneity. Health Serv. Res. 2012, 47, 2377–2397. [Google Scholar] [CrossRef]
- Hawkins, B.A.; Diniz-Filho, J.A.F.; Mauricio Bini, L.; De Marco, P.; Blackburn, T.M. Red herrings revisited: Spatial autocorrelaton and parameter estimation in geographical ecology. Ecography 2007, 30, 375–384. [Google Scholar] [CrossRef]
| Heatwave Days | HeatIndex | |||
|---|---|---|---|---|
| Estimate | p Value | Estimate | p Value | |
| Smoothed | ||||
| EQI | NA | 0.004 | NA | 0.006 |
| Heat | NA | 0.354 | NA | 0.001 |
| Geosmoother | NA | 0.000 | NA | 0.000 |
| Linear | ||||
| Age | 115.21 | 0.000 | 116.1 | 0.000 |
| Female | −32.84 | 0.000 | −32.1 | 0.000 |
| White | 6.21 | 0.000 | 6.9 | 0.000 |
| Medicaid | −1.40 | 0.691 | −1.6 | 0.651 |
| HCC | 895.63 | 0.002 | 837.7 | 0.005 |
| Income | 0.01 | 0.010 | 0.0 | 0.031 |
| Doctors | −0.46 | 0.001 | −0.4 | 0.003 |
| Hospitals | 34.81 | 0.000 | 31.5 | 0.000 |
| Urban | 59.48 | 0.000 | 59.5 | 0.000 |
| Fit statistics | ||||
| R-sq.(adj) | 0.65 | 0.65 | ||
| Deviance explained | 0.68 | 0.69 | ||
| Moran’s I | 0.00 | 0.5 | 0.00 | 0.4 |
| Estimate | p Value | |
|---|---|---|
| Smoothed | ||
| Air | NA | 0.930 |
| Water | NA | 0.920 |
| Land | NA | 1.000 |
| Built | NA | 0.002 |
| Social | NA | 0.000 |
| Heat | NA | 0.320 |
| Geosmoother | NA | 0.000 |
| Linear | ||
| Age | 78.40 | 0.000 |
| Female | 1.05 | 0.909 |
| White | 5.24 | 0.001 |
| Medicaid | −12.54 | 0.001 |
| HCC | 1081.61 | 0.000 |
| Income | 0.01 | 0.000 |
| Doctors | −0.63 | 0.000 |
| Hospitals | 48.41 | 0.000 |
| Urban | 19.34 | 0.159 |
| Fit statistics | ||
| R-sq.(adj) | 0.66 | |
| Deviance explained | 0.70 | |
| Moran’s I | −0.01 | 0.7 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Becker, D.A. Environmental Quality, Extreme Heat, and Healthcare Expenditures. Int. J. Environ. Res. Public Health 2024, 21, 1322. https://doi.org/10.3390/ijerph21101322
Becker DA. Environmental Quality, Extreme Heat, and Healthcare Expenditures. International Journal of Environmental Research and Public Health. 2024; 21(10):1322. https://doi.org/10.3390/ijerph21101322
Chicago/Turabian StyleBecker, Douglas A. 2024. "Environmental Quality, Extreme Heat, and Healthcare Expenditures" International Journal of Environmental Research and Public Health 21, no. 10: 1322. https://doi.org/10.3390/ijerph21101322





