The Development of an Oral Health Nursing Tool for Patients with a Psychotic Disorder: A Human-Centred Design with a Feasibility Test
Abstract
:1. Introduction
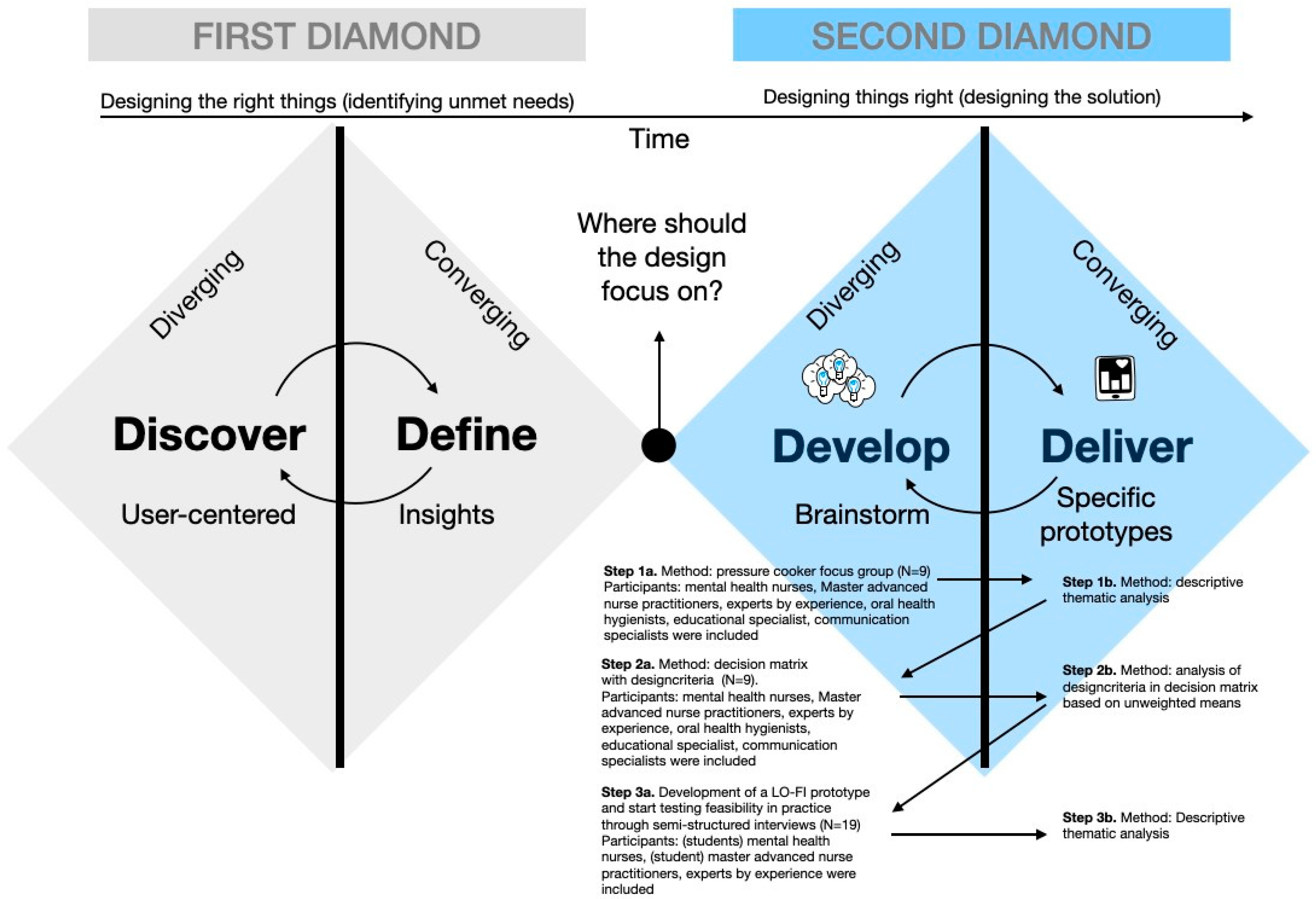
2. Methods
2.1. Study Design
2.2. Study Population
2.3. Data Collection
- Step 1a: Pressure cooker focus group session
2.4. Analysis
2.5. Ethical Considerations
3. Results
3.1. Participants and Outcome Focus Groups: Step 1
- Key theme 1: Patients and MHNs in practice regarding oral health
“A patient is not aware of it himself; patients live in their own reality and if patients are ill, they simply are not always aware of it. MHNs need to bring this up for discussion”. (Participant 9, MHN)
“For example, I also have a patient, and when I speak with her, I can see that she has a lot of dirt and plaque on her teeth. I discuss it with her every time, but she keeps saying, ‘No, it’s going well, and I will go to the dentist,’ and I find that challenging. I try to bring up the topic of oral care again. However, I notice that she gets annoyed when I discuss it repeatedly”. (Participant 6, MHN)
- Key theme 2: Preferred oral health tools, focusing on MHNs working with patients with psychotic disorders
“If MHNs do not have a clear understanding of the background of tools targeting patients with a psychotic disorder, MHNs cannot address, advise, or monitor them effectively”. (Participant 4, MHN/lecturer)
“If we provide this to every patient when they start receiving care, it also prevents us from discovering too late that the materials are not available. This is crucial because patients with a psychotic disorder often do not think to bring these items. If we routinely include this during the anamnesis, it will not be forgotten by MHNs”. (Participant 2, MHN)
“Mouthwashes can aid in combating these bacteria and temporarily freshening the breath. Additionally, it is important for the toothpaste to contain fluoride, as fluoride is known to protect the teeth against acids and sugars”.(Participant 5, oral health hygienist)
“Yes, that’s a great idea, and let’s especially emphasize the benefits of good oral health to keep it positive”. (Participant 1, experienced expert/communication specialist)
“In the hospital, you would also have an awareness screener to verify if the brochure has been distributed and discussed, enabling a later follow-up. These are the focal points”. (Participant 8, MHN)
- Key theme 3: Intended outcomes of tools
3.2. MCDM Results: Step 2
3.3. Development of the Brochure with Awareness Screener and the Outcomes of the Feasibility Test: Step 3
3.3.1. Development of the Brochure with Awareness Screener
3.3.2. Outcomes Feasibility Test
- Acceptability
“Content-wise, the brochure is exceptionally strong for MHNs. It is a comprehensive brochure covering diverse topics, including general oral care. For myself, it is also beneficial to read. This prompts consideration of personal application… This brochure is useful for everyone to look through. It particularly emphasizes the risks, underscoring the importance of proactive engagement with these issues”. (Participant 9, MHN and somatic screening practitioner)
- Demand
“There is no explicit demand for this; we conduct our work without adequately focusing on oral care. However, this neglect is intrinsically related to the demographic with psychotic disorders. Although the demand might not be apparent, if we as nurses provide the service and remain attentive, then such a brochure, I surmise, would be beneficial in enhancing our alertness to these needs”. (Participant 3, MHN and somatic screening practitioner)
- Implementation (expected issues)
- Practicality
“Precisely because the brochure effectively emphasizes the importance of oral care, it leads to an increased sensitization among nursing professionals about their role in oral health, making it difficult for them to overlook this aspect any longer”. (Participant 8, mental health nurse and somatic screening practitioner)
“Health insurance providers should ideally include preventative oral care in their basic coverage plans. It is peculiar that while lifestyle programs for overweight individuals are offered at no cost, dental care does not receive the same treatment. This is a significant issue, as proper oral care is equally vital for overall health”. (Participant 5, advanced nurse practitioner)
“Another important consideration involves key stakeholders, e.g., health insurers. Given the significant costs associated with oral care, particularly for uninsured individuals, it may be prudent to seek contributions from them. Addressing oral care is relevant not only from a health perspective but also from a business standpoint. Additionally, poor dental health can lead to embarrassment and social withdrawal, hindering participation in society and employment opportunities. This is where local governments can also play a role, potentially by subsidizing costs”. (Participant 12, master’s student in advanced nursing)
- Integration
“Nurses who take ownership of a specific topic tend to work with greater dedication and enthusiasm”. (Participant 12, master’s student in advanced nursing)
- Efficacy
4. Discussion
Strengths and Limitations of This Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A. A Selection of the Inspiration Cards Used to Inspire Creativity in MHNs during the Focus Group

Appendix B. Topic List Feasibility Semi-Structured Interviews
- Gender
- Age
- Educational level
- Profession
- Years of working experience with patients with a psychotic disorder
- Working with in- or outpatients
| Topics | Sample Questions |
| Acceptability | To what extent is the brochure with awareness screener judged as suitable, satisfying, or attractive to MHNs? What is the participants’ satisfaction and intention to start using? Does it fit within organisational norms and values? What substantive changes or additions are there? |
| Demand | To what extent is this brochure with awareness screener likely to be used (i.e., how much demand is likely to exist)? Is there any expressed interest? |
| Implementation | To what extent can this brochure with awareness screener be successfully delivered to MHNs in care for patients with a psychotic disorder? What success or failure can we expect? Are there resources or tools needed to implement it? Which factors can possibly affect implementation? |
| Practicality | To what extent can this brochure with awareness screener be carried out with MHNs using existing means, resources, and circumstances and without outside intervention? Do you have examples? Are there any positive or negative effects expected? Can you tell us something about the expected costs? |
| Integration | To what extent can this brochure with awareness screener be integrated within the context of work? Do you have examples? What is the perceived sustainability? What are the costs to organisations? |
| Efficacy | Does this brochure with awareness screener show promise of being successful with MHNs? What intended effects do you expect? |
Appendix C. Characteristics of Professionals and Experts Included in the Semi-Structured Interviews (n = 19)
| Male/Female | Age in Years | Profession | Education | Years of Working Experience | In- or Outpatients | |
| 1 | Female | 27 | Social psychiatric nurse | Bachelor of Nursing, Social Psychiatric Nursing | 5 | Outpatients |
| 2 | Female | 26 | Student Bachelor of Nursing | Final-year student of Bachelor of Nursing | 2 | Outpatients |
| 3 | Female | 34 | Mental health nurse and somatic screening practitioner | Bachelor of Nursing | 2 | Outpatients |
| 4 * | Female | 50 | Mental health nurse | Bachelor of Nursing | 28 | Outpatients |
| 5 | Female | 35 | Master’s-level advanced nurse practitioner | Master of Advanced Nursing Practice | 12 | Outpatients |
| 6 | Female | 39 | Master’s-level advanced nurse practitioner and manager of treatment affairs | Master of Advanced Nursing Practice |Bachelor of Business Administration | 18 | Outpatients |
| 7 * | Female | 30 | Master’s-level advanced nurse practitioner | Master of Advanced Nursing Practice | 5 | Inpatients |
| 8 | Female | 48 | Master’s-level advanced nurse practitioner | Master of Advanced Nursing Practice, Ph.D. | 20 | Inpatients |
| 9 | Female | 58 | Mental health nurse and somatic screening practitioner | Bachelor of Nursing | 20 | Outpatients |
| 10 | Female | 45 | Mental health nurse | Master of Advanced Nursing Practice | 13 | Outpatients |
| 11 | Male | 44 | Mental health nurse | Secondary vocational education in Nursing | 3 | Outpatients |
| 12 | Female | 45 | Student Master of Advanced Nursing Practice | Student Master of Advanced Nursing Practice| Bachelor of Business Administration | 14 | Outpatients |
| 13 | Female | 32 | Expert by experience | Associate degree for expert by experience, Bachelor of Social work | 5 | Inpatients |
| 14 | Male | 35 | Expert by experience | Associate degree for expert by experience | 5 | Inpatients |
| 15 | Male | 32 | Expert by experience | Associate degree for expert by experience | 3 | Inpatients |
| 16 | Female | 37 | Expert by experience and client participation representative | Bachelor French | 20 | Inpatients |
| 17 | Female | 44 | Expert by experience | Associate degree for expert by experience, Bachelor of Business Economics | 2 | Inpatients |
| 18 | Male | 33 | Expert by experience | Associate degree for expert by experience | 2 | Inpatients and outpatients |
| 19 | Male | 34 | Expert by experience | Associate degree for expert by experience | 4 | Outpatients |
| * Participants were also engaged in earlier studies [23]. | ||||||
Appendix D. Preview of the Layout of the Brochure
Appendix E. Content of the Brochure with Awareness Screener for MHNs (Translated from Dutch)
- Introduction: The Importance of Good Oral Health
- 2.
- Psychological and Social Complaints|Stigma
- 3.
- Physical Complaints
- 4.
- Risk Factors
- -
- Mental health (such as stress or anxiety). Stress or anxiety can contribute to serious oral health conditions. Stress and anxiety suppress the immune system, making people more susceptible to disease and infection. Stress affects oral health, leading to a dryer mouth more quickly.
- -
- Fear of the dentist? Talk about it. Dentists and dental hygienists are there to help and are willing to discuss the situation. There are many options available, including taking anti-anxiety medication before an appointment or using conscious sedation.
- -
- Medication. Side effects of antipsychotics (e.g., clozapine, olanzapine, quetiapine) can cause dry mouth (xerostomia) or insufficient saliva (hyposalivation). This is covered in more detail in the “Medication” chapter.
- -
- Smoking and cannabis use. When people smoke, harmful substances like nicotine and tar are released into the mouth. Nicotine reduces the blood flow to the gums, making them less accessible to immune cells. It also prevents the gums from bleeding quickly, so someone may not notice if there is something wrong with their gums. Smoking also reduces saliva production. With a shortage of immune cells and saliva, there will be fewer defense agents in the oral cavity, increasing the risk of plaque, cavities, and subsequently gum inflammation. Smokers have more plaque than non-smokers. If not carefully removed, plaque develops into tartar and cavities. Tartar causes gum problems such as gum inflammation. As the blood vessels narrow due to smoking, inflamed gums are noticed later, and by then there may already be penetration into the jawbone, potentially causing teeth to become loose and fall out.
- -
- Diabetes. It is well known that antipsychotics often have side effects, but they can also lead to the development of type 2 diabetes (metabolic problems). People with diabetes are more susceptible to mouth inflammation. Healing of inflamed gums often proceeds less well in these people. With both types of diabetes, blood sugar is often high, which can affect the mouth, leading to earlier cavities, dry mouth, fungal infections, and extra plaque, increasing the chance of gum inflammation (gingivitis and periodontitis). Inflammation in the mouth can also lead to complications in overall health.
- -
- Alcohol use. Alcohol is known to decrease saliva flow. As a result, the mouth becomes drier, and in a drier mouth, caries (tooth decay) and gum inflammation can develop more quickly. To add a fresh taste to drinks, citric acid is often added. With frequent use, food acids (both natural and added) cause tooth erosion, which is the wearing away of the tooth surface.
- 5.
- Nutrition
- 6.
- Medications, Side Effects, and Their Impact on Dental Health
- 7.
- Problems in the Mouth
- -
- Cavities. The formation of cavities is a significant side effect of medication that can cause lasting damage to the teeth. Cavities from medication can sometimes develop within weeks to months after starting the drug. The primary cause of medication-induced cavities is reduced saliva secretion. Nearly 90% of antipsychotic medications lead to a dry mouth due to reduced saliva. Tablets (such as XyliMelts) can help to reduce dry mouth symptoms.
- -
- Inflamed gums (Gingivitis). Healthy gums are pink. Inflamed gums are redder in colour, more swollen, and bleed more easily during brushing and when using floss/toothpick/interdental brush. A bad taste or bad breath can also indicate inflamed gums. Inflamed gums rarely cause pain. The inflammation at the edge of the gums is caused by bacteria in plaque, to which the gums react. Plaque calcifies into tartar and adheres firmly to the teeth and molars, forming a new layer. This cannot be removed by an individual and requires a dentist or dental hygienist. If not treated, the inflammation can damage the jawbone, leading to bone loss. Inflamed gums are preventable and curable with good oral hygiene. Bleeding gums means there is inflammation. This signal should not be ignored, and those affected should take action to get the gums healthy again. The cause of inflamed gums is plaque, so keeping the mouth clean is crucial.
- -
- Gum inflammation (Periodontitis). Periodontitis is an advanced stage of gum inflammation. Because the inflammation has been in the mouth for some time, it easily spreads from the gums to the jawbone beneath. This results in the loss of jawbone around the teeth and molars. Deep spaces form under the gums where plaque and tartar accumulate, known as pockets. These pockets need to be cleaned by a dental hygienist to heal the gums.
- -
- Bad breath (Halitosis). In most cases, bad breath originates in the oral cavity, usually due to insufficient oral hygiene and gum inflammation. Sometimes, certain bacteria remaining on the back of the tongue can cause bad breath. Brushing or scraping the tongue with a tongue scraper can be a solution, supplemented with a special antibacterial mouthwash. Chewing gum, mouthwash, or mouth spray can mask the odor, but beware, they do not remove the cause of the bad breath.
- -
- Tooth enamel erosion (tooth erosion). All foods and drinks contain acids that can harm the teeth, like soft drinks, energy drinks, fruit juices, and iced tea. Black coffee, unsweetened tea, water, and milk contain less acid. The acids from our food soften the enamel and cause tooth and gum erosion. Unfortunately, tooth erosion only becomes visible in an advanced stage when the teeth are already severely damaged.
- 8.
- Advice: What advice can you give your patients?
- -
- Brush the teeth twice a day. This can be done with a regular or electric toothbrush. Use a soft brush head. Brushing should be done before going to bed and at least once during the day.
- -
- Use fluoride toothpaste. Fluoride helps prevent tooth decay and makes the enamel less soluble. This better protects the teeth against acids and sugars from food and drinks, reducing the likelihood of cavities.
- -
- Brush thoroughly. It is important to brush thoroughly without damaging the teeth or gums. Ensure that all parts of the teeth (back, front, sides, and top) are cleaned.
- -
- Clean daily between teeth and molars using floss/interdental brushes/toothpicks. It is important to make time for this daily. Daily flossing/use of interdental brushes helps fight tooth decay and gum disease. It removes not only plaque but also any food particles left during the day. Avoid mouthwash directly after brushing, as it washes away the fluoride from the toothpaste.
- -
- Limit the number of eating and drinking moments. Moderating the frequency of eating and drinking is important to prevent tooth damage. Bacteria convert sugars, causing enamel dissolution and cavity formation. If someone chooses to enjoy something sweet, they should eat it during lunch or dinner when the mouth has more saliva. Saliva can break down acids and remove leftover food from the mouth. It is also important to limit the number of sweet/acid attacks per day to a maximum of six or seven times.
- -
- Visit a dentist or dental hygienist regularly. To prevent problems and keep the mouth and teeth in good condition, it is wise to schedule regular appointments with a dentist or dental hygienist. Typically, this means visits twice a year, but the exact frequency depends on the condition of the teeth.
- -
- Ask your patient if they have brushed their teeth. Link this to medication times.
- -
- Regularly drinking small amounts of water and rinsing food with water can provide relief.
- -
- Good oral hygiene, adequate fluid intake, and the use of (sugar-free) products that stimulate saliva flow can alleviate dry mouth symptoms and prevent complications.
- -
- Artificial saliva or tablets like XyliMelts (there are many other brands), self-adhesive tablets that stick to the gums, inside the cheek, dissolve slowly and completely and counteract dry mouth symptoms by slowly releasing xylitol, which stimulates the production of natural saliva and helps reduce the formation of plaque and cavities.
- -
- They can be used four to eight times a day and are available online as an over-the-counter product.
- 9.
- Awareness screener→→→→→Date to fill in: --/--/----
- With this awareness screener, you can revisit the brochure with your patient later and discuss individual dental care needs together.
- ○
- The content of the brochure has been reviewed, based on the needs of the individual patient.
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
| Worst imaginable | Average | Best imaginable | |||||||
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
| Worst imaginable | Average | Best imaginable | |||||||
References
- Petersen, P.E. The World Oral Health Report 2003: Continuous Improvement of Oral Health in the 21st Century—The Approach of the WHO Global Oral Health Programme: The World Oral Health Report 2003. Community Dent. Oral Epidemiol. 2003, 31, 3–24. [Google Scholar]
- Petersen, P.E. Priorities for Research for Oral Health in the 21st Century—The Approach of the WHO Global Oral Health Programme. Community Dent. Health 2005, 22, 71–74. [Google Scholar] [PubMed]
- Kisely, S.; Quek, L.H.; Pais, J.; Lalloo, R.; Johnson, N.W.; Lawrence, D. Advanced Dental Disease in People with Severe Mental Illness: Systematic Review and Meta-Analysis. Br. J. Psychiatry 2011, 199, 187–193. [Google Scholar] [CrossRef] [PubMed]
- Cormac, I.; Jenkins, P. Understanding the Importance of Oral Health in Psychiatric Patients. Adv. Psychiatr. Treat. 1999, 5, 53–60. [Google Scholar] [CrossRef]
- Kilbourne, A.M.; Horvitz-Lennon, M.; Post, E.P.; McCarthy, J.F.; Cruz, M.; Welsh, D.; Blow, F.C. Oral Health in Veterans Affairs Patients Diagnosed with Serious Mental Illness. J. Public Health Dent. 2007, 67, 42–48. [Google Scholar] [CrossRef] [PubMed]
- Kisely, S. No Mental Health without Oral Health. Can. J. Psychiatry 2016, 61, 277–282. [Google Scholar] [CrossRef] [PubMed]
- Kuipers, S.; Boonstra, N.; Kronenberg, L.; Keuning-Plantinga, A.; Castelein, S. Oral Health Interventions in Patients with a Mental Health Disorder: A Scoping Review with Critical Appraisal of the Literature. IJERPH 2021, 18, 8113. [Google Scholar] [CrossRef] [PubMed]
- Lam, P.C.; John, D.A.; Galfalvy, H.; Kunzel, C.; Lewis-Fernández, R. Oral Health–Related Quality of Life Among Publicly Insured Mental Health Service Outpatients With Serious Mental Illness. Psychiatr. Serv. 2019, 70, 1101–1109. [Google Scholar] [CrossRef] [PubMed]
- Kuipers, S.A.; Castelein, S.; Barf, H.; Kronenberg, L.; Boonstra, N. Risk Factors and Oral health-Control Comparison Between Patients Diagnosed with a Psychotic Disorder (First-Episode) and People from the General Population. J. Psychiatr. Ment. Health Nurs. 2022, 29, 430–441. [Google Scholar] [CrossRef]
- Griffiths, J.; Jones, V.; Leeman, I.; Lewis, D.; Blankenstein, R. Oral Health Care for People with Mental Health Problems; British Society for Disability and Oral Health: London, UK, 2000. [Google Scholar]
- McCreadie, R.G.; Stevens, H.; Henderson, J.; Hall, D.; McCaul, R.; Filik, R.; Young, G.; Sutch, G.; Kanagaratnam, G.; Perrington, S.; et al. The Dental Health of People with Schizophrenia. Acta Psychiatr. Scand. 2004, 110, 306–310. [Google Scholar] [CrossRef]
- Persson, K.; Axtelius, B.; SÖderfeldt, B.; Östman, M. Monitoring Oral Health and Dental Attendance in an Outpatient Psychiatric Population. J. Psychiatr. Ment. Health Nurs. 2009, 16, 263–271. [Google Scholar] [CrossRef]
- Slack-Smith, L.; Hearn, L.; Scrine, C.; Durey, A. Barriers and Enablers for Oral Health Care for People Affected by Mental Health Disorders. Aust. Dent. J. 2017, 62, 6–13. [Google Scholar] [CrossRef] [PubMed]
- Roebroek, L.O.; Bruins, J.; Boonstra, A.; Veling, W.; Jörg, F.; Sportel, B.E.; Delespaul, P.A.; Castelein, S. The Effects of a Computerized Clinical Decision Aid on Clinical Decision-Making in Psychosis Care. J. Psychiatr. Res. 2022, 156, 532–537. [Google Scholar] [CrossRef] [PubMed]
- Happell, B.; Scott, D.; Platania-Phung, C. Perceptions of Barriers to Physical Health Care for People with Serious Mental Illness: A Review of the International Literature. Issues Ment. Health Nurs. 2012, 33, 752–761. [Google Scholar] [CrossRef] [PubMed]
- Middleton, K.R.; Anton, S.D.; Perri, M.G. Long-Term Adherence to Health Behavior Change. Am. J. Lifestyle Med. 2013, 7, 395–404. [Google Scholar] [CrossRef] [PubMed]
- Nightingale, F. Notes on Nursing: What It Is, and What It Is Not; Dover Publications: New York, NY, USA, 1969; ISBN 978-0-486-22340-7. [Google Scholar]
- Riegel, F.; Crossetti, M.D.G.O.; Martini, J.G.; Nes, A.A.G. Florence Nightingale’s Theory and Her Contributions to Holistic Critical Thinking in Nursing. Rev. Bras. Enferm. 2021, 74, e20200139. [Google Scholar] [CrossRef] [PubMed]
- Huber, M.; Knottnerus, J.A.; Green, L.; Horst, H.V.D.; Jadad, A.R.; Kromhout, D.; Leonard, B.; Lorig, K.; Loureiro, M.I.; Meer, J.W.M.V.D.; et al. How Should We Define Health? BMJ 2011, 343, d4163. [Google Scholar] [CrossRef] [PubMed]
- Happell, B.; Platania-Phung, C.; Scott, D. Physical Health Care for People with Mental Illness: Training Needs for Nurses. Nurse Educ. Today 2013, 33, 396–401. [Google Scholar] [CrossRef] [PubMed]
- Kuipers, S.; Castelein, S.; Kronenberg, L.; van ’t Veer, J.; Boonstra, N. A Human-Centered Design Approach to Develop Oral Health Nursing Interventions in Patients with a Psychotic Disorder. Int. J. Environ. Res. Public Health 2023, 20, 3475. [Google Scholar] [CrossRef]
- Prochaska, J.O.; DiClemente, C.C. Transtheoretical Therapy: Toward a More Integrative Model of Change. Psychother. Theory Res. Pract. 1982, 19, 276–288. [Google Scholar] [CrossRef]
- Kuipers, S.; Castelein, S.; Malda, A.; Kronenberg, L.; Boonstra, N. Oral Health Experiences and Needs among Young Adults after a First-Episode Psychosis: A Phenomenological Study. J. Psychiatr. Ment. Health Nurs. 2018, 25, 475–485. [Google Scholar] [CrossRef]
- Design Council. Eleven Lessons: Managing Design in Eleven Global Companies; Design Council: London, UK, 2007. [Google Scholar]
- Kulcsar, I. The Characteristics of a New Semantic Standards Development Approach: The Pressure Cooker Method. Master’s Thesis, University of Twente, Enschede, The Netherlands, 2023. [Google Scholar]
- van ’t Veer, J.; Wouters, E.; Veeger, M.; van der Lugt, R. Ontwerpen Voor Zorg en Welzijn; Eerste druk, tweede oplage; Uitgeverij Coutinho: Bussum, The Netherlands; ISBN 978-90-469-0691-0.
- Pressure Cooker. Een Effectieve Formule Voor Het Realiseren van Je Doelen. Available online: https://www.gamechanger.nl/pressure-cooker-sessie# (accessed on 20 September 2023).
- Casakin, H.P. Metaphors in Design Problem Solving: Implications for Design Creativity. Int. J. Des. 2007, 1, 23–35. [Google Scholar]
- Marsh, K.; Lanitis, T.; Neasham, D.; Orfanos, P.; Caro, J. Assessing the Value of Healthcare Interventions Using Multi-Criteria Decision Analysis: A Review of the Literature. PharmacoEconomics 2014, 32, 345–365. [Google Scholar] [CrossRef] [PubMed]
- Bowen, D.J.; Kreuter, M.; Spring, B.; Cofta-Woerpel, L.; Linnan, L.; Weiner, D.; Bakken, S.; Kaplan, C.P.; Squiers, L.; Fabrizio, C.; et al. How We Design Feasibility Studies. Am. J. Prev. Med. 2009, 36, 452–457. [Google Scholar] [CrossRef]
- De Cocker, K.; Veldeman, C.; De Bacquer, D.; Braeckman, L.; Owen, N.; Cardon, G.; De Bourdeaudhuij, I. Acceptability and Feasibility of Potential Intervention Strategies for Influencing Sedentary Time at Work: Focus Group Interviews in Executives and Employees. Int. J. Behav. Nutr. Phys. Act. 2015, 12, 22. [Google Scholar] [CrossRef]
- Braun, V.; Clarke, V. Using Thematic Analysis in Psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef]
- Braun, V.; Clarke, V. Reflecting on Reflexive Thematic Analysis. Qual. Res. Sport Exerc. Health 2019, 11, 589–597. [Google Scholar] [CrossRef]
- Torrance, G.W.; Feeny, D.; Furlong, W. Visual Analog Scales: Do They Have a Role in the Measurement of Preferences for Health States? Med. Decis. Mak. 2001, 21, 329–334. [Google Scholar] [CrossRef]
- Sanderson, K.; Nicholson, J.; Graves, N.; Tilse, E.; Oldenburg, B. Mental Health in the Workplace: Using the ICF to Model the Prospective Associations between Symptoms, Activities, Participation and Environmental Factors. Disabil. Rehabil. 2008, 30, 1289–1297. [Google Scholar] [CrossRef] [PubMed]
- Barik, A.L.; Purwaningtyas, R.A.; Astuti, D. The Effectiveness of Traditional Media (Leaflet and Poster) to Promote Health in a Community Setting in the Digital Era: A Systematic Review. J. NERS 2019, 14, 76–80. [Google Scholar] [CrossRef]
- Fogg Behavior Model. Available online: https://behaviormodel.org/ (accessed on 20 October 2023).
- Rogers, E.M. Diffusion of Innovations, Social, science, 5th ed.; Free Press trade paperback edition; Free Press: New York, NY, USA; London, UK; Toronto, ON, Canada; Sydney, Australia, 2003; ISBN 978-0-7432-2209-9. [Google Scholar]
- Miles, J.M.; Scott, E.S. A New Leadership Development Model for Nursing Education. J. Prof. Nurs. 2019, 35, 5–11. [Google Scholar] [CrossRef]
- Buswell, G.; Haime, Z.; Lloyd-Evans, B.; Billings, J. A Systematic Review of PTSD to the Experience of Psychosis: Prevalence and Associated Factors. BMC Psychiatry 2021, 21, 9. [Google Scholar] [CrossRef]
- Patterson-Norrie, T.; Ramjan, L.; Sousa, M.S.; George, A. Oral Health and Individuals with a Lived Experience of an Eating Disorder: A Qualitative Study. J. Eat. Disord. 2023, 11, 121. [Google Scholar] [CrossRef]
- Kouidrat, Y.; Amad, A.; Lalau, J.-D.; Loas, G. Eating Disorders in Schizophrenia: Implications for Research and Management. Schizophr. Res. Treat. 2014, 2014, 791573. [Google Scholar] [CrossRef]
- Common European Framework of Reference for Languages: Learning, Teaching, Assessment; Europarat (Ed.) 10th print; Cambridge University Press: Cambridge, UK, 2010; ISBN 978-0-521-80313-7. [Google Scholar]
- Van Aken, J.; Chandrasekaran, A.; Halman, J. Conducting and Publishing Design Science Research: Inaugural Essay of the Design Science Department of the Journal of Operations Management. J. Oper. Manag. 2016, 47–48, 1–8. [Google Scholar] [CrossRef]

| Part | Profession | Male/ Female | Age in Years | Education | Years of Working Experience | Focus Group |
|---|---|---|---|---|---|---|
| 1 | Communication specialist/content maker/expert by experience 1 | Male | 31 | Central Institute for Training Sports Leaders | 5–9 | 1 |
| 2 | Mental health nurse (flexible assertive community treatment) | Male | 27 | Bachelor of Nursing | 0–4 | 1 |
| 3 | Education and research consultant | Female | 48 | Bachelor of Nursing, Master of Educational Sciences | 0–4 | 1 |
| 4 | Lecturer in nursing research and mental health nurse | Female | 53 | Ph.D. student, Bachelor of Nursing, Master of Social Work, Master of Health Care | 10–14 | 1 |
| 5 | Oral health hygienist | Female | 25 | Bachelor of Oral Health Hygiene, Master of Health Innovation | 0–4 | 1 |
| 6 * | Master’s-level advanced nurse practitioner | Female | 47 | Ph.D., Master of Advanced Nursing Practice | >24 | 2 |
| 7 | Team leader of Academy of Health and Out of the Box Thinking | Female | 52 | Bachelor of Movement Sciences | 5–9 | 2 |
| 8 * | Mental health nurse (outpatients) | Female | 50 | Bachelor of Nursing | >24 | 2 |
| 9 | Expert by experience | Female | 32 | Student, Bachelor of Social Work | 0–4 | 2 |
| 10 * | Expert by experience 2 | Male | 48 | Associate degree for Expert by Experience | 5–9 | N/A |
| Tool | Prototype | Mean | Focus Group |
|---|---|---|---|
| 4 | Brochure for MHNs and patients: Importance of Oral Care Risk Factors Oral Complaints Physical/Psychological Symptoms Shame/Anxiety Medication Side Effects Dental Consequences Nutrition | 4.0 | 1 and 2 |
| 8 | Clinical Education Session involving the presentation of experiential narratives to students by experiential experts (successful stories). | 3.9 | 1 and 2 |
| 15 | A website where you can access all information easily and conveniently through a QR code. | 3.9 | 1 |
| 5 | Awareness screener as an insert in the brochure (prototype 4) for future reference: Assessing your satisfaction (or dissatisfaction) with your oral health, identifying desired changes, and determining the necessary steps. | 3.7 | 2 |
| 11 | Pocket Card: This Is How You Brush Your Teeth. A compact card illustrating oral care practices. | 3.6 | 1 |
| 13 | Assessment of the Impact of Oral Health Care on Quality of Life (OHIP 14): A brief, validated questionnaire comprising 14 questions regarding perceived oral health over a one-month period. | 3.6 | 1 |
| 14 | Oral health screening:(validated for non-dental professionals in Dutch). | 3.5 | 1 |
| 7 | Instructional Video for Patients and MHNs on How to Brush and Floss Teeth. | 3.5 | 1 and 2 |
| 1 | Video: Nursing Professional and Expert by Experience: A Discussion of Personal Narratives Concerning Oral Health Care. This encompasses an exploration of first-hand experiences relating to oral health care. Queries addressed include the nature of these experiences, the methodologies employed for managing them, the status of the involved individuals’ oral health, and the outcomes or benefits that have been realised. | 3.4 | 1 and 2 |
| 3 | Mirror-Based Dental Care Reminder Sticker. | 3.4 | 1 and 2 |
| 9 | Daily Schedule for Patients: In this daily schedule, patients and nursing staff collaboratively document activities such as waking up, breakfast, medication, and toothbrushing. | 3.4 | 1 and 2 |
| 2 | A toiletry bag or box (M/F) containing the following items: Toothbrush Toothpaste (containing fluoride) Dental floss picks Mouthwash Plaque-disclosing tablets (a literature-supported pill that highlights dental plaque) | 3.3 | 1 and 2 |
| 12 | Poster for Waiting Room/Office Living Room/Hallway/Drop-in Centre for Homeless Individuals. | 3.3 | 1 and 2 |
| 10 | Pocket Card: Do not Forget Your Oral Health. This card facilitates discussion about current oral care practices (self-care, dental visits, dental condition). | 3.2 | 1 |
| 6 | Toren C Instructional Video on Toothbrushing that is light-hearted, positive, and very humourous. | 2.9 | 2 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kuipers, S.; Castelein, S.; Kronenberg, L.; Veer, J.v.’.; Boonstra, N. The Development of an Oral Health Nursing Tool for Patients with a Psychotic Disorder: A Human-Centred Design with a Feasibility Test. Int. J. Environ. Res. Public Health 2024, 21, 492. https://doi.org/10.3390/ijerph21040492
Kuipers S, Castelein S, Kronenberg L, Veer Jv’, Boonstra N. The Development of an Oral Health Nursing Tool for Patients with a Psychotic Disorder: A Human-Centred Design with a Feasibility Test. International Journal of Environmental Research and Public Health. 2024; 21(4):492. https://doi.org/10.3390/ijerph21040492
Chicago/Turabian StyleKuipers, Sonja, Stynke Castelein, Linda Kronenberg, Job van ’t Veer, and Nynke Boonstra. 2024. "The Development of an Oral Health Nursing Tool for Patients with a Psychotic Disorder: A Human-Centred Design with a Feasibility Test" International Journal of Environmental Research and Public Health 21, no. 4: 492. https://doi.org/10.3390/ijerph21040492





