Association between the Quantity of Nurse–Doctor Interprofessional Collaboration and in-Patient Mortality: A Systematic Review
Abstract
1. Background
2. Methods
2.1. Eligibility Criteria
2.2. Information Sources
2.3. Search Strategy
2.4. Selection Process
2.5. Multiple Papers from a Single Study
2.6. Checking for Retraction
2.7. Data Collection Process
2.8. Data Items
2.9. Study Risk of Bias Assessment
2.10. Protocol Amendment
3. Results
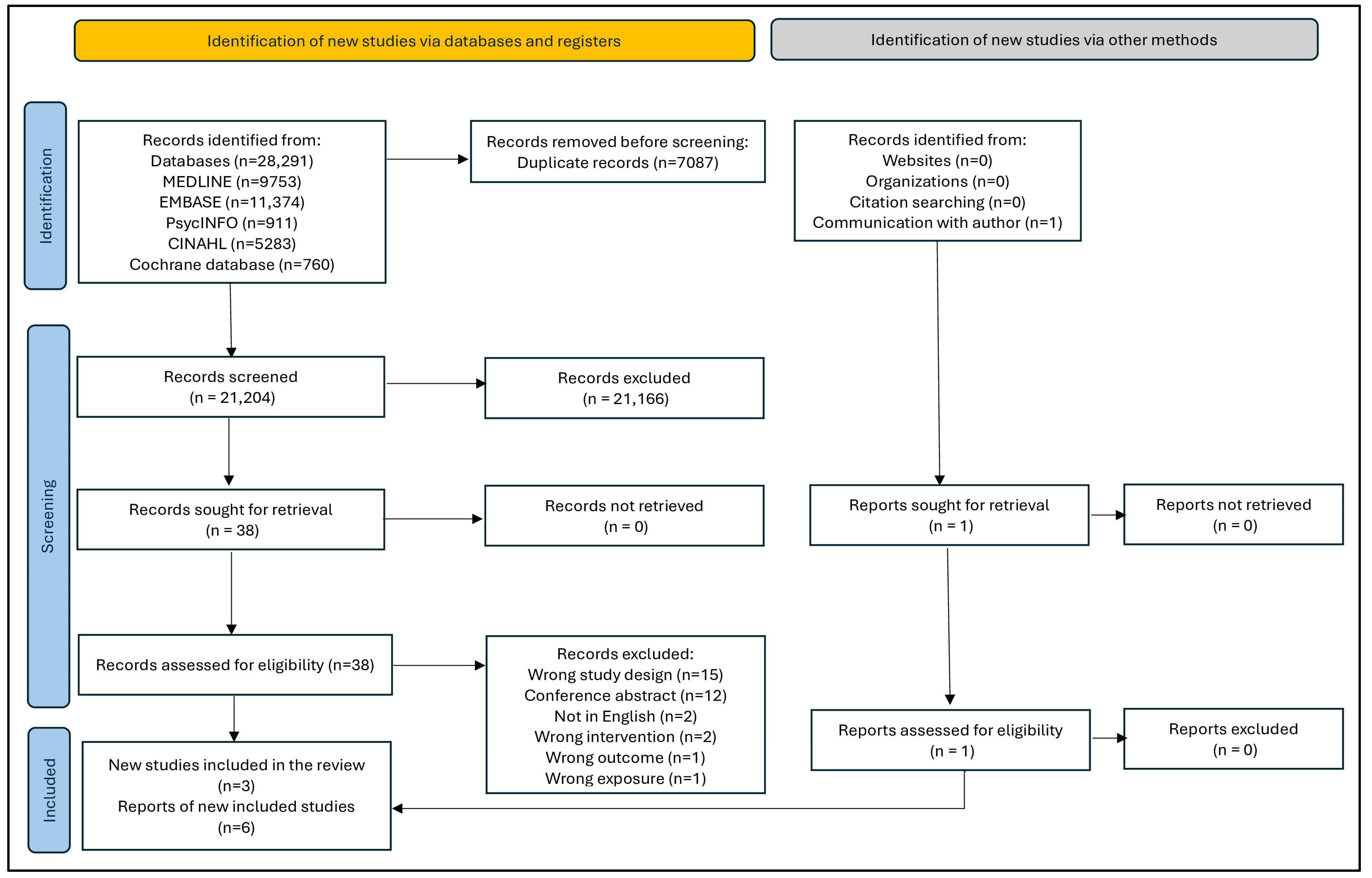
3.1. Study Selection
3.2. Study Characteristics
3.3. Clinical Settings
3.4. Study Participants
3.5. Definition of Mortality in the Included Studies
3.6. Description of the Measures of the Quantity of Nurse–Doctor Collaboration
3.7. Decision about Transfer (DAT)
3.8. Collaboration and Satisfaction about Care Decisions (CSACD)
3.9. Practice Environment Scale of the Nurse Work Index (PES-NWI)
3.10. Quality Appraisal
3.11. Results of Individual Studies
3.12. Meta-Analysis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bridges, D.; Davidson, R.A.; Soule Odegard, P.; Maki, I.V.; Tomkowiak, J. Interprofessional collaboration: Three best practice models of interprofessional education. Med. Educ. Online 2011, 16, 1–10. [Google Scholar] [CrossRef]
- Lockhart-Wood, K. Collaboration between nurses and doctors in clinical practice. Br. J. Nurs. 2000, 9, 276–280. [Google Scholar] [CrossRef]
- Henry, A.D.; Laszlo, A.; Nicholson, J. What does it take to build an employment collaborative for people with disabilities? J. Vocat. Rehabil. 2015, 43, 1–15. [Google Scholar] [CrossRef]
- Tan, T.C.; Zhou, H.; Kelly, M. Nurse-physician communication—An integrated review. J. Clin. Nurs. 2017, 26, 3974–3989. [Google Scholar] [CrossRef]
- Nester, J. The importance of interprofessional practice and education in the era of accountable care. North Carol. Med. J. 2016, 77, 128–132. [Google Scholar] [CrossRef] [PubMed]
- Collette, A.E.; Wann, K.; Nevin, M.L.; Rique, K.; Tarrant, G.; Hickey, L.A.; Stichler, J.F.; Toole, B.M.; Thomason, T. An exploration of nurse-physician perceptions of collaborative behaviour. J. Interprof. Care 2017, 31, 470–478. [Google Scholar] [CrossRef]
- Kaiser, L.; Bartz, S.; Neugebauer, E.A.M.; Pietsch, B.; Pieper, D. Interprofessional collaboration and patient-reported outcomes in inpatient care: Protocol for a systematic review. Syst. Rev. 2018, 7, 126. [Google Scholar] [CrossRef]
- Specchia, M.L.; Frisicale, E.M.; Carini, E.; Di Pilla, A.; Cappa, D.; Barbara, A.; Ricciardi, W.; Damiani, G. The impact of tumor board on cancer care: Evidence from an umbrella review. BMC Health Serv. Res. 2020, 20, 73. [Google Scholar] [CrossRef] [PubMed]
- Pannick, S.; Davis, R.; Ashrafian, H.; Byrne, B.E.; Beveridge, I.; Athanasiou, T.; Wachter, R.M.; Sevdalis, N. Effects of Interdisciplinary Team Care Interventions on General Medical Wards: A Systematic Review. JAMA Intern. Med. 2015, 175, 1288–1298. [Google Scholar] [CrossRef]
- Zwarenstein, M.; Goldman, J.; Reeves, S. Interprofessional collaboration: Effects of practice-based interventions on professional practice and healthcare outcomes. Cochrane Database Syst. Rev. 2009, 3, CD000072. [Google Scholar] [CrossRef]
- Martin, J.S.; Ummenhofer, W.; Manser, T.; Spirig, R. Interprofessional collaboration among nurses and physicians: Making a difference in patient outcome. Swiss Med. Wkly. 2010, 140, w13062. [Google Scholar] [CrossRef]
- Reeves, S.; Pelone, F.; Harrison, R.; Goldman, J.; Zwarenstein, M. Interprofessional collaboration to improve professional practice and healthcare outcomes. Cochrane Database Syst. Rev. 2017, 6, CD000072. [Google Scholar] [CrossRef] [PubMed]
- Ma, C.; McHugh, M.D.; Aiken, L.H. Organization of hospital nursing and 30-day readmissions in Medicare patients undergoing surgery. Med. Care 2015, 53, 65. [Google Scholar] [CrossRef] [PubMed]
- Ma, C.; Park, S.H.; Shang, J. Inter- and intra-disciplinary collaboration and patient safety outcomes in U.S. acute care hospital units: A cross-sectional study. Int. J. Nurs. Stud. 2018, 85, 1–6. [Google Scholar] [CrossRef]
- Pantha, S.; Jones, M.; Gray, R. Inter-Professional Collaboration and Patient Mortality: Protocol for a Systematic Review and Meta-Analysis. Nurs. Rep. 2020, 10, 15–22. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, 105906. [Google Scholar] [CrossRef]
- Babineau, J. Product review: Covidence (systematic review software). J. Can. Health Libr. Assoc. 2014, 35, 68–71. [Google Scholar] [CrossRef]
- Li, T.; Higgins, J.P.; Deeks, J.J. Chapter 5: Collecting data. In Cochrane Handbook for Systematic Reviews of Interventions Version 6.0; Higgins, J.P.T., Thomas, J., Chandler, J., Cumpston, M., Li, T., Page, M.J., Welch, V., Eds.; Cochrane: Hoboken, NJ, USA, 2019. [Google Scholar]
- Thomas, B.H.; Ciliska, D.; Dobbins, M.; Micucci, S. A Process for Systematically Reviewing the Literature: Providing the Research Evidence for Public Health Nursing Interventions. Worldviews Evid.-Based Nurs. 2004, 1, 176–184. [Google Scholar] [CrossRef] [PubMed]
- Armijo-Olivo, S.; Stiles, C.R.; Hagen, N.A.; Biondo, P.D.; Cummings, G.G. Assessment of study quality for systematic reviews: A comparison of the Cochrane Collaboration Risk of Bias Tool and the Effective Public Health Practice Project Quality Assessment Tool: Methodological research. J. Eval. Clin. Pract. 2012, 18, 12–18. [Google Scholar] [CrossRef] [PubMed]
- Baggs, J.G. Nuse-Physician Collaboration in the Intensive Care Unit. Ph.D. Dissertation, University of Rochester, Rochester, NY, USA, 1990. [Google Scholar]
- Baggs, J.G.; Ryan, S.A.; Phelps, C.E.; Richeson, J.F.; Johnson, J.E. The association between interdisciplinary collaboration and patient outcomes in a medical intensive care unit. Heart Lung J. Crit. Care 1992, 21, 18–24. [Google Scholar]
- Baggs, J.G.; Schmitt, M.H.; Mushlin, A.I.; Mitchell, P.H.; Eldredge, D.H.; Oakes, D.; Hutson, A.D. Association between nurse-physician collaboration and patient outcomes in three intensive care units. Crit. Care Med. 1999, 27, 1991–1998. [Google Scholar] [CrossRef] [PubMed]
- Kang, X.L. Association of Nurse-Physician Teamwork and Hospital Surgical Patient Mortality. Ph.D. Dissertation, University of Pennsylvania, Philadelphia, PA, USA, 2016. [Google Scholar]
- Kang, X.L.; Brom, H.M.; Lasater, K.B.; McHugh, M.D. The association of nurse–physician teamwork and mortality in surgical patients. West. J. Nurs. Res. 2020, 42, 245–253. [Google Scholar] [CrossRef] [PubMed]
- Baggs, J.G.; Schmitt, M.H.; Mushlin, A.I.; Eldredge, D.H.; Oakes, D.; Hutson, A.D. Nurse-physician collaboration and satisfaction with the decision-making process in three critical care units. Am. J. Crit. Care 1997, 6, 393–399. [Google Scholar] [CrossRef] [PubMed]
- Baggs, J.G. Development of an instrument to measure collaboration and satisfaction about care decisions. J. Adv. Nurs. 1994, 20, 176–182. [Google Scholar] [PubMed]
- Lake, E.T. Development of the practice environment scale of the nursing work index. Res. Nurs. Health 2002, 25, 176–188. [Google Scholar] [CrossRef] [PubMed]
- Neves, T.M.A.; Parreira, P.M.S.D.; Graveto, J.M.G.N.; Rodrigues, V.J.L.; Marôco Domingos, J.P. Practice environment scale of the nursing work index: Portuguese version and psychometric properties. J. Nurs. Manag. 2018, 26, 833–841. [Google Scholar] [CrossRef]
- Hanrahan, N.P. Measuring inpatient psychiatric environments: Psychometric properties of the Practice Environment Scale-Nursing Work Index (PES-NWI). Int. J. Psychiatr. Nurs. Res. 2007, 12, 1521–1528. [Google Scholar] [PubMed]
- Lucas, P.; Jesus, E.; Almeida, S.; Araújo, B. Validation of the Psychometric Properties of the Practice Environment Scale of Nursing Work Index in Primary Health Care in Portugal. Int. J. Environ. Res. Public Health 2021, 18, 6422. [Google Scholar] [CrossRef]
- Peltonen, J.; Leino-Kilpi, H.; Heikkilä, H.; Rautava, P.; Tuomela, K.; Siekkinen, M.; Sulosaari, V.; Stolt, M. Instruments measuring interprofessional collaboration in healthcare–a scoping review. J. Interprof. Care 2020, 34, 147–161. [Google Scholar] [CrossRef]
- Dougherty, M.B.; Larson, E. A Review of Instruments Measuring Nurse-Physician Collaboration. J. Nurs. Adm. (JONA) 2005, 35, 244–253. [Google Scholar] [CrossRef]
- Nuño-Solinís, R.; Zabalegui, I.B.; Arce, R.S.; Rodríguez, L.S.M.; Polanco, N.T. Development of a questionnaire to assess interprofessional collaboration between two different care levels. Int. J. Integr. Care 2013, 13, e015. [Google Scholar] [CrossRef]
- Ødegård, A. Exploring perceptions of interprofessional collaboration in child mental health care. Int. J. Integr. Care 2006, 6, e25. [Google Scholar] [CrossRef]
- Matziou, V.; Vlahioti, E.; Perdikaris, P.; Matziou, T.; Megapanou, E.; Petsios, K. Physician and nursing perceptions concerning interprofessional communication and collaboration. J. Interprof. Care 2014, 28, 526–533. [Google Scholar] [CrossRef] [PubMed]
- Rochefort, M.M.; Tomlinson, J.S. Unexpected readmissions after major cancer surgery: An evaluation of readmissions as a quality-of-care indicator. Surg. Oncol. Clin. 2012, 21, 397–405. [Google Scholar] [CrossRef]
- Yermilov, I.; Bentrem, D.; Sekeris, E.; Jain, S.; Maggard, M.A.; Ko, C.Y.; Tomlinson, J.S. Readmissions Following Pancreaticoduodenectomy for Pancreas Cancer: A Population-Based Appraisal. Ann. Surg. Oncol. 2009, 16, 554–561. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.A. Cochrane Handbook for Systematic Reviews of Interventions; John Wiley & Sons: Hoboken, NJ, USA, 2019. [Google Scholar] [CrossRef]
- Gray, R. Why do all systematic reviews have fifteen studies? Nurse Author Ed. 2020, 30, 27–29. [Google Scholar] [CrossRef]
- Yaffe, J.; Montgomery, P.; Hopewell, S.; Shepard, L.D. Empty Reviews: A Description and Consideration of Cochrane Systematic Reviews with No Included Studies. PLoS ONE 2012, 7, e36626. [Google Scholar] [CrossRef] [PubMed]
- Gray, R. Empty systematic reviews: Identifying gaps in knowledge or a waste of time and effort? Nurse Author Ed. 2021, 31, 42–44. [Google Scholar] [CrossRef]
- Shahian, D.M.; Wolf, R.E.; Iezzoni, L.I.; Kirle, L.; Normand, S.-L.T. Variability in the measurement of hospital-wide mortality rates. N. Engl. J. Med. 2010, 363, 2530–2539. [Google Scholar] [CrossRef]
- Walters, D.M.; McMurry, T.L.; Isbell, J.M.; Stukenborg, G.J.; Kozower, B.D. Understanding Mortality as a Quality Indicator After Esophagectomy. Ann. Thorac. Surg. 2014, 98, 506–512. [Google Scholar] [CrossRef]
- Hassani, S.; Lindman, A.S.; Kristoffersen, D.T.; Tomic, O.; Helgeland, J. 30-Day survival probabilities as a quality indicator for Norwegian hospitals: Data management and analysis. PLoS ONE 2015, 10, e0136547. [Google Scholar] [CrossRef] [PubMed]
- Fischer, C.; Lingsma, H.F.; Marang-van de Mheen, P.J.; Kringos, D.S.; Klazinga, N.S.; Steyerberg, E.W. Is the readmission rate a valid quality indicator? A review of the evidence. PLoS ONE 2014, 9, e112282. [Google Scholar] [CrossRef] [PubMed]
- Adams, R.J.; Smart, P.; Huff, A.S. Shades of grey: Guidelines for working with the grey literature in systematic reviews for management and organizational studies. Int. J. Manag. Rev. 2017, 19, 432–454. [Google Scholar] [CrossRef]
- Bosso, C.E.; Caetano, R.D.; Cardoso, A.P.; Souza, O.A.; Pena, R.; Mescolotte, M.M.; Souza, I.A.; Mescolotte, G.M. Impact of multidisciplinary healthcare team in mortality and readmission rate in a brazilian cardiac intensive care unit. In Proceedings of the 37th International Symposium on Intensive Care and Emergency Medicine, Brussels, Belgium, 21–24 March 2017. [Google Scholar]
- Cogan, L.; Romero-Ortuno, R. Acute Hospital admissions from a nursing home facility—A 3 year study. Ir. J. Med. Sci. 2013, 182, S242–S243. [Google Scholar]
| Citation | Additional Citation | Study Site | Study Type | Study Participants | Measure of the Quantity of Interprofessional Collaboration (Score Range) | Perceived Quantity of Nurse –Doctor Collaboration Mean (SD) | Outcome |
|---|---|---|---|---|---|---|---|
| Baggs (1990) 1 [21] | Baggs et al. (1992) [22] | 17-bed medical ICU | prospective, observational | Patient (n = 286) Nurse (n = 56) Doctor (n = 31) | Decision About Transfer (1–7) | Nurse: 4.1 (2.2) Doctor: 4.4 (2.0) | Nurses’ reported collaboration not associated with mortality of patients (B = −0.25, t = −1.83, p = 0.068). A significant association between nurses’ reported collaboration and negative patient outcomes (B = −0.22, t = −2.34, p = 0.020). No association between doctors’ reported collaboration and negative patient outcomes. |
| Baggs et al. (1999) [23] | Baggs et al. 2 (1994) [26] | ICUs from three hospitals 16-bed medical ICU, 20-bed surgical ICU, 7-bed mixed ICU | prospective observational | Patient (n = 1432) Nurse (n = 162) Doctor (n = 160) [Resident doctor (n = 63), Attending doctor (n = 97)] | Collaboration and Satisfaction about Care Decisions (CSACD) scale (1–49) | Medical ICU 3 Nurse: 30.7 Doctor: 31.1 Surgical ICU 3 Nurse: 24.6 Resident: 27.8 Attending: 37.5 Mixed ICU 3 Nurse: 30.6 Doctor: 31.9 | The association between collaboration and patient mortality was not reported in the manuscript. A significant association between nurses’ reported collaboration and negative patient outcomes (p = 0.037) in MICU. No association between nurses’ reported collaboration and negative patient outcomes in surgical and mixed ICUs. No statistically significant association between doctors’ reported collaboration and negative patient outcomes in any of the three ICUs. |
| Kang (2016) 1 [24] | Kang et al. (2020) [25] | Adult acute care hospitals (n = 665) | secondary data analysis | Patient (n = 1,321,904) Nurse (n = 29,391) | Nurse–physician relations subscale (1–4) in the Practice Environment Scale of the Nurse Work Index | Nurse: 2.90 (0.22) | A significant association between collaboration and patient outcomes [OR = 0.98, 95% CI = 0.96, 0.999, p < 0.001] even after controlling for patient and hospital characteristics, nurse teamwork, and education. |
| Scheme 1990 | Criteria | Baggs (1990) [21] | Baggs et al. (1999) [23] | Kang (2016) [24] |
|---|---|---|---|---|
| A | Selection bias | Strong | Moderate | Moderate |
| B | Study design | Weak | Weak | Weak |
| C | Confounders | Weak | Weak | Weak |
| D | Blinding | Weak | Weak | Weak |
| E | Data collection methods | Strong | Strong | Strong |
| F | Withdrawals and drop-outs | Not applicable | Not applicable | Not applicable |
| G | Intervention integrity | - | - | - |
| H | Analysis | - | - | - |
| Global Rating 1 Strong (no weak ratings) 2 Moderate (one weak rating) 3 Weak (two or more weak ratings) | Weak | Weak | Weak | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pantha, S.; Jones, M.; Moyo, N.; Pokhrel, B.; Kushemererwa, D.; Gray, R. Association between the Quantity of Nurse–Doctor Interprofessional Collaboration and in-Patient Mortality: A Systematic Review. Int. J. Environ. Res. Public Health 2024, 21, 494. https://doi.org/10.3390/ijerph21040494
Pantha S, Jones M, Moyo N, Pokhrel B, Kushemererwa D, Gray R. Association between the Quantity of Nurse–Doctor Interprofessional Collaboration and in-Patient Mortality: A Systematic Review. International Journal of Environmental Research and Public Health. 2024; 21(4):494. https://doi.org/10.3390/ijerph21040494
Chicago/Turabian StylePantha, Sandesh, Martin Jones, Nompilo Moyo, Bijaya Pokhrel, Diana Kushemererwa, and Richard Gray. 2024. "Association between the Quantity of Nurse–Doctor Interprofessional Collaboration and in-Patient Mortality: A Systematic Review" International Journal of Environmental Research and Public Health 21, no. 4: 494. https://doi.org/10.3390/ijerph21040494
APA StylePantha, S., Jones, M., Moyo, N., Pokhrel, B., Kushemererwa, D., & Gray, R. (2024). Association between the Quantity of Nurse–Doctor Interprofessional Collaboration and in-Patient Mortality: A Systematic Review. International Journal of Environmental Research and Public Health, 21(4), 494. https://doi.org/10.3390/ijerph21040494








