Relationship between Environmental Conditions and Utilisation of Community-Based Mental Health Care: A Comparative Study before and during the COVID-19 Pandemic in Italy
Abstract
:1. Introduction
2. Materials and Methods
2.1. Data Collection
2.2. Model Estimating Air Pollutant Concentrations
2.3. Construction of the Epidemiological Models
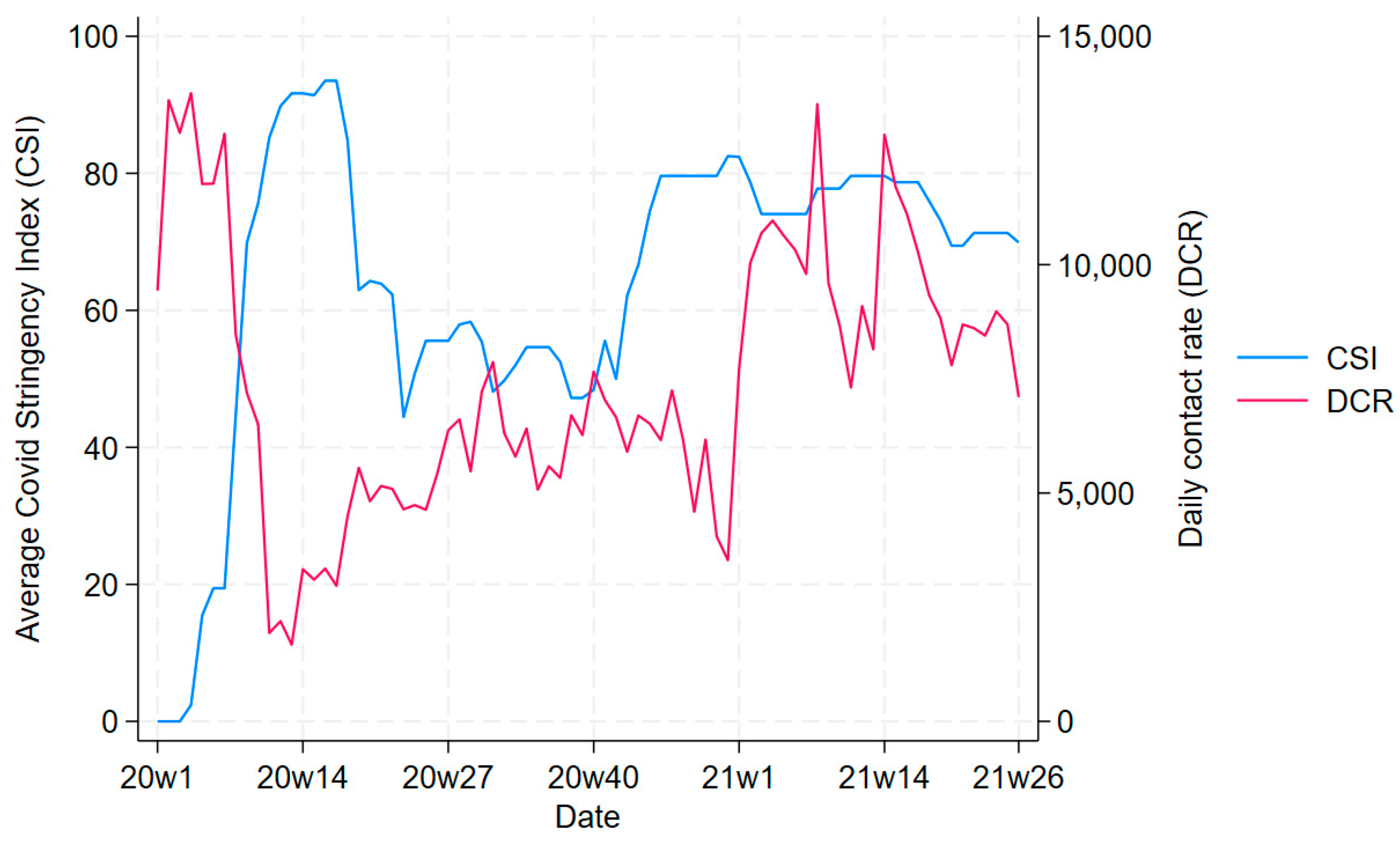
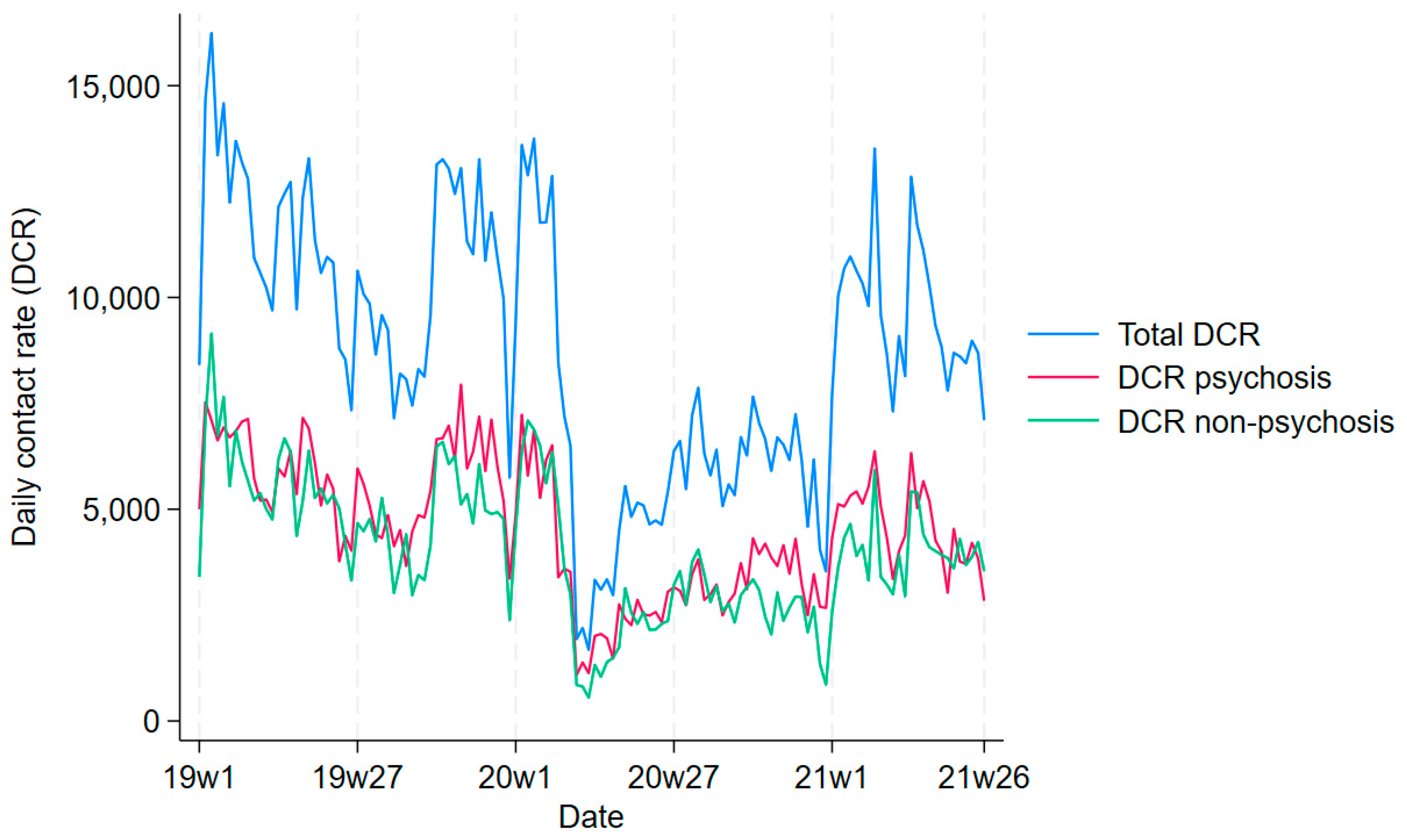
3. Results
4. Discussion
Limitations and Strengths
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Tsai, W.-L.; McHale, M.R.; Jennings, V.; Marquet, O.; Hipp, J.A.; Leung, Y.-F.; Floyd, M.F. Relationships between Characteristics of Urban Green Land Cover and Mental Health in U.S. Metropolitan Areas. Int. J. Environ. Res. Public Health 2018, 15, 340. [Google Scholar] [CrossRef] [PubMed]
- Hernandez, D.C.; Daundasekara, S.S.; Zvolensky, M.J.; Reitzel, L.R.; Maria, D.S.; Alexander, A.C.; Kendzor, D.E.; Businelle, M.S. Urban Stress Indirectly Influences Psychological Symptoms through Its Association with Distress Tolerance and Perceived Social Support among Adults Experiencing Homelessness. Int. J. Environ. Res. Public Health 2020, 17, 5301. [Google Scholar] [CrossRef] [PubMed]
- Norton, B.A.; Mears, M.; Warren, P.H.; Siriwardena, G.M.; Plummer, K.E.; Turner, T.; Hancock, S.; Grafius, D.R.; Evans, K.L. Biodiversity and environmental stressors along urban walking routes. Urban For. Urban Green. 2023, 85, 127951. [Google Scholar] [CrossRef]
- Pelgrims, I.; Devleesschauwer, B.; Guyot, M.; Keune, H.; Nawrot, T.S.; Remmen, R.; Saenen, N.D.; Trabelsi, S.; Thomas, I.; Aerts, R.; et al. Association between urban environment and mental health in Brussels, Belgium. BMC Public Health 2021, 21, 635. [Google Scholar] [CrossRef] [PubMed]
- Liu, L.; Xue, P.; Li, S.X.; Zhang, J.; Zhou, J.; Zhang, W. Urban-rural disparities in mental health problems related to COVID-19 in China. Gen. Hosp. Psychiatry 2021, 69, 119–120. [Google Scholar] [CrossRef] [PubMed]
- Hubbard, G.; Daas, C.D.; Johnston, M.; Murchie, P.; Thompson, C.W.; Dixon, D. Are Rurality, Area Deprivation, Access to Outside Space, and Green Space Associated with Mental Health during the COVID-19 Pandemic? A Cross Sectional Study (CHARIS-E). Int. J. Environ. Res. Public Health 2021, 18, 3869. [Google Scholar] [CrossRef] [PubMed]
- Menculini, G.; Bernardini, F.; Attademo, L.; Balducci, P.M.; Sciarma, T.; Moretti, P.; Tortorella, A. The Influence of the Urban Environment on Mental Health during the COVID-19 Pandemic: Focus on Air Pollution and Migration—A Narrative Review. Int. J. Environ. Res. Public Health 2021, 18, 3920. [Google Scholar] [CrossRef] [PubMed]
- Qiu, M.; Zhang, J. Exploring the perceived restorativeness of natural soundscapes under the global pandemic of COVID-19: A moderated mediation model. PLoS ONE 2021, 16, e0256855. [Google Scholar] [CrossRef] [PubMed]
- Thompson, D.A.; Fry, R.; Watkins, A.; Mizen, A.; Akbari, A.; Garrett, J.; Geary, R.; Lovell, R.; Lyons, R.; Nieuwenhuijsen, M.; et al. Exposure to green-blue spaces and mental health: A retrospective e-cohort study in Wales. Lancet 2021, 398, S85. [Google Scholar] [CrossRef]
- Remme, R.P.; Frumkin, H.; Guerry, A.D.; King, A.C.; Mandle, L.; Sarabu, C.; Bratman, G.N.; Giles-Corti, B.; Hamel, P.; Han, B.; et al. An ecosystem service perspective on urban nature, physical activity, and health. Proc. Natl. Acad. Sci. USA 2021, 118, e2018472118. [Google Scholar] [CrossRef]
- Cuijpers, P.; Miguel, C.; Ciharova, M.; Kumar, M.; Brander, L.; Kumar, P.; Karyotaki, E. Impact of climate events, pollution, and green spaces on mental health: An umbrella review of meta-analyses. Psychol. Med. 2023, 53, 638–653. [Google Scholar] [CrossRef]
- McDuffie, E.; Martin, R.; Yin, H.; Brauer, M. Global Burden of Disease from Major Air Pollution Sources (GBD MAPS): A Global Approach. Res. Rep. Health Eff. Inst. 2021, 210, 1–45. [Google Scholar]
- Ioannidis, J.P.A. Air pollution as cause of mental disease: Appraisal of the evidence. PLoS Biol. 2019, 17, e3000370. [Google Scholar] [CrossRef] [PubMed]
- Fan, S.-J.; Heinrich, J.; Bloom, M.S.; Zhao, T.-Y.; Shi, T.-X.; Feng, W.-R.; Sun, Y.; Shen, J.-C.; Yang, Z.-C.; Yang, B.-Y.; et al. Ambient air pollution and depression: A systematic review with meta-analysis up to 2019. Sci. Total Environ. 2020, 701, 134721. [Google Scholar] [CrossRef]
- World Health Organization. WHO Global Air Quality Guidelines. Particular Matter (PM2.5 and PM10), Ozone, Nitrogen Dioxide, Sulfur Dioxide and Carbon Monoxide; World Health Organization: Geneva, Switzerland, 2021. [Google Scholar]
- Bruyneel, L.; Kestens, W.; Alberty, M.; Karakaya, G.; Van Woensel, R.; Horemans, C.; Trimpeneers, E.; Vanpoucke, C.; Fierens, F.; Nawrot, T.S.; et al. Short-Term exposure to ambient air pollution and onset of work incapacity related to mental health conditions. Environ. Int. 2022, 164, 107245. [Google Scholar] [CrossRef] [PubMed]
- Rautio, N.; Filatova, S.; Lehtiniemi, H.; Miettunen, J. Living environment and its relationship to depressive mood: A systematic review. Int. J. Soc. Psychiatry 2018, 64, 92–103. [Google Scholar] [CrossRef] [PubMed]
- Konijnendijk, C.C. Evidence-based guidelines for greener, healthier, more resilient neighbourhoods: Introducing the 3–30–300 rule. J. For. Res. 2023, 34, 821–830. [Google Scholar] [CrossRef]
- Kim, S.Y.; Bang, M.; Wee, J.H.; Min, C.; Yoo, D.M.; Han, S.-M.; Kim, S.; Choi, H.G. Short- and long-term exposure to air pollution and lack of sunlight are associated with an increased risk of depression: A nested case-control study using meteorological data and national sample cohort data. Sci. Total Environ. 2021, 757, 143960. [Google Scholar] [CrossRef]
- Bauer, M.; Glenn, T.; Achtyes, E.D.; Alda, M.; Agaoglu, E.; Altinbaş, K.; Andreassen, O.A.; Angelopoulos, E.; Ardau, R.; Vares, E.A.; et al. Variations in seasonal solar insolation are associated with a history of suicide attempts in bipolar I disorder. Int. J. Bipolar Disord. 2021, 9, 26. [Google Scholar] [CrossRef]
- Frangione, B.; Villamizar, L.A.R.; Lang, J.J.; Colman, I.; Lavigne, E.; Peters, C.; Anisman, H.; Villeneuve, P.J. Short-term changes in meteorological conditions and suicide: A systematic review and meta-analysis. Environ. Res. 2022, 207, 112230. [Google Scholar] [CrossRef]
- Liu, Q.; Wang, W.; Gu, X.; Deng, F.; Wang, X.; Lin, H.; Guo, X.; Wu, S. Association between particulate matter air pollution and risk of depression and suicide: A systematic review and meta-analysis. Environ. Sci. Pollut Res. 2021, 28, 9029–9049. [Google Scholar] [CrossRef] [PubMed]
- Donisi, V.; Tedeschi, F.; Percudani, M.; Fiorillo, A.; Confalonieri, L.; De Rosa, C.; Salazzari, D.; Tansella, M.; Thornicroft, G.; Amaddeo, F. Prediction of community mental health service utilization by individual and ecological level socio-economic factors. Psychiatry Res. 2013, 209, 691–698. [Google Scholar] [CrossRef] [PubMed]
- Chang-Quan, H.; Zheng-Rong, W.; Yong-Hong, L.; Yi-Zhou, X.; Qing-Xiu, L. Education and Risk for Late Life Depression: A Meta-Analysis of Published Literature. Int. J. Psychiatry Med. 2010, 40, 109–124. [Google Scholar] [CrossRef] [PubMed]
- Li, Z.; Page, A.; Martin, G.; Taylor, R. Attributable risk of psychiatric and socio-economic factors for suicide from individual-level, population-based studies: A systematic review. Soc. Sci. Med. 2011, 72, 608–616. [Google Scholar] [CrossRef] [PubMed]
- Geranios, K.; Kagabo, R.; Kim, J. Impact of COVID-19 and Socioeconomic Status on Delayed Care and Unemployment. Health Equity 2022, 6, 91–97. [Google Scholar] [CrossRef] [PubMed]
- Chen, P.J.; Pusica, Y.; Sohaei, D.; Prassas, I.; Diamandis, E.P. An overview of mental health during the COVID-19 pandemic. Diagnosis 2021, 8, 403–412. [Google Scholar] [CrossRef] [PubMed]
- Salari, N.; Hosseinian-Far, A.; Jalali, R.; Vaisi-Raygani, A.; Rasoulpoor, S.; Mohammadi, M.; Rasoulpoor, S.; Khaledi-Paveh, B. Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: A systematic review and meta-analysis. Glob. Health 2020, 16, 57. [Google Scholar] [CrossRef]
- Gémes, K.; Bergström, J.; Papola, D.; Barbui, C.; Lam, A.I.F.; Hall, B.J.; Seedat, S.; Morina, N.; Quero, S.; Campos, D.; et al. Symptoms of anxiety and depression during the COVID-19 pandemic in six European countries and Australia–Differences by prior mental disorders and migration status. J. Affect. Disord. 2022, 311, 214–223. [Google Scholar] [CrossRef] [PubMed]
- Witteveen, A.B.; Young, S.Y.; Cuijpers, P.; Ayuso-Mateos, J.L.; Barbui, C.; Bertolini, F.; Cabello, M.; Cadorin, C.; Downes, N.; Franzoi, D.; et al. COVID-19 and common mental health symptoms in the early phase of the pandemic: An umbrella review of the evidence. PLoS Med. 2023, 20, e1004206. [Google Scholar] [CrossRef]
- Tarsitani, L.; Pinucci, I.; Tedeschi, F.; Patane, M.; Papola, D.; Palantza, C.; Acarturk, C.; Bjorkenstam, E.; Bryant, R.; Burchert, S.; et al. Resilience of people with chronic medical conditions during the COVID-19 pandemic: A 1-year longitudinal prospective survey. BMC Psychiatry 2022, 22, 633. [Google Scholar] [CrossRef]
- Lasalvia, A.; Rigon, G.; Rugiu, C.; Negri, C.; Del Zotti, F.; Amaddeo, F.; Bonetto, C. The psychological impact of COVID-19 among primary care physicians in the province of Verona, Italy: A cross-sectional study during the first pandemic wave. Fam. Pr. 2022, 39, 65–73. [Google Scholar] [CrossRef] [PubMed]
- Datta, S.; Mukherjee, T. Impact of COVID-19 stress on the psychological health of sexual & gender minority individuals: A systematic review. Front. Glob. Women’s Health 2023, 4, 1132768. [Google Scholar]
- Lasalvia, A.; Bodini, L.; Amaddeo, F.; Porru, S.; Carta, A.; Poli, R.; Bonetto, C. The Sustained Psychological Impact of the COVID-19 Pandemic on Health Care Workers One Year after the Outbreak—A Repeated Cross-Sectional Survey in a Tertiary Hospital of North-East Italy. Int. J. Environ. Res. Public Health 2021, 18, 13374. [Google Scholar] [CrossRef] [PubMed]
- Wu, T.; Jia, X.; Shi, H.; Niu, J.; Yin, X.; Xie, J.; Wang, X. Prevalence of mental health problems during the COVID-19 pandemic: A systematic review and meta-analysis. J. Affect. Disord. 2021, 281, 91–98. [Google Scholar] [CrossRef] [PubMed]
- Bertolini, F.; Witteveen, A.B.; Young, S.; Cuijpers, P.; Ayuso-Mateos, J.L.; Barbui, C.; Cabello, M.; Cadorin, C.; Downes, N.; Franzoi, D.; et al. Risk of SARS-CoV-2 infection, severe COVID-19 illness and COVID-19 mortality in people with pre-existing mental disorders: An umbrella review. BMC Psychiatry 2023, 23, 181. [Google Scholar] [CrossRef]
- Diaz, A.; Baweja, R.; Bonatakis, J.K.; Baweja, R. Global health disparities in vulnerable populations of psychiatric patients during the COVID-19 pandemic. WJP 2021, 11, 94–108. [Google Scholar] [CrossRef] [PubMed]
- Vancampfort, D.; Correll, C.U.; Galling, B.; Probst, M.; De Hert, M.; Ward, P.B.; Rosenbaum, S.; Gaughran, F.; Lally, J.; Stubbs, B. Diabetes mellitus in people with schizophrenia, bipolar disorder and major depressive disorder: A systematic review and large scale meta-analysis. World Psychiatry 2016, 15, 166–174. [Google Scholar] [CrossRef] [PubMed]
- Salvi, V.; Aguglia, A.; Barone-Adesi, F.; Bianchi, D.; Donfrancesco, C.; Dragogna, F.; Palmieri, L.; Serafini, G.; Amore, M.; Mencacci, C. Cardiovascular risk in patients with severe mental illness in Italy. Eur. Psychiatry 2020, 63, e96. [Google Scholar] [CrossRef] [PubMed]
- Bodini, L.; Bonetto, C.; Maccagnani, A.; Bonora, A.; Polati, E.; Ricci, G.; Paolillo, C.; Amaddeo, F.; Lasalvia, A. Changes in emergency psychiatric consultations in time of COVID-19: A retrospective observational study in the Verona Academic Hospital over the two pandemic years 2020–2021. BMC Emerg. Med. 2023, 23, 18. [Google Scholar] [CrossRef]
- Prina, E.; Tedeschi, F.; Salazzari, D.; Botte, T.; Ballarin, M.; Rabbi, L.; Imperadore, G.; Roccato, S.; Nicolaou, S.; Ruggeri, M.; et al. Effect of COVID-19 pandemic on utilisation of community-based mental health care in North-East of Italy: A psychiatric case register study. Epidemiol. Psychiatr. Sci. 2023, 32, e17. [Google Scholar] [CrossRef]
- Meloni, S.; de Girolamo, G.; Rossi, R. COVID-19 e servizi di salute mentale in Europa. E&P 2020, 44 (Suppl. S2), 383–393. [Google Scholar]
- Carpiniello, B.; Tusconi, M.; Zanalda, E.; Di Sciascio, G.; Di Giannantonio, M. Psychiatry during the COVID-19 pandemic: A survey on mental health departments in Italy. BMC Psychiatry 2020, 20, 593. [Google Scholar] [CrossRef] [PubMed]
- Fiorillo, A.; Sampogna, G.; Giallonardo, V.; Del Vecchio, V.; Luciano, M.; Albert, U.; Carmassi, C.; Carrà, G.; Cirulli, F.; Dell’osso, B.; et al. Effects of the lockdown on the mental health of the general population during the COVID-19 pandemic in Italy: Results from the COMET collaborative network. Eur. Psychiatry 2020, 63, e87. [Google Scholar] [CrossRef]
- Gkatzelis, G.; Gilman, J.B.; Brown, S.S.; Eskes, H.; Gomes, A.R.; Lange, A.C.; McDonald, B.C.; Peischl, J.; Petzold, A.; Thompson, C.R.; et al. The global impacts of COVID-19 lockdowns on urban air pollution. Elem. Sci. Anthr. 2021, 9, 00176. [Google Scholar] [CrossRef]
- Kreutz, J.; Heitmann, J.; Schäfer, A.-C.; Aldudak, S.; Schieffer, B.; Schieffer, E. Environmental factors and their impact on the COVID-19 pandemic. Herz 2023, 48, 234–238. [Google Scholar] [CrossRef]
- World Medical Association Declaration of Helsinki: Ethical Principles for Medical Research Involving Human Subjects. JAMA 2013, 310, 2191. [CrossRef]
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. J. Clin. Epidemiol. 2008, 61, 344–349. [Google Scholar] [CrossRef] [PubMed]
- Katschning, H.; StraBmayr, C. Comparative Effectiveness Research on Psychiatric HOSpitalisation by Record LINKage of Large Administrative Data Sets in Six European Countries. Available online: https://cordis.europa.eu/project/id/603264 (accessed on 2 November 2023).
- Lo, S.B.; Huber, C.G.; Meyer, A.; Weinmann, S.; Luethi, R.; Dechent, F.; Borgwardt, S.; Lieb, R.; Lang, U.E.; Moeller, J. The relationship between psychological characteristics of patients and their utilization of psychiatric inpatient treatment: A cross-sectional study, using machine learning. PLoS ONE 2022, 17, e0266352. [Google Scholar] [CrossRef]
- Europian Union. Copernicus. Available online: https://www.copernicus.eu/en (accessed on 21 November 2023).
- Daya Sagar, B.S.; Cheng, Q.; Agterberg, F. (Eds.) Handbook of Mathematical Geosciences: Fifty Years of IAMG; Springer International Publishing: Cham, Germany, 2018; Available online: http://link.springer.com/10.1007/978-3-319-78999-6 (accessed on 18 October 2023).
- Bivand, R.S. Exploratory Spatial Data Analysis. In Handbook of Applied Spatial Analysis; Fischer, M., Getis, A., Eds.; Springer: Berlin/Heidelberg, Germany, 2010. [Google Scholar] [CrossRef]
- Wackernagel, H. Multivariate Geostatistics: An Introduction with Applications; Springer: Berlin/Heidelberg, Germany, 2003. [Google Scholar] [CrossRef]
- Hale, T.; Angrist, N.; Goldszmidt, R.; Kira, B.; Petherick, A.; Phillips, T.; Webster, S.; Cameron-Blake, E.; Hallas, L.; Majumdar, S.; et al. A global panel database of pandemic policies (Oxford COVID-19 Government Response Tracker). Nat. Hum. Behav. 2021, 5, 529–538. [Google Scholar] [CrossRef]
- Higgins, J.P.; Ramsay, C.; Reeves, B.C.; Deeks, J.J.; Shea, B.; Valentine, J.C.; Tugwell, P.; Wells, G. Issues relating to study design and risk of bias when including non-randomized studies in systematic reviews on the effects of interventions. Res. Synth. Methods. 2013, 4, 12–25. [Google Scholar] [CrossRef]
- StataCorp. Stata Statistical Software: Release 18; StataCorp LLC: College Station, TX, USA, 2023. [Google Scholar]
- Kleeman, A.; Foster, S. ‘It feels smaller now’: The impact of the COVID-19 lockdown on apartment residents and their living environment–A longitudinal study. J. Environ. Psychol. 2023, 89, 102056. [Google Scholar] [CrossRef] [PubMed]
- Grøsland, M.; Larsen, V.B.; Reneflot, A.; Hart, R.K. The COVID-19 pandemic’s impact on mental health care use among Norwegian students in higher education: A nation-wide register-based pre-post cohort study. BMC Health Serv. Res. 2022, 22, 1506. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Ke, X.; Min, M.; Zhang, Y.; Dai, Y.; Tang, L. Do We Need More Urban Green Space to Alleviate PM2.5 Pollution? A Case Study in Wuhan, China. Land 2022, 11, 776. [Google Scholar] [CrossRef]
- Britton, E.; Kindermann, G.; Domegan, C.; Carlin, C. Blue care: A systematic review of blue space interventions for health and wellbeing. Health Promot. Int. 2020, 35, 50–69. [Google Scholar] [CrossRef] [PubMed]
- Universitat Autònoma de Barceloma. Integrated System Analysis of Urban Vegetation and Agriculture (URBAG). 2023. Available online: https://urbag.eu/ (accessed on 2 November 2023).
- Amaddeo, F.; Beecham, J.; Bonizzato, P.; Fenyo, A.; Knapp, M.; Tansella, M. The use of a case register to evaluate the costs of psychiatric care. Acta Psychiatr. Scand. 1997, 95, 189–198. [Google Scholar] [CrossRef] [PubMed]
- Amaddeo, F.; Zambello, F.; Tansella, M.; Thornicroft, G. Accessibility and pathways to psychiatric care in a community-based mental health system. Soc. Psychiatry Psychiatr. Epidemiol. 2001, 36, 500–507. [Google Scholar] [CrossRef] [PubMed]
- Amaddeo, F.; Barbui, C.; Perini, G.; Biggeri, A.; Tansella, M. Avoidable mortality of psychiatric patients in an area with a community-based system of mental health care. Acta Psychiatr. Scand. 2007, 115, 320–325. [Google Scholar] [CrossRef]
- Copernicus. Urban Atlas Land Cover/Land Use 2018 (Vector), Europe, 6-Yearly. 2023. Available online: https://land.copernicus.eu/en/products/urban-atlas/urban-atlas-2018 (accessed on 2 November 2023).
- Copernicus. Tree Cover Density 2018 (Raster 10 m and 100 m), Europe, 3-Yearly. 2023. Available online: https://land.copernicus.eu/en/products/high-resolution-layer-tree-cover-density/tree-cover-density-2018 (accessed on 2 November 2023).
- Istat. Basi Territoriali e Variabili Censuarie. 2023. Available online: https://www.istat.it/it/archivio/104317 (accessed on 2 November 2023).
- Zulian, G.; Marando, F.; Mentaschi, L.; Alzetta, C.; Wilk, B.; Maes, J. Green balance in urban areas as an indicator for policy support: A multi-level application. One Ecosyst. 2022, 7, 1–39. [Google Scholar] [CrossRef]
| N | % | |
|---|---|---|
| All patients | 3923 | 100.00% |
| Gender | ||
| Female | 2225 | 56.72% |
| Male | 1698 | 43.28% |
| Age (n missing = 22) | ||
| 18–24 years | 312 | 8.00% |
| 25–44 years | 968 | 24.81% |
| 45–64 years | 1736 | 44.50% |
| ≥65 years | 885 | 22.69% |
| Citizenship (n missing = 22) | ||
| Italian | 3338 | 85.57% |
| Others | 563 | 14.43% |
| Marital status (n missing = 337) | ||
| Single | 1684 | 46.96% |
| Married | 1181 | 32.93% |
| Separated/divorced/widowed | 721 | 20.11% |
| Living situation (n missing = 406) | ||
| Alone | 715 | 20.35% |
| With family members | 2651 | 75.44% |
| Sheltered or residential facility | 148 | 4.21% |
| Diagnosis (n missing = 83) | ||
| Schizophrenia and related disorders | 660 | 16.82% |
| Affective disorders | 806 | 20.55% |
| Neurotic and somatoform disorders | 1420 | 36.20% |
| Personality disorders | 290 | 7.39% |
| Other diagnoses | 664 | 16.93% |
| Coefficient | SE | p-Value | 95% CI | |
|---|---|---|---|---|
| Percentage of working days | −0.746 | 1.662 | 0.654 | (−4.003; 2.511) |
| Lagged value of the daily contact rate | 0.089 | 0.0004 | <0.001 | (0.088; 0.089) |
| Solar radiation (KWs) | −0.170 | 0.103 | 0.097 | (−0.372; 0.031) |
| PM2.5 concentration | −0.003 | 0.013 | 0.824 | (−0.027; 0.022) |
| NO2 concentration | 0.081 | 0.016 | <0.001 | (0.049; 0.113) |
| Percentage of tree cover | −0.036 | 0.028 | 0.194 | (−0.090; 0.018) |
| Green areas > 2 hectares around the CB centroid | 0.138 | 0.497 | 0.780 | (−0.836; 1.113) |
| Watercourses around the CB centroid | −0.194 | 0.603 | 0.748 | (−1.375; 0.987) |
| Percentage of inhabitants with at most primary school education | 0.052 | 0.022 | 0.017 | (0.009; 0.095) |
| Percentage of inhabitants living in rented apartments (%) | 0.033 | 0.012 | 0.007 | (0.009; 0.056) |
| Unemployment rate (%) | 0.045 | 0.058 | 0.435 | (−0.069; 0.160) |
| Lagged value of solar radiation (KWs) | −0.164 | 0.101 | 0.103 | (−0.362; 0.033) |
| The proportion of days with PM2.5 above the threshold from the previous week | −0.458 | 0.317 | 0.148 | (−1.079; 0.162) |
| The proportion of days with NO2 above the threshold from the previous week | 0.307 | 0.995 | 0.758 | (−1.643; 2.258) |
| Coefficient | SE | p-Value | 95% CI | |
|---|---|---|---|---|
| Percentage of working days | 2.430 | 1.523 | 0.111 | (−0.556; 5.416) |
| Lagged value of the daily contact rate | 0.088 | 0.0004 | <0.001 | (0.088; 0.089) |
| Solar radiation (KWs) | −0.138 | 0.137 | 0.314 | (−0.405; 0.130) |
| PM2.5 concentration | −0.020 | 0.018 | 0.248 | (−0.055; 0.014) |
| NO2 concentration | 0.034 | 0.019 | 0.064 | (−0.002; 0.071) |
| Percentage of tree cover | −0.058 | 0.028 | 0.040 | (−0.113; −0.003) |
| Green areas > 2 hectares around the CB centroid | −0.155 | 0.506 | 0.759 | (−1.148; 0.837) |
| Watercourses around the CB centroid | −0.187 | 0.614 | 0.761 | (−1.391; 1.017) |
| Rate of inhabitants with at most primary school education | 0.076 | 0.022 | <0.001 | (0.032; 0.119) |
| Rate of inhabitants living in rented apartments | 0.046 | 0.012 | <0.001 | (0.022; 0.070) |
| Unemployment rate | 0.080 | 0.059 | 0.178 | (−0.036; 0.196) |
| Lagged value of solar radiation (KWs) | −0.424 | 0.139 | 0.002 | (−0.670; −0.151) |
| The proportion of days with PM2.5 above the threshold from the previous week | 0.175 | 0.496 | 0.724 | (−0.797; 1.148) |
| The proportion of days with NO2 above the threshold from the previous week | −0.700 | 1.047 | 0.504 | (−2.753; 1.353) |
| Pandemic period | −0.269 | 0.821 | 0.743 | (−1.879; 1.340) |
| Rate of inhabitants with at most primary school education * pandemic period | −0.044 | 0.008 | <0.001 | (−0.059; −0.029) |
| Rate of inhabitants living in rented apartments * pandemic period | −0.024 | 0.004 | <0.001 | (−0.032; −0.016) |
| Unemployment rate * pandemic period | −0.063 | 0.020 | 0.001 | (−0.102; −0.024) |
| Solar radiation (KWs) * pandemic period | −0.163 | 0.165 | 0.322 | (−0.487; 0.160) |
| PM2.5 concentration * pandemic period | 0.032 | 0.024 | 0.181 | (−0.015; 0.078) |
| NO2 concentration * pandemic period | −0.016 | 0.025 | 0.526 | (−0.064; 0.033) |
| Percentage of tree cover * pandemic period | 0.038 | 0.010 | <0.001 | (0.020; 0.057) |
| Green areas above 2 hectares around the CB centroid * pandemic period | 0.552 | 0.172 | 0.001 | (0.214; 0.890) |
| Lagged value of solar radiation (KWs) * pandemic period | 0.243 | 0.168 | 0.149 | (−0.087; 0.142) |
| Lagged value of the proportion of days with PM2.5 above the threshold from the previous week * pandemic period | −0.659 | 0.661 | 0.319 | (−1.955; 0.637) |
| Lagged value of the proportion of days with NO2 above the threshold from the previous week * pandemic period | 0.817 | 1.399 | 0.559 | (−1.925; 3.558) |
| Watercourses around the CB centroid * pandemic period | −0.018 | 0.216 | 0.932 | (−0.442;0.405) |
| Coefficient | SE | p-Value | 95% CI | |
|---|---|---|---|---|
| Percentage of working days | 1.749 | 1.624 | 0.282 | (−1.435; 4.932) |
| Lagged value of the daily contact rate | 0.089 | 0.0004 | <0.001 | (0.088; 0.089) |
| Rate of inhabitants with at most primary school education | 0.052 | 0.022 | 0.017 | (0.009; 0.095) |
| Rate of inhabitants living in rented apartments | 0.033 | 0.012 | 0.007 | (0.009; 0.056) |
| Unemployment rate | 0.046 | 0.058 | 0.427 | (−0.068; 0.161) |
| Holidays in weeks with a travel ban | 0.297 | 0.312 | 0.341 | (−0.314; 0.908) |
| Year 2020 | −1.111 | 0.133 | <0.001 | (−1.371; −0.851) |
| Year 2021 | −0.342 | 0.284 | 0.229 | (−0.900; 0.216) |
| Lockdown | −1.510 | 0.286 | <0.001 | (−2.070; −0.950) |
| Intermediate restrictions | −0.537 | 0.261 | 0.039 | (−1.048; −0.026) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Prina, E.; Tedeschi, F.; Lasalvia, A.; Salazzari, D.; Latini, S.; Rabbi, L.; Marando, F.; van Rijn, E.; Wollgast, J.; Pisoni, E.; et al. Relationship between Environmental Conditions and Utilisation of Community-Based Mental Health Care: A Comparative Study before and during the COVID-19 Pandemic in Italy. Int. J. Environ. Res. Public Health 2024, 21, 661. https://doi.org/10.3390/ijerph21060661
Prina E, Tedeschi F, Lasalvia A, Salazzari D, Latini S, Rabbi L, Marando F, van Rijn E, Wollgast J, Pisoni E, et al. Relationship between Environmental Conditions and Utilisation of Community-Based Mental Health Care: A Comparative Study before and during the COVID-19 Pandemic in Italy. International Journal of Environmental Research and Public Health. 2024; 21(6):661. https://doi.org/10.3390/ijerph21060661
Chicago/Turabian StylePrina, Eleonora, Federico Tedeschi, Antonio Lasalvia, Damiano Salazzari, Sara Latini, Laura Rabbi, Federica Marando, Elaine van Rijn, Jan Wollgast, Enrico Pisoni, and et al. 2024. "Relationship between Environmental Conditions and Utilisation of Community-Based Mental Health Care: A Comparative Study before and during the COVID-19 Pandemic in Italy" International Journal of Environmental Research and Public Health 21, no. 6: 661. https://doi.org/10.3390/ijerph21060661
APA StylePrina, E., Tedeschi, F., Lasalvia, A., Salazzari, D., Latini, S., Rabbi, L., Marando, F., van Rijn, E., Wollgast, J., Pisoni, E., Bessagnet, B., Beauchamp, M., & Amaddeo, F. (2024). Relationship between Environmental Conditions and Utilisation of Community-Based Mental Health Care: A Comparative Study before and during the COVID-19 Pandemic in Italy. International Journal of Environmental Research and Public Health, 21(6), 661. https://doi.org/10.3390/ijerph21060661







