Models of Governance of Disability Therapy Support Workers in Rural and Remote Settings: A Systematic Scoping Review
Abstract
1. Introduction
2. Review Questions
- What governance models for disability support/therapy workers in rural and remote settings exist and what are the key components of these models?
- What contexts and mechanisms are required to successfully apply governance models for disability therapy support workers (DTSW) in rural and remote settings?
3. Materials and Methods
3.1. Inclusion Criteria
3.1.1. Participants
- A direct patient care role and may have application to broader public health outcomes;
- A national professional organization with a code of ethics/conduct and clearly defined membership requirements;
- University health sciences courses (not medical, dental, or nursing) at Australian Qualifications Framework (AQF) Level 7 or higher, accredited by their relevant national accreditation body;
- Clearly articulated national entry level competency standards and assessment procedures;
- A defined core scope of practice;
- Robust and enforceable regulatory mechanisms;
- Are autonomous practitioners;
- Practice in an evidence-based paradigm, using an internationally recognized body of knowledge to protect, restore, and maintain optimal physical, sensory, psychological, cognitive, social, and cultural function;
- May utilize or supervise assistants, technicians, and support workers.
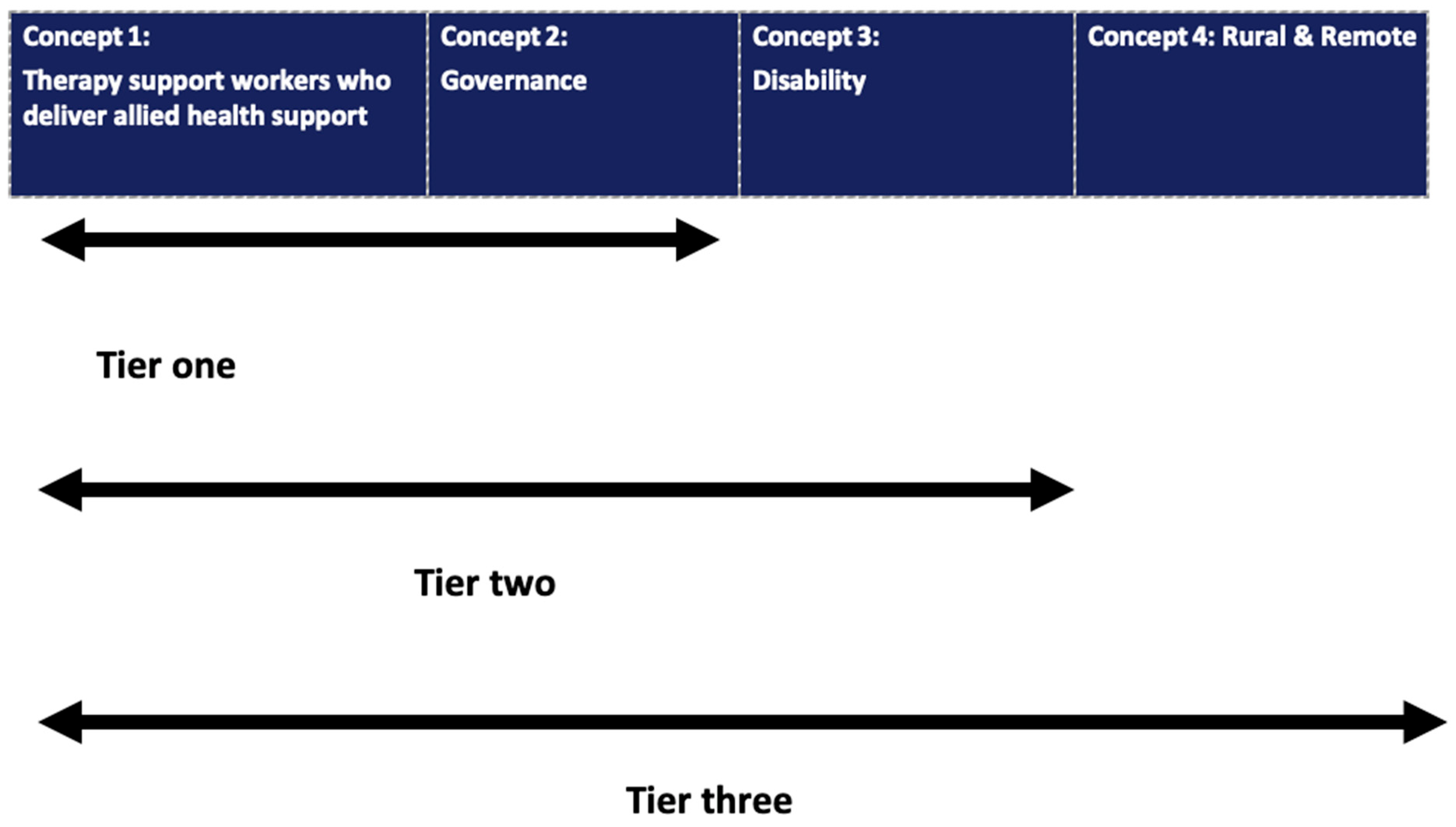
3.1.2. Concept
3.1.3. Context
3.1.4. People with Disability
3.2. Types of Sources
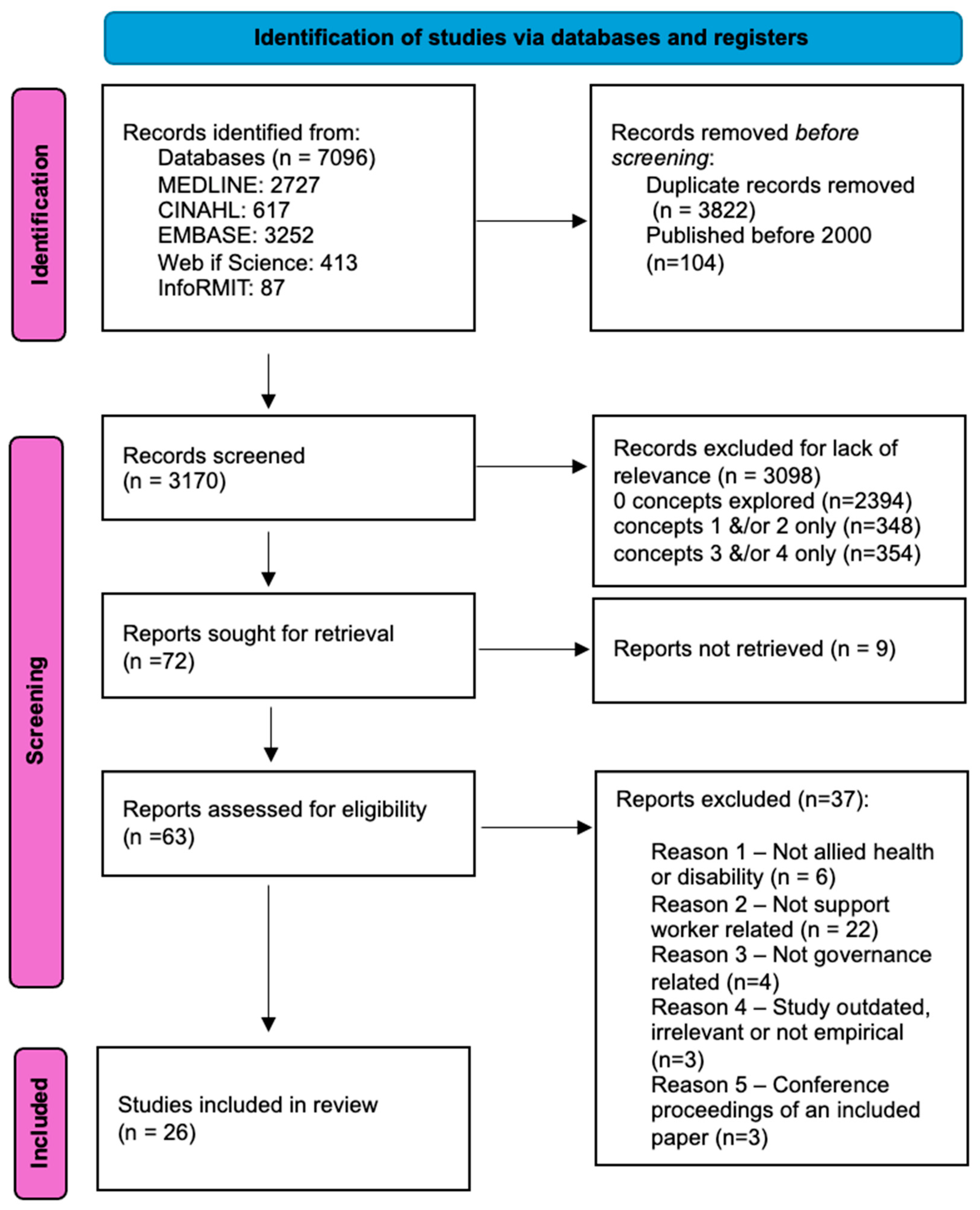
3.3. Method
3.3.1. Search Strategy
3.3.2. Information Sources
3.3.3. Study Selection
3.3.4. Data Extraction
3.3.5. Data Presentation
4. Results
4.1. What Are the Key Components of Governance Models/Interventions for Disability Therapy Support Workers in Rural and Remote Settings?
4.1.1. Capabilities
4.1.2. Competence
4.1.3. Supervision, Support, Assessment of Competency, Credentialling and Care Plans
4.2. What Contexts and Mechanisms Are Required to Successfully Apply Governance Models for Disability Support Workers in Rural and Remote Settings?
Contexts
4.3. Mechanisms
4.3.1. Capability Mechanisms
4.3.2. Successful Capability Is Facilitated by the following Mechanisms
4.3.3. Successful Governance Is Facilitated by Competency Mechanisms
4.3.4. Successful Supervision Is Facilitated by the following Mechanisms
4.3.5. Successful Formal Assessment of Competence and Credentialling Are Facilitated by the following Mechanisms
4.4. Success and Impact
4.5. Strength and Quality of the Evidence
5. Discussion
- Decision making skills;
- Building relationships with clients;
- Advocating for clients;
- Communication and interaction skills;
- Risk assessment and risk management skills;
- Building relationships with multiple stakeholders;
- Adapting to client needs/client-centred care;
- Counselling;
- Critical thinking/clinical judgement/clinical reasoning;
- Providing clients with emotional support;
- Negotiating role boundaries;
- Empowering clients;
- Providing personal and compassionate support.
- Consistent and sufficient staffing;
- Clear job and role descriptions for all staff;
- Whole of community approach/multisector coordination to delivery of care;
- Training and professional development is routinely provided, resourced and supported;
- Support worker knowledge and skills are valued;
- Staff are provided time, resources, and opportunity to look after their wellbeing;
- Sufficient time is made available to staff to develop relationships/negotiate role boundaries;
- Clear lines of communication and accountability;
- Culture of organization is relaxed/playful and supportive;
- Simplified funding models;
- Encouraging and supportive leadership style;
- Safety precautions incorporated into training protocols;
- Enablement culture;
- AHPs involved in developing training packages;
- Project resourcing;
- Clear accountability and liability around training assessment;
- Acknowledging complexity of the supervision/workplace context (rural).
Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Disability Reform Council. National Disability Insurance Scheme Integrated Market, Sector and Workforce Strategy; Australian Government: Canberra, Australia, 2005.
- National Disability Services. State of the Disability Sector Report; National Disability Services: Canberra, Australia, 2018. [Google Scholar]
- Mucic, A. Building a Workforce Using Allied Health Assistants. 2019. Available online: https://www.disabilityservicesconsulting.com.au/resources/building-workforce-allied-health-assistants (accessed on 30 March 2020).
- NSW Ministry of Health. Allied Health Assistant Framework. NSW Government. 2013. Available online: http://www1.health.nsw.gov.au/pds/ActivePDSDocuments/GL2013_005.pdf (accessed on 30 March 2020).
- Department of Health and Human Services. Supervision and Delegation Framework for Allied Health Assistants and the Support Workforce in Disability. 2018. Available online: https://www2.health.vic.gov.au/-/media/health/files/collections/policies-and-guidelines/a/allied-health-in-disability---supervision-and-delegation-framework.pdf?la=en&hash=17C8B0DA1306D5944508699B58349590B1BE4CCA (accessed on 30 March 2020).
- Main, R. Implementation of the National Disability Insurance Scheme and the Provision of Disability Services in New South Wales; Portfolio Committee No. 2; Health and Community Services: Sydney, Australia, 2018. [Google Scholar]
- World Health Organisation. International Classification of Functioning, Disability and Health; World Health Organisation: Geneva, Switzerland, 2001. [Google Scholar]
- Moran, A.; Enderby, P.; Nancarrow, S. Defining and identifying common elements of and contextual influences on the roles of support workers in health and social care: A thematic analysis of the literature. J. Eval. Clin. Pract. 2011, 17, 1191–1199. [Google Scholar] [CrossRef] [PubMed]
- Braithwaite, J.; Travaglia, J.F. An overview of clinical governance policies, practices and initiatives. Aust. Health Rev. 2008, 32, 10–22. [Google Scholar] [CrossRef] [PubMed]
- Pawson, R.; Tilley, N. Realistic Evaluation; Sage Publications Limited: New York, NY, USA, 1997. [Google Scholar]
- Baxter, S.; Killoran, A.; Kelly, M.; Goyder, E. Synthesizing diverse evidence: The use of primary qualitative data analysis methods and logic models in public health reviews. Public Health 2010, 124, 99–106. [Google Scholar] [CrossRef] [PubMed]
- Peters, M.; Godfrey, C.; McInerney, P.; Baldini, S.; Khalil, H.; Parker, D. Chapter 11: Scoping Reviews. In Joanna Briggs Institute Reviewer’s Manual; Aromataris, E., Munn, Z., Eds.; The Joanna Briggs Institute: Adelaide, Australia, 2017. [Google Scholar]
- Allied Health Professions Australia [AHPA]. What Is Allied Health? 2019. Available online: https://ahpa.com.au/what-is-allied-health/ (accessed on 30 March 2020).
- Sevices for Australian Rural and Remote Allied Health (SARRAH). A Framework for the Classification of the Health Professional Workforce; SARRAH: Canberra, Australia, 2007. [Google Scholar]
- Greater Northern Australia Regional Training Network. Project Report: Rural and Remote Generalist—Allied Health Project; Greater Northern Australia Regional Training Network: Cairns, Australia, 2013. [Google Scholar]
- Keane, S.; Smith, T.N.; Lincoln, M.; Wagner, S.R.; Lowe, S.E. The rural allied health workforce study (RAHWS): Background, rationale and questionnaire development. Rural Remote Health 2008, 8, 1132. [Google Scholar] [CrossRef]
- Nancarrow, S.A.; Roots, A.; Grace, S.; Moran, A.M.; Vanniekerk-Lyons, K. Implementing large-scale workforce change: Learning from 55 pilot sites of allied health workforce redesign in Queensland, Australia. Hum. Resour. Health 2013, 11, 66. [Google Scholar] [CrossRef] [PubMed]
- Services for Australian Rural and Remote Allied Health (SARRAH). The Allied Health Rural Generalist Pathway; SARRAH: Canberra, Australia, 2019; Available online: https://sarrah.org.au/ahrgp (accessed on 30 March 2020).
- Services for Australian Rural and Remote Allied Health (SARRAH). Position Statement: Allied Health Professions and Rural Generalism; SARRAH: Canberra, Australia, 2016. [Google Scholar]
- Retief, M.; Letsosa, R. Models of disability: A brief overview. Hts Teol. Stud. Theol. Stud. 2018, 74, 8. [Google Scholar] [CrossRef]
- Scally, G.; Donaldson, L.J. The NHS’s 50 anniversary. Clinical governance and the drive for quality improvement in the new NHS in England. BMJ 1998, 317, 61–65. [Google Scholar] [CrossRef] [PubMed]
- National Disability Insurance Scheme (Quality Indicators) Guidelines 2018; Commissioner of the NDIS Quality and Safeguards Commission: New South Wales, Australia, 2018.
- National Disability Insurance Scheme Quality and Safeguards Commission. NDIS Code of Conduct (NDIS Providers); Australian Government: Canberra, Australia, 2018.
- Booth, A. “Brimful of starlite”: Toward standards for reporting literature searches. J. Med. Libr. Assoc. 2006, 94, 421–429. [Google Scholar] [PubMed]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [PubMed]
- Hong, Q.N.; Pluye, P.; Fabregues, S.; Bartlett, G.; Boardman, F.; Cargo, M.; Dagenais, P.; Gagnon, M.-P.; Griffiths, F.; Nicolau, B.; et al. Mixed Methods Appraisal Tool (MMAT) Version 18: User Guide; Department of Family Medicine, McGill University: Montréal, QC, Canada, 2018. [Google Scholar]
- Antaki, C.; Webb, J. When the larger objective matters more: Support workers’ epistemic and deontic authority over adult service-users. Sociol. Health Illn. 2019, 41, 1549–1567. [Google Scholar] [CrossRef] [PubMed]
- Asher, L.; Hanlon, C.; Birhane, R.; Habtamu, A.; Eaton, J.; Weiss, H.A.; Patel, V.; Fekadu, A.; De Silva, M. Community-based rehabilitation intervention for people with schizophrenia in Ethiopia (RISE): A 12 month mixed methods pilot study. BMC Psychiatry 2018, 18, 250. [Google Scholar] [CrossRef] [PubMed]
- Banks, S. “Knowing me, knowing you’: Disability support worker as emotional mediator? Sexualities 2016, 19, 659–676. [Google Scholar] [CrossRef]
- Bhattacharjya, S.; Lenker, J. Using Smartphones to Disseminate Video-Based Rehabilitation Training Materials in Resource-Poor Regions in India. Arch. Phys. Med. Rehabilitation. 2019, 100, e140. [Google Scholar] [CrossRef]
- Bouchonville, M.F.; Hager, B.W.; Kirk, J.B.; Qualls, C.R.; Arora, S. Endo echo improves primary care provider and community health worker self-efficacy in complex diabetes management in medically underserved communities. Endocr. Pract. 2018, 24, 40–46. [Google Scholar] [CrossRef] [PubMed]
- Bourke, J.A.; Nunnerley, J.L.; Sullivan, M.; Derrett, S. Relationships and the transition from spinal units to community for people with a first spinal cord injury: A New Zealand qualitative study. Disabil. Health J. 2019, 12, 257–262. [Google Scholar] [CrossRef] [PubMed]
- Bourne, J.; Selman, M.; Hackett, S. Learning from support workers: Can a dramatherapy group offer a community provision to support changes in care for people with learning disabilities and mental health difficulties? Br. J. Learn. Disabil. 2020, 48, 59–68. [Google Scholar] [CrossRef]
- Brooker, J.; Julian, J.; Webber, L.; Chan, J.; Shawyer, F.; Meadows, G. Evaluation of an Occupational Mindfulness Program for Staff Employed in the Disability Sector in Australia. Mindfulness 2013, 4, 122–136. [Google Scholar] [CrossRef]
- Chappell, P.; Johannsmeier, C. The impact of community based rehabilitation as implemented by community rehabilitation facilitators on people with disabilities, their families and communities within South Africa. Disabil. Rehabil. 2009, 31, 7–13. [Google Scholar] [CrossRef] [PubMed]
- Ennion, L.; Rhoda, A. Roles and challenges of the multidisciplinary team involved in prosthetic rehabilitation, in a rural district in South Africa. J. Multidiscip. Healthc. 2016, 9, 565–573. [Google Scholar] [CrossRef] [PubMed]
- Forster, S.; Iacono, T. Disability support workers’ experience of interaction with a person with profound intellectual disability. J. Intellect. Dev. Disabil. 2008, 33, 137–147. [Google Scholar] [CrossRef] [PubMed]
- Gilmore, B.; MacLachlan, M.; McVeigh, J.; McClean, C.; Carr, S.; Duttine, A.; Mannan, H.; McAuliffe, E.; Mji, G.; Eide, A.H.; et al. A study of human resource competencies required to implement community rehabilitation in less resourced settings. Hum. Resour. Health 2017, 15, 70. [Google Scholar] [CrossRef]
- Goodale, B.; Spitz, S.; Beattie, N.; Lin, I. Training rural and remote therapy assistants in Western Australia. Rural Remote Health 2007, 7, 1–10. [Google Scholar] [CrossRef]
- Haines, D.; Wright, J.; Comerasamy, H. Occupational Therapy Empowering Support Workers to Change How They Support People with Profound Intellectual and Multiple Disabilities to Engage in Activity. J. Policy Pract. Intellect. Disabil. 2018, 15, 295–306. [Google Scholar] [CrossRef]
- Hoyle, L.; Brown, M.; Donaldson, J.; Karatzias, T. Invasive Clinical Intervention Education for Social Care Support Workers of Adults: A Review of the Current Literature. J. Policy Pract. Intellect. Disabil. 2017, 14, 240–250. [Google Scholar] [CrossRef]
- Hussain, R.; Wark, S.; Muller, A.; Ryan, P.; Parmenter, T. Personal relationships during end-of-life care: Support staff views of issues for individuals with intellectual disability. Res. Dev. Disabil. 2019, 87, 21–30. [Google Scholar] [CrossRef]
- Iacono, T.; Davis, R.; Humphreys, J.; Chandler, N. GP and support people’s concerns and priorities for meeting the health care needs of individuals with developmental disabilities: A metropolitan and non-metropolitan comparison. J. Intellect. Dev. Disabil. 2003, 28, 353–368. [Google Scholar] [CrossRef]
- Iacono, T.; Humphreys, J.; Davis, R.; Chandler, N. Health care service provision for country people with developmental disability: An Australian perspective. Res. Dev. Disabil. 2004, 25, 265–284. [Google Scholar] [CrossRef]
- Lin, I.; Goodale, B. Improving the supervision of therapy assistants in Western Australia: The Therapy Assistant Project (TAP). Rural Remote Health 2006, 6, 1–12. [Google Scholar] [CrossRef]
- Mason, V.; Williams, V. Enabling good emotional support for and with people with learning disabilities. Tizard Learn. Disabil. Rev. 2017, 22, 144–147. [Google Scholar] [CrossRef]
- Moskos, M.; Isherwood, L. Individualised funding and its implications for the skills and competencies required by disability support workers in Australia. Labour Ind. A J. Soc. Econ. Relat. Work. 2019, 29, 34–51. [Google Scholar] [CrossRef]
- Narayan, J.; Pratapkumar, R.; Reddy, S.P. Community managed services for persons with intellectual disability: Andhra Pradesh experience. J. Intellect. Disabil. 2017, 21, 248–258. [Google Scholar] [CrossRef] [PubMed]
- Venema, E.; Vlaskamp, C.; Otten, S. The role of volunteers in the social integration of people with intellectual disabilities. Res. Pract. Intellect. Dev. Disabil. 2018, 5, 154–167. [Google Scholar] [CrossRef]
- Wark, S.; Hussain, R.; Edwards, H. Rural and Remote Area Service Provision for People Aging With Intellectual Disability. J. Policy Pract. Intellect. Disabil. 2013, 10, 62–70. [Google Scholar] [CrossRef]
- Wark, S.; Hussain, R.; Edwards, H. Assisting individuals ageing with learning disability: Support worker perspectives. Tizard Learn. Disabil. Rev. 2015, 20, 213–222. [Google Scholar] [CrossRef]
- Australian Commission on Safety and Quality in Health Care. National Safety and Quality Health Service Standards: Training and Competencies for Recognising and Responding to Clinical Deterioration in Acute Care; Australian Government: Canberra, Australia, 2014.
- O’Sullivan, B.G.; Cairns, A.; Gurney, T.M. Understanding the field of rural health academic research: A national qualitative, interview-based study. Rural Remote Health 2020, 20, 6116. [Google Scholar] [CrossRef]
- Moran, A.; Haines, H.; Raschke, N.; Schmidt, D.; Koschel, A.; Stephens, A.; Opie, C.; Nancarrow, S. Mind the gap: Is it time to invest in embedded researchers in regional, rural and remote health services to address health outcome discrepancies for those living in rural, remote and regional areas? Aust. J. Prim. Health 2019, 25, 104–107. [Google Scholar] [CrossRef] [PubMed]
- Nancarrow, S.A.; Borthwick, A.M. The Allied Health Professions: A Sociological Perspective; Bristol University Press, Policy Press: Bristol, UK, 2021. [Google Scholar]
| Concept 1: Therapy Support Workers Who Deliver Allied Health Support |
Concept 2:
Governance |
Concept 3:
Disability |
Concept 4:
Rural and Remote |
|---|---|---|---|
| Therapy support workers who deliver allied health support | Governance | Disability | Rural and Remote |
| Assistant practitioner *.mp or | Governance | Disability * therapy.mp or | Rural health/or |
| Community health workers/or | Quality | Disabled persons/or | Rural health services.mp or |
| Auxiliary personnel *.mp or | Safe (ty) | Disabled people.mp or | Rural population.mp or |
| MM Allied health personnel or | Effective | Disabled persons/or | MM Rural Health Personnel or |
| Allied health workers.mp or | Risk | Disability * service *.mp or | MM Rural Health Centers OR |
| Allied health assistant *.mp or | Accountable/accountability | MM “Health Services for Persons with Disabilities” | MM “Services for Australian Rural and Remote Allied Health or |
| Allied health helper *.mp or | Person-centred | Rural | |
| Allied health aide *.mp or | Complaint | ||
| Personal care workers.mp or | Incident | ||
| Personal care assistant *.mp or | Misconduct | ||
| Patient care workers.mp or | Neglect | ||
| Personal care helper *.mp or | Violence | ||
| Personal care aide *.mp or | Abuse | ||
| Patient care helper *.mp or | Supervision | ||
| Patient care aide * or | Delegation | ||
| Patient care assistant *.mp or | Allocating tasks | ||
| Support worker *.mp or | Training | ||
| Support helper *.mp or | Competent/competency | ||
| Support aide *.mp | Transferring tasks | ||
| Health worker *.tw or | Qualification | ||
| Health assistant *.tw or | Responsibility/responsibilities | ||
| Health worker *.mp or | Knowledge | ||
| Health assistant *.mp or | Skills | ||
| Community rehabilitation helper *.mp or | Development | ||
| Community rehabilitation worker *.mp or | Professional | ||
| Community rehabilitation assistant *.mp or | Development | ||
| Community rehabilitation aide *.mp or | Skill level | ||
| Community health helper *.mp or | Credential | ||
| Community health worker *.mp | Communication | ||
| Community health assistant *.mp or | Education | ||
| Community health aide *.mp or | Instruction | ||
| Therapy support worker *.mp or | Assess | ||
| Disability * support worker *.mp or | |||
| Workforce/or | |||
| Health Workforce.mp | |||
| MM “Physical Therapist Assistants” or |
| Process | Detail |
|---|---|
| Sampling strategy | Selective: samples databases from medicine, nursing, allied health, and social science fields within specified limits. |
| Type of study | All, quantitative research (randomized controlled trial, controlled clinical trial, controlled before and after study, uncontrolled before and after study), qualitative research (grounded theory, ethnography, action research, exploratory approaches, phenomenology, and systematic reviews). Published reports, evaluations, guidelines, and frameworks. |
| Approaches | Subject searching, citation searching, contact with authors. |
| Range of years | January 2000–May 2020. |
| Inclusion and exclusions ¶ | Inclusion: empirical study or published report, evaluation, framework, or guideline describing governance models pertaining to allied health assistants, therapy assistants, and disability therapy support workers who deliver care and interventions under the guidance of allied health professionals and specifically in disability contexts (Tier 2) and in regional, remote, and/or rural areas (Tier 3). |
| Terms used | See concept map (Table 1) |
| Electronic sources | CINAHL; EMBASE; InfoRMIT:Health Collection; MEDLINE and Web of Science. |
| Process | Decision | ||
|---|---|---|---|
| 1. Does the paper examine the assistant/support workforce (Concept 1)? | Yes—Go to 2 | No—Exclude | Cannot tell—Get full paper |
| 2. Does the paper relate to the allied health professions (outside of acute health or rehabilitation settings) (Concept 1)? | Yes—Go to 3 | No—Exclude | Cannot tell—get full paper |
| 3. Does the paper examine a governance model, framework, policy, intervention, or evaluation (Concept 2)? | Yes—Go to 4 | No—Exclude or consider for background | Cannot tell—Get full paper |
| 4. Does the study provide detail of the governance model or intervention (Concept 2)? | Yes –Include as Tier 1 evidence and go to 5 | No—Exclude or consider for background | Cannot tell—Get full paper |
| 5. Does the paper relate to the disability sector (Concept 3)? | Yes—Include as Tier 2 evidence and go to 6 | No—Include paper for Tier 1 evidence | Cannot tell—Get full paper |
| 6. Does the study examine regional, rural and/or remote areas (Concept 4)? | Yes—Include as Tier 3 evidence | No—Include paper for Tier 1 or 2 evidence and check references | Cannot tell—Get full paper |
| Reference | Governance Component | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Capability (Soft Skills) | Capability (Intrinsic Attributes) | Competency | Supervision | Credentialling | Assessment of Competence | Professional Development | Support Structures | Care Plans | |
| [27] | X | ||||||||
| [28] | X | X | |||||||
| [29] | X | X | |||||||
| [30] | |||||||||
| [31] | X | ||||||||
| [32] | X | X | |||||||
| [33] | X | ||||||||
| [34] | X | ||||||||
| [35] | X | ||||||||
| [36] | X | X | |||||||
| [37] | X | ||||||||
| [38] | X | X | X | X | X | ||||
| [39] | X | X | |||||||
| [40] | |||||||||
| [41] | X | X | X | X | X | X | |||
| [42] | X | ||||||||
| [43] | X | ||||||||
| [44] | X | X | |||||||
| [45] | X | ||||||||
| [46] | X | ||||||||
| [47] | X | X | X | ||||||
| [48] | X | ||||||||
| [49] | X | ||||||||
| [50] | X | X | |||||||
| [51] | X | X | |||||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Moran, A.; Bulkeley, K.; Johnsson, G.; Tam, E.; Maloney, C. Models of Governance of Disability Therapy Support Workers in Rural and Remote Settings: A Systematic Scoping Review. Int. J. Environ. Res. Public Health 2024, 21, 693. https://doi.org/10.3390/ijerph21060693
Moran A, Bulkeley K, Johnsson G, Tam E, Maloney C. Models of Governance of Disability Therapy Support Workers in Rural and Remote Settings: A Systematic Scoping Review. International Journal of Environmental Research and Public Health. 2024; 21(6):693. https://doi.org/10.3390/ijerph21060693
Chicago/Turabian StyleMoran, Anna, Kim Bulkeley, Genevieve Johnsson, Elaine Tam, and Catherine Maloney. 2024. "Models of Governance of Disability Therapy Support Workers in Rural and Remote Settings: A Systematic Scoping Review" International Journal of Environmental Research and Public Health 21, no. 6: 693. https://doi.org/10.3390/ijerph21060693
APA StyleMoran, A., Bulkeley, K., Johnsson, G., Tam, E., & Maloney, C. (2024). Models of Governance of Disability Therapy Support Workers in Rural and Remote Settings: A Systematic Scoping Review. International Journal of Environmental Research and Public Health, 21(6), 693. https://doi.org/10.3390/ijerph21060693






