Users’ Perceptions of Access to and Quality of Unified Health System Services in Brazil: A Cross-Sectional Study and Implications to Healthcare Management Challenges
Abstract
1. Introduction
2. Methods
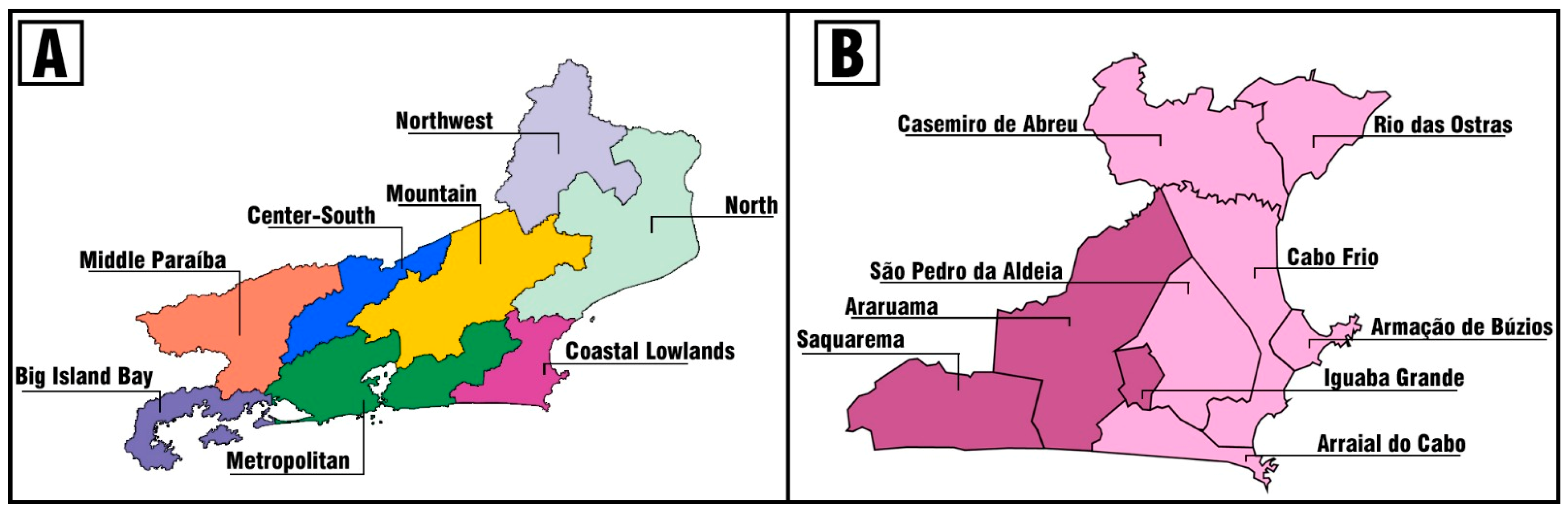
2.1. Study Design and Setting
2.2. Survey Instrument and Pilot Study
2.3. Data Collection and Inclusion Criteria
2.4. Data Analysis
2.5. Ethical Aspects
3. Results
3.1. Population Characteristics
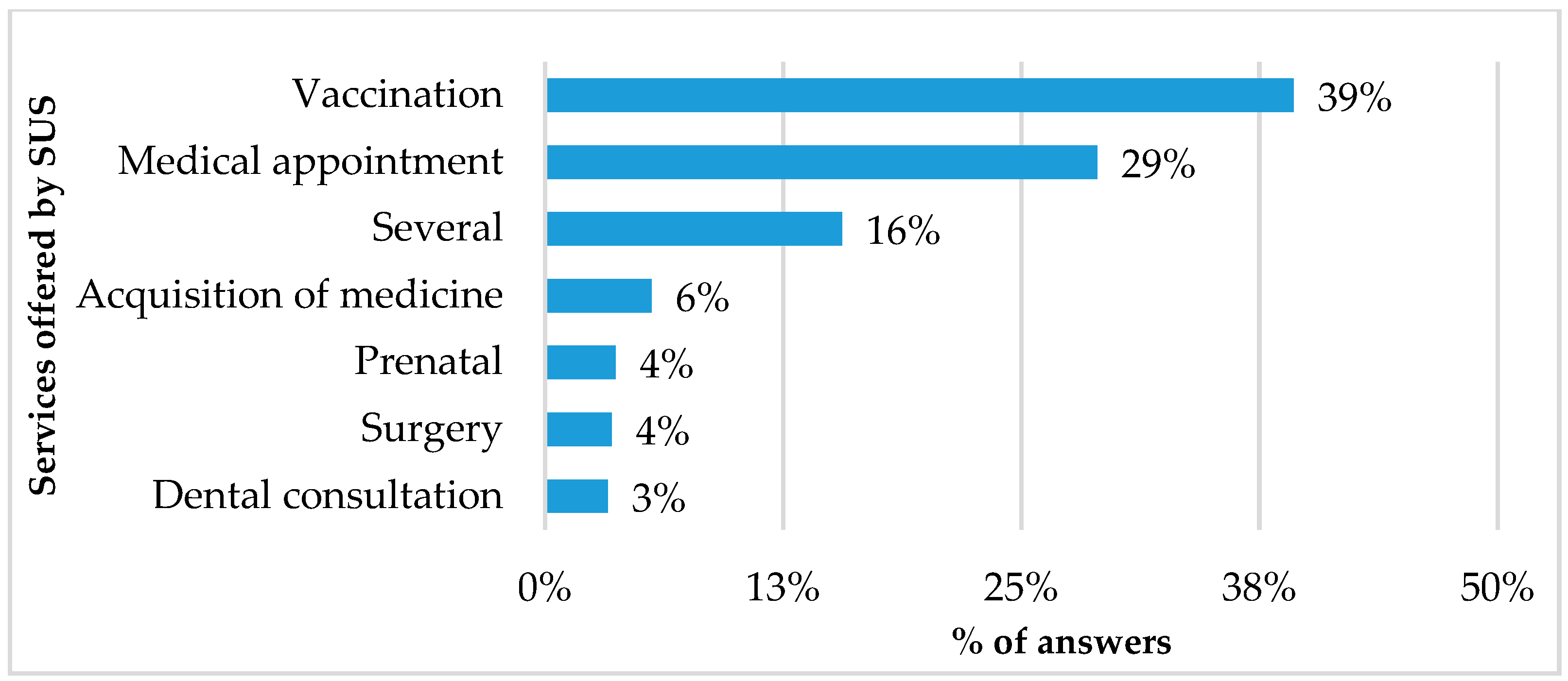
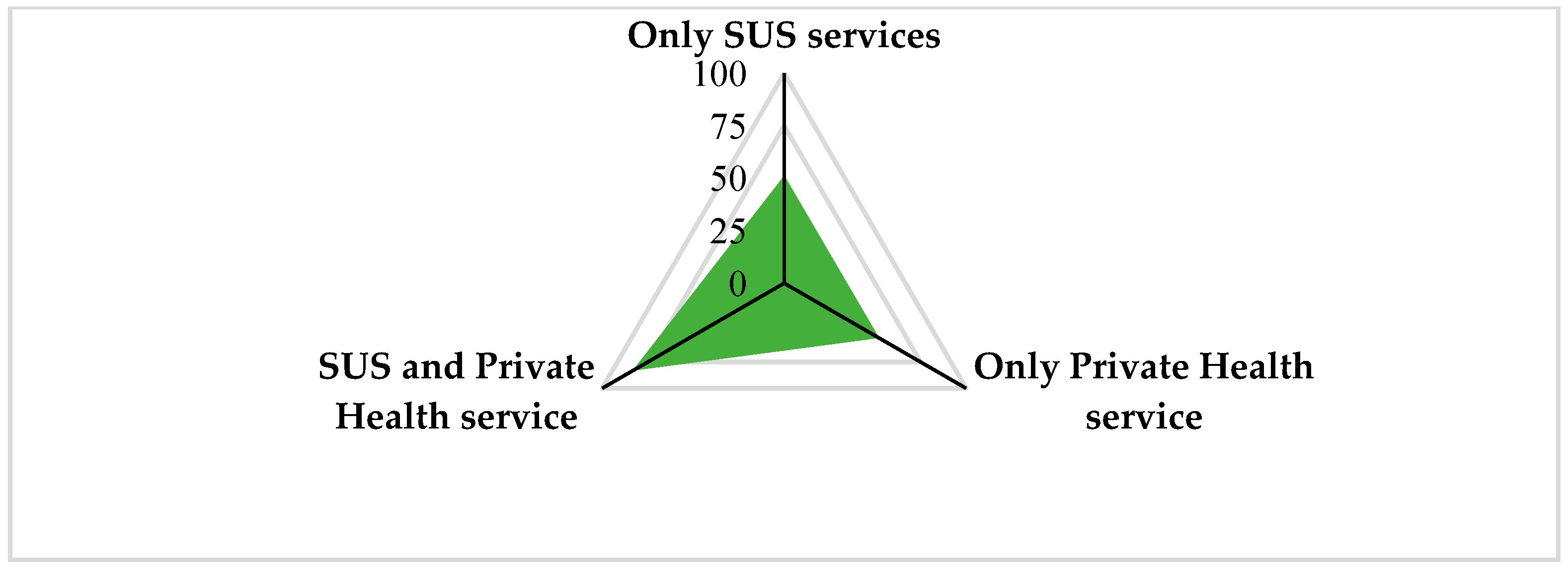
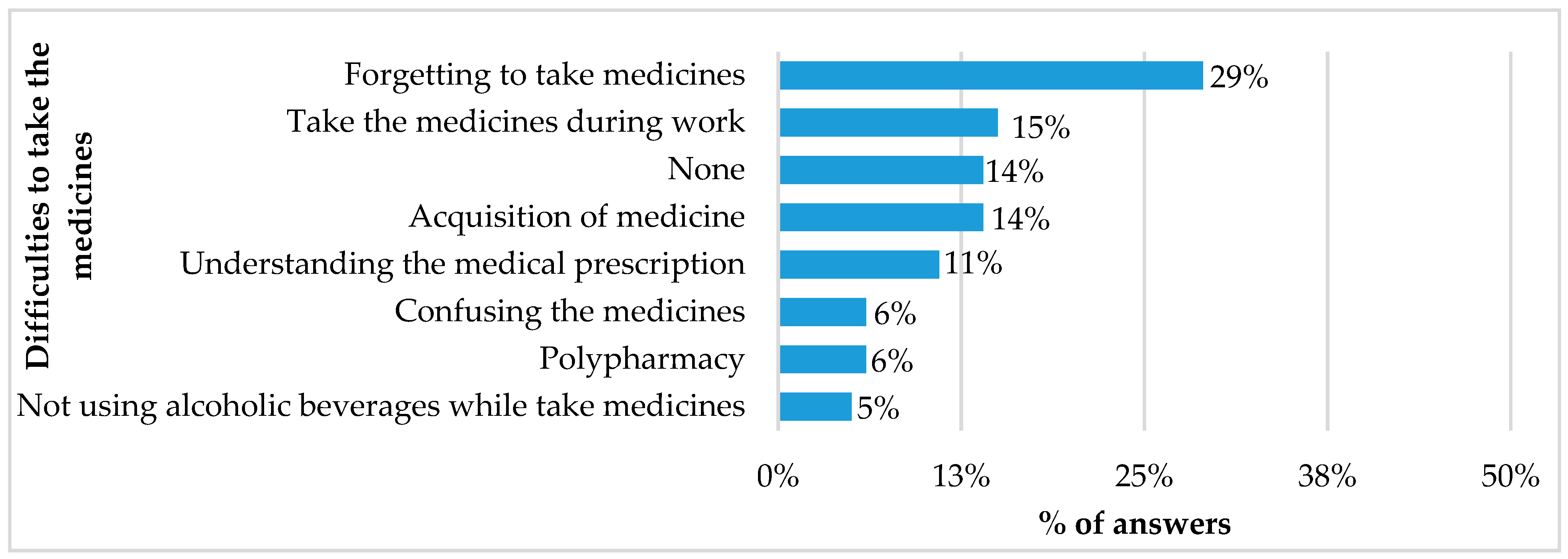
3.2. Step Two: SUS Users’ Perceptions Regarding Access to and Quality of Health Services
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- BRASIL. Emenda Constitucional nº 29, de 13 de Setembro de 2000. Constituição da República Federativa do Brasil de 1988; Presidência da República: Brasília, Brazil, 2000. [Google Scholar]
- BRASIL. Lei nº 8.080, de 19 de Setembro de 1990; Presidência da República: Brasília, Brazil, 1990. Available online: https://www.planalto.gov.br/ccivil_03/leis/l8080.htm (accessed on 15 January 2024).
- BRASIL. Lei nº 8.142, de 28 de Dezembro de 1990; Presidência da República: Brasília, Brazil, 1990. Available online: https://www.planalto.gov.br/ccivil_03/leis/l8142.htm (accessed on 29 February 2024).
- BRASIL. Emenda Constitucional nº 95, de 15 de Dezembro de 2016; Presidência da República: Brasília, Brazil, 2016. Available online: https://www.planalto.gov.br/ccivil_03/constituicao/emendas/emc/emc95.htm (accessed on 29 February 2024).
- Matta, G.C. Princípios e diretrizes do Sistema Único de Saúde. In Políticas de Saúde: Organização e Operacionalização do Sistema Único de Saúde; Matta, G.C., Pontes, A.L.d.M., Eds.; Coleção Educação Profissional e Docência em Saúde: A formação e o trabalho do agente comunitário de saúde, 3; EPSJV/FIOCRUZ: Rio de Janeiro, Brazil, 2007; pp. 61–80. [Google Scholar]
- Ministry of Health. Portaria N° 4.279, de 30 de Dezembro de 2010. Estabelece Diretrizes Para a Organização da Rede de Atenção à Saúde no Âmbito do Sistema Único de Saúde (SUS); Ministry of Health: Brasília, Brazil, 2010. [Google Scholar]
- Castro, M.C.; Massuda, A.; Almeida, G.; Menezes-Filho, N.A.; Andrade, M.V.; de Souza Noronha, K.V.M.; Rocha, R.; Macinko, J.; Hone, T.; Tasca, R.; et al. Brazil’s unified health system: The first 30 years and prospects for the future. Lancet 2019, 394, 345–356. [Google Scholar] [CrossRef] [PubMed]
- Starfield, B.; Shi, L.; Macinko, J. Contribution of Primary Care to Health Systems and Health. Milbank Q. 2005, 83, 457–502. [Google Scholar] [CrossRef]
- NESCON. Atenção Primária deve Solucionar a Maioria dos Problemas de Saúde; Nescon/UFMG: Belo Horizonte, Brazil, 2015; Available online: https://www.nescon.medicina.ufmg.br/atencao-primaria-deve-solucionar-maioria-dos-problemas-de-saude/ (accessed on 16 January 2024).
- World Health Organization; Organization for Economic Co-operation and Development & International Bank for Reconstruction and Development. Delivering Quality Health Services: A Global Imperative for Universal Health Coverage; World Health Organization: Geneva, Switzerland, 2018; Available online: https://iris.who.int/handle/10665/272465 (accessed on 10 January 2024).
- Macinko, J.; Starfield, B.; Shi, L. The Contribution of Primary Care Systems to Health Outcomes within Organization for Economic Cooperation and Development (OECD) Countries, 1970–1998. Health Serv. Res. 2003, 38, 831–865. [Google Scholar] [CrossRef]
- Simão, C.C.A.L.; Costa, M.B.; Colugnati, F.A.B.; de Paula, E.A.; Vanelli, C.P.; de Paula, R.B. Quality of Care of Patients with Diabetes in Primary Health Services in Southeast Brazil. J. Environ. Public Health 2017, 2017, e1709807. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5654281/pdf/JEPH2017-1709807.pdf (accessed on 29 March 2024). [CrossRef]
- Senn, N.; Breton, M.; Ebert, S.T.; Lamoureux-Lamarche, C.; Lévesque, J.F. Assessing primary care organization and performance: Literature synthesis and proposition of a consolidated framework. Health Policy 2021, 125, 160–167. [Google Scholar] [CrossRef]
- Ministry of Health. Portaria Programa Nacional de Imunizações—Vacinação; Ministry of Health: Brasília, Brazil, 2023. [Google Scholar]
- Cmas, D.; Maranhão, A.G.K.; Teixeira, A.M.; Fantinato, F.F.S.; Domingues, R.A.S. 46 Anos do Programa Nacional de Imunizações: Uma História Repleta de Conquistas e Desafios a Serem Superados. Cad. Saúde Pública [Internet] 2020, 36, e00222919. [Google Scholar] [CrossRef]
- Ministry of Health. Vacinômetro COVID-19; Ministry of Health: Brasília, Brazil, 2024. Available online: https://infoms.saude.gov.br/extensions/SEIDIGI_DEMAS_Vacina_C19/SEIDIGI_DEMAS_Vacina_C19.html (accessed on 29 March 2024).
- IBGE. Censo 2022. De 2010 2022, População Brasileira Cresce 6.5% e Chega a 203.1 Milhõe; IBGE: Brasília, Brazil, 2023. [Google Scholar]
- BRASIL. Lei nº. 141, de 13 de Janeiro de 2012; Diário Oficial da União: Brasília, Brazil, 2012. [Google Scholar]
- Ministry of Health. Conselho Nacional de Saúde Recomenda Ampliação de Recursos para o SUS e Garantia do piso Constitucional; Ministry of Health: Brasília, Brazil, 2023. [Google Scholar]
- ANS NEW. Beneficiários de Planos Privados de Saúde, por Cobertura Assistencial (Brasil—2014–2024). Available online: https://www.gov.br/ans/pt-br/acesso-a-informacao/perfil-do-setor/dados-gerais (accessed on 22 May 2024).
- Samuelson-Kiraly, C.; Montague, T.; Nemis-White, J.; MacPherson, N.; Martin, L.; Aylen, J.; Gogovor, A.; Mitchell, J.I. Access and quality of health care in Canada: Insights from 1998 to the presents. Healthc. Manag. Forum 2020, 33, 253–258. [Google Scholar] [CrossRef]
- ANS. Dados Gerais. In Beneficiários de Planos Privados de Saúde, por Cobertura Assistencial (Brasil—2013–2023); ANS: Brasília, Brazil, 2024. Available online: https://www.gov.br/ans/pt-br/acesso-a-informacao/perfil-do-setor/dados-gerais (accessed on 30 March 2024).
- Godói, I.P.; Santos, A.S.; Reis, E.A.; Lemos, L.L.P.; Brandão, C.M.R.; Alvares, J.; Acurcio, F.A.; Godman, B.; Guerra Júnior, A.A. Consumer Willingness to Pay for Dengue Vaccine (CYD-TDV, Dengvaxia®) in Brazil; Implications for Future Pricing Considerations. Front. Pharmacol. 2017, 8, 41. [Google Scholar] [CrossRef]
- Campbell, S.M.; Roland, M.O.; Buetow, S.A. Defining quality of care. Soc. Sci. Med. 2000, 51, 1611–1625. Available online: https://pubmed.ncbi.nlm.nih.gov/11072882/ (accessed on 29 March 2024). [CrossRef]
- Agency for Healthcare Research and Quality. Six Domains of Health Care Quality. Available online: https://www.ahrq.gov/talkingquality/measures/six-domains.html (accessed on 30 March 2024).
- Stopa, S.R.; Malta, D.C.; Monteiro, C.N.; Szwarcwald, C.L.; Goldbaum, M.; Cesar, C.L.G. Use of and access to health services in Brazil, 2013 National Health Survey. Rev. Saúde Pública 2017, 51 (Suppl. 1), 3s. [Google Scholar] [CrossRef]
- De Fátima Vasques Monteiro, M.; Barbosa, C.P.; Vertamatti, M.A.F.; Tavares, M.N.A.; de Oliveira Carvalho, A.C.; Alencar, A.P.A. Access to public health services and integral care for women during the puerperal gravid period period in Ceará, Brazil. BMC Health Serv. Res. 2019, 19, 851. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6868722/ (accessed on 29 March 2024). [CrossRef]
- Vilarins, G.C.M.; Pinho, D.L.M. Application of conceptual mapping in the regulation of access to public health services in the Federal District, Brazil. Ciência Saúde Coletiva 2021, 26, 5829–5840. Available online: https://www.scielo.br/j/csc/a/WJ9KwSsQXcvcRsvc864VBgb/?lang=pt (accessed on 29 March 2024). [CrossRef]
- Bittencourt, S.D.D.A.; Domingues, R.M.; Reis, L.G.; Ramos, M.M.; Leal, M.D. Adequacy of public maternal care services in Brazil. Reprod. Health 2016, 13, 120. Available online: https://pubmed.ncbi.nlm.nih.gov/27766964/ (accessed on 29 March 2024). [CrossRef]
- Pinto, R.D.S.; Roncalli, A.G.; Abreu, M.H.; Vargas, A.M. Use of Public Oral Health Services by the Adult Population: A Multi-level Analysis. PLoS ONE 2016, 11, e0145149. Available online: https://pubmed.ncbi.nlm.nih.gov/26730714/ (accessed on 29 March 2024). [CrossRef][Green Version]
- Hercos, B.V.S.; Berezovsky, A. Quality of the ophthalmological service to outpatients of the public and private healthcare systems. Arq. Bras. Oftalmol. 2017, 80, 350–354. Available online: https://pubmed.ncbi.nlm.nih.gov/29267568/ (accessed on 29 March 2024). [CrossRef]
- Carvalho, M.; Queiroz, A.B.A.; Ferreira, M.A.; Moura, M.A.V.; Pinto, C.B.; Vieira, B.D.G. Ineffectiveness of information and access to health services: Vulnerability to human papillomavirus. Int. Nurs. Rev. 2019, 66, 280–289. Available online: https://pubmed.ncbi.nlm.nih.gov/30815859/ (accessed on 29 March 2024). [CrossRef]
- Soeiro, O.M.; Tavares, N.U.L.; Do Nascimento Júnior, J.M.; Guerra Junior, A.A.; Costa, E.A.; de Assis Acurcio, F.; Guibu, I.A.; Álvares, J.; de Oliveira Karnikowski, M.G.; Leite, S.N.; et al. Patient satisfaction with pharmaceutical services in Brazilian primary health care. Rev. Saúde Pú-Blica (Online) 2017, 51, 1S–11S. [Google Scholar] [CrossRef]
- Garcia, M.M.; Azevedo, P.S.; Mirelman, A.; Safatle, L.P.; Iunes, R.; Bennie, M.C.; Godman, B.; Guerra Junior, A.A. Funding and Service Organization to Achieve Universal Health Coverage for Medicines: An Economic Evaluation of the Best Investment and Service Organization for the Brazilian Scenario. Front. Pharmacol. 2020, 11, 370. [Google Scholar] [CrossRef]
- Souza, E.C.F.D.; de Vilar, R.L.A.; De Sá Pinto Dantas Rocha, N.; da Costa Uchôa, S.A.; de Medeiros Rocha, P. Acesso e acolhimento na atenção básica: Uma análise da percepção dos usuários e profissionais de saúde. Cad. Saúde Pública Rio Jan. 2008, 24 (Suppl. 1), s100–s110. [Google Scholar] [CrossRef]
- WHO Library Cataloguing; World Health Organization. Global Strategy on Human Resources for Health: Workforce 2030; WHO: Geneva, Switzerland, 2016. [Google Scholar]
- WHO Library Cataloguing; World Health Organization. Monitoring the Building Blocks of Health Systems: A Handbook of Indicators and Their Measurement Strategies; WHO: Geneva, Switzerland, 2010. [Google Scholar]
- OECD. Primary Health Care in Low- and Middle-Income Countries. Realizing the Potential of Primary Health Care. OECD iLibrary. Available online: https://www.oecd-ilibrary.org/sites/5a3b7d49-en/index.html?itemId=/content/component/5a3b7d49-en (accessed on 22 January 2024).
- The Commonwealth Fund. Mirror, Mirror 2021: Reflecting Poorly. Available online: https://www.commonwealthfund.org/publications/fund-reports/2021/aug/mirror-mirror-2021-reflecting-poorly (accessed on 22 January 2024).
- Nunes, L.O.; Castanheira, E.R.L.; Sanine, P.R.; Akerman, M.; Nemes, M.I.B. Performance assessment of primary health care facilities in Brazil: Concordance between web-based questionnaire and in-person interviews with health personnel. PLoS ONE 2023, 18, e0281085. [Google Scholar] [CrossRef]
- IBGE. Panorama; Instituto Brasileiro de Geografia e Estatística: Rio de Janeiro, Brazil, 2022. Available online: https://cidades.ibge.gov.br/brasil/rj/panorama (accessed on 18 February 2024).
- Kuschnir, R.; Chorny, A.; Lira, A.M.L.E.; Sonoda, G.; Fonseca, T.M.P. Regionalização no Estado do Rio de Janeiro: O Desafio de Aumentar Acesso e Diminuir Desigualdades. A Gestão do SUS no Âmbito Estadual: O Caso do Rio de Janeiro; Editora FIOCRUZ: Rio de Janeiro, Brazil, 2010; pp. 215–240. [Google Scholar]
- Diagnóstico de Saúde da Região da Baixada Litorânea; Secretaria de Saúde do Governo do Estado do Rio de Janeiro: Rio de Janeiro, Brazil 2020. Available online: https://www.saude.rj.gov.br/comum/code/MostrarArquivo.php?C=MzUwNzA%2C (accessed on 28 February 2024).
- Rio da Ostras. Dados Municipais; Prefeitura Municipal de Rio das Ostras: Rio de Janeiro, Brazil, 2024. Available online: https://www.riodasostras.rj.gov.br/dados-municipais/#:~:text=O%20resultado%20do%20Censo%202022,foi%20de%2048%2C09%25 (accessed on 29 March 2024).
- Defesa Civil do Estado do Rio de Janeiro. Relação de Municípios do Estado do Rio de Janeiro por data de adesão, Brazil. 2024. Available online: https://www.defesacivil.rj.gov.br/index.php/cidades-resilientes/item/61-relacao-de-municipios-do-estado-do-rio-de-janeiro-por-data-de-adesao (accessed on 28 May 2024).
- IBGE. Dados Sobre Estados Brasileiros. Panorama Cabo Frio, Brazil. 2023. Available online: https://cidades.ibge.gov.br/brasil/rj/cabo-frio/panorama (accessed on 18 February 2024).
- IBGE. Dados Sobre Estados Brasileiros. Panorama Rio das Ostras, Brazil. 2023. Available online: https://cidades.ibge.gov.br/brasil/rj/rio-das-ostras/panorama (accessed on 18 February 2024).
- Ministry of Health. Secretaria de Ciência, Tecnologia e Insumos Estratégicos. Componente Populacional: Introdução, Método e Instrumentos/Ministério da Saúde, Secretaria de Ciência, Tecnologia e Insumos Estratégicos; il.—Série Pnaum—Pesquisa Nacional sobre Acesso, Utilização e Promoção do Uso Racional de Medicamentos no Brasil; Caderno 1; Ministério da Saúde: Brasília, Brazil, 2016; 80p. [Google Scholar]
- Ministry of Health. Programa Nacional de Melhoria do Acesso e da Qualidade da Atenção Básica (PMAQ); Ministry of Health: Brasília, Brazil, 2011. Available online: https://www.gov.br/saude/pt-br/composicao/saps/pmaq (accessed on 23 February 2024).
- Galloway, A. Convenience Sampling—An Overview|ScienceDirect Topics. Encyclopedia of Social Measurement. Non-Probability Sampling—Convenience Sampling; Elsevier: Amsterdam, The Netherlands, 2005; ISBN 978-0-12-369398-3. Available online: https://www.sciencedirect.com/topics/computer-science/convenience-sampling#:~:text=Convenience%20Sampling-,Definition,in%20a%20workplace%2C%20for%20example (accessed on 23 May 2024).
- BRASIL. Histórico de Cotação; Banco Central do Brasil: Brasília, Brazil, 2023. Available online: https://www.bcb.gov.br/estabilidadefinanceira/historicocotacoes (accessed on 22 February 2024).
- BRASIL. Lei n. 14.663, de 28 de Agosto de 2023; Presidência da República: Brasília, Brazil, 2023. Available online: https://www.planalto.gov.br/ccivil_03/_Ato2023-2026/2023/Lei/L14663.htm (accessed on 22 February 2024).
- Bousquat, A.; Giovanella, L.; Campos, E.M.S.; Almeida, P.F.; Martins, C.L.; Mota, P.H.D.S.; Mendonça, M.H.M.; Medina, M.G.; Viana, A.L.D.; Fausto, M.C.R.; et al. Primary health care and the coordination of care in health regions: Managers’ and users’ perspective. Cienc. Saude Coletiva 2017, 22, 1141–1154. Available online: https://pubmed.ncbi.nlm.nih.gov/28444041/ (accessed on 29 March 2024). [CrossRef]
- Boing, A.; Andrade, F.; Bertoldi, A.; Glazer, K.; Peres, A.; Massuda, A.; Boing, A. Prevalências e desigualdades no acesso aos medicamentos por usuários do Sistema Único de Saúde no Brasil em 2013 e 2019. Cad. Saúde Pública 2022, 38, e00114721. [Google Scholar] [CrossRef]
- De Carvalho, A.L.B.; de Jesus, W.L.A.; Senra, I.M.V.B. Regionalization in the SUS: Implementation process, challenges and perspectives in the critical view of system managers. Ciência Saúde Coletiva 2017, 22, 1155–1164. Available online: https://www.scielo.br/j/csc/a/X5tq3bQgN8XkGkths95ctkz/?lang=en# (accessed on 20 May 2024).
- Peixoto, R.T.; Campos, M.R.; Luiza, V.L.; Mendes, L.V. O farmacêutico na Atenção Primária à Saúde no Brasil: Análise comparativa 2014–2017. Saúde Debate 2022, 46, 358–375. Available online: https://www.scielo.br/j/sdeb/a/3LgFkWC3ryTCc79YQnhSmdv/?format=pdf&lang=pt (accessed on 22 January 2024). [CrossRef]
- Tôrres, L.L.; Azevedo, P.S.; Rocha Sarmento, T.T.; Ramalho-de-Oliveira, D.; Reis, E.A.; Dias Godói, I.P.; Guerra Júnior, A.A.; Ruas, C.M. Acceptability and consumers’ willingness to pay for comprehensive medication management services in Brazil. J. Comp. Eff. Res. 2024, 13, e230127. [Google Scholar] [CrossRef]
- IBGE. Síntese de Indicadores Sociais: Uma Análise das Condições de Vida da População Brasileira; IBGE: Brasilia, Brazil, 2014. Available online: http://biblioteca.ibge.gov.br/visualizacao/livros/liv91983.pdf (accessed on 30 March 2024).
| Variable | n | (%) * |
| Female | 134 | 67.0% |
| Male | 66 | 33.0% |
| Age Profile (years old) | ||
| 18–25 | 21 | 10.5% |
| 26–45 | 103 | 51.5% |
| 46–60 | 54 | 27.0% |
| More than 60 | 22 | 11.0% |
| Race/skin color | ||
| White | 73 | 36.5% |
| Black | 30 | 15.0% |
| Brown | 94 | 47.0% |
| Other | 3 | 1.5% |
| Education level | ||
| Never attended school | 2 | 1.0% |
| Incomplete elementary education | 21 | 10.5% |
| Completed elementary school | 14 | 7.0% |
| Incomplete high school | 10 | 5.0% |
| Completed high school | 54 | 27.0% |
| Incomplete college | 36 | 18.0% |
| Completed college or more | 63 | 31.5% |
| Family income * (number of times the minimum wage) ** | ||
| Up to 1 | 17 | 8.5% |
| 1–2 | 46 | 23.0% |
| 2–3 | 42 | 21.0% |
| 3–5 | 51 | 25.5% |
| 5–10 | 27 | 13.5% |
| 10–20 | 3 | 1.5% |
| >20 | 2 | 1.0% |
| Use of SUS services—Yes | 195 | 97.5% |
| Has a private health plan—Yes | 95 | 47.5% |
| Clinical Condition | % |
|---|---|
| Other respiratory diseases | 26.2% |
| Anxiety/Depression | 13.8% |
| Hypertension | 12.4% |
| Other diseases | 12.0% |
| Chronic Obstructive Pulmonary Disease | 11.3% |
| Dyslipidemia | 10.5% |
| Joint Disorders | 7.7% |
| Diabetes Mellitus | 3.1% |
| Other Cardiovascular problems | 3.0% |
| Relevance of SUS n (%) | ||||||||
| Frequency | Indispensable/Essential | Complementary | Indifferent | p-Value | ||||
| Always | 27 (81.8%) | 3 (9.1%) | 3 (9.1%) | 0.031 | ||||
| Frequently | 37 (100.0%) | 0 (0.00%) | 0 (0.00%) | |||||
| Sometimes | 74 (88.1%) | 6 (7.1%) | 4 (4.8%) | |||||
| Rarely | 34 (82.9%) | 7 (17.1%) | 0 (0.00%) | |||||
| ALL | 172 (88.2%) | 16 (8.2%) | 7 (3.6%) | |||||
| Access to SUS services n (%) | ||||||||
| Frequency | Very good | Good | Neither good nor bad | Bad | Very bad | p-value | ||
| Always | 2 (5.7%) | 12 (34.3%) | 14 (40.0%) | 5 (14.3%) | 2 (5.7%) | 0.002 | ||
| Frequently | 0 (0.00%) | 5 (13.8%) | 21 (55.6%) | 11 (30.6%) | 0 (0.00%) | |||
| Sometimes | 1 (1.2%) | 10 (12.8%) | 39 (47.5%) | 23 (29.5%) | 7 (9.0%) | |||
| Rarely | 3 (7.3%) | 3 (7.3%) | 15 (34.15%) | 12 (29.3%) | 9 (21.9%) | |||
| ALL | 6 (3.1%) | 30 (15.8%) | 90 (44.7%) | 51 (26.7%) | 18 (9.7%) | |||
| Quality of SUS services n (%) | ||||||||
| Frequency | Very good | Good | Neither good nor bad | Bad | Very bad | p-value | ||
| Always | 4 (11.8%) | 8 (23.5%) | 14 (38.3%) | 8 (23.5%) | 1 (2.9%) | 0.000 | ||
| Frequently | 1 (2.7%) | 5 (13.5%) | 17 (43.3%) | 15 (40.5%) | 0 (0.0%) | |||
| Sometimes | 0 (0.00%) | 14 (16.9%) | 51 (60.2%) | 14 (16.9%) | 5 (6.0%) | |||
| Rarely | 4 (10.8%) | 8 (21.6%) | 10 (24.4%) | 9 (24.3%) | 7 (18.9%) | |||
| ALL | 9 (4.7%) | 35 (18.3%) | 92 (46.1%) | 46 (24.1%) | 13 (6.8%) | |||
| Presence of the Pharmacist in the Pharmacy n (%) | ||||||||
| Acquisition of Medicines | Always | Often | Sometimes | Rarely | Never | p-Value | ||
| Public Pharmacy | 1 (10.0%) | 2 (20.0%) | 1 (10.0%) | 0 (0.0%) | 6 (60.0%) | 0.001 | ||
| Public and Private | 6 (18.8%) | 6 (18.8%) | 14 (43.8%) | 5 (15.6%) | 1 (3.1%) | |||
| ALL | 7 (16.7%) | 8 (19.1%) | 15 (35.7%) | 5 (11.8%) | 7 (16.7%) | |||
| Role of the Pharmacist in patient guidance n (%) | ||||||||
| Acquisition of medicines | Indispensable/Essential | Indifferent | Unnecessary | p-value | ||||
| Public Pharmacy | 2 (22.2%) | 6 (66.7%) | 1 (11.1%) | 0.0005 | ||||
| Public and Private | 42 (97.7%) | 1 (2.3%) | 0 (0.0%) | |||||
| ALL | 44 (84.6%) | 7 (13.5%) | 1 (1.9%) | |||||
| Access to SUS Services n (%) | ||||
|---|---|---|---|---|
| Access to SUS Services | Infrastructure | Health Professionals | Services | p-Value |
| Very good | 7(77.8%) | 2 (22.2%) | 0 (0.0%) | 0.88 |
| Good | 24 (75.0%) | 6 (18.7%) | 2 (6.3%) | |
| Neither good nor bad | 62 (75.6%) | 11 (13.4%) | 9 (11.0%) | |
| Bad | 33 (78.6%) | 4 (9.5%) | 5 (11.90%) | |
| Very bad | 10 (76.9%) | 1 (7.7%) | 2 (15.4%) | |
| ALL | 136 (76.4%) | 24 (13.5%) | 18 (10.1%) | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Souza, J.S.; Reis, E.A.; Godman, B.; Campbell, S.M.; Meyer, J.C.; Sena, L.W.P.; Godói, I.P.D. Users’ Perceptions of Access to and Quality of Unified Health System Services in Brazil: A Cross-Sectional Study and Implications to Healthcare Management Challenges. Int. J. Environ. Res. Public Health 2024, 21, 721. https://doi.org/10.3390/ijerph21060721
Souza JS, Reis EA, Godman B, Campbell SM, Meyer JC, Sena LWP, Godói IPD. Users’ Perceptions of Access to and Quality of Unified Health System Services in Brazil: A Cross-Sectional Study and Implications to Healthcare Management Challenges. International Journal of Environmental Research and Public Health. 2024; 21(6):721. https://doi.org/10.3390/ijerph21060721
Chicago/Turabian StyleSouza, Jhoyce S., Edna A. Reis, Brian Godman, Stephen M. Campbell, Johanna C. Meyer, Luann W. P. Sena, and Isabella P. D. Godói. 2024. "Users’ Perceptions of Access to and Quality of Unified Health System Services in Brazil: A Cross-Sectional Study and Implications to Healthcare Management Challenges" International Journal of Environmental Research and Public Health 21, no. 6: 721. https://doi.org/10.3390/ijerph21060721
APA StyleSouza, J. S., Reis, E. A., Godman, B., Campbell, S. M., Meyer, J. C., Sena, L. W. P., & Godói, I. P. D. (2024). Users’ Perceptions of Access to and Quality of Unified Health System Services in Brazil: A Cross-Sectional Study and Implications to Healthcare Management Challenges. International Journal of Environmental Research and Public Health, 21(6), 721. https://doi.org/10.3390/ijerph21060721








