Perceived Public Participation and Health Delivery in Local Government Districts in Uganda
Abstract
:1. Introduction
2. Global Health Governance
3. Decentralised Health Policy
4. Participation Planning and Health System
5. Health Service Delivery Challenges in Sub-Saharan Africa
6. Principal Agent Theory
7. Materials and Methods
7.1. Case Study Approach
7.2. Sampling Procedures and the Participants
7.3. Data Collection Instruments
8. Data Analysis
- Prepared the raw text retrieved from the various government institutions;
- Defined the unit of analysis;
- Developed categories and a coding scheme;
- Validated the coding scheme on sample text;
- Coded the entire text;
- Assessed consistency within the codes;
- Drew conclusions in the codes;
- Finally, we reported the findings.
- Collation of field research notes and transcription of audio interviews.
- Developing data codes (logically inductive) from the field data;
- Transformation of data codes into comprehensive labels or themes;
- Organisation of themes, labels, and categories by identifying and sorting similar phrases, patterns, relationships, and commonalties or disparities;
- The fragmented categories and labels that were sorted and scrutinised into meaningful and manageable transcript to segment patterns, thoughts, and processes; and
- The segmented patterns identified in the transcripts were carefully interpreted juxtaposing them to previous studies, theories, and frameworks to construct some level of generalisations.
9. Findings and Discussion
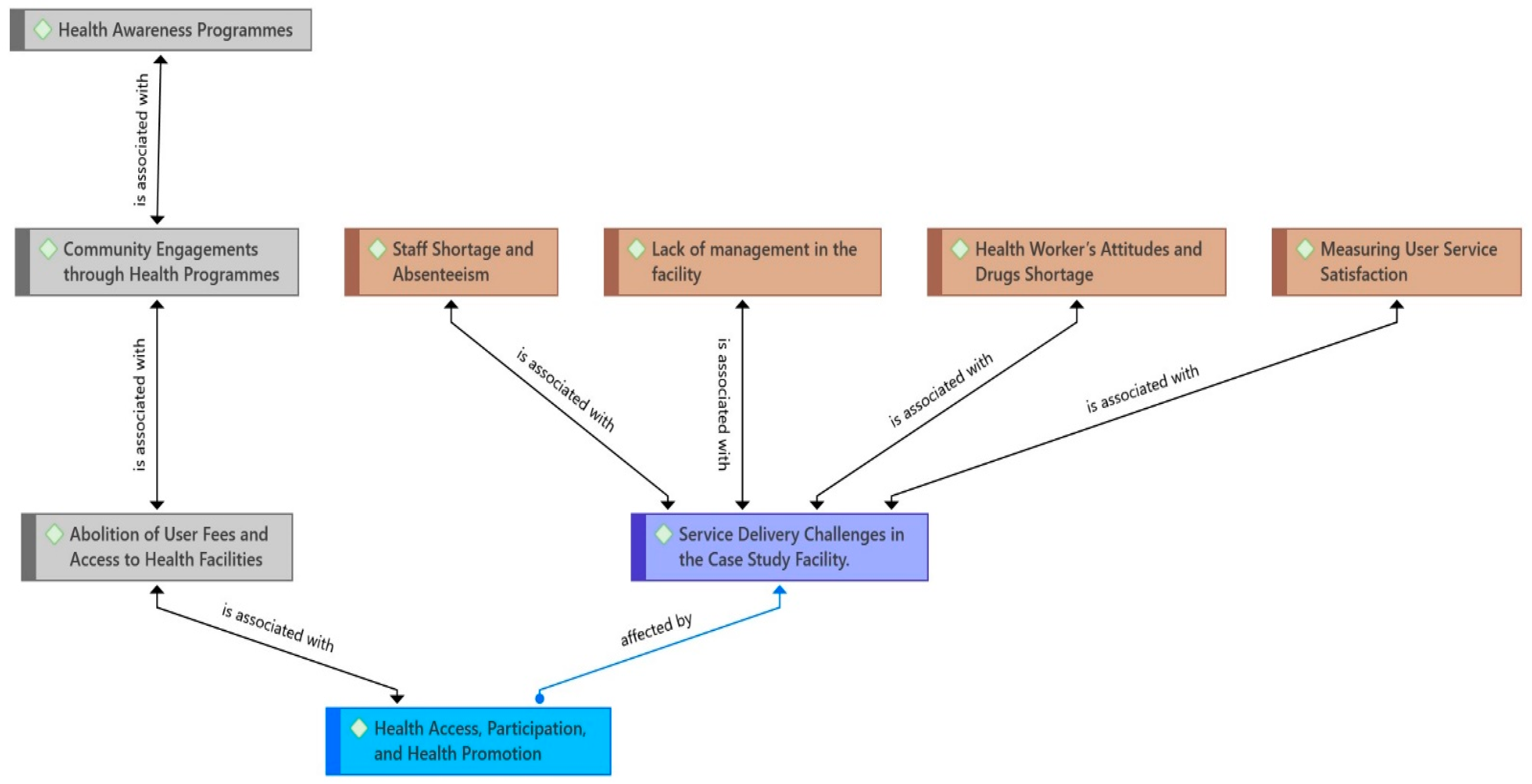
9.1. Perceived Citizen Participation in Health Delivery
It has never happened here, and I don’t think it is possible to happen; they need a long process to do it, which is hard for common people, but even those who would wish to do it get scared because they don’t know whether people will cooperate(HB).
9.2. Health Access, Participation and Health Promotion
9.2.1. Abolition of User Fees and Access to Health Facilities
Previously before the abolition of user fees in private clinics, the services were much better. The finances from the private clinics helped in supporting the day-to-day operation of the hospital. The allocated budget from the central government is not enough and for that reason majority of our colleagues have decided to go(HW).
9.2.2. Community Engagements through Health Programmes
Some people with ways to raise money prefer private clinics. They do not even mind about going to a public hospital. They go to private clinics and hospitals because they believe that public hospital services are bad(HA).
“People who live in remote areas often feel a strong connection to their community, but they may not be aware of their rights or how to ask for better services. That’s why I believe that education is crucial for everyone. People with a good education can speak up for their rights and demand better services”(LC).
9.2.3. Health Awareness Programmes
Participation is because we have non-selective government programmes that include all genders and different groups. Here, we do not have marginalised groups, so if someone doesn’t take part, it means that they, as individuals, are naturally not developmental(LC).
Men lie behind in participation in government programmes due to their unwillingness to participate. There has always been a debate in the council on social problems, where we have found out that men spend most of their time in bars drinking(LC).
9.3. Service Delivery Challenges in the Case Study Facility
9.3.1. Staff Shortage and Absenteeism
The expected percentage of staff in the hospital is 39%, but most of the staff normally don’t report, and even when they do, they come in late and leave early. So, you can imagine, some time back, we had only one midwife who would conduct and administer 90 patients, go to the store to fetch medication, and carry out 12 deliveries daily(HA).
9.3.2. Lack of Management in the Facility
Management is still a challenge here in this hospital. Our medical superintendent is the district health officer, so he sometimes comes once a week or sometimes does not. Supervision is very poor; everyone does as he pleases(HW).
There are so many cases of unfulfilled delivery services; a case in point is a pregnant mother who failed in a health centre here and was referred to Itojo Hospital in critical condition. As the patient approached the medics, was asked for money, and ignored until this female patient finally produced the money(HB).
We cannot control someone who hides and gives the money to the nurse because there are no cameras in the hospital; how can we do that?(HW).
9.3.3. Health Worker’s Attitudes and Drugs Shortage
“There are many cases where people who need medical attention cannot receive it due to problems with delivery services. For example, a pregnant woman who was having difficulty with her pregnancy went to a local health centre for help but was told to go to Itojo Hospital. On arrival, the medical staff asked her for money before they would help her, even though the patient was in very bad labour pain. The patient didn’t have the money at first, but eventually found a way to pay and got the help at lastd”(HB).
9.3.4. Measuring User Service Satisfaction
When you come to this place (hospital) you are not different from someone in a court of law waiting for the death sentence.
So, you can imagine, some time back, we had only one midwife who would conduct and administer 90 patients, go to the store to fetch medication, and carry out 12 deliveries per day(HW).
10. Discussion
11. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Suarez-Herrera, J.C.; Diaz-Castro, L.; Ramirez-Rojas, M.G.; Pelcastre-Villafuerte, B.E. Unpacking participation in healthcare governance: Lessons from two local health councils in Brazil and Spain. Int. J. Health Plann. Manag. 2024, 39, 1097–1112. [Google Scholar] [CrossRef] [PubMed]
- McCollum, R.; Limato, R.; Otiso, L.; Theobald, S.; Taegtmeyer, M. Health system governance following devolution: Comparing experiences of decentralisation in Kenya and Indonesia. BMJ Glob. Health 2018, 3, e000939. [Google Scholar] [CrossRef] [PubMed]
- Masefield, S.C.; Msosa, A.; Grugel, J. Challenges to effective governance in a low income healthcare system: A qualitative study of stakeholder perceptions in Malawi. BMC Health Serv. Res. 2020, 20, 1142. [Google Scholar] [CrossRef] [PubMed]
- Malakoane, B.; Heunis, J.C.; Chikobvu, P.; Kigozi, N.G.; Kruger, W.H. Public health system challenges in the Free State, South Africa: A situation appraisal to inform health system strengthening. BMC Health Serv. Res. 2020, 20, 58. [Google Scholar] [CrossRef]
- Kimaro, H.C.; Sahay, S. Information Technology for Development An institutional perspective on the process of decentralization of health information systems: A case study from Tanzania An Institutional Perspective on the Process of Decentralization of Health Information Systems. Inf. Technol. Dev. 2007, 13, 363–390. [Google Scholar] [CrossRef]
- Wallace, L.J.; Kapiriri, L. Priority setting for maternal, newborn and child health in Uganda: A qualitative study evaluating actual practice. BMC Health Serv. Res. 2019, 19, 465. [Google Scholar] [CrossRef] [PubMed]
- Pfeiffer, J.; Chapman, R.R. Anthropological Perspectives on Structural Adjustment and Public Health. Annu. Rev. Anthropol. 2010, 39, 149–165. [Google Scholar] [CrossRef]
- Yates, R.; Murindwa, G.; Mcpake, B. Health Systems Reforms in Uganda: Processes and Outputs; Tashobya, C.K., Ssengooba, F., Cruz, V.O., Eds.; Health Systems Development Programme, London School of Hygiene & Tropical Medicine: London, UK, 2006. [Google Scholar]
- Mulumba, M.; Ruano, A.L.; Perehudoff, K.; Ooms, G. Decolonizing Health Governance: A Uganda Case Study on the Influence of Political History on Community Participation. Health Hum. Rights J. 2021, 23, 259–271. [Google Scholar]
- Karuga, R.; Kok, M.; Luitjens, M.; Mbindyo, P.; Broerse, J.E.W. Participation in primary health care through community-level health committees in Sub-Saharan Africa: A qualitative synthesis. BMC Public Health 2022, 22, 359. [Google Scholar] [CrossRef]
- World Health Organization. Voice, Agency, Empowerment–Handbook on Social Participation for Universal Health Coverage. 2021. Available online: https://www.who.int/publications/i/item/9789240027794 (accessed on 20 January 2024).
- Lodenstein, E.; Mafuta, E.; Kpatchavi, A.C.; Servais, J.; Dieleman, M.; Broerse, J.E.W.; Barry, A.A.B.; Mambu, T.M.N.; Toonen, J. Social accountability in primary health care in West and Central Africa: Exploring the role of health facility committees. BMC Health Serv. Res. 2017, 17, 403. [Google Scholar] [CrossRef]
- Mccoy, D.C.; Hall, J.A.; Ridge, M. A systematic review of the literature for evidence on health facility committees in low- and middle-income countries. Health Policy Plan. 2012, 27, 449–466. [Google Scholar] [CrossRef] [PubMed]
- Williams, J.J. Social change and community participation: The case of health facilities boards in the Western Cape of South Africa. In Space for Change; Cornwall, A., Coelho, V.S., Eds.; Zed Books: London, UK, 2007; pp. 95–113. [Google Scholar]
- Medard, T.; Yawe, B.L.; Bosco, O.J. Health Care Delivery System in Uganda: A review. Tanzan J. Health Res. 2017, 24, 57–64. [Google Scholar]
- Kiiza, F.; Kayibanda, D.; Tumushabe, P.; Kyohairwe, L.; Atwine, R.; Kajabwangu, R.; Kiconco, R. Frequency and Factors Associated with Hyperglycaemia First Detected during Pregnancy at Itojo General Hospital, South Western Uganda: A Cross-Sectional Study. J. Diabetes Res. 2020, 2020, 4860958. [Google Scholar] [CrossRef] [PubMed]
- Byamukama, P. Financing and health service delivery in Uganda Government Hospitals: A case of Masindi General Hospital. Available online: https://umispace.umi.ac.ug/xmlui/handle/20.500.12305/826 (accessed on 13 June 2024).
- Europe, C. The Pharmacist at the Crossroads of New Health Risks—An Indispensable Partner for their Management: Proceedings, Strasbourg, 20–22 October 1999. In The Pharmacist at the Crossroads of New Health Risks—An Indispensable Partner for Their Management; Council of Europe: Strasbourg, France, 2000; Volume 46, p. 536. [Google Scholar]
- Onzima, B. Public Accountability: Explaining Variation across Local Governments in Uganda. Master’s Thesis, University of Bergen, Bergen, Norway, 2013. [Google Scholar]
- Mooketsane, K.S.; Phirinyane, M.B. Health governance in Sub-Saharan Africa. Glob. Soc. Policy 2015, 15, 345–348. [Google Scholar] [CrossRef] [PubMed]
- Lewis, M.; Pettersson, G. Governance in Health Care Delivery Raising Performance. Policy Research Working Paper WPS5074 5074 Governance in Health Care Delivery Raising Performance; The World Bank Development Economics Department & Human Development Department: Washington, DC, USA, 2009. [Google Scholar]
- Bank, T.W. World Development Indicators 2015; The World Bank: Washington, DC, USA, 2015; Available online: http://elibrary.worldbank.org (accessed on 8 June 2024).
- Oliveira, R.; Santinha, G.; Marques, T.S. The Impacts of Health Decentralization on Equity, Efficiency, and Effectiveness: A Scoping Review. Sustainability 2023, 16, 386. [Google Scholar] [CrossRef]
- Martinussen, P.E.; Rydland, H.T. Is a Decentralised Health Policy Associated With Better Self-rated Health and Health Services Evaluation ? A Comparative Study of European Countries. Int. J. Health Policy Manag. 2021, 10, 55–66. [Google Scholar] [CrossRef] [PubMed]
- Leonardsen, A.-C.L.; Lappegard, Ø.; Garåsen, H.A. Decentralised health services. J. Nor. Med. Assoc. 2017, 137, 1–7. [Google Scholar]
- Boadu, E.S.; Ile, I. The politics of youth participation in social intervention programmes in Ghana: Implications for participatory monitoring and evaluation (PM&E). J. Rev. Glob. Econ. 2018, 7, 913–925. [Google Scholar]
- Nordjo, E.; Boadu, E.S.; Ahenkan, A.; Nordjo, E. Community participation in enterprise development programmes for poverty reduction and sustainable development in Ghana programmes for poverty reduction and sustainable development in Ghana. Commun. Dev. 2023, 54, 1–24. [Google Scholar] [CrossRef]
- De Maeseneer, J.; Li, D.; Palsdottir, B.; Mash, B.; Aarendonk, D.; Stavdal, A.; Moosa, S.; Decat, P.; Kiguli-Malwadde, E.; Ooms, G.; et al. Universal health coverage and primary health care: The 30 by 2030 campaign. Bull. World Health Organ. 2020, 98, 812–814. [Google Scholar] [CrossRef]
- Franchini, M.; Salvatori, M.; Denoth, F.; Molinaro, S.; Pieroni, S. Participation in Low Back Pain Management: It Is Time for the To-Be Scenarios in Digital Public Health. Int. J. Environ. Res. Public Health 2022, 19, 7805. [Google Scholar] [CrossRef] [PubMed]
- Haustein, E.; Lorson, P.C. Co-creation and co-production in municipal risk governance—A case study of citizen participation in a German city. Public Manag. Rev. 2023, 25, 376–403. [Google Scholar] [CrossRef]
- World Health Organization. WHO Constitution on the Right to Health and the Role of the State in Ensuring This Right Is Attainable. The Constitution Affirms the Importance of Informed Opinion and Cooperation of Citizens in Achieving Health Gains. 2006. Available online: https://www.who.int/about/accountability/governance/constitution (accessed on 13 June 2024).
- Dean, H. Social policy and human rights: Re-thinking the engagement. Soc Policy Soc. 2008, 7, 1–12. [Google Scholar] [CrossRef]
- Chancel, L.; Cogneau, D.; Gethin, A.; Myczkowski, A.; Robilliard, A.S. Income inequality in Africa, 1990–2019: Measurement, patterns, determinants. World Dev. 2023, 163, 106162. [Google Scholar] [CrossRef]
- Eusebio, C.; Bakola, M.; Stuckler, D. Commentary How to Achieve Universal Health Coverage: A Case Study of Uganda Using the Political Process Model. Kerman Univ. Med. Sci. 2023, 12, 7307. [Google Scholar] [CrossRef]
- Mukuru, M.; Gorry, J.; Kiwanuka, S.N.; Gibson, L.; Musoke, D. Designed to Fail ? Revisiting Uganda’s Maternal Health Policies to Understand Policy Design Issues Underpinning Missed Targets for Reduction of Maternal Mortality Ratio (MMR): 2000–2015. Int. J. Health Policy Manag. 2022, 11, 2124–2134. [Google Scholar] [CrossRef] [PubMed]
- Oluwafemi, P.; Fajobi, O.; Oluwatobi, T.; Olaniyan, M.E.; Abdulazeez, O.; Blessing, O.; Oko, C. Healthcare systems strengthening in Africa: The call for action to achieve SDG 3. Int. J. Health Plann. Mgmt. 2022, 37, 14–20. [Google Scholar]
- Batley, R.; Mcloughlin, C. The Politics of Public Services: A Service Characteristics Approach. World Dev. 2015, 74, 275–285. [Google Scholar] [CrossRef]
- Golooba-mutebi, F. When Popular Participation Won’t Improve Service Provision: Primary Health Care in Uganda. Dev. Policy Rev. 2005, 23, 165–182. [Google Scholar] [CrossRef]
- Devarajan, S.; Widlund, I. The Politics of Service Delivery in Democracies: Better Access for the Poor; Expert Group on Development Issues, Ministry of Foreign Affairs: Stockholm, Sweden, 2007; Volume 1, pp. 1–178.
- Pratt, J.W. Principals and Agents: The Structure of Business; Harvard Business School Press: Boston, MA, USA, 1985; pp. 1–10. [Google Scholar]
- Hedge, D.M.; Scicchitano, M.J.; Metz, P. The Principal-Agent Model and Regulatory Federalism. West Polit. Q. 1991, 44, 1055–1080. [Google Scholar] [CrossRef]
- Kumar, K. Conducting Key Informant Interviews in Developing Countries (p. 1). Washington DC: Agency for International Development. [Internet]. Vol. 1, NBER Working Paper Seriesking Paper Series. 1989. Available online: https://www.unhcr.org/publications/manuals/4d9352319/unhcr-protection-training-manual-european-border-entry-officials-2-legal.html?query=excom (accessed on 13 June 2024).
- Mariotto, F.L.; Zanni, P.P.; Salati, G.H.; de Moraes, M. What is the use of a single-case study in management research? Rev. Adm. Empres 2014, 54, 358–369. [Google Scholar] [CrossRef]
- Wiersma, W. Research Methods in Education: An Introduction, 7th ed.; Ally & Bacon: Boston, MA, USA, 2000. [Google Scholar]
- Patton, M.Q. Qualitative Evaluation and Research Methods, 3rd ed.; Sage Publications: Thousand Oaks, CA, USA, 2002. [Google Scholar]
- Bowen, G. Document Analysis as a Qualitative Research Method. Qual. Res. J. 2009, 9, 27–40. [Google Scholar] [CrossRef]
- Bossert, T. digitalization and rural health delivery in ghana: Opportunities, challenges, and implications 1. introduction digitalization has the potential to revolutionize rural health delivery in ghana by improving access, efficiency, and quality of healthcare serv. Soc. Sci. Med. 1998, 47, 1513–1527. [Google Scholar] [CrossRef] [PubMed]
- Clarke, V.; Braun, V. Thematic analysis. J. Posit. Psychol. 2017, 9760, 297–298. [Google Scholar] [CrossRef]
- Lincoln, Y.S.; Guba, E.G. But Is It Rigorous? Authenticity in Trustworthiness and Naturalistic Evaluation. New Dir. Progr. Eval. 1986, 30, 73–84. [Google Scholar] [CrossRef]
- Kusnanto, H. Principal-Agent and Stakeholder Approaches in Decentralized Health Care: The Indonesian Case; Reaserch Paper 198; Takemi Program, Harvard School of Public Health: Boston, CA, USA, 2001. [Google Scholar]
- Donaldson, S.I.; Lipsey, M.W. Roles for theory in evaluation practice. In Handbook of Evaluation; Shaw, I., Greene, J., Mark, M., Eds.; Sage: Thousand Oaks, CA, USA, 2001; pp. 1–31. [Google Scholar]
- Laffont, J.J.; Martimort, D. The Theory of Incentives I: The Principal-Agent Model; Princeton University Press: Princeton, NJ, USA, 2001; pp. 1–381. [Google Scholar]
- Lambert, H.; Mckevitt, C. Anthropology in health research: From qualitative methods to multidisciplinarity. BML 2002, 325, 210–213. [Google Scholar] [CrossRef] [PubMed]
- Bailey, A.; Mujune, V. Multi—Level change strategies for health: Learning from people—Centered advocacy in Uganda. Int. J. Equity Health 2024, 21, 143. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Wildemuth, B. Qualitative Analy sis of Content. In Applications of Social Research Methods to Questions in Information and Library Science, 2nd ed.; Wildemuth, B.M., Ed.; Libraries Unlimited: Santa Barbara, CA, USA, 2017; pp. 318–330. [Google Scholar]
- Berg, B.L. Qualitative Research Methods for the Social Sciences, 4th ed.; Allyn and Bacon: Boston, Poland, 2001. [Google Scholar]
- Bradley, J. Methodological Issues and Practices in Qualitative. In Symposium on Qualitative Research: Theory, Methods, and Applications; The University of Chicago Press: Chicago, IL, USA, 1993; Volume 63, pp. 431–449. Available online: https://www.jstor.org/stable/4308865 (accessed on 13 June 2024).
- Nabyonga-orem, J.; Karamagi, H.; Atuyambe, L.; Bagenda, F.; Okuonzi, S.A.; Walker, O. Maintaining quality of health services after abolition of user fees: A Uganda case study. BMC Health Serv. Res. 2008, 8, 102. [Google Scholar] [CrossRef]
| Document Type | Year | Title | Institution | Document Origin/Source/Author |
|---|---|---|---|---|
| Policy document report | 2020 | Policy Brief on Revitalising Civil Servants Performance for Sustainable Development | Cabinet secretariate | Ministry of Health Library. library.health.go.ug |
| Policy document report | 2021 | National Emergency Medical Services Policy | Ministry of Health | Ministry of Health Library. library.health.go.ug |
| Policy research series | 2011 | Local government councils’ performance and public service delivery in Uganda | Advocates Coalition for Development and Environment (ACODE) * | Advocates Coalition for Development and Environment (www.acode-u.org, accessed on 13 Jan 2024) |
| Policy document | 2018 | Community Health Extension Workers National Strategy (2018–2022) | Ministry of health | Ministry of Health Library. library.health.go.ug |
| News Brief | 2022 | Ntungamo RDC calls for improved monitoring of health services | Ntungamo District Local Government | District Website www.ntungamo.go.ug (accessed on 13 Jan 2024) |
| News Brief | 2023 | Ntungamo deputy RDC cautions health workers against absenteeism. | Ntungamo District Local Government | District Website |
| News Brief | 2023 | Ntungamo gets 1.4 billion health facility | Ntungamo District Local Government | District Website |
| News Brief | 2024 | locals tipped on utilising government health facilities | Ntungamo District Local Government | District Website |
| News Brief | 2024 | Ntungamo RDC advocates for increased HIV awareness | Ntungamo District Local Government | District Website |
| News Brief | 2021 | civil servants cautioned on absenteeism | Ntungamo District Local Government | District Website |
| News Brief | 2021 | Authorities call for collective efforts in the fight against HIV/aids | Ntungamo District Local Government | District Website |
| News Brief | 2018 | Ntungamo leaders calls for calm amidst complaints over unpaid salaries | Ntungamo District Local Government | District Website |
| Book: Guidelines | 2018 | Guidelines for Regional Referral Hospital Management Boards 2018 | Uganda ministry of health | Ministry of Health Library. library.health.go.ug |
| Book: Guidelines | 2019 | Guidelines for General Hospital Management Boards 2019 | Uganda ministry of health | Ministry of Health Library. library.health.go.ug |
| Report | 2012 | Report on the State of Regional Referral Hospitals in Uganda Towards the Realisation of the Right to Health | Uganda ministry of health | Ministry of Health Library. library.health.go.ug |
| Book: Guidelines | 2016 | Guidelines for Community Health Departments for hospitals | Uganda ministry of health | Ministry of Health Library. library.health.go.ug |
| Book: regional referral hospitals | 2003 | Guidelines on Hospital management boards for referral hospitals | Uganda ministry of health | Ministry of Health Library. library.health.go.ug |
| Book: Guidelines | 2010 | Guidelines on hospital management committee for district hospitals | Uganda ministry of health | Ministry of Health Library. library.health.go.ug |
| Book: Guidelines | 2021 | Guidelines for the Decentralisation of the Uganda Medical Board | Uganda ministry of health | Ministry of Health Library. library.health.go.ug |
| Governance report | 2022 | Special Report on New threats to human security in the Anthropocene 2022 | UNDP | Ministry of Health Library. library.health.go.ug |
| Variable | Description | Number of Respondents |
|---|---|---|
| HW | Health workers | 10 |
| HA | Health administrators | 3 |
| HB | Health beneficiaries (Patients/Residents) | 45 |
| LC | Local councillors | 5 |
| HCM | Health committee members | 3 |
| Total | 66 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mukiga, A.K.; Boadu, E.S.; Edson, T. Perceived Public Participation and Health Delivery in Local Government Districts in Uganda. Int. J. Environ. Res. Public Health 2024, 21, 820. https://doi.org/10.3390/ijerph21070820
Mukiga AK, Boadu ES, Edson T. Perceived Public Participation and Health Delivery in Local Government Districts in Uganda. International Journal of Environmental Research and Public Health. 2024; 21(7):820. https://doi.org/10.3390/ijerph21070820
Chicago/Turabian StyleMukiga, Alex Kihehere, Evans Sakyi Boadu, and Tayebwa Edson. 2024. "Perceived Public Participation and Health Delivery in Local Government Districts in Uganda" International Journal of Environmental Research and Public Health 21, no. 7: 820. https://doi.org/10.3390/ijerph21070820





