Refined Feasibility Testing of an 8-Week Sport and Physical Activity Intervention in a Rural Middle School
Abstract
:1. Introduction
2. Materials and Methods
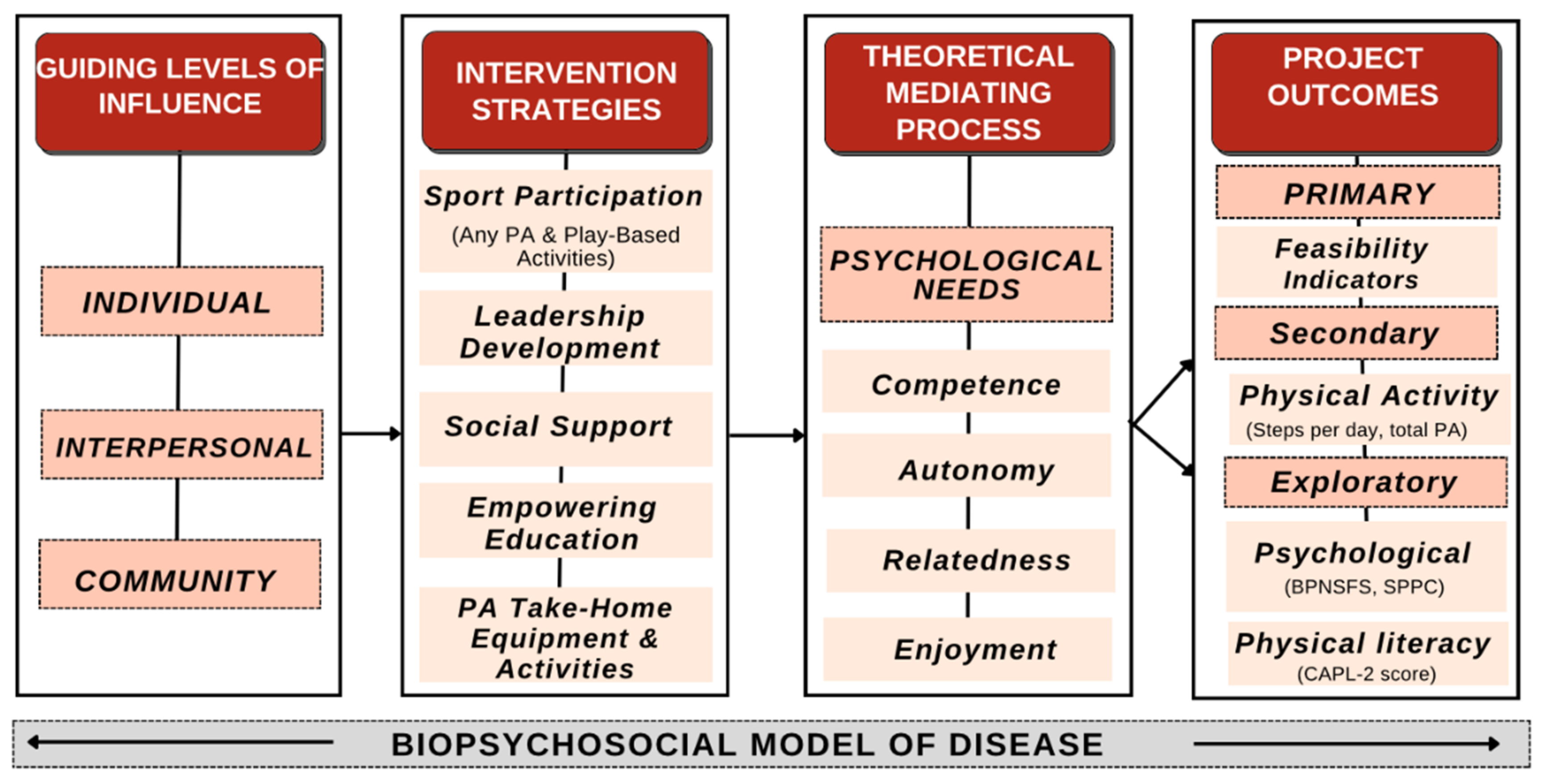
2.1. Conceptual Framework
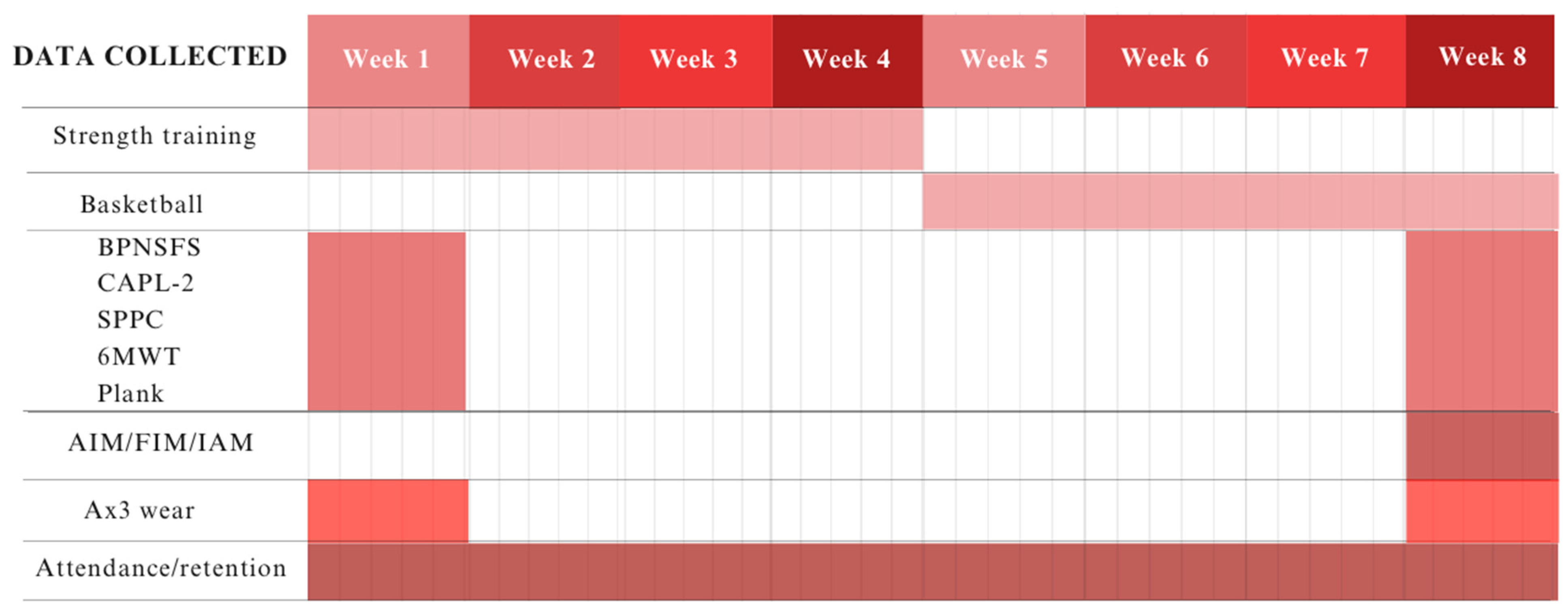
2.2. Design
2.3. Intervention
2.4. Sample Size and Sample
2.5. Measures
2.5.1. Trial-Related Feasibility Indicators
2.5.2. Intervention-Related Feasibility Indicators
2.5.3. Physiological Assessment
2.5.4. Psychological Outcomes
2.6. Procedure
2.7. Data Analysis
3. Results
3.1. Trial-Related Feasibility Indicators
3.2. Intervention-Related Feasibility Indicators
3.3. Cost
3.4. Physiological and Psychological Outcomes
3.5. Physiological and Psychological Relationships
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| CVD | cardiovascular disease |
| PA | physical activity |
| ORBIT | Obesity-Related Behavioral Intervention Trials |
| AIM | Acceptability of Intervention Measure |
| IAM | Intervention Appropriateness Measure |
| FIM | Feasibility of Intervention Measure |
| BPNSFS | Basic Psychological Needs Satisfaction and Frustration Scale |
| CAPL-2 | Canadian Assessment of Physical Literacy (version 2) |
| SPPC | Self-Perception Profile for Children |
| 6MWT | 6 min walk test |
References
- Meyer, U.; Schindler, C.; Zahner, L.; Ernst, D.; Hebestreit, H.; van Mechelen, W.; Rocca, H.-P.B.-L.; Probst-Hensch, N.; Puder, J.J.; Kriemler, S. Long-Term Effect of a School-Based Physical Activity Program (KISS) on Fitness and Adiposity in Children: A Cluster-Randomized Controlled Trial. PLoS ONE 2014, 9, e87929. [Google Scholar] [CrossRef] [PubMed]
- Eloranta, A.-M.; Sallinen, T.; Viitasalo, A.; Lintu, N.; Väistö, J.; Jalkanen, H.; Tompuri, T.T.; Soininen, S.; Haapala, E.A.; Kiiskinen, S.; et al. The effects of a 2-year physical activity and dietary intervention on plasma lipid concentrations in children: The PANIC Study. Eur. J. Nutr. 2021, 60, 425–434. [Google Scholar] [CrossRef]
- Dobbins, M.; Husson, H.; DeCorby, K.; LaRocca, R.L. School-based physical activity programs for promoting physical activity and fitness in children and adolescents aged 6 to 18. Cochrane Database Syst. Rev. 2013, 2013, CD007651. [Google Scholar] [CrossRef] [PubMed]
- Tsao, C.W.; Aday, A.W.; Almarzooq, Z.I.; Alonso, A.; Beaton, A.Z.; Bittencourt, M.S.; Boehme, A.K.; Buxton, A.E.; Carson, A.P.; Commodore-Mensah, Y.; et al. Heart disease and stroke statistics—2022 update: A report from the American Heart Association. Circulation 2022, 145, E153–E639. [Google Scholar] [CrossRef] [PubMed]
- U.S. Department of Health and Human Services. Physical Activity Guidelines for Americans; U.S. Department of Health and Human Services: Washington, DC, USA, 2023.
- Chaput, J.-P.; Willumsen, J.; Bull, F.; Chou, R.; Ekelund, U.; Firth, J.; Jago, R.; Ortega, F.B.; Katzmarzyk, P.T. 2020 WHO guidelines on physical activity and sedentary behaviour for children and adolescents aged 5–17 years: Summary of the evidence. Int. J. Behav. Nutr. Phys. Act. 2020, 17, 141. [Google Scholar] [CrossRef] [PubMed]
- Saunders, T.J.; Gray, C.E.; Poitras, V.J.; Chaput, J.-P.; Janssen, I.; Katzmarzyk, P.T.; Olds, T.; Gorber, S.C.; Kho, M.E.; Sampson, M.; et al. Combinations of physical activity, sedentary behaviour and sleep: Relationships with health indicators in school-aged children and youth. Appl. Physiol. Nutr. Metab. 2016, 41, S283–S293. [Google Scholar] [CrossRef] [PubMed]
- Western, M.J.; Armstrong, M.E.G.; Islam, I.; Morgan, K.; Jones, U.F.; Kelson, M.J. The effectiveness of digital interventions for increasing physical activity in individuals of low socioeconomic status: A systematic review and meta-analysis. Int. J. Behav. Nutr. Phys. Act. 2021, 18, 148. [Google Scholar] [CrossRef] [PubMed]
- Hesketh, K.R.; Lakshman, R.; van Sluijs, E.M.F. Barriers and facilitators to young children’s physical activity and sedentary behaviour: A systematic review and synthesis of qualitative literature. Obes. Rev. 2017, 18, 987–1017. [Google Scholar] [CrossRef]
- Clayton, P.; Connelly, J.; Ellington, M.; Rojas, V.; Lorenzo, Y.; Trak-Fellermeier, M.A.; Palacios, C. Facilitators and barriers of children’s participation in nutrition, physical activity, and obesity interventions: A systematic review. Obes. Rev. 2021, 22, e13335. [Google Scholar] [CrossRef]
- Omura, J.D.; Carlson, S.A.; Brown, D.R.; Hopkins, D.P.; Kraus, W.E.; Staffileno, B.A.; Thomas, R.J.; Lobelo, F.; Fulton, J.E. Built environment approaches to increase physical activity: A science advisory from the American Heart Association. Circulation 2020, 142, E160–E166. [Google Scholar] [CrossRef]
- Pedersen, M.R.L.; Bredahl, T.V.G.; Elmose-Østerlund, K.; Hansen, A.F. Motives and barriers related to physical activity within different types of built environments: Implications for health promotion. Int. J. Environ. Res. Public Health 2022, 19, 9000. [Google Scholar] [CrossRef] [PubMed]
- Hu, D.; Zhou, S.; Crowley-McHattan, Z.J.; Liu, Z. Factors that influence participation in physical activity in school-aged children and adolescents: A systematic review from the social ecological model perspective. Int. J. Environ. Res. Public Health 2021, 18, 3147. [Google Scholar] [CrossRef] [PubMed]
- Barnes, J.; Altimate, E.; Farrell, P.; Brown, R.; Burnett, C., III; Gamble, L.; Davis, J. Creating and sustaining authentic partnerships with community in a systemic model. J. High Educ. Outreach. Engagem. 2009, 14, 15–29. [Google Scholar]
- Whitley, M.A.; Massey, W.V.; Camiré, M.; Boutet, M.; Borbee, A. Sport-based youth development interventions in the United States: A systematic review. BMC Public Health 2019, 19, 89. [Google Scholar] [CrossRef] [PubMed]
- Perkins, D.F.; Noam, G.G. Characteristics of sports-based youth development programs. New Dir. Youth Dev. 2007, 75–84, 8–9. [Google Scholar] [CrossRef]
- Kwon, S.; Welch, S.; Mason, M. Physical education environment and student physical activity levels in low-income communities. BMC Public Health 2020, 20, 147. [Google Scholar] [CrossRef] [PubMed]
- Bevans, K.B.; Fitzpatrick, L.-A.; Sanchez, B.M.; Riley, A.W.; Forrest, C. Physical education resources, class management, and student physical activity levels: A structure-process-outcome approach to evaluating physical education effectiveness. J. Sch. Health 2010, 80, 573–580. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. School Health Guidelines to Promote Healthy Eating and Physical Activity; U.S. Department of Health and Human Services, Centers for Disease Control and Prevention: Atlanta, GA, USA, 2011.
- Buja, A.; Rabensteiner, A.; Sperotto, M.; Grotto, G.; Bertoncello, C.; Cocchio, S.; Baldovin, T.; Contu, P.; Lorini, C.; Baldo, V. Health literacy and physical activity: A systematic review. J. Phys. Act. Health 2020, 17, 1259–1274. [Google Scholar] [CrossRef]
- Deci, E.L.; Ryan, R.M. Intrinsic Motivation and Self-Determination in Human Behavior; Plenum Press: New York, NY, USA, 1985. [Google Scholar] [CrossRef]
- Owen, K.B.; Smith, J.; Lubans, D.R.; Ng, J.Y.Y.; Lonsdale, C. Self-determined motivation and physical activity in children and adolescents: A systematic review and meta-analysis. Prev. Med. 2014, 67, 270–279. [Google Scholar] [CrossRef]
- Watkins, J.M.; Greeven, S.J.; Heeter, K.N.; Brunnemer, J.E.; Otile, J.; Solá, P.A.F.; Dutta, S.; Hobson, J.M.; Evanovich, J.M.; Coble, C.J.; et al. Human-centered participatory co-design with children and adults for a prototype lifestyle intervention and implementation strategy in a rural middle school. BMC Public Health 2024, 24, 845. [Google Scholar] [CrossRef]
- John, J.M.; Haug, V.; Thiel, A. Physical activity behavior from a transdisciplinary biopsychosocial perspective: A scoping review. Sports Med. Open 2020, 6, 49. [Google Scholar] [CrossRef] [PubMed]
- Ryan, R.M.; Deci, E.L. Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. Am. Psychol. 2000, 55, 68–78. [Google Scholar] [CrossRef] [PubMed]
- Olafsen, A.H.; Deci, E.L.; Halvari, H. Basic psychological needs and work motivation: A longitudinal test of directionality. Motiv. Emot. 2018, 42, 178–189. [Google Scholar] [CrossRef]
- Goode, A.P.; Hall, K.S.; Batch, B.C.; Huffman, K.M.; Hastings, S.N.; Allen, K.D.; Shaw, R.J.; Kanach, F.A.; McDuffie, J.R.; Kosinski, A.S.; et al. The impact of interventions that integrate accelerometers on physical activity and weight loss: A systematic review. Ann. Behav. Med. 2017, 51, 79–93. [Google Scholar] [CrossRef]
- Cerin, E.; Cain, K.L.; Oyeyemi, A.L.; Owen, N.; Conway, T.L.; Cochrane, T.; VAN Dyck, D.; Schipperijn, J.; Mitáš, J.; Toftager, M.; et al. Correlates of agreement between accelerometry and self-reported physical activity. Med. Sci. Sports Exerc. 2016, 48, 1075–1084. [Google Scholar] [CrossRef] [PubMed]
- Bean, C.; McFadden, T.; Fortier, M.; Forneris, T. Understanding the relationships between programme quality, psychological needs satisfaction, and mental well-being in competitive youth sport. Int. J. Sport Exerc. Psychol. 2021, 19, 246–264. [Google Scholar] [CrossRef]
- National Institute on Minority Health and Health Disparities. NIMHD Research Framework; National Institute on Minority Health and Health Disparities: Bethesda, MD, USA, 2017.
- Czajkowski, S.M.; Powell, L.H.; Adler, N.; Naar-King, S.; Reynolds, K.D.; Hunter, C.M.; Laraia, B.; Olster, D.H.; Perna, F.M.; Peterson, J.C.; et al. From ideas to efficacy: The ORBIT model for developing behavioral treatments for chronic diseases. Health Psychol. 2015, 34, 971–982. [Google Scholar] [CrossRef]
- Beets, M.W.; von Klinggraeff, L.; Weaver, R.G.; Armstrong, B.; Burkart, S. Small studies, big decisions: The role of pilot/feasibility studies in incremental science and premature scale-up of behavioral interventions. Pilot Feasibility Stud. 2021, 7, 173. [Google Scholar] [CrossRef] [PubMed]
- Pfledderer, C.D.; von Klinggraeff, L.; Burkart, S.; Wolfenden, L.; Ioannidis, J.P.A.; Beets, M.W. Feasibility indicators in obesity-related behavioral intervention preliminary studies: A historical scoping review. Pilot Feasibility Stud. 2023, 9, 46. [Google Scholar] [CrossRef]
- Curran, G.M.; Bauer, M.; Mittman, B.; Pyne, J.M.; Stetler, C. Effectiveness-implementation hybrid designs. Med. Care 2012, 50, 217–226. [Google Scholar] [CrossRef]
- Faul, F.; Erdfelder, E.; Buchner, A.; Lang, A.-G. Statistical power analyses using G*Power 3.1: Tests for correlation and regression analyses. Behav. Res. Methods 2009, 41, 1149–1160. [Google Scholar] [CrossRef] [PubMed]
- Teresi, J.A.; Yu, X.; Stewart, A.L.; Hays, R.D. Guidelines for designing and evaluating feasibility pilot studies. Med. Care 2022, 60, 95–103. [Google Scholar] [CrossRef] [PubMed]
- Hedayatrad, L.; Stewart, T.; Duncan, S. Concurrent validity of ActiGraph GT3X+ and Axivity AX3 accelerometers for estimating physical activity and sedentary behavior. J. Meas. Phys. Behav. 2021, 4, 1–8. [Google Scholar] [CrossRef]
- Brønd, J.C.; Grøntved, A.; Andersen, L.B.; Arvidsson, D.; Olesen, L.G. Simple method for the objective activity type assessment with preschoolers, children and adolescents. Children 2020, 7, 72. [Google Scholar] [CrossRef] [PubMed]
- Stewart, T.; Narayanan, A.; Hedayatrad, L.; Neville, J.; Mackay, L.; Duncan, S. A dual-accelerometer system for classifying physical activity in children and adults. Med. Sci. Sports Exerc. 2018, 50, 2595–2602. [Google Scholar] [CrossRef] [PubMed]
- Feng, Y.; Wong, C.K.; Janeja, V.; Kuber, R.; Mentis, H.M. Comparison of tri-axial accelerometers step-count accuracy in slow walking conditions. Gait Posture 2017, 53, 11–16. [Google Scholar] [CrossRef] [PubMed]
- ATS Statement: Guidelines for the six-minute walk test. Am. J. Respir. Crit. Care Med. 2002, 166, 111–117. [CrossRef] [PubMed]
- Šakan, D. Validation of the Basic Psychological Need Satisfaction and Frustration Scale (BPNSFS). Eur. J. Psychol. 2022, 41, 2227–2240. [Google Scholar]
- Liga, F.; Ingoglia, S.; Cuzzocrea, F.; Inguglia, C.; Costa, S.; Lo Coco, A.; Larcan, R. The Basic Psychological Need Satisfaction and Frustration Scale: Construct and Predictive Validity in the Italian Context. J. Personal. Assess. 2020, 102, 102–112. [Google Scholar] [CrossRef]
- Harter, S. Self-Perception Profile for Children: Manual and Questionnaires; University of Denver, Department of Psychology: Denver, CO, USA, 2012. [Google Scholar]
- Ferro, M.A.; Tang, J. Psychometric Properties of the Self-Perception Profile for Children in Children with Chronic Illness. J. Can. Acad. Child Adolesc. Psychiatry 2017, 26, 119–124. [Google Scholar]
- Warburton, D.E.R.; Jamnik, V.K.; Bredin, S.S.D.; Gledhill, N. International launch of the PAR-Q+ and ePARmed-X+. Health Fit. J. Can. 2011, 4, 38. [Google Scholar]
- RStudio Team. RStudio: Integrated Development for R; RStudio, PBC: Boston, MA, USA, 2024. [Google Scholar]
- Migueles, J.H.; Rowlands, A.V.; Huber, F.; Sabia, S.; van Hees, V.T. GGIR: A Research Community–Driven Open Source R Package for Generating Physical Activity and Sleep Outcomes From Multi-Day Raw Accelerometer Data. J. Meas. Phys. Behav. 2019, 2, 188–196. [Google Scholar] [CrossRef]
- Watkins, J.M.; Brunnemer, J.E.; Heeter, K.N.; Medellin, A.M.; Churchill, W.C.; Goss, J.M.; Hobson, J.M.; Werner, N.E.; Weaver, R.G.; Kercher, V.M.M.; et al. Evaluating the feasibility and acceptability of a co-designed physical activity intervention for rural middle schoolers: A pilot study. BMC Public Health 2024, 24, 1830. [Google Scholar] [CrossRef]
- Gorely, T.; Nevill, M.E.; Morris, J.G.; Stensel, D.J.; Nevill, A. Effect of a school-based intervention to promote healthy lifestyles in 7–11 year old children. Int. J. Behav. Nutr. Phys. Act. 2009, 6, 5. [Google Scholar] [CrossRef]
- Vander Ploeg, K.A.; Maximova, K.; McGavock, J.; Davis, W.; Veugelers, P. Do school-based physical activity interventions increase or reduce inequalities in health? Soc. Sci. Med. 2014, 112, 80–87. [Google Scholar] [CrossRef] [PubMed]
- Schüller, I.; Demetriou, Y. Physical activity interventions promoting social competence at school: A systematic review. Educ. Res. Rev. 2018, 25, 39–55. [Google Scholar] [CrossRef]
- Shang, Y.; Chen, S.-P.; Liu, L.-P. The role of peer relationships and flow experience in the relationship between physical exercise and social anxiety in middle school students. BMC Psychol. 2023, 11, 428. [Google Scholar] [CrossRef]
- Gould, D.; Voelker, D.K. Enhancing Youth Leadership Through Sport and Physical Education. J. Phys. Educ. Recreat. Danc. 2012, 83, 38–41. [Google Scholar] [CrossRef]
- Weiss, M.; Kipp, L.; Bolter, N. Training for Life: Optimizing Positive Youth Development Through Sport and Physical Activity. In The Oxford Handbook of Sport and Performance Psychology; Oxford University Press: Oxford, UK, 2012. [Google Scholar]
- Majed, E.; Ruiz, Y.; Amireault, S.; Reed, J.B.; Snyder, F.J.; McDonough, M.H.; Blankenship, B. Examining Positive Youth Development Interventions with a Physical Activity Component to Address Bullying Among Pre- and Early Adolescents: A Critical Review of the Literature. J. Early Adolesc. 2022, 42, 389–413. [Google Scholar] [CrossRef]
- Reddon, H.; Meyre, D.; Cairney, J. Physical Activity and Global Self-worth in a Longitudinal Study of Children. Med. Sci. Sports Exerc. 2017, 49, 1606–1613. [Google Scholar] [CrossRef]
- Haugen, T.; Säfvenbom, R.; Ommundsen, Y. Physical activity and global self-worth: The role of physical self-esteem indices and gender. Ment. Health Phys. Act. 2011, 4, 49–56. [Google Scholar] [CrossRef]
- Project Play. Youth Sports Playbook; Aspen Institute: Washington, DC, USA, 2024. [Google Scholar]
- Kercher, K.A.; Steinfeldt, J.A.; Rettke, D.J.; Zuidema, T.R.; Walker, M.J.; Kercher, V.M.M.; Silveyra, P.; Seo, D.-C.; Macy, J.T.; Hulvershorn, L.A.; et al. Association Between Head Impact Exposure, Psychological Needs, and Indicators of Mental Health Among U.S. High School Tackle Football Players. J. Adolesc. Health 2023, 72, 502–509. [Google Scholar] [CrossRef] [PubMed]
| Test Group | Control Group | |
|---|---|---|
| Gender (n) | ||
| Female | 14 | 5 |
| Male | 10 | 6 |
| Age (M, SD) | ||
| Female | 12.4 (0.5) | 12.9 (0.3) |
| Male | 12.7 (0.4) | 12.7 (0.3) |
| CAPL-2 Score (M, SD) | ||
| Female | 4.18 (2.08) | 6.45 (3.69) |
| Male | 6.09 (1.75) | 5.88 (2.97) |
| Variable | Test Mean | Test Median | Test SD | Control Mean | Control Median | Control SD |
|---|---|---|---|---|---|---|
| FIM | 17.42 | 18 | 2.63 | 16.63 | 17 | 4.12 |
| AIM | 16.85 | 17 | 3.69 | 17.72 | 19 | 2.28 |
| IAM | 17.23 | 18 | 2.62 | 16.09 | 20 | 5.59 |
| Variable | Test Pre-Post Mean Difference | Test p-Value | Control Pre-Post Mean Difference | Control p-Value |
|---|---|---|---|---|
| Plank | −1.44 | 0.891 | 15.31 | 0.395 |
| 6MWT | −14.71 | 0.467 | −26.55 | 0.168 |
| Resting HR | −3.17 | 0.407 | 3.27 | 0.371 |
| Autonomy | 2.78 | 0.023 * | 2.00 | 0.300 |
| Competence | −0.58 | 0.670 | −0.73 | 0.757 |
| Relatedness | 0.90 | 0.536 | 1.55 | 0.516 |
| Athletic Competence | −1.14 | 0.130 | −0.82 | 0.426 |
| Social Competence | 2.48 | 0.005 * | −1.00 | 0.542 |
| Global Self-Worth | 1.38 | 0.028 * | −1.73 | 0.132 |
| CAPL-2 | 0.816 | 0.123 | 0.27 | 0.412 |
| Variables | Control Mean (SD) | Test Mean (SD) |
|---|---|---|
| Pre-Intervention | ||
| Avg. Daily Steps | 2071.50 (2172.79) | 4213.71 (4954.87) |
| Total PA (min) | 127.41 (72.58) | 181.011 (122.391) |
| Post-Intervention | ||
| Avg. Daily Steps | 2681.05 (2739.53) | 5898.19 (8807.48) |
| Total PA (min) | 294.27 (201.52) | 324.23 (223.11) |
| Variables and Time | t-Score | 95% CI | p-Value |
|---|---|---|---|
| Control vs. Test | |||
| Pre-Intervention | |||
| Avg. Daily Steps | 1.612 | [−4099.308, 3409.243] | 0.118 |
| Total PA (min) | 1.637 | [−20.499, 128.327] | 0.115 |
| Post-Intervention | |||
| Avg. Daily Steps | 1.35 | [−1333.400, 5384.334] | 0.192 |
| Total PA (min) | 0.741 | [−153.987, 212.575] | 0.741 |
| Test Group | |||
| Avg. Daily Steps | 2.484 | [−1017.728, 7814.223] | 0.025 |
| Total PA (min) | 2.293 | [−272.607, 130.840] | 0.031 |
| Control Group | |||
| Avg. Daily Steps | 2.36 | [−4582.974, 3674.117] | 0.041 |
| Total PA (min) | 2.702 | [−326.006, 123.049] | 0.026 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Watkins, J.M.; Goss, J.M.; Major, M.G.; Kwaiser, M.M.; Medellin, A.M.; Hobson, J.M.; Martinez Kercher, V.M.; Kercher, K.A. Refined Feasibility Testing of an 8-Week Sport and Physical Activity Intervention in a Rural Middle School. Int. J. Environ. Res. Public Health 2024, 21, 913. https://doi.org/10.3390/ijerph21070913
Watkins JM, Goss JM, Major MG, Kwaiser MM, Medellin AM, Hobson JM, Martinez Kercher VM, Kercher KA. Refined Feasibility Testing of an 8-Week Sport and Physical Activity Intervention in a Rural Middle School. International Journal of Environmental Research and Public Health. 2024; 21(7):913. https://doi.org/10.3390/ijerph21070913
Chicago/Turabian StyleWatkins, Janette M., Janelle M. Goss, McKenna G. Major, Megan M. Kwaiser, Andrew M. Medellin, James M. Hobson, Vanessa M. Martinez Kercher, and Kyle A. Kercher. 2024. "Refined Feasibility Testing of an 8-Week Sport and Physical Activity Intervention in a Rural Middle School" International Journal of Environmental Research and Public Health 21, no. 7: 913. https://doi.org/10.3390/ijerph21070913
APA StyleWatkins, J. M., Goss, J. M., Major, M. G., Kwaiser, M. M., Medellin, A. M., Hobson, J. M., Martinez Kercher, V. M., & Kercher, K. A. (2024). Refined Feasibility Testing of an 8-Week Sport and Physical Activity Intervention in a Rural Middle School. International Journal of Environmental Research and Public Health, 21(7), 913. https://doi.org/10.3390/ijerph21070913






