The Effect of Inspiratory Muscle Training on Health-Related Fitness in College Students
Abstract
:1. Introduction
2. Materials and Method
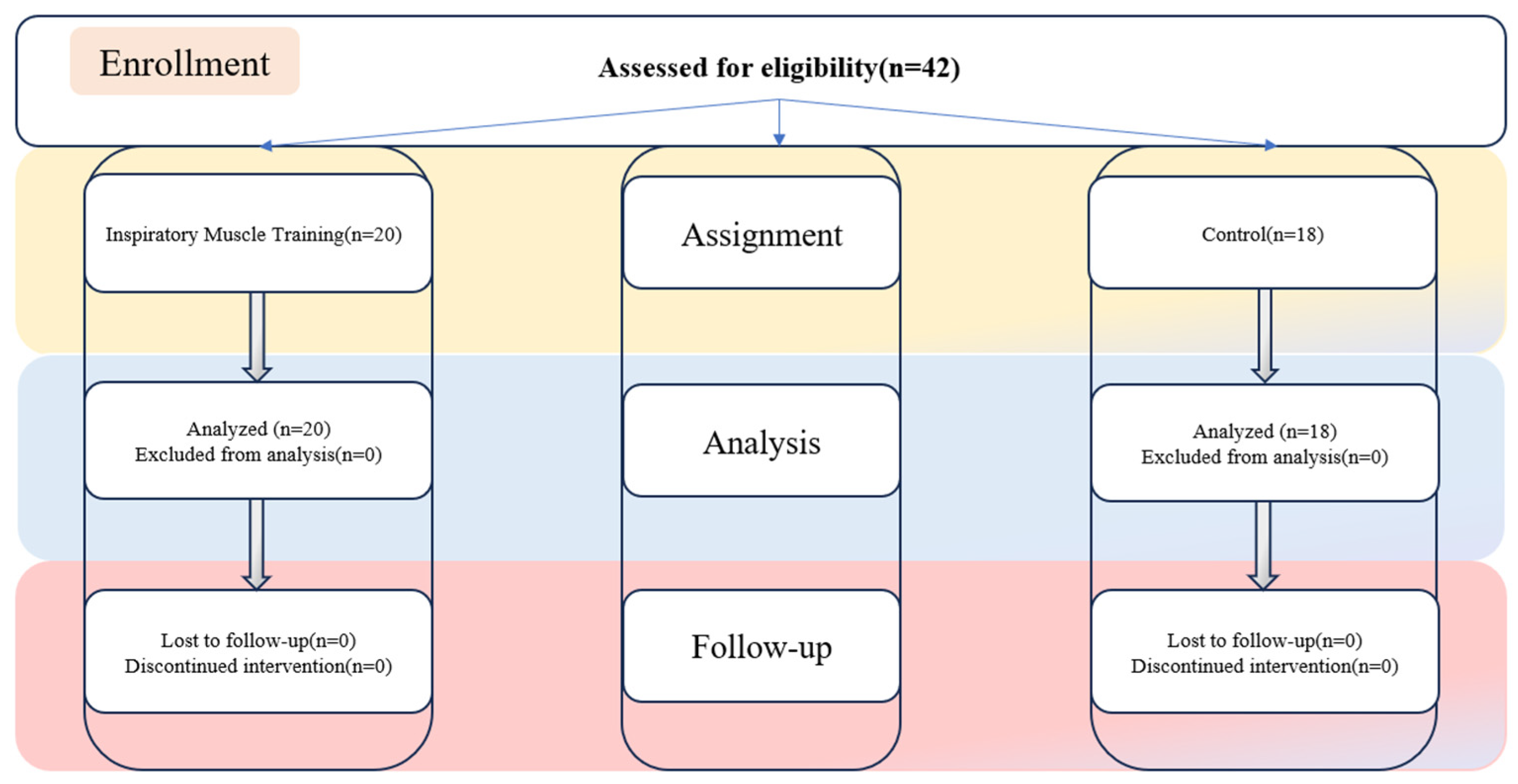
2.1. Participants
2.2. Experimental Design and Task
2.3. Measurements
2.3.1. Maximal Inspiratory Pressure (MIP) Assessment
2.3.2. Pulmonary Function Assessment
2.3.3. Exercise Tolerance and Cardiac Function Assessment
2.3.4. Athletic Performance Assessment
2.3.5. Inspiratory Muscle Training
2.4. Statistical Analysis
3. Results
3.1. Comparative Analysis of Participants’ Pre-Experimental Test Metrics
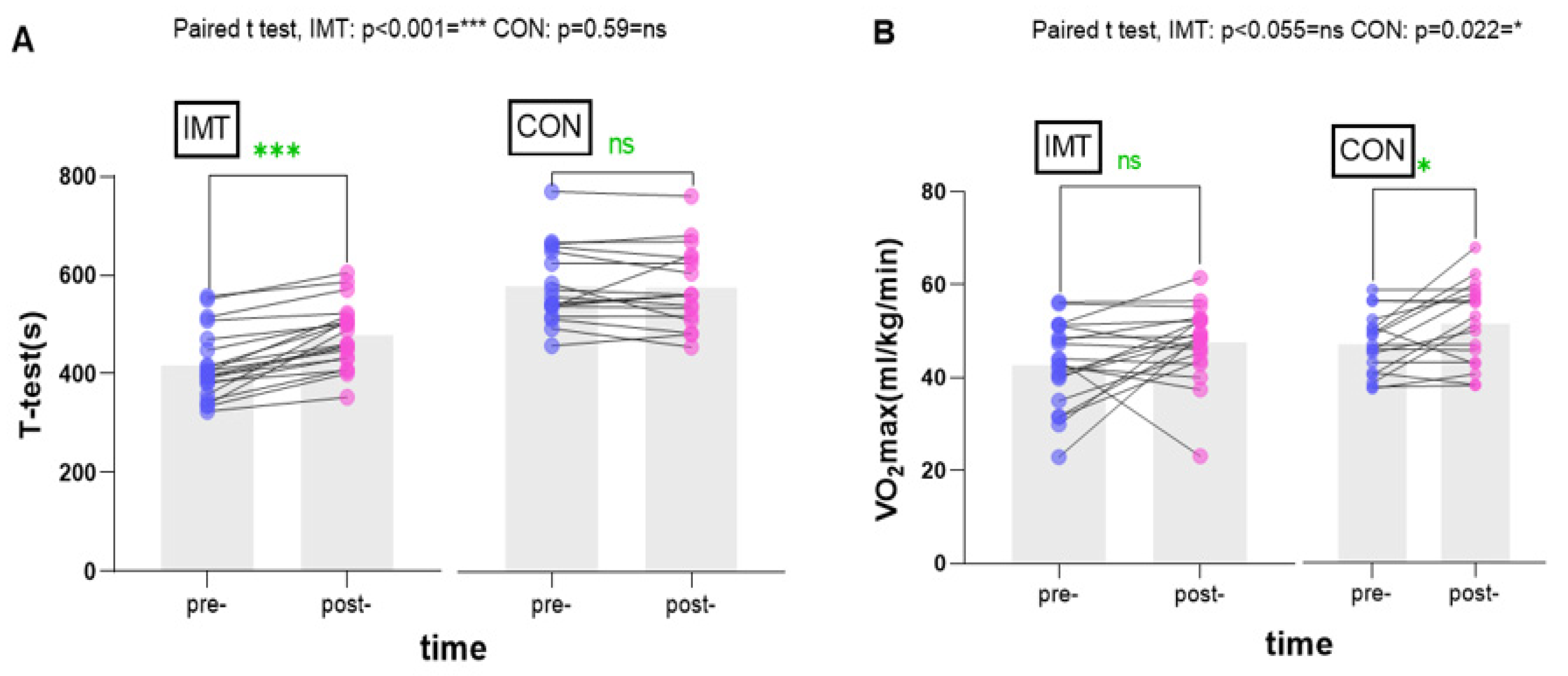
3.2. Comparative Analysis of Test Metrics before and after the Participants’ Experiment
4. Discussion
4.1. Effects of Inspiratory Muscle Training in Maximal Inspiratory Pressure and Pulmonary Function Assessment
4.2. Effects of Inspiratory Muscle Training on Exercise Tolerance and Cardiac Function Assessment
4.3. Effects of Inspiratory Muscle Training in Athletic Performance Assessments
5. Conclusions
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Tian, R.; Wang, Z.H.; Dong, Y.H.; Yang, Z.P.; Ma, J. A cross-section study on physical endurance level in primary and middle school students in China, 2014. Zhonghua Liu Xing Bing Xue Za Zhi 2017, 38, 592–596. [Google Scholar] [CrossRef] [PubMed]
- Ruiz, J.R.; Castro-Piñero, J.; Artero, E.G.; Ortega, F.B.; Sjöström, M.; Suni, J.; Castillo, M.J. Predictive validity of health-related fitness in youth: A systematic review. Br. J. Sports Med. 2009, 43, 909. [Google Scholar] [CrossRef] [PubMed]
- Barrett, S.; Huffman, F.; Johnson, P.; Campa, A.; Magnus, M.; Ragoobirsingh, D. Physical Activity and Metabolic Risk Factors among Jamaican Adolescents (LB443). FASEB J. 2014, 28, LB443. [Google Scholar] [CrossRef]
- Oueslati, F.; Berriri, A.; Boone, J.; Ahmaidi, S. Respiratory muscle strength is decreased after maximal incremental exercise in trained runners and cyclists. Respir. Physiol. Neurobiol. 2018, 248, 25–30. [Google Scholar] [CrossRef] [PubMed]
- Illi, S.K.; Held, U.; Frank, I.; Spengler, C.M. Effect of respiratory muscle training on exercise performance in healthy individuals: A systematic review and meta-analysis. Sports Med. 2012, 42, 707–724. [Google Scholar] [CrossRef] [PubMed]
- HajGhanbari, B.; Yamabayashi, C.; Buna, T.R.; Coelho, J.D.; Freedman, K.D.; Morton, T.A.; Palmer, S.A.; Toy, M.A.; Walsh, C.; Sheel, A.W.; et al. Effects of respiratory muscle training on performance in athletes: A systematic review with meta-analyses. J. Strength Cond. Res. 2013, 27, 1643–1663. [Google Scholar] [CrossRef] [PubMed]
- Shei, R.J.; Paris, H.L.; Wilhite, D.P.; Chapman, R.F.; Mickleborough, T.D. The role of inspiratory muscle training in the management of asthma and exercise-induced bronchoconstriction. Phys. Sportsmed. 2016, 44, 327–334. [Google Scholar] [CrossRef] [PubMed]
- Sales, A.T.d.N.; Fregonezi, G.A.d.F.; Ramsook, A.H.; Guenette, J.A.; Lima, I.N.D.F.; Reid, W.D. Respiratory muscle endurance after training in athletes and non-athletes: A systematic review and meta-analysis. Phys. Ther. Sport 2016, 17, 76–86. [Google Scholar] [CrossRef]
- Martín-Sánchez, C.; Barbero-Iglesias, F.J.; Amor-Esteban, V.; Martín-Sánchez, M.; Martín-Nogueras, A.M. Long-Term Effects of Inspiratory Muscle Training in Institutionalized Elderly Women: A Double-Blind Randomized Controlled Trial. Gerontology 2023, 69, 30–36. [Google Scholar] [CrossRef]
- Najafi, A.; Ebrahim, K.; Ahmadizad, S.; Jahani Ghaeh Ghashlagh, G.R.; Javidi, M.; Hackett, D. Improvements in soccer-specific fitness and exercise tolerance following 8 weeks of inspiratory muscle training in adolescent males. J. Sports Med. Phys. Fit. 2019, 59, 1975–1984. [Google Scholar] [CrossRef]
- Kilding, A.E.; Brown, S.; McConnell, A.K. Inspiratory muscle training improves 100 and 200 m swimming performance. Eur. J. Appl. Physiol. 2010, 108, 505–511. [Google Scholar] [CrossRef] [PubMed]
- Ohya, T.; Kusanagi, K.; Koizumi, J.; Ando, R.; Katayama, K.; Suzuki, Y. Effect of Moderate- or High-Intensity Inspiratory Muscle Strength Training on Maximal Inspiratory Mouth Pressure and Swimming Performance in Highly Trained Competitive Swimmers. Int. J. Sports Physiol. Perform. 2022, 17, 343–349. [Google Scholar] [CrossRef] [PubMed]
- Rożek-Piechura, K.; Kurzaj, M.; Okrzymowska, P.; Kucharski, W.; Stodółka, J.; Maćkała, K. Influence of Inspiratory Muscle Training of Various Intensities on the Physical Performance of Long-Distance Runners. J. Hum. Kinet. 2020, 75, 127–137. [Google Scholar] [CrossRef] [PubMed]
- Hodges, P.W.; Gandevia, S.C. Changes in intra-abdominal pressure during postural and respiratory activation of the human diaphragm. J. Appl. Physiol. 2000, 89, 967–976. [Google Scholar] [CrossRef]
- Hodges, P.W.; Butler, J.E.; McKenzie, D.K.; Gandevia, S.C. Contraction of the human diaphragm during rapid postural adjustments. J. Physiol. 1997, 505 Pt 2, 539–548. [Google Scholar] [CrossRef] [PubMed]
- Ozmen, T.; Gunes, G.Y.; Ucar, I.; Dogan, H.; Gafuroglu, T.U. Effect of respiratory muscle training on pulmonary function and aerobic endurance in soccer players. J. Sports Med. Phys. Fit. 2017, 57, 507–513. [Google Scholar] [CrossRef] [PubMed]
- Mackała, K.; Kurzaj, M.; Okrzymowska, P.; Stodółka, J.; Coh, M.; Rożek-Piechura, K. The Effect of Respiratory Muscle Training on the Pulmonary Function, Lung Ventilation, and Endurance Performance of Young Soccer Players. Int. J. Environ. Res. Public Health 2019, 17, 234. [Google Scholar] [CrossRef]
- El-Deen, H.A.B.; Alanazi, F.S.; Ahmed, K.T. Effects of inspiratory muscle training on pulmonary functions and muscle strength in sedentary hemodialysis patients. J. Phys. Ther. Sci. 2018, 30, 424–427. [Google Scholar] [CrossRef]
- Forbes, S.; Game, A.; Syrotuik, D.; Jones, R.; Bell, G.J. The effect of inspiratory and expiratory respiratory muscle training in rowers. Res. Sports Med/ 2011, 19, 217–230. [Google Scholar] [CrossRef]
- Cavalcante Silva, R.L.; Hall, E.; Maior, A.S. Inspiratory muscle training improves performance of a repeated sprints ability test in professional soccer players. J. Bodyw. Mov. Ther. 2019, 23, 452–455. [Google Scholar] [CrossRef]
- de Sousa, M.M.; Pimentel, M.D.S.; Sobreira, I.A.; Barros, R.J.; Borghi-Silva, A.; Mazzoli-Rocha, F. Inspiratory Muscle Training Improves Aerobic Capacity in Amateur Indoor Football Players. Int. J. Sports Med. 2021, 42, 456–463. [Google Scholar] [CrossRef]
- Smart, N.A.; Giallauria, F.; Dieberg, G. Efficacy of inspiratory muscle training in chronic heart failure patients: A systematic review and meta-analysis. Int. J. Cardiol. 2013, 167, 1502–1507. [Google Scholar] [CrossRef]
- Mickleborough, T.D.; Nichols, T.; Lindley, M.R.; Chatham, K.; Ionescu, A.A. Inspiratory flow resistive loading improves respiratory muscle function and endurance capacity in recreational runners. Scand. J. Med. Sci. Sports 2010, 20, 458–468. [Google Scholar] [CrossRef]
- Stavrou, V.T.; Tourlakopoulos, K.N.; Daniil, Z.; Gourgoulianis, K.I. Respiratory Muscle Strength: New Technology for Easy Assessment. Cureus 2021, 13, e14803. [Google Scholar] [CrossRef]
- Miller, M.R.; Hankinson, J.; Brusasco, V.; Burgos, F.; Casaburi, R.; Coates, A.; Crapo, R.; Enright, P.; van der Grinten, C.P.; Gustafsson, P.; et al. Standardisation of spirometry. Eur. Respir. J. 2005, 26, 319–338. [Google Scholar] [CrossRef]
- Guidetti, L.; Meucci, M.; Bolletta, F.; Emerenziani, G.P.; Gallotta, M.C.; Baldari, C. Validity, reliability and minimum detectable change of COSMED K5 portable gas exchange system in breath-by-breath mode. PLoS ONE 2018, 13, e0209925. [Google Scholar] [CrossRef]
- Perez-Suarez, I.; Martin-Rincon, M.; Gonzalez-Henriquez, J.J.; Fezzardi, C.; Perez-Regalado, S.; Galvan-Alvarez, V.; Juan-Habib, J.W.; Morales-Alamo, D.; Calbet, J.A.L. Accuracy and Precision of the COSMED K5 Portable Analyser. Front. Physiol. 2018, 9, 1764. [Google Scholar] [CrossRef] [PubMed]
- Chang, Y.-C.; Chang, H.-Y.; Ho, C.-C.; Lee, P.-F.; Chou, Y.-C.; Tsai, M.-W.; Chou, L.-W. Effects of 4-Week Inspiratory Muscle Training on Sport Performance in College 800-Meter Track Runners. Medicina 2021, 57, 72. [Google Scholar] [CrossRef]
- Cohen, J. A power primer. Psychol. Bull. 1992, 112, 155–159. [Google Scholar] [CrossRef] [PubMed]
- Aznar-Lain, S.; Webster, A.L.; Cañete, S.; San Juan, A.F.; López Mojares, L.M.; Pérez, M.; Lucia, A.; Chicharro, J.L. Effects of inspiratory muscle training on exercise capacity and spontaneous physical activity in elderly subjects: A randomized controlled pilot trial. Int. J. Sports Med. 2007, 28, 1025–1029. [Google Scholar] [CrossRef]
- Volianitis, S.; McConnell, A.K.; Koutedakis, Y.; McNaughton, L.; Backx, K.; Jones, D.A. Inspiratory muscle training improves rowing performance. Med. Sci. Sports Exerc. 2001, 33, 803–809. [Google Scholar] [CrossRef] [PubMed]
- Kwok, T.M.K.; Jones, A.Y.M. Target-flow Inspiratory Muscle Training Improves Running Performance in Recreational Runners: A Randomized Controlled Trial. Hong Kong Physiother. J. 2009, 27, 48–54. [Google Scholar] [CrossRef]
- Kraemer, W.J.; Fleck, S.J.; Evans, W.J. Strength and power training: Physiological mechanisms of adaptation. Exerc. Sport Sci. Rev. 1996, 24, 363–397. [Google Scholar] [CrossRef] [PubMed]
- Shei, R.-J. Recent Advancements in Our Understanding of the Ergogenic Effect of Respiratory Muscle Training in Healthy Humans: A Systematic Review. J. Strength Cond. Res. 2018, 32, 2665–2676. [Google Scholar] [CrossRef]
- Sperlich, B.; Fricke, H.; de Marées, M.; Linville, J.W.; Mester, J. Does respiratory muscle training increase physical performance? Mil. Med. 2009, 174, 977–982. [Google Scholar] [CrossRef]
- Nicks, C.R.; Morgan, D.W.; Fuller, D.K.; Caputo, J.L. The influence of respiratory muscle training upon intermittent exercise performance. Int. J. Sports Med. 2009, 30, 16–21. [Google Scholar] [CrossRef]
- Tong, T.K.; Fu, F.H.; Eston, R.; Chung, P.K.; Quach, B.; Lu, K. Chronic and acute inspiratory muscle loading augment the effect of a 6-week interval program on tolerance of high-intensity intermittent bouts of running. J. Strength Cond. Res. 2010, 24, 3041–3048. [Google Scholar] [CrossRef]
- Tong, T.K.; Fu, F.H.; Chung, P.K.; Eston, R.; Lu, K.; Quach, B.; Nie, J.; So, R. The effect of inspiratory muscle training on high-intensity, intermittent running performance to exhaustion. Appl. Physiol. Nutr. Metab. 2008, 33, 671–681. [Google Scholar] [CrossRef] [PubMed]


| Anthropological Information | IMT Group (n = 20) Mean ± SD | Control Group (n = 18) Mean ± SD | p |
|---|---|---|---|
| Age, years | 18.55 ± 0.89 | 18.67 ± 1.08 | 0.74 |
| Height, cm | 176.9 ± 6.48 | 176.06 ± 5.6 | 0.67 |
| Mass, kg | 68.65 ± 10.63 | 68.39 ± 12.5 | 0.95 |
| BMI | 21.98 ± 3.59 | 22.00 ± 4.40 | 0.93 |
| Variables | IMT Group (n = 20) | Control Group (n = 18) | t/Z | p |
|---|---|---|---|---|
| Pre- | Pre- | |||
| MIP | ||||
| MIP (cmH2O) | 100.50 ± 27.30 | 96.72 ± 24.33 | 0.448 | 0.66 |
| pulmonary function | ||||
| PEF (L/min) | 451.10 ± 124.13 | 460.39 ± 96.04 | −0.256 | 0.80 |
| PEF (%) | 70.65 ± 19.50 | 72.11 ± 14.97 | −0.073 | 0.942 |
| FVC (L) | 3.30 ± 0.906 | 2.90 ± 0.94 | 1.307 | 0.199 |
| FEV1 (L) | 3.28 ± 0.90 | 2.82 ± 0.85 | 1.597 | 0.119 |
| FEV1 (%) | 63.65 ± 15.75 | 58.17 ± 17.53 | 1.016 | 0.316 |
| FEV1/FVC (%) | 95.30 ± 8.85 | 97.94 ± 3.49 | −0.550 | 0.583 |
| Exercise tolerance | ||||
| VO2max (mL/min/kg) | 42.72 ± 9.03 | 47.08 ± 6.54 | −1.685 | 0.10 |
| METS | 12.22 ± 2.59 | 13.44 ± 1.85 | −1.667 | 0.104 |
| RQ | 1.12 ± 0.10 | 1.05 ± 0.1 | −1.934 | 0.053 |
| VE (L/min) | 77.62 ± 26.74 | 73.27 ± 18.44 | 0.576 | 0.57 |
| BR (%) | 53.41 ± 15.74 | 55.65 ± 11.03 | −0.501 | 0.62 |
| HRmax (bpm) | 190.25 ± 16.29 | 189.89 ± 8.67 | −0.834 | 0.404 |
| VO2/HR (mL/beat) | 15.10 ± 2.22 | 16.92 ± 3.45 | −1.579 | 0.114 |
| t-test (s) | 417.00 ± 70.19 | 433.67 ± 58.52 | −1.023 | 0.306 |
| Athletic Performance | ||||
| 1000 m test (s) | 265.15 ± 19.60 | 259.28 ± 38.60 | −0.951 | 0.342 |
| IMT Group | t/Z | ES | p | Control Group | t/Z | ES | p | |||
|---|---|---|---|---|---|---|---|---|---|---|
| Pre- | Post- | Pre- | Post- | |||||||
| MIP (cmH2O) | 100.50 ± 27.30 | 150.65 ± 28.51 | −3.921 | 1.797 | <0.001 | 96.72 ± 24.33 | 99.06 ± 24.74 | −0.953 | 0.095 | 0.354 |
| PEF (L/min) | 451.10 ± 124.13 | 567.25 ± 70.54 | −3.734 | 1.151 | <0.001 | 460.39 ± 96.04 | 477.17 ± 88.97 | −0.501 | 0.181 | 0.616 |
| PEF (%) | 70.65 ± 19.50 | 90.60 ± 11.78 | −3.772 | 1.238 | <0.001 | 72.11 ± 14.97 | 76.11 ± 13.99 | −0.640 | 0.276 | 0.522 |
| FVC (L) | 3.30 ± 0.906 | 2.75 ± 0.91 | 2.582 | 0.606 | 0.018 | 2.90 ± 0.94 | 2.80 ± 0.98 | 0.536 | 0.104 | 0.599 |
| FEV1 (L) | 3.28 ± 0.90 | 2.75 ± 0.91 | 2.506 | 0.586 | 0.021 | 2.82 ± 0.85 | 2.80 ± 0.98 | 0.136 | 0.22 | 0.893 |
| FEV1 (%) | 63.65 ± 15.75 | 58.25 ± 19.64 | 1.264 | 0.303 | 0.222 | 58.17 ± 17.53 | 57.50 ± 18.43 | 0.188 | 0.037 | 0.853 |
| FEV1/FVC (%) | 95.30 ± 8.85 | 100 ± 0.00 | −2.371 | 0.751 | 0.018 | 97.94 ± 3.49 | 98.22 ± 5.86 | −0.405 | 0.058 | 0.686 |
| VO2max (mL/min/kg) | 42.73 ± 9.03 | 47.58 ± 8.08 | −2.041 | 0.566 | 0.055 | 47.08 ± 6.54 | 51.58 ± 8.76 | −2.291 | 0.582 | 0.022 |
| METS | 12.22 ± 2.59 | 13.60 ± 2.31 | −2.030 | 0.562 | 0.057 | 13.44 ± 1.85 | 14.74 ± 2.66 | −2.546 | 0.567 | 0.021 |
| RQ | 1.12 ± 0.10 | 1.01 ± 0.07 | 4.786 | 1.274 | <0.001 | 1.05 ± 0.1 | 0.94 ± 0.08 | −3.468 | 1.215 | <0.001 |
| VE (L/min) | 77.62 ± 26.74 | 85.17 ± 20.84 | −1.016 | 0.315 | 0.323 | 73.27 ± 18.44 | 71.63 ± 19.89 | 0.534 | 0.086 | 0.60 |
| BR (%) | 53.41 ± 15.74 | 49.09 ± 12.44 | 0.993 | 0.305 | 0.333 | 55.65 ± 11.03 | 59.19 ± 13.32 | −1.034 | 0.289 | 0.301 |
| HRmax (bpm) | 190.25 ± 16.29 | 198.00 ± 10.04 | −2.266 | 0.573 | 0.023 | 189.89 ± 8.67 | 191.44 ± 7.30 | −1.514 | 0.193 | 0.13 |
| VO2/HR (mL/beat) | 15.10 ± 2.22 | 16.47 ± 3.49 | −1.868 | 0.468 | 0.062 | 16.92 ± 3.45 | 18.28 ± 3.97 | −2.587 | 0.366 | 0.019 |
| t-test (s) | 417.00 ± 70.19 | 478.05 ± 65.11 | −3.920 | 0.902 | <0.001 | 433.67 ± 58.52 | 431.89 ± 59.98 | −0.545 | 0.03 | 0.586 |
| 1000 m test (s) | 265.15 ± 19.60 | 252.55 ± 20.21 | 5.042 | 0.633 | <0.001 | 259.28 ± 38.60 | 263.22 ± 32.35 | −1.527 | 0.111 | 0.127 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Qin, L.; Liu, S.; Hu, S.; Feng, L.; Wang, H.; Gong, X.; Xuan, W.; Lu, T. The Effect of Inspiratory Muscle Training on Health-Related Fitness in College Students. Int. J. Environ. Res. Public Health 2024, 21, 1088. https://doi.org/10.3390/ijerph21081088
Qin L, Liu S, Hu S, Feng L, Wang H, Gong X, Xuan W, Lu T. The Effect of Inspiratory Muscle Training on Health-Related Fitness in College Students. International Journal of Environmental Research and Public Health. 2024; 21(8):1088. https://doi.org/10.3390/ijerph21081088
Chicago/Turabian StyleQin, Lili, Siyu Liu, Shuang Hu, Linlin Feng, Huan Wang, Xingzhou Gong, Wei Xuan, and Tianfeng Lu. 2024. "The Effect of Inspiratory Muscle Training on Health-Related Fitness in College Students" International Journal of Environmental Research and Public Health 21, no. 8: 1088. https://doi.org/10.3390/ijerph21081088








