A Scoping Review of Non-Communicable Diseases among the Workforce as a Threat to Global Peace and Security in Low-Middle Income Countries
Abstract
:1. Introduction
2. Materials and Methods
2.1. Inclusion Criteria
2.2. Search Strategy
2.3. Outcome Variable
2.4. Data Extraction and Analysis
3. Results
3.1. Characteristics of Selected Articles
3.2. The Nature and Impact of NCDs in LMIC
NCDs among the Workforce
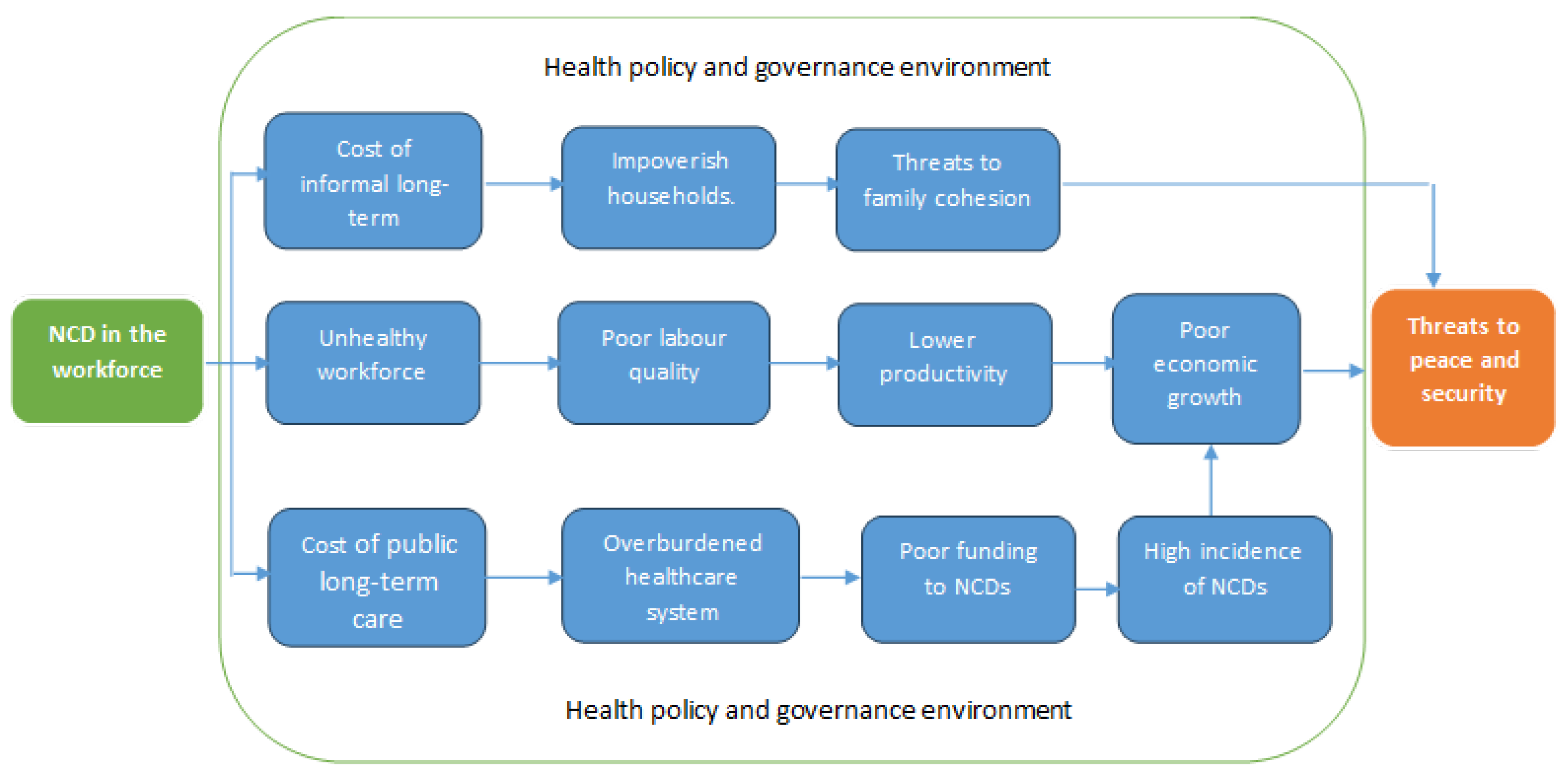
3.3. NCDs in the Workforce as a Threat to Peace and Security
4. Discussion
5. Strengths and Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Global Action Plan for the Prevention and Control of Noncommunicable Diseases 2013–2020; World Health Organization: Geneva, Switzerland, 2013. [Google Scholar]
- GBD 2019 Risk Factors Collaborators. Global burden of 87 risk factors in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020, 396, 1223–1249. [Google Scholar] [CrossRef] [PubMed]
- Roth, G.A.; Mensah, G.A.; Johnson, C.O.; Addolorato, G.; Ammirati, E.; Baddour, L.M.; Barengo, N.C.; Beaton, A.Z.; Benjamin, E.J.; Benziger, C.P.; et al. Global burden of cardiovascular diseases and risk factors, 1990–2019: Update from the GBD 2019 study. J. Am. Coll. Cardiol. 2020, 76, 2982–3021. [Google Scholar] [CrossRef] [PubMed]
- Piot, P.; Caldwell, A.; Lamptey, P.; Nyrirenda, M.; Mehra, S.; Cahill, K.; Aerts, A. Addressing the growing burden of non–communicable disease by leveraging lessons from infectious disease management. J. Glob. Health 2016, 6, 010304. [Google Scholar] [CrossRef]
- World Bank Country and Lending Groups. Country Classification for the 2025 Fiscal Year. 2024. Available online: https://datahelpdesk.worldbank.org/knowledgebase/articles/906519 (accessed on 1 July 2024).
- Ndione, I.; Aerts, A.; Barshilia, A.; Boch, J.; Rosiers, S.D.; Ferrer, J.M.E.; Saric, J.; Seck, K.; Sene, B.N.; Steinmann, P.; et al. Fostering cardiovascular health at work–case study from Senegal. BMC Public Health 2021, 21, 1108. [Google Scholar] [CrossRef]
- World Health Organization. Noncommunicable Diseases. 2023. Available online: https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases#:~:text=NCDs%20disproportionately%20affect%20people%20in,deaths%20(31.4%20million)%20occur (accessed on 1 July 2024).
- Gostin, L.O.; Abou-Taleb, H.; Roache, S.; Alwan, A. Legal priorities for prevention of non-communicable diseases: Innovations from WHO’s Eastern Mediterranean region. Public Health 2017, 144, 4–12. [Google Scholar] [CrossRef]
- World Health Organization. Noncommunicable Diseases: Role of Legislation in Preventing and Controlling Noncommunicable Diseases in the Eastern Mediterranean Region. 2024. Available online: https://www.emro.who.int/noncommunicable-diseases/publications/questions-and-answers-on-role-of-legislation-in-preventing-and-controlling-noncommunicable-diseases-in-the-region.html (accessed on 1 July 2024).
- Ndubuisi, N.E. Noncommunicable diseases prevention in low-and middle-income countries: An overview of health in all policies (HiAP). INQUIRY J. Health Care Organ. Provis. Financ. 2021, 58, 0046958020927885. [Google Scholar] [CrossRef]
- Elhadi, Y.A.M. Progress and challenges in implementing non-communicable disease policies in Sudan. Health Res. Policy Syst. 2023, 21, 130. [Google Scholar] [CrossRef] [PubMed]
- Alliance, N. Tackling non-communicable diseases in workplace settings in low-and middle-income countries. In A Call to Action and Practical Guidance; 2017 ed.; Non-Communicable diseases (NCD) Alliance: Geneva, Switzerland, 2018. [Google Scholar]
- Shah, S.; Munyuzangabo, M.; Gaffey, M.F.; Kamali, M.; Jain, R.P.; Als, D.; Meteke, S.; Radhakrishnan, A.; Siddiqui, F.J.; Ataullahjan, A.; et al. Delivering non-communicable disease interventions to women and children in conflict settings: A systematic review. BMJ Glob. Health 2020, 5 (Suppl. S1), e002047. [Google Scholar] [CrossRef]
- Idris, I.B.; Azit, N.A.; Ghani, S.R.A.; Nor, S.F.S.; Nawi, A.M. A systematic review on noncommunicable diseases among working women. Ind. Health 2021, 59, 146–160. [Google Scholar] [CrossRef]
- Agaba, E.I.; Akanbi, M.O.; Agaba, P.A.; Ocheke, A.N.; Gimba, Z.M.; Daniyam, S.; Okeke, E.N. A survey of non-communicable diseases and their risk factors among university employees: A single institutional study. Cardiovasc. J. Afr. 2017, 28, 377–384. [Google Scholar] [CrossRef]
- Tipayamongkholgul, M.; Kongtip, P.; Woskie, S. Association between occupations and selected noncommunicable diseases: A matched case-control among Thai informal workers. J. Occup. Health 2021, 63, e12249. [Google Scholar] [CrossRef]
- Ndiaye, A.A.; Tall, A.B.; Gueye, B.; Fall, I.S.; Seck, S.M.; Mbodj, A.B.; Ngom-Gueye, N.F.; Gaye, A.; Tal-Dia, A. A cross-sectional survey on non-communicable diseases and risk factors in the Senegalese Army. Health 2016, 8, 1529–1541. [Google Scholar] [CrossRef]
- Ngan, W.B.; Belinga, L.E.E.; Nlo’o, A.S.P.E.; Roche, F.; Goethals, L.; Mandengue, S.H.; Bongue, B. Surveillance of Cardiovascular Risk Factors in the Fifth Military Sector Health Center, Ngaoundere, Cameroon: Observational Study. JMIR Form. Res. 2020, 4, e18567. [Google Scholar] [CrossRef]
- Whitaker, J.; Rickard, R.; Leather, A.; Davies, J. Exploring the global health and defence engagement interface. BMJ Mil. Health 2023, 170, e65–e69. [Google Scholar] [CrossRef]
- Asadi-Lari, M.; Teymourlouy, A.A.; Maleki, M.; Afshari, M. Opportunities and challenges of global health diplomacy for prevention and control of noncommunicable diseases: A systematic review. BMC Health Serv. Res. 2021, 21, 1193. [Google Scholar] [CrossRef] [PubMed]
- Falqui, L.; Li, F.; Xue, Y. Global health diplomacy in humanitarian action. Confl. Health 2024, 18, 46. [Google Scholar] [CrossRef] [PubMed]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.; Horsley, T.; Weeks, L.; et al. PRISMA extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef]
- Page, M.; McKenzie, J.; Bossuyt, P.; Boutron, I.; Hoffmann, T.; Mulrow, C.; Shamseer, L.; Tetzlaff, J.; Akl, E.; Brennan, S.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Int. J. Surg. 2021, 372, n71. [Google Scholar]
- Wamai, R.G.; Kengne, A.P.; Levitt, N. Non-communicable diseases surveillance: Overview of magnitude and determinants in Kenya from STEPwise approach survey of 2015. BMC Public Health 2018, 18, 1224. [Google Scholar] [CrossRef]
- Allen, L.; Cobiac, L.; Townsend, N. Quantifying the global distribution of premature mortality from non-communicable diseases. J. Public Health 2017, 39, 698–703. [Google Scholar] [CrossRef]
- Baxter, L.M.; Eldin, M.S.; Al Mohammed, A.; Saim, M.; Checchi, F. Access to care for non-communicable diseases in Mosul, Iraq between 2014 and 2017: A rapid qualitative study. Confl. Health 2018, 12, 48. [Google Scholar] [CrossRef] [PubMed]
- GBD 2017 Risk Factor Collaborators. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018, 392, 1923–1994. [Google Scholar]
- Bloom, D.E.; Chisholm, D.; Jané-Llopis, E.; Prettner, K.; Stein, A.; Feigl, A. From Burden to “Best Buys”: Reducing the Economic Impact of Non-Communicable Diseases; World Health Organization: Geneva, Switzerland, 2011. [Google Scholar]
- Fox, J.; Desai, M.M.; Britten, K.; Lucas, G.; Luneau, R.; Rosenthal, M.S. Mental-health conditions, barriers to care, and productivity loss among officers in an urban police department. Conn. Med. 2012, 76, 525. [Google Scholar]
- Buckman, J.E.J.; Forbes, H.J.; Clayton, T.; Jones, M.; Jones, N.; Greenberg, N.; Sundin, J.; Hull, L.; Wessely, S.; Fear, N.T. Early Service leavers: A study of the factors associated with premature separation from the UK Armed Forces and the mental health of those that leave early. Eur. J. Public Health 2013, 23, 410–415. [Google Scholar] [CrossRef]
- Bhatia, K.M.; Pandit, N. Prevalence of chronic morbidity and sociodemographic profile of police personnel–a study from Gujarat. J. Clin. Diagn. Res. JCDR 2017, 11, LC06. [Google Scholar] [CrossRef] [PubMed]
- Mohammed, J. Knowledge of, and attitude to cardiovascular disease risk factors among members of the Nigerian armed forces. World J. Public Health 2012, 1, 23–27. [Google Scholar]
- Heydari, S.T.; Khoshdel, A.; Sabayan, B.; Abtahi, F.; Zamirian, M.; Sedaghat, S. Prevalence of cardiovascular risk factors among military personnel in southern Iran. Iran. Cardiovasc. Res. J. 2010, 4, 22–27. [Google Scholar]
- Al-Dahi, S.; Al-Khashan, H.; Al Madeer, M.A.M.; Al-Saif, K.; Al-Amri, M.D.S.; Al-Ghamdi, O.; Al-Helali, N.; Selim, M.; Mishriky, A.M. Assessment of Framingham cardiovascular disease risk among militaries in the Kingdom of Saudi Arabia. Mil. Med. 2013, 178, 299–305. [Google Scholar] [CrossRef]
- Gantt, C.J.; Neely, J.A.; Villafana, I.A.; Chun, C.S.; Gharabaghli, S.M. Analysis of weight and associated health consequences of the active duty staff at a major Naval medical center. Mil. Med. 2008, 173, 434–440. [Google Scholar] [CrossRef]
- Wenzel, D.; Souza, J.M.P.D.; Souza, S.B.D. Prevalence of arterial hypertension in young military personnel and associated factors. Rev. Saude Publica 2009, 43, 789–795. [Google Scholar] [CrossRef]
- Gorham, E.D.; Barrett-Connor, E.; Highfill-McRoy, R.M.; Mohr, S.B.; Garland, C.F.; Garland, F.C.; Ricordi, C. Incidence of insulin-requiring diabetes in the US military. Diabetologia 2009, 52, 2087–2091. [Google Scholar] [CrossRef]
- Laclaustra-Gimeno, M.; González-García, M.P.; Casasnovas-Lenguas, J.A.; Luengo-Fernández, E.; León-Latre, M.; Portero-Pérez, P.; Del Río-Ligorit, A.; Giner-Soria, A.; Ferreira-Montero, I.J. Cardiovascular risk factor progression in young males at 15-year follow-up in the General Military Academy of Zaragoza (AGEMZA) Study. Rev. Española Cardiol. (Engl. Ed.) 2006, 59, 671–678. [Google Scholar] [CrossRef]
- Grósz, A.; Tóth, E.; Péter, I. A 10-year follow-up of ischemic heart disease risk factors in military pilots. Mil. Med. 2007, 172, 214–219. [Google Scholar] [CrossRef] [PubMed]
- Alghamdi, A.S.; Yahya, M.A.; Alshammari, G.M.; Osman, M.A. Prevalence of overweight and obesity among police officers in Riyadh City and risk factors for cardiovascular disease. Lipids Health Dis. 2017, 16, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Tharkar, S.; Kumpatla, S.; Muthukumaran, P.; Viswanathan, V. High prevalence of metabolic syndrome and cardiovascular risk among police personnel compared to general population in India. JAPI 2008, 56, 19263681. [Google Scholar]
- Sparrow, D.; Jr, H.T.; Weiss, S.T. Coronary heart disease in police officers participating in the normative aging study. Am. J. Epidemiol. 1983, 118, 508–513. [Google Scholar] [CrossRef]
- Smith, D.R.; Devine, S.U.E.; Leggat, P.A.; Ishitake, T. Alcohol and tobacco consumption among police officers. Kurume Med. J. 2005, 52, 63–65. [Google Scholar] [CrossRef]
- Ardiana, M.; Harsoyo, P.M.; Hermawan, H.O.; Sufiyah, I.M.; Firmanda, D.R.; Desita, S.R.; Paramitha, A.D.; Hariftiyani, A.S.; Shabrina, F.A.; Triastuti, F. Higher cardiovascular risks and Atherogenic Index of Plasma found in police officers of developing country in Surabaya, East Java, Indonesia. Clin. Epidemiol. Glob. Health 2022, 17, 101132. [Google Scholar] [CrossRef]
- Ngo, V.K.; Rubinstein, A.; Ganju, V.; Kanellis, P.; Loza, N.; Rabadan-Diehl, C.; Daar, A.S. Grand challenges: Integrating mental health care into the non-communicable disease agenda. PLoS Med. 2013, 10, e1001443. [Google Scholar] [CrossRef] [PubMed]
- Sahle, B.W.; Slewa-Younan, S.; Melaku, Y.A.; Ling, L.; Renzaho, A.M.N. A bi-directional association between weight change and health-related quality of life: Evidence from the 11-year follow-up of 9916 community-dwelling adults. Qual. Life Res. 2020, 29, 1697–1706. [Google Scholar] [CrossRef] [PubMed]
- Peterson, A.L.; Severson, H.H.; Andrews, J.A.; Gott, S.P.; Cigrang, J.A.; Gordon, J.S.; Hunter, C.M.; Martin, G.C. Smokeless tobacco use in military personnel. Mil. Med. 2007, 172, 1300–1305. [Google Scholar] [CrossRef]
- Lin, J.; Zhu, K.; Soliván-Ortiz, A.M.; Larsen, S.L.; Schneid, T.R.; Shriver, C.D.; Lee, S. Deployment and smokeless tobacco use among active duty service members in the US Military. Mil. Med. 2019, 184, e183–e190. [Google Scholar] [CrossRef]
- Almond, N.; Kahwati, L.; Kinsinger, L.; Porterfield, D. The prevalence of overweight and obesity among US military veterans. Mil. Med. 2008, 173, 544–549. [Google Scholar] [CrossRef]
- Violanti, J.M.; Vena, J.E.; Petralia, S. Mortality of a police cohort: 1950–1990. Am. J. Ind. Med. 1998, 33, 366–373. [Google Scholar] [CrossRef]
- Chretien, J.-P.; Blazes, D.L.; Coldren, R.L.; Lewis, M.D.; Gaywee, J.; Kana, K.; Sirisopana, N.; Vallejos, V.; Mundaca, C.C.; Montano, S.; et al. The importance of militaries from developing countries in global infectious disease surveillance. Bull. World Health Organ. 2007, 85, 174–180. [Google Scholar] [CrossRef]
- Moreira, O.C.; Oliveira, R.A.R.D.; Oliveira, C.E.P.D.; Doimo, L.A.; Amorim, P.R.D.S.; Marins, J.C.B. Anthropometric, cardiovascular and functional variables as indicators of health related physical fitness in university professors. Fisioter. Mov. 2015, 28, 545–554. [Google Scholar] [CrossRef]
- CheSerek, M.J.; Wu, G.-R.; Shen, L.I.Y.; ShI, Y.-H.; Le, G.-W. Disparities in the prevalence of metabolic syndrome (MS) and its components among university employees by age, gender and occupation. J. Clin. Diagn. Res. JCDR 2014, 8, 65. [Google Scholar]
- Ibrahim, N.K.; Hijazi, N.A.; Al-Bar, A.A. Prevalence and determinants of prehypertension and hypertension among preparatory and secondary school teachers in Jeddah. J. Egypt. Public Health Assoc. 2008, 83, 183–203. [Google Scholar]
- Greiw, A.; Gad, Z.; Mandil, A.; Wagdi, M.; Elneihoum, A. Risk factors for cardiovascular diseases among school teachers in Benghazi, Libya. Ibnosina J. Med. Biomed. Sci. 2010, 2, 168–177. [Google Scholar]
- Awosan, K.J.; Ibrahim, M.T.O.; Sabir, A.A.; Ejimodu, P. Awareness and prevalence of risk factors of coronary heart disease among teachers and bankers in Sokoto, Nigeria. J. Med. Med. Sci. 2013, 4, 337–342. [Google Scholar]
- Setto, J.M.; Bonolo, P.D.F.; Franceschini, S.D.C.C. Relationship between health behaviors and self-reported diseases by public employees. Fisioter. Mov. 2016, 29, 477–485. [Google Scholar] [CrossRef]
- Hegde, S.K.B.; Sathiyanarayanan, S.; Venkateshwaran, S.; Sasankh, A.; Ganeshkumar, P.; Balaji, R. Prevalence of diabetes, hypertension and obesity among doctors and nurses in a medical college hospital in Tamil Nadu, India. World 2015, 1, 235–239. [Google Scholar]
- Sharma, D.; Vatsa, M.; Lakshmy, R.; Narang, R.; Bahl, V.K.; Gupta, S.K. Study of cardiovascular risk factors among tertiary hospital employees and their families. Indian Heart J. 2012, 64, 356–363. [Google Scholar] [CrossRef] [PubMed]
- Gupta, A.; Gupta, R.; Lal, B.; Singh, A.K.; Kothari, K. Prevalence of coronary risk factors among Indian physicians. J. Assoc. Physicians India 2001, 49, 1148–1152. [Google Scholar]
- Shafei, M.N.; Awang, A.F.; Mohamad, W.M. Prevalence of metabolic syndrome and its associated factors among female nurses in a teaching hospital in North-Eastern state of Malaysia. J. Public Health Epidemiol. 2011, 3, 394–400. [Google Scholar]
- De Wet-Billings, N.; Frade, S. Non-communicable disease comorbidities (NCDCs) among youth in South Africa: The causal contribution of not being in school or work and other socioeconomic characteristics. J. Public Health 2022, 30, 1205–1212. [Google Scholar] [CrossRef]
- World Health Organisation. Good Practice in Occupational Health Services: A Contribution to Workplace Health; EUR/02/5041181; WHO ROE: Copenhagen, Denmark, 2002. [Google Scholar]
- World Health Organisation. Preventing Noncommunicable Diseases in the Workplace through Diet and Physical Activity: WHO/World Economic Forum Report of a Joint Event; World Health Organisation: Geneva, Switzerland, 2008. [Google Scholar]
- Gowshall, M.; Taylor-Robinson, S.D. The increasing prevalence of non-communicable diseases in low-middle income countries: The view from Malawi. Int. J. Gen. Med. 2018, 11, 255–264. [Google Scholar] [CrossRef] [PubMed]
- World Health Organisation. Global Status Report on Noncommunicable Diseases 2014. Geneva. July 2014. Available online: https://www.who.int/publications/i/item/9789241564854 (accessed on 26 April 2024).
- Witter, S.; Zou, G.; Diaconu, K.; Senesi, R.G.B.; Idriss, A.; Walley, J.; Wurie, H.R. Opportunities and challenges for delivering non-communicable disease management and services in fragile and post-conflict settings: Perceptions of policy-makers and health providers in Sierra Leone. Confl. Health 2020, 14, 3. [Google Scholar] [CrossRef]
- Rogers, H.E.; Akiteng, A.R.; Mutungi, G.; Ettinger, A.S.; Schwartz, J.I. Capacity of Ugandan public sector health facilities to prevent and control non-communicable diseases: An assessment based upon WHO-PEN standards. BMC Health Serv. Res. 2018, 18, 606. [Google Scholar] [CrossRef]
- Mondo, C.K.; Otim, M.A.; Akol, G.; MuSoke, R.; Orem, J. The prevalence and distribution of non-communicable diseases and their risk factors in Kasese district, Uganda: Cardiovascular topics. Cardiovasc. J. Afr. 2013, 24, 52–57. [Google Scholar] [CrossRef]
- Porter, C. Ottawa to Bangkok: Changing health promotion discourse. Health Promot. Int. 2007, 22, 72–79. [Google Scholar] [CrossRef]
- Hanson, A. Workplace Health Promotion: A Salutogenic Approach; AuthorHouse: Bloomington, IN, USA, 2007. [Google Scholar]
- World Bank. The growing danger of non-communicable diseases: Acting now to reverse course. In Proceedings of the World Bank Human Development Network, Washington, DC, USA, 1 September 2011. [Google Scholar]
- Nikolic, I.A.; Stanciole, A.E.; Zaydman, M. Chronic Emergency: Why NCDs Matter; World Baank: Washington, DC, USA, 2011. [Google Scholar]
- Mayer-Foulkes, D.A. A survey of macro damages from non-communicable chronic diseases: Another challenge for global governance. Glob. Econ. J. 2011, 11, 1850220. [Google Scholar] [CrossRef]
- Marc, S.; Nugent, R.A.; David, S.; Rocco, L. Chronic Disease: An Economic Perspective; The Oxford Health Alliance: London, UK, 2006. [Google Scholar]
- NCD Alliance and Novartis Foundation. Tackling Noncommunicable Diseases in Workplace Settings in Low- and Middle-in Comecountries: A Call to Action and Practical Guidance. 2017. Available online: https://ncdalliance.org/sites/default/files/resource_files/Tackling%20noncommunicable%20diseases%20in%20workplace%20settings%20in%20LMICs_WEB.pdf (accessed on 1 July 2024).
- WHO; UNDP. What Ministries of Labour and Employment Need to Know: Non Communicable Diseases? WHO/UNDP: New York, NY, USA, 2006. [Google Scholar]
- Johns, G. Presenteeism in the workplace: A review and research agenda. J. Organ. Behav. 2010, 31, 519–542. [Google Scholar] [CrossRef]
- Olawuyi, A.T.; Adeoye, I.A. The prevalence and associated factors of non-communicable disease risk factors among civil servants in Ibadan, Nigeria. PLoS ONE 2018, 13, e0203587. [Google Scholar] [CrossRef]
- Chisholm, D.; Sweeny, K.; Sheehan, P.; Rasmussen, B.; Smit, F.; Cuijpers, P.; Saxena, S. Scaling-up treatment of depression and anxiety: A global return on investment analysis. Lancet Psychiatry 2016, 3, 415–424. [Google Scholar] [CrossRef]
- Horner, L.K.; Kadiwal, L.; Sayed, Y.; Barrett, A.; Durrani, N.; Novelli, M. Literature Review: The Role of Teachers in Peacebuilding; UNICEF Research Consortium on Education and Peace Building: Amsterdam, The Netherlands, 2015. [Google Scholar]
- MacQueen, G.; Santa-Barbara, J. Peace building through health initiatives. BMJ 2000, 321, 293–296. [Google Scholar] [CrossRef]
- Hannink, J.; Womenss, I. Not Just a Nurse: Nurses as Peaceworkers in Hadassah Ein Kerem. Honours Thesis, Wellesley College, Wellesley, MA, USA, 2016. [Google Scholar]
- Mensah, G.A.; Bakris, G. The United Nations high level meeting addresses noncommunicable diseases, but where is hypertension? J. Clin. Hypertens. 2011, 13, 787. [Google Scholar] [CrossRef]
- Rijal, A.; Adhikari, T.B.; Khan, J.A.M.; Berg-Beckhoff, G. The economic impact of non-communicable diseases among households in South Asia and their coping strategy: A systematic review. PLoS ONE 2018, 13, e0205745. [Google Scholar] [CrossRef] [PubMed]

| Main Keywords | Synonyms/Similar Keywords |
|---|---|
| Workforce | “workforce” OR “workers” |
| Non-communicable disease | “Non-communicable disease” OR “NCDs” |
| Peace and security | “peace” or “security”, OR “peace” AND “security” |
| Low-middle income countries * | “Low-middle income countries” “LMIC” |
| Authors | Country | Type Article | Study Design | Sample | Emerging Themes |
|---|---|---|---|---|---|
| [2] | International | Peer review | Systematic Meta Analysis | N/A | NCD as the leading level 2 risk factor for death globally was high systolic blood pressure in 2019. Slow progress in LMICs |
| [1] | International | Peer review | Report | N/A | Recognizes NDCs as a major threat to public health globally. Calls on member states to take immediate actions to address NCDs through a global action plan |
| [24] | Sierra Leone | Peer review | Participatory mixed method | 28 | Rising cases in NCDs with poorly distributed health workforce and resources in a post-war and Ebola environment. |
| [6] | Senegal | Peer review | Mixed method | Varied | The threat of NCDs on workplace health and wellness and interventions to mitigate them. The study recognizes the role of private sector companies in improving cardiovascular population health in LMICs. |
| [16] | Thailand | Peer review | Case control study | Varied | Growing threats if selected NCDs among informal sector workers. Calls for the need to examine the risk factors, raise awareness, and strong collaboration between public health and workforce |
| [25] | South Africa | Peer review | Data extracted from a national survey | 1103 | NCDs among the youth. Youth diagnosed with NCDs require intervention before it escalates into other disease. |
| [3] | International | Peer review | Meta analysis | N/A | The increasing burden of cardiovascular diseases requires attention. Risk factors are modifiable. Calls for countries to invest in public health programs to promote healthy ageing. |
| [4] | International | Peer review | Review article | N/A | LMIC face a growing threat of NCDs. Important lessons can be learned from the management of infectious diseases. |
| [26] | Kenya | Peer review | Survey/Review | 6000 | This study examined NCDs and associated risk factors in Kenya. There are reported increase of death due to NCDs |
| [27] | International | Peer review | Meta-analysis of WHO data | N/A | The paper reported higher mortality due to NCDs in developing countries. Analysis of relative risk shows developing countries face a 1.5 times higher risk of premature NCD death than people living in high-income countries. There is therefore inequality in the distribution of NCD risks globally. |
| [28] | International | Peer reviewed | Symposium report | N/A | NCDs are reported as the largest death burden in LMICs with a call on all governments to tackle the pandemic. |
| [29] | Malawi | Peer review | Review paper | N/A | The rising incidence of NCD mortality in Malawi and sub-Sahara Africa. However, there is limited data on the associated risk factors. The paper advocates for health promotion to tackle the incidence. |
| [30] | International | Grey literature | Report | N/A | This global report on the prevention and control of NCDs captures data about NCD in 2014. It reports on the challenges, opportunities, and priorities in tackling NCDs. |
| [31] | International | Peer review | Meta analysis | N/A | This paper is an assessment of 84 environmental and occupational, behavioral, and metabolic risks in different locations. The increasing trend of NDC is a global public health challenge and an opportunity. |
| [32] | Iraq | Peer review | Qualitative study | 16 | This Iraqi study reported of the profound effect of conflict on NCDs. The analysis shows barriers to NCD care in a post-conflict environment. |
| [33] | Uganda | Peer review | Survey | 611 | The study reported of NDC as a growing concern in Uganda. It also analysis the risk factors within the country. Gender plays a role in NDC among the population. |
| [34] | International | Grey literature | Report | N/A | NCD is escalating globally with implications for public health and the economy. NCD affecting the business sector including agriculture, especially in South Asia. |
| [35] | International | Grey literature | Review report | N/A | The precarity on NCD is LMIC. This report acknowledged the workplace as influential in fostering good health, especially in LMIC. Adverse impact of NCD on the economy calls for actions to address the issue from the workplace environment. |
| [36] | International | Grey literature | Report | N/A | NCDs impact the quality of life of individuals, families, and the economy. Workplace health promotion targeting physical activity and diet can promote health among the workforces. |
| [37] | International | Grey literature | Report | N/A | The report acknowledges the growing danger of NCDs and its potential cost to economies, especially in developing countries. It draws a link between NDCs and economic prospects of a nation. The report encourages LMIC, to take necessary actions to address NCDs |
| [38] | International | Grey literature | Report | N/A | This report examines the risk of NCDs in LMICs. The report states: “The overall economic and social cost of NCDs vastly exceeds their direct medical costs”. Draws a strong correlation between NCDs and the economy. |
| [39] | International | Peer review | Review paper | N/A | The paper reported that NCDs long term macroeconomic impacts It affects the working population which impacts labour, saving and investment, resulting in human capital depreciation. |
| [40] | International | Grey literature | Report | N/A | The paper reports of NCDs, those affected—mainly the working group population, and the economic consequences—‘cost-of-illness microeconomic, and macroeconomic data. |
| [41] | International | Grey literature | Report | N/A | This fact sheet about NCDs draws on the labour force implications and calls on countries to take steps to prevent it. The report states “NCDs decrease the labour force, reduce productivity and reduce economic growth”. |
| [42] | Nigeria | Peer review | A cross-sectional survey | 606 | The paper reports a high prevalence of cardiometabolic risk factors among the workforce and recommends targeted preventive and therapeutic interventions among the working class. |
| [43] | International | Peer review | Report | N/A | This paper reports on the United Nations High-Level Meeting on Noncommunicable Diseases. It highlights the burden of NCDs and their associated economic cost, especially hypertension, and the actions to take to control it. |
| [44] | United States | Peer review | community-based participatory research | 150 | Mental health issues among the Police workforce |
| [45] | India | Peer review | Cross sectional survey | 982 | Prevalence of NDCs among Police personnel in the study area were low because they remained physically active. |
| [46] | Nigeria | Peer review | Cross sectional survey | 82 | NCD knowledge and attitude among the Armed Forces |
| [17] | Senegal | Peer review | Cross sectional survey | 1224 | Increasing of NCDs among the Senegalese Army highlighting the importance of risk factors. The paper argued for an intervention based on prevention and health promotion. |
| [47] | Iran | Peer review | Cross sectional survey | 341 | Prevalence of NCDs among the military |
| [48] | Kingdom of Saudi Arabia | Peer review | National survey | 10,500 | Prevalence of NCDs among the military |
| [49] | Kingdom of Saudi Arabia | Peer review | Cross sectional survey | 160 | Prevalence of NCDs among the Police—high proportion of overweight and obese police personnel. Increasing risk factors of NCDs |
| [50] | Indonesia | Peer review | Cross sectional survey | 978 | Increasing risk factor of hypertension and diabetes among the Police Force |
| Origin and scope | International | 17 |
| Africa | 9 | |
| South-East Asia | 3 | |
| Middle East | 4 | |
| North America | 1 | |
| Type of paper | Peer reviewed | 26 |
| Grey literature | 8 | |
| Method | Primary research and national surveys | 16 |
| Reviews and meta-analysis | 8 | |
| Reports and unclassified | 10 |
| Emerging Features of NCDs in LMICS | Impact of NCDs in LMICs |
|---|---|
| Higher mortality rate from NCDs |
| Workforce Sector | NCD Impact on the Workforce |
|---|---|
| Absenteeism Loss of skills Disability Death Rising cost of healthcare |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Doh, D.; Dahwa, R.; Renzaho, A.M.N. A Scoping Review of Non-Communicable Diseases among the Workforce as a Threat to Global Peace and Security in Low-Middle Income Countries. Int. J. Environ. Res. Public Health 2024, 21, 1143. https://doi.org/10.3390/ijerph21091143
Doh D, Dahwa R, Renzaho AMN. A Scoping Review of Non-Communicable Diseases among the Workforce as a Threat to Global Peace and Security in Low-Middle Income Countries. International Journal of Environmental Research and Public Health. 2024; 21(9):1143. https://doi.org/10.3390/ijerph21091143
Chicago/Turabian StyleDoh, Daniel, Rumbidzai Dahwa, and Andre M. N. Renzaho. 2024. "A Scoping Review of Non-Communicable Diseases among the Workforce as a Threat to Global Peace and Security in Low-Middle Income Countries" International Journal of Environmental Research and Public Health 21, no. 9: 1143. https://doi.org/10.3390/ijerph21091143






