Phase Ib Study of Atezolizumab Plus Interferon-α with or without Bevacizumab in Patients with Metastatic Renal Cell Carcinoma and Other Solid Tumors
Abstract
:1. Introduction
2. Materials and Methods
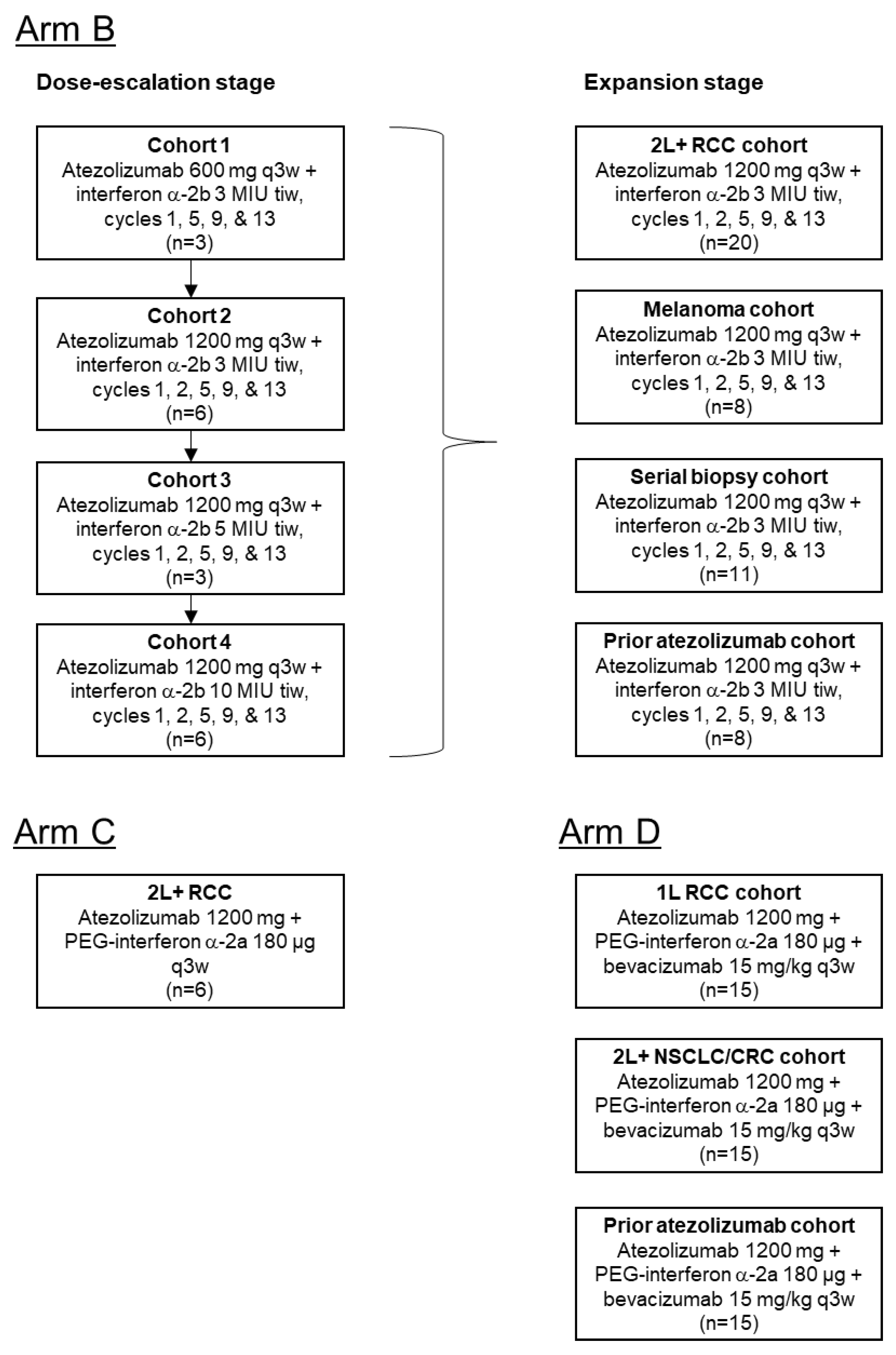
2.1. Study Design
2.2. Patients
2.3. Treatment
2.4. Endpoints and Assessments
3. Results
3.1. Patients
3.2. Dose Escalation
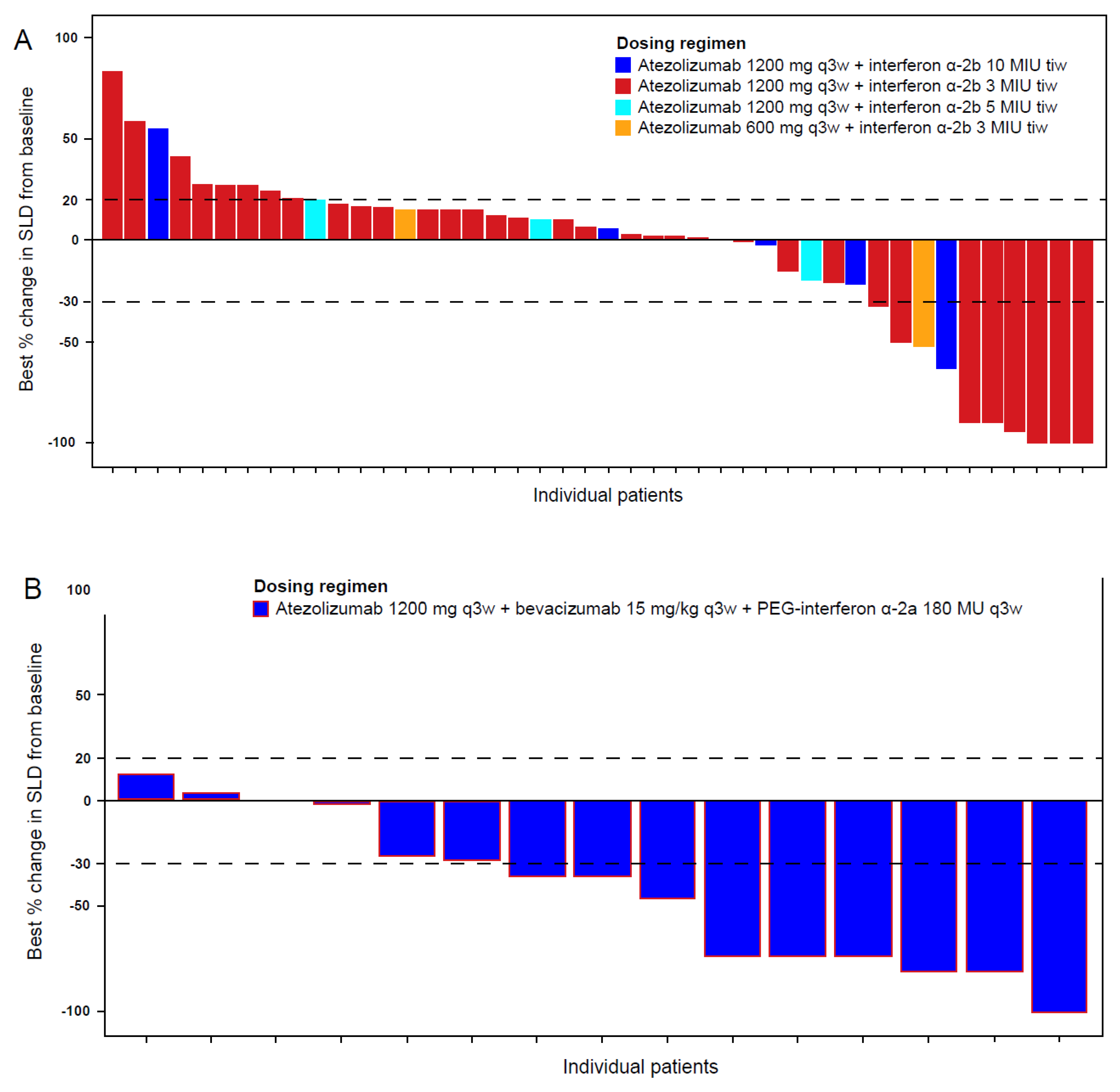
3.3. Safety and Activity: Arm B (Atezolizumab plus Interferon α-2b)
3.4. Safety and Activity: Arm C (Atezolizumab Plus PEG-Interferon α-2a)
3.5. Safety and Activity: Arm D (Atezolizumab Plus PEG-Interferon α-2a and Bevacizumab)
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Aapro, M.S. Advances in systemic treatment of malignant melanoma. Eur. J. Cancer 1993, 29, 613–617. [Google Scholar] [CrossRef]
- Wang, X.; Lopez, R.; Luchtel, R.A.; Hafizi, S.; Gartrell, B.; Shenoy, N. Immune evasion in renal cell carcinoma: Biology, clinical translation, future directions. Kidney Int. 2021, 99, 75–85. [Google Scholar] [CrossRef] [PubMed]
- Hodi, F.S.; Sileni, V.C.; Gonzalez, R.; Grob, J.-J.; Rutkowski, P.; Cowey, C.L.; Lao, C.D.; Schadendorf, D.; Wagstaff, J.; Dummer, R.; et al. Nivolumab plus ipilimumab or nivolumab alone versus ipilimumab alone in advanced melanoma (CheckMate 067): 4-year outcomes of a multicentre, randomised, phase 3 trial. Lancet Oncol. 2018, 19, 1480–1492. [Google Scholar] [CrossRef]
- Hodi, F.S.; O’Day, S.J.; McDermott, D.F.; Weber, R.W.; Sosman, J.A.; Haanen, J.B.; Gonzalez, R.; Robert, C.; Schadendorf, D.; Hassel, J.C.; et al. Improved Survival with Ipilimumab in Patients with Metastatic Melanoma. N. Engl. J. Med. 2010, 363, 711–723. [Google Scholar] [CrossRef]
- Motzer, R.J.; Escudier, B.; McDermott, D.F.; George, S.; Hammers, H.J.; Srinivas, S.; Tykodi, S.S.; Sosman, J.A.; Procopio, G.; Plimack, E.R.; et al. Nivolumab versus Everolimus in Advanced Renal-Cell Carcinoma. N. Engl. J. Med. 2015, 373, 1803–1813. [Google Scholar] [CrossRef] [PubMed]
- Motzer, R.J.; Penkov, K.; Haanen, J.; Rini, B.; Albiges, L.; Campbell, M.T.; Venugopal, B.; Kollmannsberger, C.; Negrier, S.; Uemura, M.; et al. Avelumab plus Axitinib versus Sunitinib for Advanced Renal-Cell Carcinoma. N. Engl. J. Med. 2019, 380, 1103–1115. [Google Scholar] [CrossRef] [PubMed]
- Motzer, R.J.; Tannir, N.M.; McDermott, D.F.; Aren Frontera, O.; Melichar, B.; Choueiri, T.K.; Plimack, E.R.; Barthélémy, P.; Porta, C.; George, S.; et al. Nivolumab plus Ipilimumab versus Sunitinib in Advanced Renal-Cell Carcinoma. N. Engl. J. Med. 2018, 378, 1277–1290. [Google Scholar] [CrossRef]
- Ascierto, P.A.; Long, G.V.; Robert, C.; Brady, B.; Dutriaux, C.; Di Giacomo, A.M. Survival Outcomes in Patients With Previously Untreated BRAF Wild-Type Advanced Melanoma Treated With Nivolumab Therapy: Three-Year Follow-up of a Randomized Phase 3 Trial. JAMA Oncol. 2019, 5, 187–194. [Google Scholar] [CrossRef] [Green Version]
- Schachter, J.; Ribas, A.; Long, G.V.; Arance, A.; Grob, J.-J.; Mortier, L.; Daud, A.; Carlino, M.S.; McNeil, C.; Lotem, M.; et al. Pembrolizumab versus ipilimumab for advanced melanoma: Final overall survival results of a multicentre, randomised, open-label phase 3 study (KEYNOTE-006). Lancet 2017, 390, 1853–1862. [Google Scholar] [CrossRef]
- Rini, B.I.; Plimack, E.R.; Stus, V.; Gafanov, R.; Hawkins, R.; Nosov, D.; Pouliot, F.; Alekseev, B.; Soulières, D.; Melichar, B.; et al. Pembrolizumab plus Axitinib versus Sunitinib for Advanced Renal-Cell Carcinoma. N. Engl. J. Med. 2019, 380, 1116–1127. [Google Scholar] [CrossRef] [PubMed]
- Rizzo, A.; Mollica, V.; Santoni, M.; Ricci, A.D.; Rosellini, M.; Marchetti, A.; Montironi, R.; Ardizzoni, A.; Massari, F. Impact of Clinicopathological Features on Survival in Patients Treated with First-line Immune Checkpoint Inhibitors Plus Tyrosine Kinase Inhibitors for Renal Cell Carcinoma: A Meta-analysis of Randomized Clinical Trials. Eur. Urol. Focus 2021. [Google Scholar] [CrossRef]
- Massari, F.; Rizzo, A.; Mollica, V.; Rosellini, M.; Marchetti, A.; Ardizzoni, A.; Santoni, M. Immune-based combinations for the treatment of metastatic renal cell carcinoma: A meta-analysis of randomised clinical trials. Eur. J. Cancer 2021, 154, 120–127. [Google Scholar] [CrossRef] [PubMed]
- Khetani, V.V.; Portal, D.E.; Shah, M.R.; Mayer, T.; Singer, E.A. Combination drug regimens for metastatic clear cell renal cell carcinoma. World J. Clin. Oncol. 2020, 11, 541–562. [Google Scholar] [CrossRef]
- Aricò, E.; Castiello, L.; Capone, I.; Gabriele, L.; Belardelli, F. Type I Interferons and Cancer: An Evolving Story Demanding Novel Clinical Applications. Cancers 2019, 11, 1943. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Seliger, B.; Ruiz-Cabello, F.; Garrido, F. Chapter 7 IFN Inducibility of Major Histocompatibility Antigens in Tumors. Adv. Cancer Res. 2008, 101, 249–276. [Google Scholar] [CrossRef]
- Blank, C.; Brown, I.; Peterson, A.C.; Spiotto, M.; Iwai, Y.; Honjo, T.; Gajewski, T.F. PD-L1/B7H-1 inhibits the effector phase of tumor rejection by T cell receptor (TCR) transgenic CD8+ T cells. Cancer Res. 2004, 64, 1140–1145. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Terawaki, S.; Chikuma, S.; Shibayama, S.; Hayashi, T.; Yoshida, T.; Okazaki, T.; Honjo, T. IFN-α Directly Promotes Programmed Cell Death-1 Transcription and Limits the Duration of T Cell-Mediated Immunity. J. Immunol. 2011, 186, 2772–2779. [Google Scholar] [CrossRef] [PubMed]
- Davar, D.; Wang, H.; Chauvin, J.-M.; Pagliano, O.; Fourcade, J.J.; Ka, M.; Menna, C.; Rose, A.; Sander, C.; Borhani, A.A.; et al. Phase Ib/II Study of Pembrolizumab and Pegylated-Interferon Alfa-2b in Advanced Melanoma. J. Clin. Oncol. 2018, 36, 3450. [Google Scholar] [CrossRef]
- Escudier, B.; Pluzanska, A.; Koralewski, P.; Ravaud, A.; Bracarda, S.; Szczylik, C.; Chevreau, C.; Filipek, M.; Melichar, B.; Bajetta, E.; et al. Bevacizumab plus interferon alfa-2a for treatment of metastatic renal cell carcinoma: A randomised, double-blind phase III trial. Lancet 2007, 370, 2103–2111. [Google Scholar] [CrossRef]
- Bouzin, C.; Brouet, A.; De Vriese, J.; Dewever, J.; Feron, O. Effects of Vascular Endothelial Growth Factor on the Lymphocyte-Endothelium Interactions: Identification of Caveolin-1 and Nitric Oxide as Control Points of Endothelial Cell Anergy. J. Immunol. 2007, 178, 1505–1511. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Huang, Y.; Chen, X.; Dikov, M.M.; Novitskiy, S.V.; Mosse, C.A.; Yang, L.; Carbone, D.P. Distinct roles of VEGFR-1 and VEGFR-2 in the aberrant hematopoiesis associated with elevated levels of VEGF. Blood 2007, 110, 624–631. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hirsch, L.; Flippot, R.; Escudier, B.; Albiges, L. Immunomodulatory Roles of VEGF Pathway Inhibitors in Renal Cell Carcinoma. Drugs 2020, 80, 1169–1181. [Google Scholar] [CrossRef] [PubMed]
- Wallin, J.J.; Bendell, J.C.; Funke, R.; Sznol, M.; Korski, K.; Jones, S.; Hernandez, G.; Mier, J.; He, X.; Hodi, F.S.; et al. Atezolizumab in combination with bevacizumab enhances antigen-specific T-cell migration in metastatic renal cell carcinoma. Nat. Commun. 2016, 7, 12624. [Google Scholar] [CrossRef] [PubMed]
- McDermott, D.F.; Huseni, M.A.; Atkins, M.B.; Motzer, R.J.; Rini, B.I.; Escudier, B.; Fong, L.; Joseph, R.W.; Pal, S.K.; Reeves, J.A.; et al. Clinical activity and molecular correlates of response to atezolizumab alone or in combination with bevacizumab versus sunitinib in renal cell carcinoma. Nat Med. 2018, 24, 749–757. [Google Scholar] [CrossRef]
- Rini, B.I.; Powles, T.; Atkins, M.B.; Escudier, B.; McDermott, D.F.; Suarez, C.; Bracarda, S.; Stadler, W.M.; Donskov, F.; Lee, J.L.; et al. Atezolizumab plus bevacizumab versus sunitinib in patients with previously untreated metastatic renal cell carcinoma (IMmotion151): A multicentre, open-label, phase 3, randomised controlled trial. Lancet 2019, 393, 2404–2415. [Google Scholar] [CrossRef]
- Taleb, K.; Auffray, C.; Villefroy, P.; Pereira, A.; Hosmalin, A.; Gaudry, M.; Le Bon, A. Chronic Type I IFN Is Sufficient To Promote Immunosuppression through Accumulation of Myeloid-Derived Suppressor Cells. J. Immunol. 2016, 198, 1156–1163. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sarasin-Filipowicz, M.; Wang, X.; Yan, M.; Duong, F.H.T.; Poli, V.; Hilton, D.J.; Zhang, D.-E.; Heim, M.H. Alpha interferon induces long-lasting refractoriness of JAK-STAT signaling in the mouse liver through induction of USP18/UBP43. Mol. Cell. Biol. 2009, 29, 4841–4851. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Heathcote, E.J.; Shiffman, M.L.; Cooksley, W.G.E.; Dusheiko, G.M.; Lee, S.S.; Balart, L.; Reindollar, R.; Reddy, R.K.; Wright, T.L.; Lin, A.; et al. Peginterferon Alfa-2a in Patients with Chronic Hepatitis C and Cirrhosis. N. Engl. J. Med. 2000, 343, 1673–1680. [Google Scholar] [CrossRef] [Green Version]
- Zeuzem, S.; Feinman, S.V.; Rasenack, J.; Heathcote, E.J.; Lai, M.-Y.; Gane, E.; O’Grady, J.; Reichen, J.; Diago, M.; Lin, A.; et al. Peginterferon Alfa-2a in Patients with Chronic Hepatitis C. N. Engl. J. Med. 2000, 343, 1666–1672. [Google Scholar] [CrossRef] [Green Version]
- McDermott, D.F.; Sosman, J.A.; Sznol, M.; Massard, C.; Gordon, M.S.; Hamid, O.; Powderly, J.D.; Infante, J.R.; Fassò, M.; Wang, Y.V.; et al. Atezolizumab, an Anti–Programmed Death-Ligand 1 Antibody, in Metastatic Renal Cell Carcinoma: Long-Term Safety, Clinical Activity, and Immune Correlates From a Phase Ia Study. J. Clin. Oncol. 2016, 34, 833–842. [Google Scholar] [CrossRef] [PubMed]
- Finn, R.S.; Qin, S.; Ikeda, M.; Galle, P.R.; Ducreux, M.; Kim, T.-Y.; Kudo, M.; Breder, V.; Merle, P.; Kaseb, A.O.; et al. Atezolizumab plus Bevacizumab in Unresectable Hepatocellular Carcinoma. N. Engl. J. Med. 2020, 382, 1894–1905. [Google Scholar] [CrossRef] [PubMed]
- Socinski, M.A.; Jotte, R.M.; Cappuzzo, F.; Orlandi, F.; Stroyakovskiy, D.; Nogami, N.; Rodríguez-Abreu, D.; Moro-Sibilot, D.; Thomas, C.A.; Barlesi, F.; et al. Atezolizumab for First-Line Treatment of Metastatic Nonsquamous NSCLC. N. Engl. J. Med. 2018, 378, 2288–2301. [Google Scholar] [CrossRef] [PubMed]
- Patel, S.P.; Kurzrock, R. PD-L1 Expression as a Predictive Biomarker in Cancer Immunotherapy. Mol. Cancer Ther. 2015, 14, 847–856. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Characteristic | Arm B | Arm C | Arm D |
|---|---|---|---|
| Atezo + IFNα | Atezo + PEG-IFNα | Atezo + PEG-IFNα + Bev | |
| (n = 65) | (n = 6) | (n = 45) | |
| Tumor type, n (%) | |||
| RCC | 50 (76.9) | 6 (100) | 21 (46.7) |
| Melanoma | 14 (21.5) | 0 | 3 (6.7) |
| CRC | 0 | 0 | 14 (31.1) |
| NSCLC | 1 (1.5) | 0 | 7 (15.6) |
| Age group, n (%) | |||
| <65 y | 39 (60.0) | 2 (33.3) | 30 (66.7) |
| ≥65 y | 26 (40.0) | 4 (66.7) | 15 (33.3) |
| Sex, n (%) | |||
| Male | 56 (86.2) | 6 (100) | 27 (60.0) |
| Female | 9 (13.8) | 0 | 18 (40.0) |
| Race, n (%) | |||
| Black or African American | 3 (4.6) | 0 | 7 (15.6) |
| White | 60 (92.3) | 6 (100) | 32 (71.1) |
| Asian | 1 (1.5) | 0 | 4 (8.9) |
| Unknown | 1 (1.5) | 0 | 2 (4.4) |
| ECOG performance status, n (%) | |||
| 0 | 49 (75.4) | 3 (50.0) | 32 (72.7) a |
| 1 | 16 (24.6) | 3 (50.0) | 12 (27.3) a |
| Prior systemic therapy, n (%) | |||
| Yes | 55 (84.6) | 6 (100) | 30 (66.7) |
| No | 10 (15.4) | 0 | 15 (33.3) |
| Prior cancer surgery, n (%) | |||
| Yes | 61 (93.8) | 6 (100) | 26 (57.8) |
| No | 4 (6.2) | 0 | 19 (42.2) |
| Prior radiotherapy, n (%) | |||
| Yes | 36 (55.4) | 3 (50.0) | 16 (35.6) |
| No | 29 (44.6) | 3 (50.0) | 29 (64.4) |
| PD-L1 IC score, n (%) b | |||
| IC0 | 30 (46.2) | 4 (66.7) | 27 (60.0) |
| IC1/2/3 | 26 (40.0) | 1 (16.7) | 3 (6.7) |
| Unknown | 9 (13.8) | 1 (16.7) | 15 (33.3) |
| PD-L1 TC score, n (%) c | |||
| TC0 | 51 (78.5) | 5 (83.3) | 28 (62.2) |
| TC1/2/3 | 5 (7.7) | 0 | 2 (4.4) |
| Unknown | 9 (13.8) | 1 (16.7) | 15 (33.3) |
| Patients with at Least 1, n (%) | Arm B | Arm C | Arm D |
|---|---|---|---|
| Atezo + IFNα | Atezo + PEG-IFNα | Atezo + PEG-IFNα + Bev | |
| (n = 65) | (n = 6) | (n = 45) | |
| Treatment-emergent AE of any grade | 65 (100) | 6 (100) | 45 (100) |
| Treatment-emergent AE with fatal outcome | 3 (4.6) | 0 | 1 (2.2) |
| Serious treatment-emergent AE | 19 (29.2) | 4 (66.7) | 19 (42.2) |
| Treatment-emergent Grade 3–5 AE | 25 (38.5) | 3 (50.0) | 28 (62.2) |
| AE leading to drug withdrawal | |||
| AE leading to atezo withdrawal | 3 (4.6) | 1 (16.7) | 1 (2.2) |
| AE leading to IFNα withdrawal | 3 (4.6) | – | – |
| AE leading to PEG-IFNα withdrawal | – | 1 (16.7) | 2 (4.4) |
| AE leading to bev withdrawal | – | – | 8 (17.8) |
| AE leading to drug dose modification/interruption | |||
| AE leading to atezo dose interruption | 13 (20.0) | 2 (33.3) | 7 (15.6) |
| AE leading to IFNα dose modification/interruption | 7 (10.8) | – | – |
| AE leading to PEG-IFNα dose modification/interruption | – | 2 (33.3) | 6 (13.3) |
| AE leading to bev dose interruption | – | – | 11 (24.4) |
| AE, n (%) | Arm B | Arm C | Arm D | ||||
|---|---|---|---|---|---|---|---|
| Atezo + IFNα | Atezo + PEG-IFNα | Atezo + PEG-IFNα + Bev | |||||
| (n = 65) | (n = 6) | (n = 45) | |||||
| Atezo | IFNα | Atezo | PEG-IFNα | Atezo | PEG-IFNα | Bev | |
| Any treatment-related AE | 44 (67.7) | 60 (92.3) | 6 (100) | 6 (100) | 38 (84.4) | 38 (84.4) | 39 (86.7) |
| Fatigue | 18 (27.7) | 25 (38.5) | 2 (33.3) | 2 (33.3) | 23 (51.1) | 25 (55.6) | 16 (35.6) |
| Chills | 12 (18.5) | 27 (41.5) | 0 | 0 | 6 (13.3) | 6 (13.3) | 5 (11.1) |
| Pyrexia | 8 (12.3) | 23 (35.4) | 0 | 1 (16.7) | 7 (15.6) | 8 (17.8) | 5 (11.1) |
| Arthralgia | 11 (16.9) | 9 (13.8) | 0 | 0 | 4 (8.9) | 8 (17.8) | 1 (2.2) |
| Myalgia | 7 (10.8) | 14 (21.5) | 0 | 0 | 6 (13.3) | 4 (8.9) | 2 (4.4) |
| Headache | 4 (6.2) | 6 (9.2) | 1 (16.7) | 1 (16.7) | 5 (11.1) | 5 (11.1) | 5 (11.1) |
| Nausea | 5 (7.7) | 7 (10.8) | 0 | 1 (16.7) | 6 (13.3) | 7 (15.6) | 6 (13.3) |
| Influenza-like illness | 3 (4.6) | 8 (12.3) | 0 | 0 | 5 (11.1) | 9 (20.0) | 4 (8.9) |
| Proteinuria | 1 (1.5) | 1 (1.5) | 0 | 0 | 1 (2.2) | 1 (2.2) | 12 (26.7) |
| Hypertension | 0 | 0 | 0 | 0 | 0 | 1 (2.2) | 10 (22.2) |
| Hypothyroidism | 8 (12.3) | 2 (3.1) | 1 (16.7) | 0 | 5 (11.1) | 1 (2.2) | 0 |
| Cough | 2 (3.1) | 2 (3.1) | 1 (16.7) | 1 (16.7) | 1 (2.2) | 2 (4.4) | 1 (2.2) |
| Epistaxis | 0 | 1 (1.5) | 0 | 0 | 0 | 0 | 5 (11.1) |
| Eyelid ptosis | 0 | 0 | 1 (16.7) | 1 (16.7) | 0 | 0 | 0 |
| Blood creatinine phosphokinase increase | 0 | 0 | 1 (16.7) | 1 (16.7) | 0 | 0 | 0 |
| Transaminase increase | 0 | 0 | 1 (16.7) | 1 (16.7) | 0 | 0 | 0 |
| Decreased appetite | 4 (6.2) | 5 (7.7) | 1 (16.7) | 1 (16.7) | 2 (4.4) | 4 (8.9) | 2 (4.4) |
| Myasthenia gravis | 0 | 0 | 1 (16.7) | 1 (16.7) | 0 | 0 | 0 |
| Acute respiratory failure | 0 | 0 | 1 (16.7) | 1 (16.7) | 0 | 0 | 0 |
| Hyperthyroidism | 0 | 0 | 1 (16.7) | 1 (16.7) | 2 (4.4) | 0 | 0 |
| Vomiting | 3 (4.6) | 4 (6.2) | 1 (16.7) | 1 (16.7) | 0 | 1 (2.2) | 1 (2.2) |
| Muscular weakness | 0 | 1 (1.5) | 1 (16.7) | 1 (16.7) | 1 (2.2) | 1 (2.2) | 1 (2.2) |
| Pneumonia | 0 | 0 | 1 (16.7) | 1 (16.7) | 0 | 0 | 0 |
| Hypoxia | 0 | 0 | 1 (16.7) | 0 | 0 | 0 | 0 |
| Respiratory acidosis | 0 | 0 | 1 (16.7) | 0 | 0 | 0 | 0 |
| Tumor-associated fever | 0 | 0 | 1 (16.7) | 0 | 0 | 0 | 0 |
| Anemia | 3 (4.6) | 5 (7.7) | 0 | 1 (16.7) | 3 (6.7) | 3 (6.7) | 2 (4.4) |
| Infusion-related reaction | 1 (1.5) | 0 | 0 | 1 (16.7) | 1 (2.2) | 0 | 0 |
| Arm B Atezo + IFNα | Arm C Atezo + PEG-IFNα (n = 6) | Arm D Atezo + PEG-IFNα + Bev | ||||
|---|---|---|---|---|---|---|
| All Patients (n = 65) | CPI-Naive RCC (n = 45) | Cohort 1: 1L RCC (n = 15) | Cohort 2: 2L+ CRC/NSCLC (n = 15) | Cohort 3: Prior CPI (n = 15) | ||
| Response, n (%) [95% CI] | ||||||
| Objective response rate | 13 (20.0) | 8 (17.8) | 0 | 7 (46.7) | 2 (13.3) | 2 (13.3) |
| [10.3–29.7] | [6.6–28.9] | [0.0–0.0] | [21.4–71.9] | [0.0–30.5] | [0.0–30.5] | |
| Complete response | 1 (1.5) | 1 (2.2) | 0 | 1 (6.7) | 0 | 0 |
| [0.0–4.5] | [0.0–6.5] | [0.0–0.0] | [0.0–19.3] | [0.0–0.0] | [0.0–0.0] | |
| Partial response | 12 (18.5) | 7 (15.6) | 0 | 6 (40.0) | 2 (13.3) | 2 (13.3) |
| [9.0–27.9] | [5.0–26.1] | [0.0–0.0] | [15.2–64.8] | [0.0–30.5] | [0.0–30.5] | |
| Stable disease | 30 (46.2) | 20 (44.4) | 2 (33.3) | 7 (46.7) | 8 (53.3) | 11 (73.3) |
| [34.0–58.3] | [29.9–59.0] | [0.0–71.0] | [21.4–71.9] | [28.1–78.6] | [50.9–95.7] | |
| Progressive disease | 20 (30.8) | 16 (35.6) | 3 (50.0) | 1 (6.7) | 5 (33.3) | 2 (13.3) |
| [19.6–42.0] | [21.6–49.5] | [10.0–90.0] | [0.0–19.3] | [9.5–57.2] | [0.0–30.5] | |
| Missing/unevaluable | 2 (3.1) | 1 (2.2) | 1 (16.7) | 0 | 0 | 0 |
| Duration of response | n = 13 | n = 8 | n = 0 | n = 7 | n = 2 | n = 2 |
| Median, month [95% CI] | 28.8 [16.8-NE] | 24.9 [3.7-NE] | – | 12.5 [4.5-NE] | NE [11.3-NE] | NE [3.1-NE] |
| Range | 2.8–51.8 a | 2.8–50.5 a | – | 2.8–25.8 a | 11.3–13.8 a | 3.1–19.4 a |
| Progression-free survival | ||||||
| Patients with event, n (%) | 58 (89.2) | 41 (91.1) | 6 (100) | 10 (66.7) | 13 (86.7) | 12 (80.0) |
| Median, month [95% CI] | 4.1 [3.0–5.5] | 3.2 [2.8–5.5] | 1.9 [1.2–4.2] | 9.0 [4.1-NE] | 3.2 [2.5–4.3] | 6.9 [4.4–8.4] |
| Range | 1–57 a | 1–52 a | 1–9 | 1–28 a | 1–25 a | 1–28 a |
| Landmark rate, % [95% CI] | ||||||
| 6 months | 33.9 [22.3–45.4] | 33.3 [19.6–47.1] | 16.7 [0.0–46.5] | 71.8 [48.3–95.3] | 26.7 [4.3–49.0] | 66.7 [42.8–90.5] |
| 1 y | 24.6 [14.1–35.1] | 20.0 [8.3–31.7] | NE | 43.1 [17.1–69.0] | 20.0 [0.0–40.2] | 17.8 [0.0–38.4] |
| 2 y | 13.3 [4.9–21.7] | 10.4 [1.2–19.6] | NE | 28.7 [5.0–52.4] | 13.3 [0.0–30.5] | 17.8 [0.0–38.4] |
| Overall survival | ||||||
| Patients with event, n (%) | 40 (61.5) | 30 (66.7) | 2 (33.3) | 2 (13.3) | 10 (66.7) | 8 (53.3) |
| Median, month [95% CI] | 29.9 [21.9–41.9] | 26.3 [15.6–37.6] | NE [2.4-NE] | NE [17.7-NE] | 12.7 [5.5–19.9] | 13.9 [10.9-NE] |
| Range | 1–59 a | 3 a–53 a | 1 a–26 a | 5 a–30 a | 3–26 a | 2–28 a |
| Landmark rate, % [95% CI] | ||||||
| 6 months | 90.6 [83.4–97.8] | 93.1 [85.5–100] | 80.0 [44.9–100] | 100 [100–100] | 72.2 [49.0–95.4] | 80.0 [59.8–100] |
| 1 y | 77.8 [67.6–88.1] | 74.4 [61.3–87.4] | 80.0 [44.9–100] | 92.9 [79.4–100] | 50.6 [24.4–76.7] | 66.7 [42.8–90.5] |
| 2 y | 54.6 [42.1–67.1] | 52.8 [37.7–67.9] | 60.0 [17.1–100] | 77.4 [47.5–100] | 16.2 [0.0–42.4] | 44.4 [18.5–70.4] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Blank, C.U.; Wong, D.J.; Ho, T.H.; Bauer, T.M.; Lee, C.B.; Bene-Tchaleu, F.; Zhu, J.; Zhang, X.; Cha, E.; Sznol, M. Phase Ib Study of Atezolizumab Plus Interferon-α with or without Bevacizumab in Patients with Metastatic Renal Cell Carcinoma and Other Solid Tumors. Curr. Oncol. 2021, 28, 5466-5479. https://doi.org/10.3390/curroncol28060455
Blank CU, Wong DJ, Ho TH, Bauer TM, Lee CB, Bene-Tchaleu F, Zhu J, Zhang X, Cha E, Sznol M. Phase Ib Study of Atezolizumab Plus Interferon-α with or without Bevacizumab in Patients with Metastatic Renal Cell Carcinoma and Other Solid Tumors. Current Oncology. 2021; 28(6):5466-5479. https://doi.org/10.3390/curroncol28060455
Chicago/Turabian StyleBlank, Christian U., Deborah J. Wong, Thai H. Ho, Todd M. Bauer, Carrie B. Lee, Fabiola Bene-Tchaleu, Jing Zhu, Xiaosong Zhang, Edward Cha, and Mario Sznol. 2021. "Phase Ib Study of Atezolizumab Plus Interferon-α with or without Bevacizumab in Patients with Metastatic Renal Cell Carcinoma and Other Solid Tumors" Current Oncology 28, no. 6: 5466-5479. https://doi.org/10.3390/curroncol28060455
APA StyleBlank, C. U., Wong, D. J., Ho, T. H., Bauer, T. M., Lee, C. B., Bene-Tchaleu, F., Zhu, J., Zhang, X., Cha, E., & Sznol, M. (2021). Phase Ib Study of Atezolizumab Plus Interferon-α with or without Bevacizumab in Patients with Metastatic Renal Cell Carcinoma and Other Solid Tumors. Current Oncology, 28(6), 5466-5479. https://doi.org/10.3390/curroncol28060455





