The Anatomy of a Hybrid In-Person and Virtual Sexual Health Clinic in Oncology
Abstract
1. Introduction
1.1. Prevalence and Severity of Impact on Health-Related Quality of Life
1.1.1. Impact on Physical Wellbeing
1.1.2. Impact on Psychological Wellbeing
1.1.3. Impact on Interpersonal Wellbeing
1.1.4. Barriers to Sexual Healthcare in Oncology
2. Materials and Methods
Previous Work
3. Results
3.1. The Sexual Health Clinic (SHC)
3.1.1. Patient Population
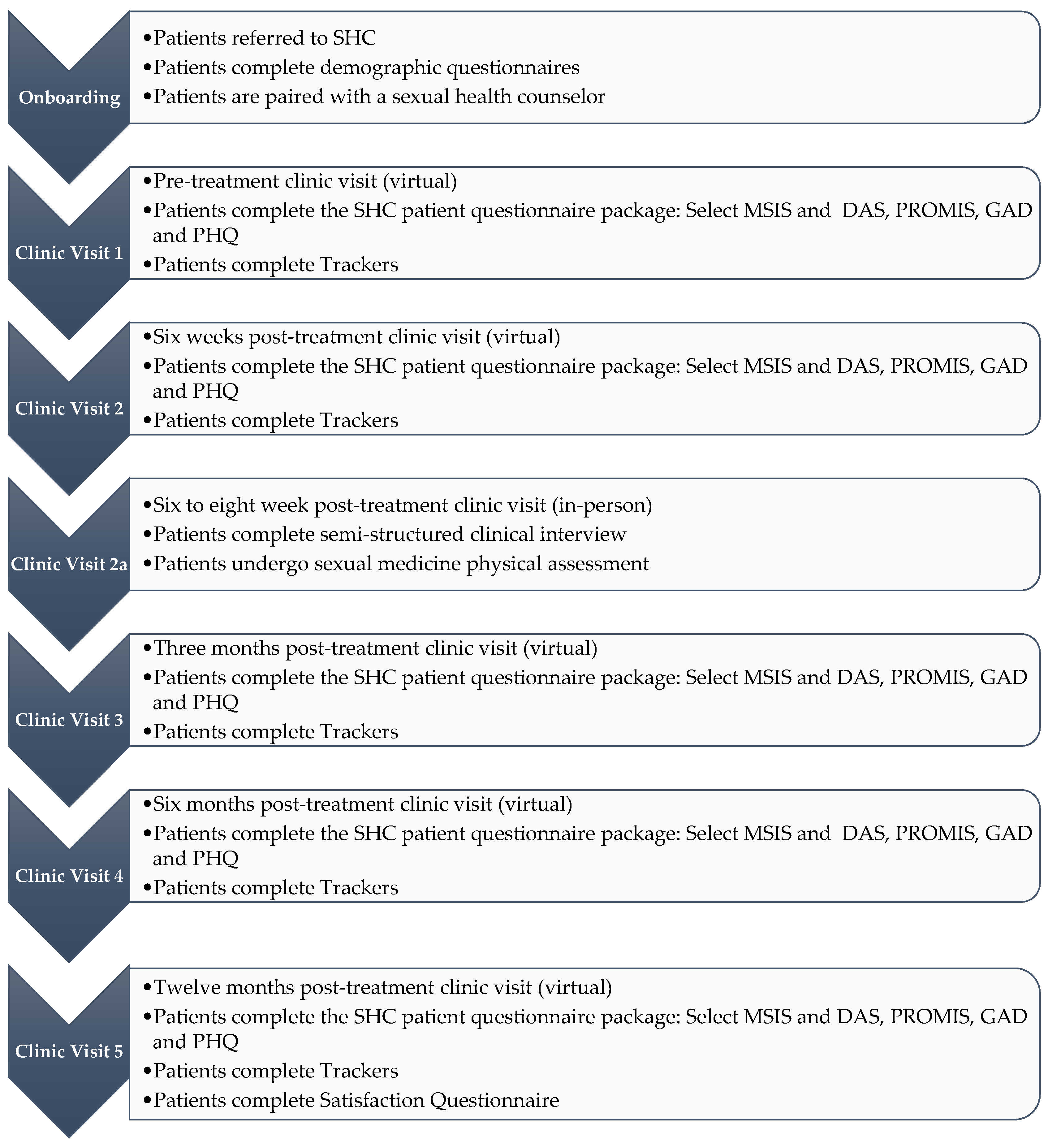
3.1.2. Clinical Visiting Program
3.1.3. Assessment
3.1.4. Intervention
3.1.5. Educational Modules
3.1.6. Virtual Sexual Health Counselors
3.1.7. Face-to-Face Clinical Visits
3.1.8. Quality Assurance and Research Program
3.2. SHC Implementation
4. Discussion
4.1. SHC and Accessibility
4.2. SHC and Affordability
4.3. SHC and Oncologist Training and Time
4.4. SHC and Digital Health Engagement and Effectiveness
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Barbera, L.; Zwaal, C.; Elterman, D.; McPherson, K.; Wolfman, W.; Katz, A.; Matthew, A. Interventions to address sexual problems in people with cancer guideline development group. Interventions to address sexual problems in people with cancer. Curr. Oncol. 2017, 24, 192–200. [Google Scholar] [CrossRef]
- Bober, S.L.; Varela, V.S. Sexuality in Adult Cancer Survivors: Challenges and Intervention. J. Clin. Oncol. 2012, 30, 3712–3719. [Google Scholar] [CrossRef]
- Katz, A.; Agrawal, L.S.; Sirohi, B. Sexuality After Cancer as an Unmet Need: Addressing Disparities, Achieving Equality. Am. Soc. Clin. Oncol. Educ. Book 2022, 42, 11–17. [Google Scholar] [CrossRef] [PubMed]
- Krouwel, E.M.; Albers, L.F.; Nicolai, M.P.J.; Putter, H.; Osanto, S.; Pelger, R.C.M.; Elzevier, H.W. Discussing Sexual Health in the Medical Oncologist’s Practice: Exploring Current Practice and Challenges. J. Cancer Educ. 2019, 35, 1072–1088. [Google Scholar] [CrossRef]
- Canadian Cancer Statistics Advisory in collaboration with the Canadian Cancer Society, Statistics Canada and the Public Health Agency of Canada. Canadian Cancer Statistics: A 2022 Special Report on Cancer Prevalence. Canadian Cancer Society. 2022. Available online: https://cancer.ca/Canadian-Cancer-Statistics-2022-EN (accessed on 5 December 2022).
- Bessa, A.; Martin, R.; Häggström, C.; Enting, D.; Amery, S.; Khan, M.S.; Cahill, F.; Wylie, H.; Broadhead, S.; Chatterton, K.; et al. Unmet needs in sexual health in bladder cancer patients: A systematic review of the evidence. BMC Urol. 2020, 20, 1–16. [Google Scholar] [CrossRef] [PubMed]
- Del Pup, L. Management of vaginal dryness and dyspareunia in estrogen sensitive cancer patients. Gynecol. Endocrinol. 2012, 28, 740–745. [Google Scholar] [CrossRef] [PubMed]
- Stavraka, C.; Ford, A.; Ghaem-Maghami, S.; Crook, T.; Agarwal, R.; Gabra, H.; Blagden, S. A study of symptoms described by ovarian cancer survivors. Gynecol. Oncol. 2012, 125, 59–64. [Google Scholar] [CrossRef]
- Goossens-Laan, C.A.; Kil, P.J.M.; Bosch, J.L.H.R.; De Vries, J. Pre-diagnosis quality of life (QoL) in patients with hematuria: Comparison of bladder cancer with other causes. Qual. Life Res. 2012, 22, 309–315. [Google Scholar] [CrossRef]
- Matthew, A.; Lutzky-Cohen, N.; Jamnicky, L.; Currie, K.; Gentile, A.; Mina, D.S.; Fleshner, N.; Finelli, A.; Hamilton, R.; Kulkarni, G.; et al. The Prostate Cancer Rehabilitation Clinic: A Biopsychosocial Clinic for Sexual Dysfunction after Radical Prostatectomy. Curr. Oncol. 2018, 25, 393–402. [Google Scholar] [CrossRef]
- White, I.D.; Wilson, J.; Aslet, P.; Baxter, A.B.; Birtle, A.; Challacombe, B.; Coe, J.; Grover, L.; Payne, H.; Russell, S.; et al. Development of UK guidance on the management of erectile dysfunction resulting from radical radiotherapy and androgen deprivation therapy for prostate cancer. Int. J. Clin. Pract. 2014, 69, 106–123. [Google Scholar] [CrossRef]
- Low, C.; Fullarton, M.; Parkinson, E.; O’Brien, K.; Jackson, S.; Lowe, D.; Rogers, S. Issues of intimacy and sexual dysfunction following major head and neck cancer treatment. Oral Oncol. 2009, 45, 898–903. [Google Scholar] [CrossRef] [PubMed]
- Schover, L.R.; van der Kaaij, M.; van Dorst, E.; Creutzberg, C.; Huyghe, E.; Kiserud, C.E. Sexual dysfunction and infertility as late effects of cancer treatment. Eur. J. Cancer Suppl. 2014, 12, 41–53. [Google Scholar] [CrossRef] [PubMed]
- Katz, A.; Dizon, D.S. Sexuality After Cancer: A Model for Male Survivors. J. Sex. Med. 2016, 13, 70–78. [Google Scholar] [CrossRef] [PubMed]
- Vermeer, W.M.; Bakker, R.M.; Kenter, G.G.; Stiggelbout, A.; Ter Kuile, M.M. Cervical cancer survivors’ and partners’ experiences with sexual dysfunction and psychosexual support. Support. Care Cancer 2015, 24, 1679–1687. [Google Scholar] [CrossRef] [PubMed]
- Bokhour, B.G.; Clark, J.A.; Inui, T.S.; Silliman, R.A.; Talcott, J.A. Sexuality after treatment for early prostate cancer. J. Gen. Intern. Med. 2001, 16, 649–655. [Google Scholar] [CrossRef]
- Goldfarb, S.; Mulhall, J.; Nelson, C.; Kelvin, J.; Dickler, M.; Carter, J. Sexual and Reproductive Health in Cancer Survivors. Semin. Oncol. 2013, 40, 726–744. [Google Scholar] [CrossRef]
- Wittmann, D. Emotional and sexual health in cancer. Curr. Opin. Support. Palliat. Care 2016, 10, 75–80. [Google Scholar] [CrossRef]
- Romanow, R. Building on Values: Report of the Commission on the Future of Health Care in Canada. 2002. Available online: https://publications.gc.ca/site/eng/9.686360/publication.html (accessed on 5 December 2022).
- Flynn, K.E.; Reese, J.B.; Jeffery, D.D.; Abernethy, A.P.; Lin, L.; Shelby, R.A.; Porter, L.S.; Dombeck, C.B.; Weinfurt, K.P. Patient experiences with communication about sex during and after treatment for cancer. Psycho-Oncol. 2011, 21, 594–601. [Google Scholar] [CrossRef]
- Lee, T.K.; Handy, A.B.; Kwan, W.; Oliffe, J.L.; Brotto, L.A.; Wassersug, R.J.; Dowsett, G.W. Impact of Prostate Cancer Treatment on the Sexual Quality of Life for Men-Who-Have-Sex-with-Men. J. Sex. Med. 2015, 12, 2378–2386. [Google Scholar] [CrossRef]
- Liaropoulos, L.; Goranitis, I. Health care financing and the sustainability of health systems. Int. J. Equity Health 2015, 14, 1–4. [Google Scholar] [CrossRef]
- Boserup, B.; McKenney, M.; Elkbuli, A. The financial strain placed on America’s hospitals in the wake of the COVID-19 pandemic. Am. J. Emerg. Med. 2021, 45, 530–531. [Google Scholar] [CrossRef]
- Michael, L.B.; Mehrotra, A.; Landon, B.E. COVID-19 and the Upcoming Financial Crisis in Health Care. NEJM Catal. 2020, 1, 2. [Google Scholar] [CrossRef]
- Matthew, A.; Jamnicky, L.; Currie, K.; Gentile, A.; Trachtenberg, J.; Alibhai, S.; Finelli, A.; Fleshner, N.; Yang, G.; Osqui, L.; et al. 320 Prostate Cancer Rehabilitation: Outcomes of a Sexual Health Clinic. J. Sex. Med. 2018, 15, S84. [Google Scholar] [CrossRef]
- Matthew, A.G.; Trachtenberg, L.J.; Yang, Z.G.; Robinson, J.; Petrella, A.; McLeod, D.; Walker, L.; Wassersug, R.; Elliott, S.; Ellis, J.; et al. An online Sexual Health and Rehabilitation eClinic (TrueNTH SHAReClinic) for prostate cancer patients: A feasibility study. Support. Care Cancer 2021, 30, 1253–1260. [Google Scholar] [CrossRef]
- Boulley, G.E.; Leroy, T.; Bernetière, C.; Paquienseguy, F.; Desfriches-Doria, O.; Préau, M. Digital health interventions to help living with cancer: A systematic review of participants’ engagement and psychosocial effects. Psycho-Oncol. 2018, 27, 2677–2686. [Google Scholar] [CrossRef] [PubMed]
- Hong, Y.; Peña-Purcell, N.C.; Ory, M.G. Outcomes of online support and resources for cancer survivors: A systematic literature review. Patient Educ. Couns. 2012, 86, 288–296. [Google Scholar] [CrossRef] [PubMed]
- Forbes, C.C.; Finlay, A.; McIntosh, M.; Siddiquee, S.; Short, C.E. A systematic review of the feasibility, acceptability, and efficacy of online supportive care interventions targeting men with a history of prostate cancer. J. Cancer Surviv. 2019, 13, 75–96. [Google Scholar] [CrossRef]
- Leykin, Y.; Thekdi, S.M.; Shumay, D.M.; Muñoz, R.F.; Riba, M.; Dunn, L.B. Internet interventions for improving psychological well-being in psycho-oncology: Review and recommendations. Psycho-Oncology 2011, 21, 1016–1025. [Google Scholar] [CrossRef] [PubMed]
- Miniwatts Marketing Group. Internet World Stats. 2022. Available online: https://www.internetworldstats.com/stats14.htm (accessed on 8 February 2023).
- Iribarren, S.J.; Cato, K.; Falzon, L.; Stone, P.W. What is the economic evidence for mHealth? A systematic review of economic evaluations of mHealth solutions. PLoS ONE 2017, 12, e0170581. [Google Scholar] [CrossRef]
- Gheorghiu, B.; Hagens, S. Cumulative Benefits of Digital Health Investments in Canada. eTELEMED 2017, 9, 69–71. [Google Scholar] [CrossRef]
- Digital Health Innovation Action Plan. Available online: https://www.fda.gov/media/106331/download (accessed on 9 February 2023).
- Ananth, H.; Jones, L.; King, M.; Tookman, A. The impact of cancer on sexual function: A controlled study. Palliat. Med. 2003, 17, 202–205. [Google Scholar] [CrossRef]
- Michie, S.; Yardley, L.; West, R.; Patrick, K.; Greaves, F. Developing and Evaluating Digital Interventions to Promote Behavior Change in Health and Health Care: Recommendations Resulting From an International Workshop. J. Med. Internet Res. 2017, 19, e232. [Google Scholar] [CrossRef]
- Althof, S.E.; Rosen, R.C.; Perelman, M.A.; Rubio-Aurioles, E. Standard Operating Procedures for Taking a Sexual History. J. Sex. Med. 2013, 10, 26–35. [Google Scholar] [CrossRef] [PubMed]
- Kang, H.S.; Kim, H.-K.; Park, S.M.; Kim, J.-H. Online-based interventions for sexual health among individuals with cancer: A systematic review. BMC Health Serv. Res. 2018, 18, 1–10. [Google Scholar] [CrossRef]
- Kelders, S.M.; Kok, R.; Ossebaard, H.C.; Van Gemert-Pijnen, J.E. Persuasive System Design Does Matter: A Systematic Review of Adherence to Web-based Interventions. J. Med. Internet Res. 2012, 14, e152. [Google Scholar] [CrossRef] [PubMed]
- Yun, Y.H.; Lee, K.S.; Kim, Y.-W.; Park, S.Y.; Lee, E.S.; Noh, D.-Y.; Kim, S.; Oh, J.H.; Jung, S.Y.; Chung, K.-W.; et al. Web-Based Tailored Education Program for Disease-Free Cancer Survivors With Cancer-Related Fatigue: A Randomized Controlled Trial. J. Clin. Oncol. 2012, 30, 1296–1303. [Google Scholar] [CrossRef] [PubMed]
| All Patients | Urinary and Bowel |
|---|---|
Introduction
|
|
| Male Sexual Function—Physical | Female Sexual Function—Physical |
|
|
| Male Sexual Function—Psychological | Female Sexual Function—Psychological |
|
|
| Sexual Wellbeing and Age | Head and Neck |
|
|
| Fertility | Social Support |
|
|
| Fatigue | |
| |
| All Patients | |
| |
| Impact on Partner | Impact on Couple |
|
|
| Patient Preference Module | |
|
|
| Bladder Cancer | Testicular Cancer |
|---|---|
| Pre-Tx | Pre-Tx |
| Sexual Health and Wellbeing as an Important Part of Cancer Care | Sexual Health and Wellbeing as an Important Part of Cancer Care |
| About the SHC | About the SHC |
| Understanding the Sexual Response Cycle | Understanding the Sexual Response Cycle |
| The Sexual Response Cycle and the Impact of Bladder Cancer Treatment | The Sexual Response Cycle and the Impact of Testicular Cancer Treatment |
| Fertility and Sperm-Banking | Fertility and Sperm-Banking |
| Urinary Diversions | Scar and Testicular Prosthesis |
| Potential Changes in Your Erectile Function | Potential Changes in Your Erectile Function |
| Frequently Asked Questions | Frequently Asked Questions |
| Managing Your Expectations of Erectile Recovery | |
| 6 weeks Post-Tx | 6 weeks Post-Tx |
| Revisiting Managing Your Expectations | Erectile Dysfunction and Erection Pills |
| Overview of Pro-Erectile Therapy | Resuming Sexual Activity |
| Pro-Erectile Treatment Decision-Making | Exploring and Expanding Your Sexual Repertoire |
| Resuming Sexual Activity | Body Image—Adapting to the Removal of a Testicle |
| Exploring and Expanding Your Sexual Repertoire | More on Fertility |
| Body Image—Adapting to Your Ostomy | |
| 3 months Post-Tx | 3 months Post-Tx |
| Potential Changes in Your Desire | Potential Changes in Your Desire |
| Potential Changes in Your Orgasm | Potential Changes in Your Orgasm |
| Male Sexual Performance Anxiety | Male Sexual Performance Anxiety |
| Impact on Your Masculinity | Impact on Your Masculinity |
| Impact on Your Sexual Partner (Female) | Impact on Your Sexual Partner (Female) |
| If You Are Single … the Issue of Disclosure | If You Are Single … the Issue of Disclosure |
| Maintain Intimacy—Understanding Intimacy and Passion | Maintain Intimacy—Understanding Intimacy and Passion |
| Sensate Focus | Sensate Focus |
| 6 months Post-Tx | 6 months Post-Tx |
| Re-Visiting Your Pro-Erectile Therapy | “Re-Challenging” Pro-Erectile Pills |
| Age and Sexual Health (Female Partner) | Age, Sexual Health, and Sexual Identity |
| Age and Sexual Health (Patient) | Grief as a Normal Emotional Response |
| Grief as a Normal Emotional Response | What Is Good Sex? |
| What Is Good Sex? | Why Do I Engage in Sex? |
| Why Do I Engage in Sex? | Common Interpersonal Misunderstandings |
| Common Interpersonal Misunderstandings | The Big Picture: Adapting to the Diagnosis and Treatment of Cancer |
| Adaptation to Changes in Your Sex Life | |
| Understanding Your Social Support | |
| Continued Communication With Your Sexual Health Coach | |
| SHC Is Not Going Anywhere | |
| 12 months Post-Tx | |
| “Re-Challenging” With Pro-Erectile Therapy | |
| The Big Picture: Adapting to the Diagnosis and Treatment of Cancer | |
| Adaption to Changes in Your Sex Life | |
| Understand Your Social Support | |
| Continued Communication With Your Sexual Health Coach | |
| SHC Is Not Going Anywhere |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Matthew, A.; Guirguis, S.; Incze, T.; Stragapede, E.; Peltz, S.; Yang, G.; Jamnicky, L.; Elterman, D. The Anatomy of a Hybrid In-Person and Virtual Sexual Health Clinic in Oncology. Curr. Oncol. 2023, 30, 2417-2428. https://doi.org/10.3390/curroncol30020184
Matthew A, Guirguis S, Incze T, Stragapede E, Peltz S, Yang G, Jamnicky L, Elterman D. The Anatomy of a Hybrid In-Person and Virtual Sexual Health Clinic in Oncology. Current Oncology. 2023; 30(2):2417-2428. https://doi.org/10.3390/curroncol30020184
Chicago/Turabian StyleMatthew, Andrew, Steven Guirguis, Taylor Incze, Elisa Stragapede, Sarah Peltz, Gideon Yang, Leah Jamnicky, and Dean Elterman. 2023. "The Anatomy of a Hybrid In-Person and Virtual Sexual Health Clinic in Oncology" Current Oncology 30, no. 2: 2417-2428. https://doi.org/10.3390/curroncol30020184
APA StyleMatthew, A., Guirguis, S., Incze, T., Stragapede, E., Peltz, S., Yang, G., Jamnicky, L., & Elterman, D. (2023). The Anatomy of a Hybrid In-Person and Virtual Sexual Health Clinic in Oncology. Current Oncology, 30(2), 2417-2428. https://doi.org/10.3390/curroncol30020184





