Abstract
Prostate cancer (PCa) is a major public health issue, as the second most common cancer and the fifth leading cause of cancer-related deaths among men. Many PCa cases are indolent and pose minimal risk, making active surveillance a suitable management approach. However, clinically significant prostate carcinoma (csPCa) can lead to serious health issues, including progression, metastasis, and death. Differentiating between insignificant prostate cancer (inPCa) and csPCa is crucial for determining appropriate treatment. Diagnosis of PCa primarily involves trans-perineal and transrectal systematic biopsies. Systematic transrectal prostate biopsy, which typically collects 10–12 tissue samples, is a standard method, but it can miss csPCa and is associated with some complications. Recent advancements, such as magnetic resonance imaging (MRI)-targeted biopsies, have been suggested to improve risk stratification and reduce overtreatment of inPCa and undertreatment of csPCa, thereby enhancing patient quality of life and treatment outcomes. Guided biopsies are increasingly recommended for their ability to better detect high-risk cancers while reducing identification of low-risk cases. MRI-targeted biopsies, especially when used as an initial biopsy in biopsy-naïve patients and those under active surveillance, have become more common. Utilization of MRI-TB alone can decrease septic complications; however, the combining of targeted biopsies with perilesional sampling is recommended for optimal detection of csPCa. Future advancements in imaging and biopsy techniques, including AI-augmented lesion detection and robotic-assisted sampling, promise to further improve the accuracy and effectiveness of PCa detection.
1. Introduction
Prostate cancer (PCa) is a significant public health concern, since it was the second most prevalent cancer and the fifth leading cause of cancer-related mortality among men in 2020, contributing to over 375,000 deaths globally during this period [1]. Estimated cancer-related mortality amounts to 11%; however, the 5-year relative survival rate for prostate cancer has increased from the mid-1970s to reach 97% in 2024 [2]. PCa is heterogeneous in terms of morphological, genetic, and clinical features and contains various morphologically and clonally distinct foci. A considerable portion of PCa cases exhibit indolent behaviour, posing minimal threat if left unidentified [3]. In case of indolent cancers, active surveillance appears to be a sufficient management mode. Conversely, clinically significant prostate carcinoma (csPCa) has substantial therapeutic implications, including progression, metastasis, and potential PCa-specific mortality [4]. The term csPCa describes a form of prostate cancer with the potential to result in mortality of the affected patient and it is used to distinguish it from tumor variants typically lacking such lethality [5]. However, the definition of csPCa includes features extending beyond histological grading to encompass individual patient factors, therefore precise specification of csPCa poses a challenge and differs in the available literature. Typically, the criteria rely on histological parameters, such as the Gleason grading system or the International Society of Urological Pathology (ISUP) grade systems [6,7]. Additional parameters, including PSA levels, race, family history, or cancer volume, may also be included in the classification [8,9]. Prostate-specific antigen (PSA) screening has contributed to the decrease in PCa mortality, but also poses the risk of overdiagnosis (since it can be increased also in benign prostatic hyperplasia, prostatitis and other non-malignant conditions) and consequent complications from unnecessary treatment [10,11]. Discrimination between clinically insignificant prostate cancer (inPCa) and csPCa is crucial in determining prostate cancer lethality [12]. However, risk stratification during diagnosis is complicated by inter- and intra-tumoral heterogeneity.
Systematic transrectal prostate biopsy serves as a standard method for the collection of tissue samples to confirm the diagnosis in patients with clinical suspicion of PCa based on elevated levels of PSA and/or abnormal findings on digital rectal examination (DRE) [13,14]. This type of prostate biopsy typically involves the systematic collection of 10–12 biopsy cores from both lobes of the prostate [5,15]. However, since this diagnostic tool has been suggested to miss csPCa and to be associated with complications, new techniques have been developed. Magnetic resonance imaging (MRI) has emerged as a valuable tool in diagnostics since it facilitates risk stratification of visible lesions based on diffusion and perfusion patterns and enables targeted biopsy needle placement [16]. MRI-targeted biopsies have been suggested to enhance the detection rates of clinically relevant PCa; however, it is the approach combining targeted and systematic biopsies that appears to offer optimal sensitivity for cancer detection [17].
This review aims to assess the evolving role of systematic biopsy in the era of targeted biopsy approaches in prostate cancer diagnosis.
2. Systematic Biopsy
Systematic transrectal ultrasound (TRUS)-guided biopsy, which has been widely used globally for decades, has progressed from sextant templates to 12-core biopsy schemes [18]. This diagnostic procedure involves sampling the peripheral zone of the prostate, where cancer is predominantly located, with 8 to 12 cores (maximum 19 cores, but most commonly 10–12) depending on prostate size [15,19]. The utilization of more comprehensive biopsy schemes, including the lateral and peripheral aspects of the prostate with increased number of sampling sites, translates into higher detection rates and reduced variation in PSA-related detection of cancer [18]. TRUS biopsy primarily relies on ultrasound use for anatomical guidance (identification of the prostate) since suspicious lesions are generally not visible using this imaging technique, potentially resulting in random and systematic errors, as well as missing significant cancers [19]. Due to variations in tumor differentiation within various areas of the prostate, sampling errors may result in under-grading [20]. The estimated false-negative rate of systematic biopsy performed in the case of any cancer is between 25% and 40% [21]. Misclassification is frequently associated with inadequate sampling of cancer lesions at their greatest diameter or highest grade [22,23].
Two primary approaches, = biopsy and transrectal biopsy with varying core numbers, are primarily used. Transrectal biopsy is typically conducted as a quick, in-office procedure under local anesthesia [24]. It involves multiple passes of the biopsy needle through the rectal mucosa, which may increase the risk of infections [25]. Extended biopsy protocols include cores from the lateral peripheral zone and those from lesions detected through palpation or imaging [26]. In turn, transrectal saturation biopsy, involving comprehensive sampling (over 20 prostate biopsies) frequently overlooks anterior zones, which diminishes its accuracy [27]. Moreover, such intensified approaches are less common due to their burden on patients, elevated complication rates, and tendency to over-diagnose insignificant prostate cancer [28]. Saturation biopsies are mostly reserved for instances of repeat biopsy procedures [26]. It appears that increasing core numbers through saturation techniques may reveal cancers overlooked during extended core sampling. However, this approach also elevates the risk of over-detecting indolent cancers without substantially enhancing cancer detection rates (CDR) or pathology concordance [29].
The trans-perineal approach for prostate biopsy serves as an alternative to the conventional transrectal route. Its advantages include improved access to the anterior aspect of the prostate gland, reduced incidence of infectious complications, and the potential for refining the three-dimensional localization and documentation of sampling through the utilization of a biopsy template with coordinates [30]. Trans-perineal biopsy may be either executed in the operating room under general or as an office procedure with local anesthesia, though the first approach is now rarely used [24]. During such biopsy, the needle is guided longitudinally along the axis of the prostate, improving anterior prostate sampling [31]. This technique has demonstrated greater capacity for detecting clinically significant prostate cancer and for upgrading men under active surveillance [32]. Moreover, trans-perineal biopsy avoids the transfer of rectal flora into the prostate and bloodstream, thus posing lower risks of infectious complications [33]. Therefore, current European Association of Urology guidelines strongly recommend performing prostate biopsy using the trans-perineal approach due to the lower risk of infectious complications [34]. However, the recent PREVENT randomized trial demonstrated that transrectal biopsy with targeted prophylaxis shows comparable infection rates to office-based trans-perineal biopsy [35]. The American Urological Association guidelines suggest that clinicians may use either a transrectal or trans-perineal biopsy route when performing a biopsy (conditional recommendation; evidence level: grade C) [36].
Template grid is frequently used for biopsy guidance, which increases procedural time and medical costs [37]. However, due to the lack of consensus on a template for - prostate biopsy in terms of the optimal number and location of biopsy cores, various types of grids have been developed, including the Barzell template, which comprises 26–35 cores. The introduction of the freehand technique has decreased anesthesia requirements from general to local or local/sedation [38]. In this technique a common access cannula is introduced through the perineal skin, allowing repeated passage of the biopsy needle through two needle puncture sites, one on each side of the perineum [24,39] This approach facilitates biopsy performance in office settings and reduces needle punctures through the skin. Some studies suggested a correlation between core number and csPCa detection, while other failed to observe such relationship [40,41,42]. In general, the number of biopsy cores should depend on prostate volume to avoid false-negative results. Previous guidelines of the European Association of Urology (2022) recommended the collection of at least 8 systematic biopsy cores in prostates with a size of <30 mL and 10- to 12-core biopsies in larger prostates [43]. Ravery et al. [44] demonstrated that TRUS-guided biopsies using either 10 or 12 cores (if total prostate volume was >50 mL) was associated with 6.6% higher cancer detection compared to the sextant biopsy method, especially in patients with a PSA level under 10 ng/mL and/or a prostate volume over 50 mL. In another study, the addition of four lateral cores at the base and mid-gland as well as two additional mid-lobar, parasagittal transition zone biopsies in case of prostates exceeding 50 mL increased cancer detection rate by 20% compared to sextant biopsy. Moreover, Lee et al. [45] demonstrated the dependency of systematic biopsy sensitivity on the number of biopsy cores taken. In their study, gradual decrease in the mean number of cores from 21.8 to 14.5, 10.9, 7.3, and 5.4 led to a statistically significant reduction in overall csPCa detection rates in non-targeted systematic biopsy by 16%, 13%, 9%, and 8%, respectively, in the entire cohort. In turn, Kwon et al. [42] demonstrated that the 20-core template outperformed the 10-core one in detecting clinically significant cancers in the entire cohort (49% vs. 41%, p = 0.02) and in the biopsy-naïve group (48% vs. 40%, p = 0.05); however, additional cores did not yield higher detection of Grade Group 1 (GG1) cancers (20-core: 35% vs. 10-core: 44%, p = 0.09). Furthermore, more clinically significant cancers were identified in the 12-core trans-perineal biopsy group compared to the 12-core TRUS biopsy (46% vs. 38%, p < 0.001). The direction of biopsies is also crucial. PCa is most likely located at the apex and base of the peripheral gland, making these sites the primary targets for biopsies, whereas midline biopsies have the lowest likelihood of positive results [18,46,47]. Various studies have indicated that the addition of laterally directed biopsies, which also sample the lateral horn, increases sensitivity of cancer detection by approximately 5% to 35% [18,46,47]. Most additional cancers were found in the far-lateral mid-lobar region, an area effectively sampled by laterally directed sextant biopsy. A systematic review of 87 studies involving 20,698 patients showed that 12-core prostate biopsy schemes, which add laterally directed cores to the standard sextant scheme, achieved a balance between cancer detection rates and adverse events [15]. Current EAU-EANM-ESTRO-ESUR-ISUP-SIOG-guidelines (2024) present data in favor of collecting a minimum of 12 samples bilaterally from apex to base, as far posterior and laterally as possible, within the peripheral gland, irrespective of the approach used in patients with no previous prostate imaging [34].
2.1. Impact of Systematic Biopsy Result on Treatment
As focal therapy gains interest, accurate identification of all tumor foci through comprehensive prostate examination becomes crucial in guaranteeing optimal patient selection and suitable ablation of all regions harboring csPCa [45]. The presence of csPCa foci in untreated regions poses a challenge to the oncological efficacy of focal therapy as a standalone strategy. Post-treatment prostate biopsies have revealed out-of-field recurrences in 4–49% of cases, which may indicate their initial under-detection at MRI imaging and subsequent biopsy, or the development of de novo multifocal disease within the prostate [48,49]. It seems that the former scenario is more probable in patients in whom the post-treatment biopsy was made within 6–12 months of focal therapy initiation. Thus, a comprehensive pre-treatment prostate biopsy may be an underutilized tool in patient selection for focal therapy. Lee et al. [45] also stressed the pivotal role of systematic biopsy (SB) in patient selection for focal therapy. Their results demonstrated that decreasing the number of cores collected during SB significantly increased the percentage of patients necessitating changes in their treatment plans compared to full systematic biopsy. The proportion of patients with altered treatment plans rose from 12% to 29% when comparing a strategy in which the mean number of non-targeted systematic cores was 14.5 to a strategy based on 5.4 cores. The standard 12-core systematic biopsy may be insufficient in case of individuals opting for focal therapy, and therefore saturation biopsy may prove to be a better option for this group. Based on the results of study which employed SB with a median of 23 cores for a median prostate volume of 43.5 mL, Lee et al. [45] suggested a sampling intensity of at least 1 core for every 2 mL of prostate volume as the optimal approach. However, comprehensive SB may not be well-tolerated in patients undergoing transrectal biopsy under local anesthesia, given the related risks of urinary retention and sepsis [45]. Moreover, the detection of significant cancers in non-targeted SB biopsy may be associated with the underestimation of the index lesion [50]. The impact of these smaller foci of untreated disease outside the index lesion on long-term oncological outcomes remains uncertain, and thus require further analysis.
2.2. Advantages of Systematic Biopsy in Detecting Prostate Cancer
PCa is multi-focal tumor in up to 80% of men, and systematic biopsy plays a crucial role in identifying foci beyond the index lesion, which may not be adequately visualized on MRI [45,51,52]. SB increases the likelihood of detecting all cancerous areas within the prostate, thereby reducing the risk of misclassifying a higher-risk patient as low-risk [53,54]. By sampling multiple regions of the prostate, it provides a thorough initial assessment of tumor characteristics, including grade, volume, and distribution [55]. This baseline information is critical for accurately stratifying patients for active surveillance programs. The study assessing the distance between cancer-containing systematic samples and MRI-visible lesions revealed that 90% of systematic biopsies comprising csPCa cores were situated within a 10-mm radius of the nearest MRI-visible lesion [56]. A proportion of 18% of csPCas were positioned beyond this 10-mm radius; however, their yield decreased as the distance from the region of interest (ROI) increased. Consequently, the clinical utility of systematic biopsy may lay in capturing perilesional csPCa when ROIs shows negative results. Focusing systematic biopsies around ROI targets, termed targeted regional biopsy, presents a potentially efficient alternative to traditional 12-core templates. It has been demonstrated in one of studies that systematic biopsies performed ipsilaterally to the ROI yielded significantly higher cancer detection rates compared to contralateral biopsies, even in cases where a targeted core showed no cancer [57,58]. Moreover, systematic biopsy appears to be essential to rule out csPCa in magnetic resonance imaging (MRI)-negative regions and confirm the presence of a discrete lesion suitable for focal therapy [59]. However, the value of systematic biopsies covering only areas non-targeted by MRI remains uncertain due to the fact that both biopsies may overlap suspicious regions [60]. Lee et al. [61] demonstrated a csPCa detection rate of 21% for non-targeted systematic biopsy, indicating that excluding systematic biopsy cores overlapping with MRI lesions would only result in a 3% missed detection rate for csPCa. Some studies have indicated that systematic biopsy might decrease the risk of underestimation the Gleason score (GS) [53,54]. Furthermore, collecting cores from areas surrounding a suspicious lesion (focal systematic biopsy) may reduce the risk of sampling error and potentially provide a more accurate estimation of the Gleason score [62]. Moreover, regular systematic biopsies during active surveillance help detect any changes in tumor grade or volume, ensuring timely intervention if the disease progresses [55]. The number of targeted cores taken per lesion affects the detection of csPCa and the estimation of the Gleason score [63]. Specifically, the current standard of obtaining three to four cores from high-volume lesions, such as PIRADS 5, may not be enough to accurately estimate the Gleason score [64]. SB provides detailed information on the location and extent of tumors within the prostate which allows surgeons to tailor the extent of lymph node dissection to individual patient risk profiles. This approach helps in maximizing the therapeutic benefit while minimizing unnecessary surgical intervention [65]. The local staging of prostate cancer is vital for planning nerve-sparing surgery, as it helps surgeons avoid the critical anatomical structures, such as neurovascular bundles, while ensuring complete cancer removal [66]. Accurate identification of the tumor’s proximity to the neurovascular bundles in SB aids in balancing the need for oncological control with the preservation of erectile function and urinary continence [44]. Thus, SB helps in minimizing the risk of the abovementioned postoperative complications by providing a clear map of the prostate and surrounding structures. The extent of PCa involvement in systematic cores may also serve as a significant prognostic indicator of biochemical progression risk or pelvic lymph node involvement. Omitting systematic biopsy cores may lead to erroneous qualification or disqualification for extended pelvic lymph node dissection [67,68].
Available evidence suggests that the omission of systematic biopsy would increase diagnostic uncertainty and worsen risk assessment, since it can translate into 5–16% of csPCa cases that may be overlooked [12,69,70,71]. The results of the GÖTEBORG-2 trial indicated that the omission of systematic biopsies decreased the detection of inPCa by 50%; however, at the same time, one in five csPCa were overlooked [72]. In general, systematic biopsies enabled the recognition of smaller tumors belonging to the intermediate-risk group (ISUP 2) that were not reported while using other methods in this trial. While considering the omission of systematic biopsy, it should be kept in mind that multiparametric magnetic resonance imaging (mpMRI) shows limited sensitivity in identifying all csPCa lesions, with approximately 30% of such lesions being undetectable on mpMRI [73]. mpMRI alone has limitations in predicting local stage and extra-prostatic extension [41,42]. In patients with higher Prostate Imaging Reporting and Data System (PI-RADS) scores, increased possibility of csPCa presence beyond the index lesion has been reported, with lesion outside the index in up to 60% of PI-RADS 5 cases [74,75]. Krausewitz et al. [12] suggested that benefits related to SB in csPCa detection were greater in patients with PI-RADS 3 lesions and increased inversely with PI-RADS grading. In turn, a Polish retrospective study of 225 patients with PCa demonstrated that omission of SB in PI-RADS 5 lesions was associated with a significant decrease in the csPCa detection rate by 6.9% [76]. Moreover, Cochrane meta-analysis of 18 studies revealed that the added value of SB in csPCa detection in biopsy-naive patients was 4.3% [4]. Similarly, in the 4 M trial and MRI-FIRST studies the estimated added value of systematic biopsy was approximately 5% [69,77]. Systematic biopsy can be performed in case of non-suspicious mpMRI results in patients with high prostate-specific antigen density (PSAD) values (>0.15 ng/mL2) due to the significantly increased risk of csPCa detection [78]. PSAD is an important predictor that enhances csPCa detection rates in PI-RADS 5 patients. Moreover, PSAD and PI-RADS scores have been found to complement each other in csPCa detection [76]. Malewski et al. [76] reported that omitting systematic biopsy at high PSAD values increased the risk of missing csPCa from 4.7% to 7.4%. In turn, the absolute detection rate of csPCa associated with the use of systematic biopsy increased from 8.1% to 26.5% for the PSAD threshold of 0.17 ng/mL2. High PSAD values have been suggested to be associated with larger tumor volumes and a higher likelihood of underestimating the Gleason score [79,80]. Therefore, in cases of high PSAD values, systematic biopsy should not be omitted in PI-RADS 5 lesions.
The available literature indicates that systematic biopsy, when added to targeted biopsy in the initial biopsy, markedly improves csPCa detection compared to repeat biopsy. The risk of missing csPCa when systematic biopsy is omitted appears to be lower in repeat biopsy compared to initial biopsy (3.5% versus 10%, respectively) [76]. Similarly, Cochrane meta-analysis confirmed that added value of systematic biopsy in repeat biopsy is marginal (~2.3%) [81]. The European Association of Urology recommendations also suggest that systematic biopsy may be omitted in repeat biopsy settings, despite weak evidence [82]. The American Urological Association guidelines suggest performance of a systematic biopsy in patients with both an absence of suspicious findings on MRI and an elevated risk for GG2+ prostate cancer (moderate recommendation, evidence level: grade C), as well in those with indications for a repeat biopsy who do not have a suspicious lesion on MRI (conditional recommendation; evidence level: grade B) [36]. In turn, in biopsy-naïve patients with a suspicious lesion on MRI, or in patients with a suspicious lesion on MRI undergoing repeat biopsy, targeted biopsies of the suspicious lesion should be performed and a systematic template biopsy may also be performed (moderate recommendation, evidence level: grade C) [36]. However, SB alone can be considered in patients with a negative PIRADS score (1–2) and low clinical suspicion of PCa (PSA density < 0.20 ng/mL/cc, negative DRE findings, no family history) and also when MRI is not available and a risk calculator indicates the need to perform a biopsy [34].
2.3. Limitations and Drawbacks of Systematic Biopsy
Despite its widespread use, systematic biopsy has some limitations, primarily related to inadequate sampling of specific prostate regions, such as the apical, middle, and anterior areas, which often result in false-negative outcomes and consequent underdiagnosis of csPCa [83,84]. Indeed, the results of various studies have demonstrated that the use of this procedure may result in the omission of csPCa as well as the overdiagnosis of inPCa and thus to potential overtreatment-related harms [85,86,87]. This might explain the limited benefits of radical treatment observed in randomized trials, such as PROTECT and PIVOT, both of which utilized systematic TRUS biopsy for cancer diagnosis [88]. According to some studies, the rate of false-negative results associated with initial systematic 12-core biopsy is 20–24%, while others show that this rate may reach up to 49% (saturation biopsy) [89,90,91]. Moreover, up to 40% of low-risk patients with a Gleason score of 3 + 3 during SB showed greater scores on postoperative pathology [92,93].
Numerous passes of biopsy needles through rectal mucosa and the increasing prevalence of drug-resistant bacterial strains translates into higher risk of sepsis and hospitalization rates following transrectal biopsy as well as greater patients’ morbidity [24]. It has been observed that urinary tract infection and prostatitis are more frequent in 18-core biopsies compared to 12-core biopsies [25]. These complications are associated with increased healthcare costs associated with antibiotic prophylaxis to prevent infection, as well as the expenses related to treating post-biopsy infection and sepsis.
Furthermore, transrectal (TR) prostate biopsy has been associated with other severe complications, including rectal bleeding, hematuria, fever, and acute urinary retention [94,95,96]. Rectal bleeding and hematuria, which are typically self-limiting complications, tend to resolve within several days. However, in patients receiving anticoagulant medications, the bleeding may become serious [33]. To reduce the risk of severe bleeding, in such patients anticoagulation therapy should be discontinued at least one week before prostate biopsy. The reduction in the number of biopsy cores could also potentially decrease bleeding complications arising from the procedure, such as bladder tamponade [97]. A high number of biopsy cores have been demonstrated to affect the trajectory of radical prostatectomy and contribute to greater blood loss [98]. Given the high rates of false negatives and complications associated with systematic TR prostate biopsy, the trans-perineal (TP) approach was introduced to enhance biopsy detection rates and safety. A systematic review and meta-analysis including 11 studies and 2569 patients demonstrated that the trans-perineal approach significantly reduced the risk of complications, such as rectal bleeding and fever, while the transrectal approach was associated with less severe patient pain [33]. Despite the administration of enemas before transrectal prostate biopsy, it is still associated with significantly higher risk of infection compared to the trans-perineal approach. Therefore, trans-perineal prostate biopsy is suggested in patients predisposed to infection, such as those with prostatitis, diabetes, or urinary catheterization, to minimize the likelihood of sepsis and severe post-procedural fever [33]. In turn, the disadvantages of trans-perineal approach include low risk of urinary retention requiring catheter placement (in 1.4% of patients), inability to pass urine, hematuria (in 16.0%), hematospermia lasting up to three months (in most men), perianal abscess (in 0.008%) and temporary erectile dysfunction (in less than 5%) [99].
3. Emergence and Advancement of Targeted Biopsy Techniques
The development of mpMRI has revolutionized PCa diagnosis by offering superior imaging modalities, including T2-weighted images, diffusion-weighted images (DWIs), and dynamic contrast-enhanced (DCE) images, thus facilitating precise delineation of suspicious lesions [14]. The introduction of PI-RADS version 2 in 2015 enabled the standardization of mpMRI results interpretation and reporting, as well as facilitating risk stratification before biopsy decisions [16]. MRI has emerged as a valuable tool for identifying suspicious areas within the prostate, facilitating targeted biopsies while minimizing unnecessary procedures in men with no detectable lesions [100,101]. The utilization of mpMRI has been found to enhance csPCa identification without the risk of overdiagnosis [71]. This technique accurately defines lesion areas suitable for targeting and, due to the integration of image fusion technology, it simplifies real-time targeted biopsy procedures. Targeted biopsies (TB) offer the advantage of focusing on mpMRI-detected lesions with lower differentiation, thereby mitigating the likelihood of under-grading. Consequently, MRI-targeted biopsies are gaining interest as adjuncts to or substitutes for SB in cases of previously negative biopsies, as initial biopsies, or during active surveillance [4]. A prospective clinical trial which assessed whether using mpMRI before SB would enhance the detection of csPCa in biopsy-naive patients demonstrated that an additional 5% ISUP2 cases could be identified with the addition of SB, but only 1% of these cases were Gleason 4 + 3 or worse [69]. Thus, it appears that, while performing mpMRI before biopsy in biopsy-naive patients shows the potential to improve the detection of csPCa, SB should not be avoided. European Association of Urology guidelines (2020) recommended the mpMRI procedure before every biopsy; however, current guidelines strongly suggest not using MRI as an initial screening tool [34,82]. Moreover, limited biopsy without MRI is suggested in men with suspicion of locally advanced disease on DRE and/or PSA>50 ng/mL, or individuals in whom curative treatment in not an option. However, an MRI procedure should be performed before prostate biopsy in men with suspected organ confined disease (strong recommendation),
3.1. Types of MRI-Targeted Biopsy
MRI-targeted biopsy (MRI-TB) methods, which include cognitive biopsy, MRI in-bore guided biopsy and MRI-ultrasound (US) software fusion biopsy, can be executed via transrectal or trans-perineal approaches [87]. Such biopsies are selectively conducted upon the identification of suspected lesions indicative of clinically significant prostate cancer on MRI scans [4].
3.1.1. Perilesional Biopsy (Figure 1)
Perilesional biopsy involves taking core samples from the area surrounding a lesion at various distances from the lesion. This method can help identify cancer cells around the lesion [102]. The diagnostic yield for csPCa could be improved by including perilesional sampling within a 10-mm radius from the ROI, potentially making “targeted regional biopsy” a standard approach [56]. Theoretical support for the importance of perilesional biopsy comes from the work of Priester et al. [103], which showed that MRI lesions typically underestimate actual cancer diameter by 11 mm and volume by three-fold. This finding was later confirmed by other studies. Brisbane et al. [56] demonstrated that 25% of csPCa cores lie within a 10-mm radius outside the MRI-identified lesion. The combination of systematic and perilesional biopsy was found to be associated with the risk of missing 7% of significant cancers, and for PIRADS ≥ 4 lesions the risk was 5% [102]. Another study showed that that the TB plus perilesional biopsy within a 10 mm radius detected 92% of csPCa cases [104]. Tschirdewahn et al. [105] found that this method identified 99% of csPCa cases. Combination of targeted and systematic cores within a 10 mm radius from the MRI lesions detected 90–92% of csPCa, while utilizing a 15 mm radius enabled the detection of 94–97% [56,104]. The distance required to encompass 90% of csPCa may vary with the PI-RADS score of the lesion: 5.5 mm for PI-RADS 5, 12 mm for PI-RADS 4, and 16 mm for PI-RADS 3 [56]. Moreover, Diamand et al. [106] revealed that perilesional sampling reduces the upgrading events in final pathology compared to systematic or targeted biopsies alone. The PI-RADS v2 Steering Committee recommends performing the biopsy of both the ROI and the surrounding perilesional tissue for PI-RADS 4 and 5 lesions [107]. According to current European Association of Urology, perilesional sampling should complement targeted biopsy in patients with MRI positive (i.e., PI-RADS ≥ 4) results (weak recommendation) [34]. Targeted biopsy with perilesional sampling can also be considered when MRI is indeterminate (PI-RADS = 3), and clinical suspicion of PCa is very low (PSA density < 0.10 ng/mL/cc, negative DRE findings, no family history).
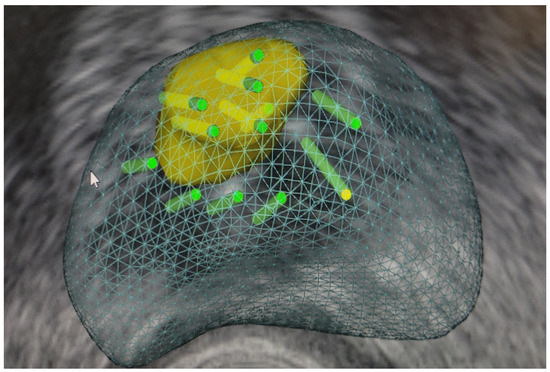
Figure 1.
Targeted fusion prostate biopsy with perilesional cores.
3.1.2. Cognitive Biopsy
Cognitive biopsy is based on utilizing MRI findings to identify suspicious regions within the prostate, followed by targeted biopsy under US guidance but without employing software registration of MRI and US images. This technique, also referred to as visually directed biopsy or cognitive fusion biopsy, relies on the operator’s interpretation of MRI to identify suspicious lesions, then using anatomical landmarks to guide biopsy to the site corresponding to US images. While feasible via transrectal or trans-perineal routes, the latter approach offers advantages, such as consistent prostate positioning for both MRI and biopsy. Moreover, this technique enables concurrent systematic biopsies. Nonetheless, cognitive biopsy’s reliance on operator proficiency poses challenges, particularly for individuals lacking experience in prostate MRI or US-guided biopsy. Difficulty in cognitive registration may arise in the absence of identifiable landmarks or in cases of large prostate glands with small targets, as well as in the presence of substantial calcifications obscuring the target [87].
3.1.3. Fusion Targeted Biopsy (Fus-TB) (Figure 2)
The combination of MRI with ultrasound fusion targeted biopsy (fus-TB) shows the strengths of both MRI and ultrasound technologies, as it enables real-time targeted biopsies guided by fusion software, thereby enhancing diagnostic accuracy [14]. This procedure is suitable for clinical settings since it does not need dedicated hardware [108]. The software aligns the lesion identified on MRI with a corresponding location on US to guide the biopsy needle to the targeted site [87]. This technique can be adapted to both transrectal and trans-perineal approaches. Registration between MRI and US can be accomplished using either rigid method, which corrects for rotational discrepancies or the elastic registration method, compensating for deformations of the prostate caused by adjacent structures or the US probe [109,110].
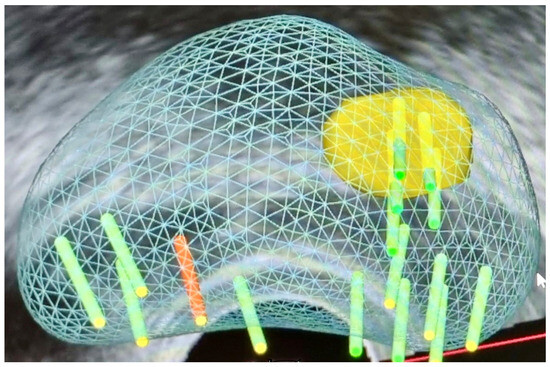
Figure 2.
Targeted biopsy with systematic cores.
Benefits of fus-TB include the possibility of documenting biopsy sites for patient follow-up during active surveillance and for quality assurance purposes [87]. Moreover, it shows high efficiency in accurately determining patients’ true pathological grades, thereby decreasing the risk of potential misclassification of inPCa and contributing to reduction in both overtreatment and undertreatment by minimizing diagnostic uncertainties [14,111,112,113]. Moreover, fus-TB addresses challenges encountered in targeting lesions not visualized by US or obscured by significant calcifications. It also holds potential as a substitute for the traditional 12-core SB, particularly in cases with prostate PI-RADS scores of 4 and 5 identified by mpMRI [114,115].
However, the drawbacks include upfront system acquisition costs, longer duration of the biopsy compared to cognitive biopsy, and the risk of technical problems during the procedure, such as failure to upload segmented images for targeting or successful MRI-US image registration. Additionally, the multi-step nature of the technique, involving MRI and US segmentation, image registration, and target sampling, is susceptible to operator-dependent errors, which can compromise the accuracy of target registration between modalities [87].
3.1.4. MRI In-Bore Biopsy
The in-bore biopsy technique is available with 1.5-T or 3-T MRI systems and can be conducted under moderate sedation or with the administration of rectal lidocaine gel. In-bore biopsy ensures precise needle placement at the target site through a transrectal approach (most commonly) but also via a trans-perineal or trans-gluteal approach [116]. In the transrectal approach, a rectal sleeve needle with a trocar is inserted, and the system software guides adjustments in needle direction and length based on MR images. After confirming correct needle placement, imaging is repeated to detect any sampling issues due to patient movement or anatomical changes. In turn, in the trans-perineal approach, a needle-guide template is fixed against the perineum. Then, the system software recognizes the target and the correct hole in the template for needle insertion, followed by adjustments until proper positioning is confirmed. The use of a robotic template for trans-perineal MRI in-bore biopsy has been reported to enhance needle placement accuracy compared to manual templates, but at the expense of significantly prolonged procedure durations (90–100 min) and considerable costs associated with robotic implementation [117]. Compared to systematic or other targeted biopsy methods, in-bore biopsy requires fewer overall cores [116,118]. However, this procedure cannot be conducted in an office setting and is more time-consuming [119,120].
3.2. Transrectal Versus Trans-Perineal Fusion Biopsy
MRI-targeted biopsy based on cognitive, fusion, or MRI in-bore techniques, can be conducted through transrectal or trans-perineal approaches. The transrectal approach positions the patient typically in the left lateral decubitus position (for cognitive and fusion techniques), or in prone position (for MRI in-bore procedures) [119]. The transrectal approach typically utilizes local anesthetic. Although the periprostatic nerve block greatly enhances peri-operative pain management when compared to the use of an anesthetic gel applied intrarectally, this method was suggested to potentially introduce or spread pathogens due to additional needle insertions through the rectum [121,122]. However, an updated meta-analysis of 28 RCTs with 4027 patients found no evidence that use of periprostatic injection for local anesthesia resulted in more infectious complications than no injection (RR: 95% CI: 1.08 [0.79–1.48]) [123].
In the transrectal approach, a needle guide is fixed to the probe, which is then inserted into the rectum to obtain biopsy specimens from the prostate through the rectal wall. The needle goes through either the transverse or sagittal plane of the prostate, primarily collecting the sample within its posterior part. However, the transrectal approach may disturb registration between MR and ultrasound images due to the oblique angulation of the transrectal probe [87]. Moreover, the risk of sepsis is the primary concern with the transrectal approach, with infection rates ranging from 0.7% to 7.0% [124,125,126]. To avoid such complication, antibiotics (e.g., fluoroquinolones) are administered; however, their common use can contribute to bacterial resistance [127]. Moreover, the use of fluoroquinolones has been found to be associated with various adverse effects, including tendon rupture, soft-tissue injuries and tendinitis, as well as aortic dissection and rupture [128,129]. Due to the increase in fluoroquinolone resistance, the European Commission has enforced strict regulations on the use of fluoroquinolones, leading to the suspension of their use for peri-operative antibiotic prophylaxis, including for prostate biopsy [130]. Current evidence indicates that in countries permitting the use of fluoroquinolones for antibiotic prophylaxis, it is recommended to administer a full day’s course or to use targeted therapy if fluoroquinolone resistance or augmented prophylaxis (combination of two or more different classes of antibiotics) for patients undergoing transrectal biopsy [131]. In patients in whom trans-perineal access is not possible, rectal swab followed by stool culture should be performed pre-biopsy. Such an approach enables the use of individual targeted antimicrobial therapy [131]. In countries where fluoroquinolones are not allowed for prostate biopsy prophylaxis, alternatives, such as cephalosporins, aminoglycosides, or Fosfomycin, can be used [131]. Moreover, various rectal preparation practices for transrectal biopsies, including enemas, povidone-iodine chlorhexidine applications and bowel preparation, are used [123]. The results of systematic review and meta-analysis demonstrated that povidone-iodine for rectal preparation before a prostate biopsy significantly decreased the risk of infection (RR 0.50, 95% CI 0.38–0.65) and the likelihood of hospitalization (RR 0.38, 95% CI 0.21–0.69). Another study showed the reduction in infection rate following the insertion of an iodophor cotton ball before placing an ultrasonic probe to the rectum during TRUS-guided prostate biopsy [132]. As a result, the trans-perineal approach, associated with a lower infection rate of 0.6%, is more and more frequently utilized [133,134]. However, as aforementioned, a recent randomized study demonstrated that transrectal biopsy with targeted prophylaxis, requiring rectal cultures and meticulous attention to the selection and administration of antibiotics, resulted in similar infection rates [35]. Targeted antibiotic prophylaxis, which relies on rectal swab and urine culture, is essential for preventing severe infections after rectal prostate biopsy [135]. However, a limitation of this approach is that screening for bacteria with resistance to a single antibiotic, such as cotrimoxazole, is not cost-effective due to the wide variety of bacterial colonies in the rectum. Therefore, routine screening generally targets multi-resistant strains, which does not eliminate the possibility of detecting bacteria resistant to only one antibiotic [136].
The trans-perineal approach carries a lower risk of hematochezia but a potentially higher risk of urinary retention depending on core sampling density [137]. Cognitive, fusion, and MRI in-bore biopsy using trans-perineal biopsies are usually conducted with the patient in the lithotomy position and the biopsy needle traverses the prostate in the craniocaudal plane from apex to base. Despite the trans-perineal approach, a transrectal ultrasound probe is still necessary for prostate imaging in cognitive and fusion biopsies. Brachytherapy grip and a stepper to stabilize it against the perineum may also be employed [138].
3.3. Number of Cores Per Target
The quantity of targeted cores obtained per lesion during targeted biopsy is important as it may affect the detection rate of csPCa and the estimation of Gleason scores [63]. Collection of only three to four cores (which is currently a standard practice) from high-volume lesions (e.g., PIRADS 5) may prove insufficient for precise estimation of Gleason scores [64]. Furthermore, the mpMRI technique has its limitations, including limited ability to predict extra-prostatic extension and local staging [76,139,140]. Consequently, relying solely on TB results may affect clinical decision-making processes, including the choice of local treatment or extension of surgical intervention.
Apart from the mpMRI, diverse ultrasound imaging techniques, such as contrast-enhanced ultrasound, computer-assisted TRUS, histoscanning, and sonoelastography are under development along with evaluation for effectiveness in localizing suspicious prostate lesions. Nevertheless, these methods require further refinement before potential integration into routine clinical practice [141].
4. Comparative Analysis of Systematic Biopsy vs. Other Diagnostic Techniques (Table 1)
The determination of the optimal biopsy strategy for patients presenting with suspected PCa lesions on MRI remains a subject of ongoing debate. SB has been suggested to be associated with a higher likelihood of overlooking aggressive PCa variants compared to fus-TB or combined biopsy (comPB) approaches, thereby posing a risk of undertreatment [142]. MpMRI of the prostate, including T2-weighted imaging, dynamic contrast enhancement, diffusion-weighted imaging (DWI) and interpretation using PI-RADS or a Likert scale, has demonstrated superior detection of csPCa and reduced identification of inPCa compared to standard transrectal biopsy [16,81,101,143,144]. Studies including men referred for biopsy due to clinical suspicion of prostate cancer have revealed that TB guided by MRI findings lead to lower rates of detecting inPCa compared to standard biopsies, with similar or enhanced detection rates for csPCa [55,69,145]. A systematic review and meta-analysis of 68 studies with a paired design and eight randomized clinical trials (RCTs) and a total of 14,709 men who received MRI-TB or SB or both demonstrated that MRI-TB more efficiently identified csPCa compared to SB (detection ratio [DR] 1.16 [95% confidence interval (CI) 1.09–1.24], p < 0.0001) as well as less inPCa (DR 0.66 [95% CI 0.57–0.76], p < 0.0001). The proportion of cores positive for cancer was also higher for MRI-TB than for systematic biopsy (relative risk (RR) 3.17 [95% CI 2.82–3.56], p < 0.0001). Moreover, adding SB to MRI-TB increased the likelihood of detecting insignificant cancer by 34% [145]. The GÖTEBORG-2 trial also demonstrated that utilization of TB alone decreased the detection of insignificant carcinomas [72].

Table 1.
Detection rates of clinically significant prostate cancers by systematic and targeted prostate biopsy.
Table 1.
Detection rates of clinically significant prostate cancers by systematic and targeted prostate biopsy.
| Study | Systematic Biopsy | Targeted Biopsy |
|---|---|---|
| Abd Ali, F., et al. [5] | 75% | 77% |
| Rouvière, O., et al. [69] | 14% | 20% |
| van der Leest, M., et al. [77] | 25% | 23% |
| Drost, F.-J.H., et al. [81] | 21,16% | 18.9% |
| Ahmed, H.U., et al. [101] | 51% | 49% |
| Klotz, L., et al. [144] | 30% | 35% |
| Kasivisvanathan, V., et al. [137] | 43% | 41% |
| Kasivisvanathan, V., et al. [112] | 26% | 38% |
| Porpiglia, F., et al. [146] | 44% | 18% |
| Tonttila, P.P., et al. [147] | 64% | 67% |
| Valerio, M., et al. [148] | 24% | 33% |
The outcomes from randomized controlled trials among biopsy-naïve subjects provide conflicting evidence regarding the superiority of MRI-TB over SB in detecting csPCa [112,146,147]. The results of the PRECISION study revealed that MRI followed by MRI-TB enabled the identification of more csPCa with fewer diagnoses of inPCa in men exhibiting an MRI-visible lesions [112]. Similar reduction of inPCa detection was demonstrated in the MRI-FIRST study [69]. Some studies revealed that MRI-targeted biopsy substantially enhanced cancer detection rates in individuals with prior negative biopsies but not in biopsy-naïve individuals [92,149].
In turn, Pezelj et al. [150] demonstrated that patients who received a TB exhibited a diminished incidence of under-grading. Although the proportion of positive cores between the mpMRI and non-mpMRI was comparable (35.3% versus 34.0%, p = 0.09), the TB group demonstrated a higher number of positive cores (4.6 vs. 3.4, p = 0.03). A greater amount of sampled material potentially facilitates more accurate tumor grading by pathologists [150]. Moreover, the prospective observational study demonstrated comparable detection rates in TB and SB; however, TB appeared to be more sensitive to intermediate- and high-grade tumors [5]. TB exhibited superior discriminatory efficacy in identifying PCa with ISUP 2 or higher, demonstrating a sensitivity of 90% and an 80% correct assignment rate. However, TB failed to detect nearly one-third of ISUP 1 tumors, among which 20% were csPCa based on current guidelines [5]. This limitation seems acceptable due to the typically indolent nature of ISUP 1 tumors, as evidenced by autopsy data indicating that a substantial proportion of men have undiagnosed PCa without compromising life expectancy. Moreover, recent research suggests delaying treatment for selected patients with intermediate-risk PCa, although definitive criteria for patient selection remain elusive [148,151]. It has been suggested that MRI-targeted biopsy may overlook some “MRI-invisible” low-volume ISUP 2 disease; however, the studies demonstrated that this type of cancer exhibits distinct biological characteristics compared to MRI-visible csPCa [152]. Overall survival for men with non-visible Gleason 3 + 4 reflected that of men with Gleason 3 + 3 disease, while men with MRI-visible prostate Gleason 3 + 4 cancer showed much worse outcomes [153]. Consequently, it has been suggested that the clinical relevance of Gleason 3 + 4 cancer identified via SB may differ from that detected via MRI-TB [85]. In turn, Nakanishi et al. [154] demonstrated that TB missed only 4.6% of csPCa cases in patients with PI-RADS 5 scores; however, it also missed as many as 22% of cases in men with PI-RADS 3 and 4 scores. Bryk et al. [57] observed a notable enhancement in the detection of csPCa with the addition of six ipsilateral SB to targeted biopsies. Conversely, contralateral SB primarily detected insignificant disease [57]. The problem of potentially overlooking the most representative regions within the target, including the so-called “penumbra”, is of high importance [107]. Recently, van der Leest et al. [77] demonstrated that incorporating four perilesional cores (“focal saturation”) improved csPCa detection. These findings indicate the potential for reduction in SB if both the lesion and surrounding tissue are adequately sampled, as suggested by PI-RADSv2.1 guidelines, which advocate for targeting both the lesion and its perilesional ‘penumbra’ [64]. Notably, all ‘target saturation biopsy methods’ are effective in diminishing potential targeting errors by surgeons or fusion software and in addressing the underestimation of lesion size on MRI [64].
In turn, the comparison of software-based three-dimensional-guided systematic prostate biopsy (3D-GSB) and conventional TRUS to assess PCa detection rates in 956 patients without prior positive biopsies and with a PSA value ≤ 20 ng/mL demonstrated no significant differences in the clinically csCDR between the 3D-GSB and TGSB groups (33.3% vs. 28.8%, p = 0.385) [155]. However, in this study, the overall CDR was significantly higher for 3D-GSB compared to TRUS (55.6% vs. 39.9%, p = 0.002). In addition, 3D-GSB detected significantly more non-significant PCa cases than TRUS (22.2% vs. 11.1%, p = 0.004). Moreover, in patients with PCa, TRUS yielded a significantly higher number of cancer-positive SB cores compared to 3D-GSB (42% vs. 25%, p < 0.001). Thus, in the opinion of the authors, at present, 3D-GSB does not seem to provide added value to conventional TRUS.
Additionally, fus-TB presents a favourable profile by increasing csPCa detection rates while reducing biopsy core requirements. While some studies report comparable overall PCa detection rates between fus-TB and SB, others highlight the superiority of the first in detecting csPCa [156,157]. One study demonstrated the superior capability of a combination of mpMRI with targeted fusion biopsy in detecting csPCa, compared to transrectal SB [71]. Vourganti et al. [158] also demonstrated that fus-TB enabled the identification of PCa in 34–37% of patients with previously negative SB, a third of whom exhibited a Gleason score of ≥7. In turn, the results of a meta-analysis and systematic review revealed no significant discrepancies in overall PCa detection rates between fus-TB and SB among patients with at least one prior negative biopsy [14]. However, subgroup analyses demonstrated a lower PCa detection rate with fus-TB in biopsy-naive patients compared to SB. Furthermore, subsequent analyses revealed that fus-TB significantly outperformed SB in detecting PCa in patients undergoing trans-perineal fus-TB; however, fus-TB did not exhibit superiority over SB in patients undergoing transrectal fus-TB [14]. It appears that the trans-perineal approach enhances overall PCa detection rates by targeting commonly missed anatomical sites, such as the apical, dorsolateral, and anterior prostatic segments [159]. A meta-analysis demonstrated that the trans-perineal approach to software fusion biopsy yielded a higher detection rate of both csPCa and anterior tumors, as well as a lower complication rate compared to the transrectal approach [160]. The trans-perineal approach also offers lower infection risks compared to transrectal methods. The superiority of fus-TB in detecting csPCa may be dependent upon sample size, as fus-TB did not outperform SB in detecting csPCa in subgroups with ≤100 samples. Moreover, the sequence of biopsy procedures may influence detection rates, with studies suggesting that performing SB first may reduce subsequent fus-TB accuracy due to tissue alterations induced by bleeding and oedema [161,162]. Conversely, performing fus-TB first may diminish the csPCa detection rate of SB as a result of the removal of tissue within clinically significant area. Moreover, the results of a systematic review and meta-analysis based on eight studies and 2603 men with suspected PCa demonstrated the non-inferiority of PCa diagnosis by the combination of TB + regional biopsy approach, thus suggesting the potential for the replacement of SB with FSB [64].
Many studies show the higher sensitivity of TB in identifying csPCa compared to standard biopsy however, due to the fact that they analysed only populations referred for biopsy based on clinical suspicion, the translation of findings to population-based screening appears challenging since, in such population, the majority of individuals referred to biopsy is expected to have lower risk of csPCa [163]. Table 1 presents selected trials and a meta-analysis with detection rates of significant prostate cancer by systematic and targeted biopsy.
5. Integration Strategies: Harmonizing Systematic and Targeted Biopsy
The MRI-based approach using the Prostate Imaging Reporting and Data System (PI-RADS) in prostate cancer evaluation has been demonstrated to enhance detection of csPCa, decrease inPCa identification, and lower the number of biopsies compared to systematic biopsy [77,101]. However, the use of MRI alone results in the omittance of a substantial amount of csPCa [4]. To ensure proper sampling of an MRI-detected lesion, a minimum of three to five cores is necessary [164,165]. Using additional perilesional or regional systematic biopsies, instead of standard sextant-based systematic biopsies, can reduce the total number of cores by avoiding systematic biopsies in MRI-negative lobes, as well as ameliorate the detection of csPCa by compensating for guidance imprecision [34]. Combined biopsy approaches, including MRI-TB and SB or fus-TB and SB, have also emerged as promising strategies to improve diagnostic efficacy, particularly in detecting csPCa [166,167]. Deng et al. [14] observed that comPB significantly augmented both overall PCa and csPCa detection rates compared to fus-TB alone. One of the meta-analyses emphasized the superiority of comPB over individual biopsy modalities in detecting csPCa [168]. Similarly, Krausewitz et al. [12] demonstrated a considerable rise in the detection rates of PCA and csPCa through combined biopsy techniques. The cumulative CDR was as high as 72%, closely resembling the results of the PRECISION trial’s CDR (71%) [112]. The authors observed that all biopsy methods when performed alone showed the underestimation of true tumor grading [12]. Other studies also indicated higher consistency with pathological tumor grading for combined biopsy compared to SB and MRI-TB [12,55]. Moreover, Krausewitz et al. [12] suggested that omitting SB could decrease unnecessary core sampling in nearly two-thirds of cases and reduce the number of men diagnosed with inPCa. In contrast, TB alone was associated with significantly improved efficiency in PCA and csPCa detection compared to SB and combined biopsy in overall and PI-RADS-dependent analyses (p < 0.001 for all), suggesting the potential to reduce biopsy-related anxiety, distress, pain, and risk of infections through a TB-limited approach [169]. However, such an approach was associated with a misdiagnosis rate of 7.4% for csPCa and 4.7% for cancers graded ≥ ISUP 4. Similarly, a comprehensive systematic literature search and analysis revealed that TB alone in MRI-positive men missed the diagnosis in 17.2% of men with ISUP grade 2 or higher PCA [4]. In turn, a combined approach including TB and focal perilesional saturation biopsy (FSB) has been suggested to decrease misdiagnosis rates of TB alone for csPCa and high-risk PCA by 92.3% and 80%, respectively [12]. However, the use of SB instead of FSB may result in a missed and/or underestimated csPCa rate of 4.7% and high-risk PCA rate of 8.5%. A proportion of 92% of misdiagnosed csPCa cases overlooked by FSB are located on the contralateral prostate lobe [64,105].
The combination of MRI-TB and SB during initial investigation is suggested by some authors; however, the precise contribution of SB to TB remains debatable [4,101,170,171]. Some experts believe that a combined approach can improve true tumor grading and that of extent, thus reducing the likelihood of misdiagnosis [55,69,172]. However, lack of certainty regarding tumor grading persists after the combined approach in one-third of cases [55]. It has been also implied that the specific reason underlying the enhanced performance of the additional combined approach could possibly be associated with the compensation for targeting errors, under-sampling of the target approach and MRI-invisible cancers, considering the multifocality of prostate cancer lesions [171,173]. The combination of lesion-targeted and SB leads to a greater yield of csPCa compared to either of these methods alone [17,55,56,71,166].
6. Conclusions
Precise risk stratification plays a pivotal role in the management of PCa patients, as it helps to lower the risk of overtreatment of inPCa as well as undertreatment of csPCa, thereby improving patients’ quality of life and optimizing treatment outcomes [14]. The results of recent studies demonstrate a shift towards a more selective approach in detecting high-risk cancers that need therapy, while adopting conservative methods in case of less aggressive tumors [5]. Guided biopsies are increasingly recommended due to their potential to enhance the detection of high-risk prostate cancer while reducing the identification of low-risk cases [174]. A Lower under-grading rate due to diminished sampling error further favors the rationale for adopting this technique as the standard in prostate cancer detection [14]. The trend towards MRI-directed management, typically involving mpMRI followed by MRI-targeted biopsy (MRI-TB), has resulted in increased utilization of MRI-TBs, prompting the standardization of MRI-TB techniques [87,175]. Isolated MRI-TB emerges as a suitable strategy for initial biopsy in biopsy-naïve individuals and those undergoing active surveillance (AS) [5]. Omitting additional SB decreases the incidence of septic complications and local inflammation, potentially improving subsequent surgical outcomes, but may also decrease the cancer detection rate. Therefore, the choice of biopsy strategy should be tailored to the individual patient’s risk profile, with a combined approach of targeted biopsies and at least perilesional sampling offering optimal sensitivity for detecting csPCa. Future advancements in imaging technologies and biopsy techniques, including artificial intelligence-augmented lesion detection and robotic-assisted sampling, hold promise for further enhancing the specificity and efficacy of PCa detection [176].
Author Contributions
Conceptualization, W.M., T.M. and Ł.N.; methodology W.M.; software, W.M.; validation, S.P., P.K. and O.T.; formal analysis W.M.; investigation, W.M.; resources, A.T.; data curation, W.M.; writing—original draft preparation, W.M.; writing—review and editing, W.M.; visualization, T.M.; supervision, Ł.N.; project administration, P.K. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
List of Abbreviations
| PCa | Prostate cancer |
| csPCA | clinically significant prostate carcinoma |
| inPCA | insignificant prostate cancer |
| MRI | magnetic resonance imaging |
| ISUP | International Society of Urological Pathology |
| PSA | Prostate-specific antigen |
| DRE | digital rectal examination |
| TRUS | transrectal ultrasound |
| CDR | cancer detection rates |
| GG | Grade group |
| SB | systematic biopsy |
| ROI | region of interest |
| GS | Gleason score |
| mpMRI | multiparametric magnetic resonance imaging |
| PI-RADS | Prostate Imaging Reporting and Data System |
| PSAD | prostate-specific antigen density |
| TR | transrectal |
| TP | trans-perineal |
| DWI | diffusion-weighted images |
| DCE | dynamic contrast-enhanced |
| TB | targeted biopsy |
| fus-TB | fusion targeted biopsy |
| comPB | combined prostate biopsy |
| RCT | randomized clinical trials |
| DR | detection ratio |
| CI | confidence interval |
| RR | relative risk |
| 3D GSB | three-dimensional-guided systematic prostate biopsy (3D-GSB) |
| FSB | focal perilesional saturation biopsy |
| AS | active surveillance |
References
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef]
- Siegel, R.L.; Giaquinto, A.N.; Jemal, A. Cancer statistics, 2024. CA Cancer J. Clin. 2024, 74, 12–49. [Google Scholar] [CrossRef]
- Bell, K.J.; Del Mar, C.; Wright, G.; Dickinson, J.; Glasziou, P. Prevalence of incidental prostate cancer: A systematic review of autopsy studies. Int. J. Cancer 2015, 137, 1749–1757. [Google Scholar] [CrossRef]
- Drost, F.J.; Osses, D.F.; Nieboer, D.; Steyerberg, E.W.; Bangma, C.H.; Roobol, M.J.; Schoots, I.G. Prostate MRI, with or without MRI-targeted biopsy, and systematic biopsy for detecting prostate cancer. Cochrane Database Syst. Rev. 2019, 4, Cd012663. [Google Scholar] [CrossRef] [PubMed]
- Abd Ali, F.; Sievert, K.-D.; Eisenblaetter, M.; Titze, B.; Hansen, T.; Barth, P.J.; Titze, U. MRI-Guided Targeted and Systematic Prostate Biopsies as Prognostic Indicators for Prostate Cancer Treatment Decisions. Cancers 2023, 15, 3915. [Google Scholar] [CrossRef]
- Epstein, J.I. An update of the Gleason grading system. J. Urol. 2010, 183, 433–440. [Google Scholar] [CrossRef] [PubMed]
- Epstein, J.I.; Egevad, L.; Amin, M.B.; Delahunt, B.; Srigley, J.R.; Humphrey, P.A.; Committee, G. The 2014 International Society of Urological Pathology (ISUP) consensus conference on Gleason grading of prostatic carcinoma: Definition of grading patterns and proposal for a new grading system. Am. J. Surg. Pathol. 2016, 40, 244–252. [Google Scholar] [CrossRef] [PubMed]
- Wolters, T.; Roobol, M.J.; van Leeuwen, P.J.; van den Bergh, R.C.; Hoedemaeker, R.F.; van Leenders, G.J.; Schröder, F.H.; van der Kwast, T.H. A critical analysis of the tumor volume threshold for clinically insignificant prostate cancer using a data set of a randomized screening trial. J. Urol. 2011, 185, 121–125. [Google Scholar] [CrossRef]
- Harnden, P.; Naylor, B.; Shelley, M.D.; Clements, H.; Coles, B.; Mason, M.D. The clinical management of patients with a small volume of prostatic cancer on biopsy: What are the risks of progression? A systematic review and meta-analysis. Cancer Interdiscip. Int. J. Am. Cancer Soc. 2008, 112, 971–981. [Google Scholar] [CrossRef]
- Gulati, R.; Psutka, S.P.; Etzioni, R. Personalized risks of over diagnosis for screen detected prostate cancer incorporating patient comorbidities: Estimation and communication. J. Urol. 2019, 202, 936–943. [Google Scholar] [CrossRef]
- Loeb, S.; Bjurlin, M.A.; Nicholson, J.; Tammela, T.L.; Penson, D.F.; Carter, H.B.; Carroll, P.; Etzioni, R. Overdiagnosis and overtreatment of prostate cancer. Eur. Urol. 2014, 65, 1046–1055. [Google Scholar] [CrossRef]
- Krausewitz, P.; Fostitsch, D.; Weiten, R.; Kluemper, N.; Stein, J.; Luetkens, J.; Kristiansen, G.; Ellinger, J.; Ritter, M. Current role of systematic biopsy in diagnosis of clinically significant prostate cancer in primary combined MRI-targeted biopsy: A high-volume single-center study. World J. Urol. 2023, 41, 19–25. [Google Scholar] [CrossRef]
- Djavan, B.; Margreiter, M. Biopsy standards for detection of prostate cancer. World J. Urol. 2007, 25, 11–17. [Google Scholar] [CrossRef]
- Deng, Y.S.; He, Y.H.; Ying, W.W.; Liu, H.L.; Li, P.Z.; Ma, C.Y.; Ding, Z.S.; Chen, X.; Wang, J.F.; Zhou, X.F. Value of three biopsy methods in prostate cancer detection: A meta-analysis and systematic review. Eur. Rev. Med. Pharmacol. Sci. 2021, 25, 2221–2234. [Google Scholar] [PubMed]
- Eichler, K.; Hempel, S.; Wilby, J.; Myers, L.; Bachmann, L.M.; Kleijnen, J. Diagnostic value of systematic biopsy methods in the investigation of prostate cancer: A systematic review. J. Urol. 2006, 175, 1605–1612. [Google Scholar] [CrossRef] [PubMed]
- Weinreb, J.C.; Barentsz, J.O.; Choyke, P.L.; Cornud, F.; Haider, M.A.; Macura, K.J.; Margolis, D.; Schnall, M.D.; Shtern, F.; Tempany, C.M. PI-RADS prostate imaging–reporting and data system: 2015, version 2. Eur. Urol. 2016, 69, 16–40. [Google Scholar] [CrossRef]
- Elkhoury, F.F.; Felker, E.R.; Kwan, L.; Sisk, A.E.; Delfin, M.; Natarajan, S.; Marks, L.S. Comparison of targeted vs systematic prostate biopsy in men who are biopsy naive: The prospective assessment of image registration in the diagnosis of prostate cancer (PAIREDCAP) study. JAMA Surg. 2019, 154, 811–818. [Google Scholar] [CrossRef]
- Presti, J.C.; O’DOWD, G.J.; Miller, M.C.; Mattu, R.; Veltri, R.W. Extended peripheral zone biopsy schemes increase cancer detection rates and minimize variance in prostate specific antigen and age related cancer rates: Results of a community multi-practice study. J. Urol. 2003, 169, 125–129. [Google Scholar] [CrossRef] [PubMed]
- Bosaily, A.E.-S.; Parker, C.; Brown, L.; Gabe, R.; Hindley, R.; Kaplan, R.; Emberton, M.; Ahmed, H.; Group, P. PROMIS—Prostate MR imaging study: A paired validating cohort study evaluating the role of multi-parametric MRI in men with clinical suspicion of prostate cancer. Contemp. Clin. Trials 2015, 42, 26–40. [Google Scholar] [CrossRef]
- Alqahtani, S.; Wei, C.; Zhang, Y.; Szewczyk-Bieda, M.; Wilson, J.; Huang, Z.; Nabi, G. Prediction of prostate cancer Gleason score upgrading from biopsy to radical prostatectomy using pre-biopsy multiparametric MRI PIRADS scoring system. Sci. Rep. 2020, 10, 7722. [Google Scholar] [CrossRef]
- Hu, Y.; Ahmed, H.U.; Carter, T.; Arumainayagam, N.; Lecornet, E.; Barzell, W.; Freeman, A.; Nevoux, P.; Hawkes, D.J.; Villers, A. A biopsy simulation study to assess the accuracy of several transrectal ultrasonography (TRUS)-biopsy strategies compared with template prostate mapping biopsies in patients who have undergone radical prostatectomy. BJU Int. 2012, 110, 812–820. [Google Scholar] [CrossRef]
- Taira, A.V.; Merrick, G.S.; Bennett, A.; Andreini, H.; Taubenslag, W.; Galbreath, R.W.; Butler, W.M.; Bittner, N.; Adamovich, E. Transperineal template-guided mapping biopsy as a staging procedure to select patients best suited for active surveillance. Am. J. Clin. Oncol. 2013, 36, 116–120. [Google Scholar] [CrossRef] [PubMed]
- Barzell, W.E.; Melamed, M.R.; Cathcart, P.; Moore, C.M.; Ahmed, H.U.; Emberton, M. Identifying candidates for active surveillance: An evaluation of the repeat biopsy strategy for men with favorable risk prostate cancer. J. Urol. 2012, 188, 762–768. [Google Scholar] [CrossRef]
- Cheng, E.; Davuluri, M.; Lewicki, P.J.; Hu, J.C.; Basourakos, S.P. Developments in optimizing transperineal prostate biopsy. Curr. Opin. Urol. 2022, 32, 85–90. [Google Scholar] [CrossRef] [PubMed]
- Ding, X.F.; Luan, Y.; Lu, S.M.; Zhou, G.C.; Huang, T.B.; Zhu, L.Y.; Guo, C.H. Risk factors for infection complications after transrectal ultrasound-guided transperineal prostate biopsy. World J. Urol. 2021, 39, 2463–2467. [Google Scholar] [CrossRef]
- Scattoni, V.; Maccagnano, C.; Zanni, G.; Angiolilli, D.; Raber, M.; Rigatti, P.; Montorsi, F. Systematic extended and saturation prostate biopsy: When and how. Minerva Urol. Nefrol. 2010, 62, 179–192. [Google Scholar] [PubMed]
- Kuru, T.H.; Wadhwa, K.; Chang, R.T.M.; Echeverria, L.M.C.; Roethke, M.; Polson, A.; Rottenberg, G.; Koo, B.; Lawrence, E.M.; Seidenader, J. Definitions of terms, processes and a minimum dataset for transperineal prostate biopsies: A standardization approach of the Ginsburg Study Group for Enhanced Prostate Diagnostics. BJU Int. 2013, 112, 568. [Google Scholar] [CrossRef] [PubMed]
- Jiang, X.; Zhu, S.; Feng, G.; Zhang, Z.; Li, C.; Li, H.; Wang, C.; Xu, Y. Is an initial saturation prostate biopsy scheme better than an extended scheme for detection of prostate cancer? A systematic review and meta-analysis. Eur. Urol. 2013, 63, 1031–1039. [Google Scholar] [CrossRef]
- Taneja, S.S.; Bjurlin, M.A.; Carter, H.B.; Cookson, M.; Gomella, L.G.; Penson, D.F.; Schellhammer, P.; Schlossberg, S.M.; Troyer, D.A.; Wheeler, T.; et al. AUA/Optimal Techniques of Prostate Biopsy and Specimen Handling. 2013. Available online: https://www.auanet.org/Documents/education/clinical-guidance/Prostate-Biopsy-WhitePaper.pdf (accessed on 22 July 2024).
- Abdulmajed, M.I.; Hughes, D.; Shergill, I.S. The role of transperineal template biopsies of the prostate in the diagnosis of prostate cancer: A review. Expert Rev. Med. Devices 2015, 12, 175–182. [Google Scholar] [CrossRef]
- Martorana, E.; Pirola, G.M.; Aisa, M.C.; Scialpi, P.; Di Blasi, A.; Saredi, G.; D’Andrea, A.; Signore, S.; Grisanti, R.; Scialpi, M. Prostate MRI and transperineal TRUS/MRI fusion biopsy for prostate cancer detection: Clinical practice updates. Turk. J. Urol. 2019, 45, 237. [Google Scholar] [CrossRef]
- Meyer, A.R.; Mamawala, M.; Winoker, J.S.; Landis, P.; Epstein, J.I.; Macura, K.J.; Allaf, M.E.; Partin, A.W.; Pavlovich, C.P.; Gorin, M.A. Transperineal prostate biopsy improves the detection of clinically significant prostate cancer among men on active surveillance. J. Urol. 2021, 205, 1069–1074. [Google Scholar] [CrossRef] [PubMed]
- Xiang, J.; Yan, H.; Li, J.; Wang, X.; Chen, H.; Zheng, X. Transperineal versus transrectal prostate biopsy in the diagnosis of prostate cancer: A systematic review and meta-analysis. World J. Surg. Oncol. 2019, 17, 31. [Google Scholar] [CrossRef] [PubMed]
- Cornford, P.; van den Bergh, R.C.; Briers, E.; Van den Broeck, T.; Brunckhorst, O.; Darraugh, J.; Eberli, D.; De Meerleer, G.; De Santis, M.; Farolfi, A.; et al. EAU-EANM-ESTRO-ESUR-ISUP-SIOG Guidelines on Prostate Cancer. Eur. Urol. 2024, 86, 148–163. [Google Scholar] [CrossRef] [PubMed]
- Hu, J.C.; Assel, M.; Allaf, M.E.; Ehdaie, B.; Vickers, A.J.; Cohen, A.J.; Ristau, B.T.; Green, D.A.; Han, M.; Rezaee, M.E.; et al. Transperineal Versus Transrectal Magnetic Resonance Imaging-targeted and Systematic Prostate Biopsy to Prevent Infectious Complications: The PREVENT Randomized Trial. Eur. Urol. 2024, 86, 61–68. [Google Scholar] [CrossRef]
- Wei, J.T.; Barocas, D.; Carlsson, S.; Coakley, F.; Eggener, S.; Etzioni, R.; Fine, S.W.; Han, M.; Kim, S.K.; Kirkby, E.; et al. Early detection of prostate cancer: AUA/SUO guideline part I: Prostate cancer screening. J. Urol. 2023, 210, 45–53. [Google Scholar] [CrossRef]
- Roberts, M.J.; Macdonald, A.; Ranasinghe, S.; Bennett, H.; Teloken, P.E.; Harris, P.; Paterson, D.; Coughlin, G.; Dunglison, N.; Esler, R. Transrectal versus transperineal prostate biopsy under intravenous anaesthesia: A clinical, microbiological and cost analysis of 2048 cases over 11 years at a tertiary institution. Prostate Cancer Prostatic Dis. 2021, 24, 169–176. [Google Scholar] [CrossRef]
- Urkmez, A.; Demirel, C.; Altok, M.; Bathala, T.K.; Shapiro, D.D.; Davis, J.W. Freehand versus Grid-Based Transperineal Prostate Biopsy: A Comparison of Anatomical Region Yield and Complications. J. Urol. 2021, 206, 894–902. [Google Scholar] [CrossRef]
- Basourakos, S.P.; Allaway, M.J.; Ross, A.E.; Schaeffer, E.M.; Hu, J.C.; Gorin, M.A. Local anaesthetic techniques for performing transperineal prostate biopsy. Nat. Rev. Urol. 2021, 18, 315–317. [Google Scholar] [CrossRef]
- Schaufler, C.; Daigle, R.; Singhaviranon, S.; Gjertson, C.K.; Albertsen, P.C.; Ristau, B.T. How many cores are enough? Optimizing the transperineal prostate biopsy template. Urol. Oncol. 2022, 40, 191.e1–191.e7. [Google Scholar] [CrossRef]
- Meng, M.V.; Elkin, E.P.; DuChane, J.; Carroll, P.R.; Investigators, C. Impact of increased number of biopsies on the nature of prostate cancer identified. J. Urol. 2006, 176, 63–69. [Google Scholar] [CrossRef]
- Kwon, H.J.; Rhew, S.A.; Yoon, C.E.; Shin, D.; Bang, S.; Park, Y.H.; Cho, H.J.; Ha, U.S.; Hong, S.-H.; Lee, J.Y.; et al. Comparing 12-core and 20-core biopsy for prostate cancer diagnosis with transperineal MR/US fusion biopsy: Assessing the effective number of systemic cores using propensity score matching. Int. Urol. Nephrol. 2023, 55, 2465–2471. [Google Scholar] [CrossRef]
- European Association of Urology. Prostate Cancer; European Association of Urology: Arnhem, The Netherlands, 2022. [Google Scholar]
- Ravery, V.; Goldblatt, L.; Royer, B.; Blanc, E.; Toublanc, M.; Boccon-Gibod, L. Extensive biopsy protocol improves the detection rate of prostate cancer. J. Urol. 2000, 164, 393–396. [Google Scholar] [CrossRef] [PubMed]
- Lee, A.Y.M.; Chen, K.; Tan, Y.G.; Lee, H.J.; Shutchaidat, V.; Fook-Chong, S.; Cheng, C.W.S.; Ho, H.S.S.; Yuen, J.S.P.; Ngo, N.T.; et al. Reducing the number of systematic biopsy cores in the era of MRI targeted biopsy—Implications on clinically-significant prostate cancer detection and relevance to focal therapy planning. Prostate Cancer Prostatic Dis. 2022, 25, 720–726. [Google Scholar] [CrossRef]
- Gore, J.L.; Shariat, S.F.; Miles, B.J.; Kadmon, D.; Jiang, N.; Wheeler, T.M.; Slawin, K.M. Optimal combinations of systematic sextant and laterally directed biopsies for the detection of prostate cancer. J. Urol. 2001, 165, 1554–1559. [Google Scholar] [CrossRef] [PubMed]
- Singh, H.; Canto, E.I.; Shariat, S.F.; Kadmon, D.; Miles, B.J.; Wheeler, T.M.; Slawin, K.M. Six additional systematic lateral cores enhance sextant biopsy prediction of pathological features at radical prostatectomy. J. Urol. 2004, 171, 204–209. [Google Scholar] [CrossRef]
- Ahdoot, M.; Lebastchi, A.H.; Turkbey, B.; Wood, B.; Pinto, P.A. Contemporary treatments in prostate cancer focal therapy. Curr. Opin. Oncol. 2019, 31, 200–206. [Google Scholar] [CrossRef] [PubMed]
- Tay, K.J.; Amin, M.B.; Ghai, S.; Jimenez, R.E.; Kench, J.G.; Klotz, L.; Montironi, R.; Muto, S.; Rastinehad, A.R.; Turkbey, B. Surveillance after prostate focal therapy. World J. Urol. 2019, 37, 397–407. [Google Scholar] [CrossRef]
- Aslim, E.J.; Law, Y.X.T.; Fook-Chong, S.M.C.; Ho, H.S.S.; Yuen, J.S.P.; Lau, W.K.O.; Lee, L.S.; Cheng, C.W.S.; Ngo, N.T.; Law, Y.M. Defining prostate cancer size and treatment margin for focal therapy: Does intralesional heterogeneity impact the performance of multiparametric MRI? BJU Int. 2021, 128, 178–186. [Google Scholar] [CrossRef]
- Wise, A.M.; Stamey, T.A.; McNeal, J.E.; Clayton, J.L. Morphologic and clinical significance of multifocal prostate cancers in radical prostatectomy specimens. Urology 2002, 60, 264–269. [Google Scholar] [CrossRef]
- Bott, S.R.; Ahmed, H.U.; Hindley, R.G.; Abdul-Rahman, A.; Freeman, A.; Emberton, M. The index lesion and focal therapy: An analysis of the pathological characteristics of prostate cancer. BJU Int. 2010, 106, 1607–1611. [Google Scholar] [CrossRef]
- Yu, A.; Yamany, T.; Mojtahed, A.; Hanna, N.; Nicaise, E.; Harisinghani, M.; Wu, C.-L.; Dahl, D.M.; Wszolek, M.; Blute, M.L. Combination MRI-targeted and systematic prostate biopsy may overestimate gleason grade on final surgical pathology and impact risk stratification. In Urologic Oncology: Seminars and Original Investigations; Elsevier: Amsterdam, The Netherlands, 2022. [Google Scholar]
- Mischinger, J.; Schöllnast, H.; Zurl, H.; Geyer, M.; Fischereder, K.; Adelsmayr, G.; Igrec, J.; Fritz, G.; Merdzo-Hörmann, M.; Elstner, J. Combining targeted and systematic prostate biopsy improves prostate cancer detection and correlation with the whole mount histopathology in biopsy naïve and previous negative biopsy patients. Front. Surg. 2022, 9, 1013389. [Google Scholar] [CrossRef]
- Ahdoot, M.; Wilbur, A.R.; Reese, S.E.; Lebastchi, A.H.; Mehralivand, S.; Gomella, P.T.; Bloom, J.; Gurram, S.; Siddiqui, M.; Pinsky, P. MRI-targeted, systematic, and combined biopsy for prostate cancer diagnosis. N. Engl. J. Med. 2020, 382, 917–928. [Google Scholar] [CrossRef]
- Brisbane, W.G.; Priester, A.M.; Ballon, J.; Kwan, L.; Delfin, M.K.; Felker, E.R.; Sisk, A.E.; Hu, J.C.; Marks, L.S. Targeted Prostate Biopsy: Umbra, Penumbra, and Value of Perilesional Sampling. Eur. Urol. 2022, 82, 303–310. [Google Scholar] [CrossRef] [PubMed]
- Bryk, D.J.; Llukani, E.; Taneja, S.S.; Rosenkrantz, A.B.; Huang, W.C.; Lepor, H. The role of ipsilateral and contralateral transrectal ultrasound-guided systematic prostate biopsy in men with unilateral magnetic resonance imaging lesion undergoing magnetic resonance imaging-ultrasound fusion-targeted prostate biopsy. Urology 2017, 102, 178–182. [Google Scholar] [CrossRef]
- Feuer, Z.; Meng, X.; Rosenkrantz, A.B.; Kasivisvanathan, V.; Moore, C.M.; Huang, R.; Deng, F.-M.; Lepor, H.; Wysock, J.S.; Huang, W.C. Application of the PRECISION trial biopsy strategy to a contemporary magnetic resonance imaging-targeted biopsy cohort—How many clinically significant prostate cancers are missed? J. Urol. 2021, 205, 740–747. [Google Scholar] [CrossRef]
- Tay, K.; Scheltema, M.; Ahmed, H.; Barret, E.; Coleman, J.; Dominguez-Escrig, J.; Ghai, S.; Huang, J.; Jones, J.; Klotz, L. Patient selection for prostate focal therapy in the era of active surveillance: An International Delphi Consensus Project. Prostate Cancer Prostatic Dis. 2017, 20, 294–299. [Google Scholar] [CrossRef]
- Patel, N.; Cricco-Lizza, E.; Kasabwala, K.; Xu, C.; Robinson, B.D.; Khani, F.; Wang, Y.; Margolis, D.; Hu, J.C. The role of systematic and targeted biopsies in light of overlap on magnetic resonance imaging ultrasound fusion biopsy. Eur. Urol. Oncol. 2018, 1, 263–267. [Google Scholar] [CrossRef] [PubMed]
- Lee, A.Y.; Yang, X.Y.; Lee, H.J.; Law, Y.M.; Huang, H.H.; Sim, A.S.; Lau, W.K.; Lee, L.S.; Cheng, C.W.; Ho, H.S. Limitations of overlapping cores in systematic and MRI-US fusion biopsy. In Urologic Oncology: Seminars and Original Investigations; Elsevier: Amsterdam, The Netherlands, 2021. [Google Scholar]
- Chung, J.H.; Park, B.K.; Song, W.; Kang, M.; Sung, H.H.; Jeon, H.G.; Jeong, B.C.; Seo, S.I.; Jeon, S.S.; Lee, H.M. TRUS-Guided Target Biopsy for a PI-RADS 3–5 Index Lesion to Reduce Gleason Score Underestimation: A Propensity Score Matching Analysis. Front. Oncol. 2022, 11, 824204. [Google Scholar] [CrossRef]
- Cata, E.; Andras, I.; Ferro, M.; Kadula, P.; Leucuta, D.; Musi, G.; Matei, D.-V.; De Cobelli, O.; Tamas-Szora, A.; Caraiani, C. Systematic sampling during MRI-US fusion prostate biopsy can overcome errors of targeting—Prospective single center experience after 300 cases in first biopsy setting. Transl. Androl. Urol. 2020, 9, 2510. [Google Scholar] [CrossRef] [PubMed]
- Hansen, N.L.; Barrett, T.; Lloyd, T.; Warren, A.; Samel, C.; Bratt, O.; Kastner, C. Optimising the number of cores for magnetic resonance imaging-guided targeted and systematic transperineal prostate biopsy. BJU Int. 2020, 125, 260–269. [Google Scholar] [CrossRef]
- Briganti, A.; Blute, M.L.; Eastham, J.H.; Graefen, M.; Heidenreich, A.; Karnes, J.R.; Montorsi, F.; Studer, U.E. Pelvic lymph node dissection in prostate cancer. Eur. Urol. 2009, 55, 1251–1265. [Google Scholar] [CrossRef]
- Walz, J.; Epstein, J.I.; Ganzer, R.; Graefen, M.; Guazzoni, G.; Kaouk, J.; Menon, M.; Mottrie, A.; Myers, R.P.; Patel, V.; et al. A Critical Analysis of the Current Knowledge of Surgical Anatomy of the Prostate Related to Optimisation of Cancer Control and Preservation of Continence and Erection in Candidates for Radical Prostatectomy: An Update. Eur. Urol. 2016, 70, 301–311. [Google Scholar] [CrossRef] [PubMed]
- Gandaglia, G.; Ploussard, G.; Valerio, M.; Marra, G.; Moschini, M.; Martini, A.; Roumiguié, M.; Fossati, N.; Stabile, A.; Beauval, J.-B. Prognostic implications of multiparametric magnetic resonance imaging and concomitant systematic biopsy in predicting biochemical recurrence after radical prostatectomy in prostate cancer patients diagnosed with magnetic resonance imaging–targeted biopsy. Eur. Urol. Oncol. 2020, 3, 739–747. [Google Scholar] [CrossRef] [PubMed]
- Gandaglia, G.; Martini, A.; Ploussard, G.; Fossati, N.; Stabile, A.; De Visschere, P.; Borgmann, H.; Heidegger, I.; Steinkohl, F.; Kretschmer, A. External validation of the 2019 Briganti nomogram for the identification of prostate cancer patients who should be considered for an extended pelvic lymph node dissection. Eur. Urol. 2020, 78, 138–142. [Google Scholar] [CrossRef]
- Rouvière, O.; Puech, P.; Renard-Penna, R.; Claudon, M.; Roy, C.; Mège-Lechevallier, F.; Decaussin-Petrucci, M.; Dubreuil-Chambardel, M.; Magaud, L.; Remontet, L.; et al. Use of prostate systematic and targeted biopsy on the basis of multiparametric MRI in biopsy-naive patients (MRI-FIRST): A prospective, multicentre, paired diagnostic study. Lancet Oncol. 2019, 20, 100–109. [Google Scholar] [CrossRef]
- Hanna, N.; Wszolek, M.F.; Mojtahed, A.; Nicaise, E.; Wu, B.; Gelpi-Hammerschmidt, F.J.; Salari, K.; Dahl, D.M.; Blute, M.L.; Harisinghani, M. Multiparametric magnetic resonance imaging-ultrasound fusion biopsy improves but does not replace standard template biopsy for the detection of prostate cancer. J. Urol. 2019, 202, 944–951. [Google Scholar] [CrossRef] [PubMed]
- Siddiqui, M.M.; Rais-Bahrami, S.; Turkbey, B.; George, A.K.; Rothwax, J.; Shakir, N.; Okoro, C.; Raskolnikov, D.; Parnes, H.L.; Linehan, W.M. Comparison of MR/ultrasound fusion–guided biopsy with ultrasound-guided biopsy for the diagnosis of prostate cancer. JAMA 2015, 313, 390–397. [Google Scholar] [CrossRef] [PubMed]
- Hugosson, J.; Månsson, M.; Wallström, J.; Axcrona, U.; Carlsson, S.V.; Egevad, L.; Geterud, K.; Khatami, A.; Kohestani, K.; Pihl, C.-G. Prostate cancer screening with PSA and MRI followed by targeted biopsy only. N. Engl. J. Med. 2022, 387, 2126–2137. [Google Scholar] [CrossRef]
- Johnson, D.C.; Raman, S.S.; Mirak, S.A.; Kwan, L.; Bajgiran, A.M.; Hsu, W.; Maehara, C.K.; Ahuja, P.; Faiena, I.; Pooli, A. Detection of individual prostate cancer foci via multiparametric magnetic resonance imaging. Eur. Urol. 2019, 75, 712–720. [Google Scholar] [CrossRef]
- Cash, H.; Maxeiner, A.; Stephan, C.; Fischer, T.; Durmus, T.; Holzmann, J.; Asbach, P.; Haas, M.; Hinz, S.; Neymeyer, J. The detection of significant prostate cancer is correlated with the Prostate Imaging Reporting and Data System (PI-RADS) in MRI/transrectal ultrasound fusion biopsy. World J. Urol. 2016, 34, 525–532. [Google Scholar] [CrossRef]
- Stabile, A.; Dell’Oglio, P.; De Cobelli, F.; Esposito, A.; Gandaglia, G.; Fossati, N.; Brembilla, G.; Cristel, G.; Cardone, G.; Losa, A. Association between Prostate Imaging Reporting and Data System (PI-RADS) score for the index lesion and multifocal, clinically significant prostate cancer. Eur. Urol. Oncol. 2018, 1, 29–36. [Google Scholar] [CrossRef] [PubMed]
- Malewski, W.; Milecki, T.; Szempliński, S.; Tayara, O.; Kuncman, Ł.; Kryst, P.; Nyk, Ł. Prostate Biopsy in the Case of PIRADS5—Is Systematic Biopsy Mandatory? J. Clin. Med. 2023, 12, 5612. [Google Scholar] [CrossRef] [PubMed]
- van der Leest, M.; Cornel, E.; Israel, B.; Hendriks, R.; Padhani, A.R.; Hoogenboom, M.; Zamecnik, P.; Bakker, D.; Setiasti, A.Y.; Veltman, J. Head-to-head comparison of transrectal ultrasound-guided prostate biopsy versus multiparametric prostate resonance imaging with subsequent magnetic resonance-guided biopsy in biopsy-naïve men with elevated prostate-specific antigen: A large prospective multicenter clinical study. Eur. Urol. 2019, 75, 570–578. [Google Scholar]
- Zhang, Y.; Zeng, N.; Zhang, F.; Huang, Y.; Tian, Y. How to make clinical decisions to avoid unnecessary prostate screening in biopsy-naïve men with PI-RADs v2 score ≤ 3? Int. J. Clin. Oncol. 2020, 25, 175–186. [Google Scholar] [CrossRef]
- Sfoungaristos, S.; Katafigiotis, I.; Perimenis, P. The role of PSA density to predict a pathological tumour upgrade between needle biopsy and radical prostatectomy for low risk clinical prostate cancer in the modified Gleason system era. Can. Urol. Assoc. J. 2013, 7, E722. [Google Scholar] [CrossRef] [PubMed]
- Magheli, A.; Hinz, S.; Hege, C.; Stephan, C.; Jung, K.; Miller, K.; Lein, M. Prostate specific antigen density to predict prostate cancer upgrading in a contemporary radical prostatectomy series: A single center experience. J. Urol. 2010, 183, 126–132. [Google Scholar] [CrossRef]
- Drost, F.-J.H.; Osses, D.; Nieboer, D.; Bangma, C.H.; Steyerberg, E.W.; Roobol, M.J.; Schoots, I.G. Prostate magnetic resonance imaging, with or without magnetic resonance imaging-targeted biopsy, and systematic biopsy for detecting prostate cancer: A Cochrane systematic review and meta-analysis. Eur. Urol. 2020, 77, 78–94. [Google Scholar] [CrossRef]
- Ljungberg, B.; Albiges, L.; Bensalah, K.; Bex, A.; Giles, R.; Hora, M.; Kuczyk, M.; Lam, T.; Marconi, L.; Canfield, S. EAU guidelines. Edn. presented at the EAU annual congress Amsterdam 2020. Eur. Urol. 2020, 67, 913–924. [Google Scholar] [CrossRef]
- Exterkate, L.; Wegelin, O.; Barentsz, J.O.; van der Leest, M.G.; Kummer, J.A.; Vreuls, W.; de Bruin, P.C.; Bosch, J.; van Melick, H.H.E.; Somford, D.M. Is There Still a Need for Repeated Systematic Biopsies in Patients with Previous Negative Biopsies in the Era of Magnetic Resonance Imaging-targeted Biopsies of the Prostate? Eur. Urol. Oncol. 2020, 3, 216–223. [Google Scholar] [CrossRef]
- Matulevičius, A.; Bakavičius, A.; Ulys, A.; Trakymas, M.; Ušinskienė, J.; Naruševičiūtė, I.; Sabaliauskaitė, R.; Žukauskaitė, K.; Jarmalaitė, S.; Jankevičius, F. Multiparametric MRI Fusion-Guided Prostate Biopsy for Detection of Clinically Significant Prostate Cancer Eliminates the Systemic Prostate Biopsy. Appl. Sci. 2022, 12, 10151. [Google Scholar] [CrossRef]
- Kasivisvanathan, V.; Emberton, M.; Moore, C.M. There Is No Longer a Role for Systematic Biopsies in Prostate Cancer Diagnosis. Eur. Urol. Open Sci. 2022, 38, 12–13. [Google Scholar] [CrossRef] [PubMed]
- Carlsson, S.; Jäderling, F.; Wallerstedt, A.; Nyberg, T.; Stranne, J.; Thorsteinsdottir, T.; Carlsson, S.V.; Bjartell, A.; Hugosson, J.; Haglind, E. Oncological and functional outcomes 1 year after radical prostatectomy for very-low-risk prostate cancer: Results from the prospective LAPPRO trial. BJU Int. 2016, 118, 205–212. [Google Scholar] [CrossRef]
- Chang, S.D.; Ghai, S.; Kim, C.K.; Oto, A.; Giganti, F.; Moore, C.M. MRI Targeted Prostate Biopsy Techniques: AJR Expert Panel Narrative Review. AJR Am. J. Roentgenol. 2021, 217, 1263–1281. [Google Scholar] [CrossRef] [PubMed]
- Hamdy, F.C.; Donovan, J.L.; Lane, J.A.; Metcalfe, C.; Davis, M.; Turner, E.L.; Martin, R.M.; Young, G.J.; Walsh, E.I.; Bryant, R.J.; et al. Fifteen-Year Outcomes after Monitoring, Surgery, or Radiotherapy for Prostate Cancer. N. Engl. J. Med. 2023, 388, 1547–1558. [Google Scholar] [CrossRef]
- Sazuka, T.; Imamoto, T.; Namekawa, T.; Utsumi, T.; Yanagisawa, M.; Kawamura, K.; Kamiya, N.; Suzuki, H.; Ueda, T.; Ota, S. Analysis of preoperative detection for apex prostate cancer by transrectal biopsy. Prostate Cancer 2013, 2013, 705865. [Google Scholar] [CrossRef]
- Lane, B.R.; Zippe, C.D.; Abouassaly, R.; Schoenfield, L.; Magi-Galluzzi, C.; Jones, J.S. Saturation technique does not decrease cancer detection during followup after initial prostate biopsy. J. Urol. 2008, 179, 1746–1750, discussion 1750. [Google Scholar] [CrossRef] [PubMed]
- Roehl, K.A.; Antenor, J.A.; Catalona, W.J. Serial biopsy results in prostate cancer screening study. J. Urol. 2002, 167, 2435–2439. [Google Scholar] [CrossRef] [PubMed]
- Schoots, I.G.; Roobol, M.J.; Nieboer, D.; Bangma, C.H.; Steyerberg, E.W.; Hunink, M.G. Magnetic resonance imaging-targeted biopsy may enhance the diagnostic accuracy of significant prostate cancer detection compared to standard transrectal ultrasound-guided biopsy: A systematic review and meta-analysis. Eur. Urol. 2015, 68, 438–450. [Google Scholar] [CrossRef]
- Tu, X.; Liu, Z.; Zhang, C.; Chang, T.; Xu, H.; Bao, Y.; Li, J.; Jin, K.; Yuan, Q.; Qiu, S.; et al. Diagnostic Role of Magnetic Resonance Imaging-Targeted Biopsy for Prostate Cancer in Biopsy-Naïve Men: A Meta-Analysis. Urol. Int. 2020, 104, 187–198. [Google Scholar] [CrossRef]
- Yuan, L.; Zhang, C.; Lu, L.; Ruan, L.; Lan, J.; Feng, S.; Luo, J. Comparison of ultrasound-guided transrectal and transperineal prostate biopsies in clinical application. Zhonghua Nan Ke Xue = Natl. J. Androl. 2014, 20, 1004–1007. [Google Scholar]
- Grummet, J.P.; Weerakoon, M.; Huang, S.; Lawrentschuk, N.; Frydenberg, M.; Moon, D.A.; O’Reilly, M.; Murphy, D. Sepsis and ‘superbugs’: Should we favour the transperineal over the transrectal approach for prostate biopsy? BJU Int. 2014, 114, 384–388. [Google Scholar] [CrossRef] [PubMed]
- Miller, J.; Perumalla, C.; Heap, G. Complications of transrectal versus transperineal prostate biopsy. ANZ J. Surg. 2005, 75, 48–50. [Google Scholar] [CrossRef]
- Ghafoori, M.; Velayati, M.; Ghasabeh, M.A.; Shakiba, M.; Alavi, M. Prostate biopsy using transrectal ultrasonography; the optimal number of cores regarding cancer detection rate and complications. Iran. J. Radiol. 2015, 12, e13257. [Google Scholar] [CrossRef] [PubMed]
- Carneiro, A.; Sivaraman, A.; Sánchez-Salas, R.; Nunes-Silva, I.; Baghdadi, M.; Srougi, V.; Di Trapani, E.; Pizzaro, F.U.; Doizi, S.; Barret, E. Un mayor número de cilindros de biopsia transrectal de próstata guiada por ultrasonido se asocia con una mayor pérdida de sangre y complicaciones perioperatorias en la prostatectomía radical asistida por robot. Actas Urológicas Españolas 2017, 41, 155–161. [Google Scholar] [CrossRef] [PubMed]
- Szabo, R.J. “Free-Hand” transperineal prostate biopsy under local anesthesia: Review of the literature. J. Endourol. 2021, 35, 525–543. [Google Scholar] [CrossRef]
- Sathianathen, N.J.; Omer, A.; Harriss, E.; Davies, L.; Kasivisvanathan, V.; Punwani, S.; Moore, C.M.; Kastner, C.; Barrett, T.; Van Den Bergh, R.C. Negative predictive value of multiparametric magnetic resonance imaging in the detection of clinically significant prostate cancer in the prostate imaging reporting and data system era: A systematic review and meta-analysis. Eur. Urol. 2020, 78, 402–414. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, H.U.; Bosaily, A.E.-S.; Brown, L.C.; Gabe, R.; Kaplan, R.; Parmar, M.K.; Collaco-Moraes, Y.; Ward, K.; Hindley, R.G.; Freeman, A. Diagnostic accuracy of multi-parametric MRI and TRUS biopsy in prostate cancer (PROMIS): A paired validating confirmatory study. Lancet 2017, 389, 815–822. [Google Scholar] [CrossRef]
- Lombardo, R.; Tema, G.; Nacchia, A.; Mancini, E.; Franco, S.; Zammitti, F.; Franco, A.; Cash, H.; Gravina, C.; Guidotti, A.; et al. Role of Perilesional Sampling of Patients Undergoing Fusion Prostate Biopsies. Life 2023, 13, 1719. [Google Scholar] [CrossRef]
- Priester, A.; Natarajan, S.; Khoshnoodi, P.; Margolis, D.J.; Raman, S.S.; Reiter, R.E.; Huang, J.; Grundfest, W.; Marks, L.S. Magnetic resonance imaging underestimation of prostate cancer geometry: Use of patient specific molds to correlate images with whole mount pathology. J. Urol. 2017, 197, 320–326. [Google Scholar] [CrossRef]
- Noujeim, J.-P.; Belahsen, Y.; Lefebvre, Y.; Lemort, M.; Deforche, M.; Sirtaine, N.; Martin, R.; Roumeguere, T.; Peltier, A.; Diamand, R. Optimizing multiparametric magnetic resonance imaging-targeted biopsy and detection of clinically significant prostate cancer: The role of perilesional sampling. Prostate Cancer Prostatic Dis. 2023, 26, 575–580. [Google Scholar] [CrossRef]
- Tschirdewahn, S.; Wiesenfarth, M.; Bonekamp, D.; Püllen, L.; Reis, H.; Panic, A.; Kesch, C.; Darr, C.; Heß, J.; Giganti, F. Detection of significant prostate cancer using target saturation in transperineal magnetic resonance imaging/transrectal ultrasonography–fusion biopsy. Eur. Urol. Focus 2021, 7, 1300–1307. [Google Scholar] [CrossRef]
- Diamand, R.; Hollans, M.; Lefebvre, Y.; Sirtaine, N.; Limani, K.; Hawaux, E.; Abou Zahr, R.; Mattlet, A.; Albisinni, S.; Roumeguère, T. The role of perilesional and multiparametric resonance imaging-targeted biopsies to reduce the risk of upgrading at radical prostatectomy pathology: A retrospective monocentric study. In Urologic Oncology: Seminars and Original Investigations; Elsevier: Amsterdam, The Netherlands, 2022. [Google Scholar]
- Padhani, A.R.; Weinreb, J.; Rosenkrantz, A.B.; Villeirs, G.; Turkbey, B.; Barentsz, J. Prostate imaging-reporting and data system steering committee: PI-RADS v2 status update and future directions. Eur. Urol. 2019, 75, 385–396. [Google Scholar] [CrossRef] [PubMed]
- Cool, D.W.; Romagnoli, C.; Izawa, J.I.; Chin, J.; Gardi, L.; Tessier, D.; Mercado, A.; Mandel, J.; Ward, A.D.; Fenster, A. Comparison of prostate MRI-3D transrectal ultrasound fusion biopsy for first-time and repeat biopsy patients with previous atypical small acinar proliferation. Can. Urol. Assoc. J. 2016, 10, 342–348. [Google Scholar] [CrossRef] [PubMed]
- Natarajan, S.; Marks, L.S.; Margolis, D.J.; Huang, J.; Macairan, M.L.; Lieu, P.; Fenster, A. Clinical application of a 3D ultrasound-guided prostate biopsy system. In Urologic Oncology: Seminars and Original Investigations; Elsevier: Amsterdam, The Netherlands, 2011. [Google Scholar]
- Ukimura, O.; Desai, M.M.; Palmer, S.; Valencerina, S.; Gross, M.; Abreu, A.L.; Aron, M.; Gill, I.S. 3-Dimensional elastic registration system of prostate biopsy location by real-time 3-dimensional transrectal ultrasound guidance with magnetic resonance/transrectal ultrasound image fusion. J. Urol. 2012, 187, 1080–1086. [Google Scholar] [CrossRef]
- Mendhiratta, N.; Rosenkrantz, A.B.; Meng, X.; Wysock, J.S.; Fenstermaker, M.; Huang, R.; Deng, F.M.; Melamed, J.; Zhou, M.; Huang, W.C.; et al. Magnetic Resonance Imaging-Ultrasound Fusion Targeted Prostate Biopsy in a Consecutive Cohort of Men with No Previous Biopsy: Reduction of Over Detection through Improved Risk Stratification. J. Urol. 2015, 194, 1601–1606. [Google Scholar] [CrossRef] [PubMed]
- Kasivisvanathan, V.; Rannikko, A.S.; Borghi, M.; Panebianco, V.; Mynderse, L.A.; Vaarala, M.H.; Briganti, A.; Budäus, L.; Hellawell, G.; Hindley, R.G.; et al. MRI-Targeted or Standard Biopsy for Prostate-Cancer Diagnosis. N. Engl. J. Med. 2018, 378, 1767–1777. [Google Scholar] [CrossRef]
- Mozer, P.; Rouprêt, M.; Le Cossec, C.; Granger, B.; Comperat, E.; de Gorski, A.; Cussenot, O.; Renard-Penna, R. First round of targeted biopsies using magnetic resonance imaging/ultrasonography fusion compared with conventional transrectal ultrasonography-guided biopsies for the diagnosis of localised prostate cancer. BJU Int. 2015, 115, 50–57. [Google Scholar] [CrossRef]
- Ukimura, O.; Marien, A.; Palmer, S.; Villers, A.; Aron, M.; de Castro Abreu, A.L.; Leslie, S.; Shoji, S.; Matsugasumi, T.; Gross, M.; et al. Trans-rectal ultrasound visibility of prostate lesions identified by magnetic resonance imaging increases accuracy of image-fusion targeted biopsies. World J. Urol. 2015, 33, 1669–1676. [Google Scholar] [CrossRef]
- Baco, E.; Rud, E.; Eri, L.M.; Moen, G.; Vlatkovic, L.; Svindland, A.; Eggesbø, H.B.; Ukimura, O. A Randomized Controlled Trial To Assess and Compare the Outcomes of Two-core Prostate Biopsy Guided by Fused Magnetic Resonance and Transrectal Ultrasound Images and Traditional 12-core Systematic Biopsy. Eur. Urol. 2016, 69, 149–156. [Google Scholar] [CrossRef]
- Verma, S.; Choyke, P.L.; Eberhardt, S.C.; Oto, A.; Tempany, C.M.; Turkbey, B.; Rosenkrantz, A.B. The current state of MR imaging–targeted biopsy techniques for detection of prostate cancer. Radiology 2017, 285, 343–356. [Google Scholar] [CrossRef]
- Tilak, G.; Tuncali, K.; Song, S.E.; Tokuda, J.; Olubiyi, O.; Fennessy, F.; Fedorov, A.; Penzkofer, T.; Tempany, C.; Hata, N. 3T MR-guided in-bore transperineal prostate biopsy: A comparison of robotic and manual needle-guidance templates. J. Magn. Reson. Imaging 2015, 42, 63–71. [Google Scholar] [CrossRef]
- Pokorny, M.; Kua, B.; Esler, R.; Yaxley, J.; Samaratunga, H.; Dunglison, N.; Gianduzzo, T.; Coughlin, G.; Holt, R.; Laing, B. MRI-guided in-bore biopsy for prostate cancer: What does the evidence say? A case series of 554 patients and a review of the current literature. World J. Urol. 2019, 37, 1263–1279. [Google Scholar] [CrossRef]
- Grummet, J.; Pepdjonovic, L.; Huang, S.; Anderson, E.; Hadaschik, B. Transperineal vs. transrectal biopsy in MRI targeting. Transl. Androl. Urol. 2017, 6, 368. [Google Scholar] [CrossRef] [PubMed]
- Cicione, A.; De Nunzio, C.; Manno, S.; Damiano, R.; Posti, A.; Lima, E.; Tubaro, A.; Balloni, F. An update on prostate biopsy in the era of magnetic resonance imaging. Minerva Urol. Nefrol. = Ital. J. Urol. Nephrol. 2018, 70, 264–274. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Perdomo, H.A.; Mejia, N.G.; Fernandez, L.; Carbonell, J. Effectiveness of periprostatic block to prevent pain in transrectal prostate biopsy: A systematic review and a network meta-analysis. Cent. Eur. J. Urol. 2019, 72, 121. [Google Scholar]
- Yang, Y.; Liu, Z.; Wei, Q.; Cao, D.; Yang, L.; Zhu, Y.; Wei, X.; Tang, Z.; Liu, L.; Han, P. The efficiency and safety of intrarectal topical anesthesia for transrectal ultrasound-guided prostate biopsy: A systematic review and meta-analysis. Urol. Int. 2017, 99, 373–383. [Google Scholar] [CrossRef] [PubMed]
- Pradere, B.; Veeratterapillay, R.; Dimitropoulos, K.; Yuan, Y.; Omar, M.I.; MacLennan, S.; Cai, T.; Bruyère, F.; Bartoletti, R.; Köves, B.; et al. Nonantibiotic Strategies for the Prevention of Infectious Complications following Prostate Biopsy: A Systematic Review and Meta-Analysis. J. Urol. 2021, 205, 653–663. [Google Scholar] [CrossRef]
- Liss, M.A.; Ehdaie, B.; Loeb, S.; Meng, M.V.; Raman, J.D.; Spears, V.; Stroup, S.P. An update of the American Urological Association white paper on the prevention and treatment of the more common complications related to prostate biopsy. J. Urol. 2017, 198, 329–334. [Google Scholar] [CrossRef]
- Borghesi, M.; Ahmed, H.; Nam, R.; Schaeffer, E.; Schiavina, R.; Taneja, S.; Weidner, W.; Loeb, S. Complications After Systematic, Random, and Image-guided Prostate Biopsy. Eur. Urol. 2017, 71, 353–365. [Google Scholar] [CrossRef]
- Anastasiadis, E.; van der Meulen, J.; Emberton, M. Hospital admissions after transrectal ultrasound-guided biopsy of the prostate in men diagnosed with prostate cancer: A database analysis in E ngland. Int. J. Urol. 2015, 22, 181–186. [Google Scholar] [CrossRef]
- Solomon, S.L.; Oliver, K.B. Antibiotic resistance threats in the United States: Stepping back from the brink. Am. Fam. Physician 2014, 89, 938–941. [Google Scholar]
- The Food and Drug Administration (FDA). FDA Drug Safety Communication: FDA Updates Warnings for Oral and Injectable Fluoroquinolone Antibiotics Due to Disabling Side Effects. Available online: https://www.fda.gov/drugs/drug-safety-and-availability/fda-drug-safety-communication-fda-updates-warnings-oral-and-injectable-fluoroquinolone-antibiotics (accessed on 2 June 2019).
- The Food and Drug Administration (FDA). Drug Safety Communication: FDA Warns about Increased Risk of Ruptures or Tears in the Aorta Blood Vessel with Fluoroquinolone Antibiotics in Certain Patients. 2018. Available online: https://www.fda.gov/drugs/drug-safety-and-availability/fda-warns-about-increased-risk-ruptures-or-tears-aorta-blood-vessel-fluoroquinolone-antibiotics (accessed on 3 June 2024).
- Disabling and Potentially Permanent Side Effects Lead to Suspension or Restrictions of Quinolone and Fluoroquinolone Antibiotics. EMA/175398/2019. 2019. Available online: https://www.ema.europa.eu/en/news/disabling-potentially-permanent-side-effects-lead-suspension-or-restrictions-quinolone-fluoroquinolone-antibiotics (accessed on 22 July 2024).
- Pilatz, A.; Dimitropoulos, K.; Veeratterapillay, R.; Yuan, Y.; Omar, M.I.; MacLennan, S.; Cai, T.; Bruyère, F.; Bartoletti, R.; Köves, B.; et al. Antibiotic Prophylaxis for the Prevention of Infectious Complications following Prostate Biopsy: A Systematic Review and Meta-Analysis. J. Urol. 2020, 204, 224–230. [Google Scholar] [CrossRef] [PubMed]
- Yu, L.; Ma, L.; Yu, H. Impact of insertion timing of iodophor cotton ball on the control of infection complications after transrectal ultrasound guided prostate biopsy. Zhonghua Yi Xue Za Zhi 2014, 94, 609–611. [Google Scholar] [PubMed]
- Davis, P.; Paul, E.; Grummet, J. Current practice of prostate biopsy in Australia and New Zealand: A survey. Urol. Ann. 2015, 7, 315–319. [Google Scholar] [CrossRef] [PubMed]
- Günzel, K.; Magheli, A.; Baco, E.; Cash, H.; Heinrich, S.; Neubert, H.; Schlegel, J.; Schostak, M.; Henkel, T.; Asbach, P. Infection rate and complications after 621 transperineal MRI-TRUS fusion biopsies in local anesthesia without standard antibiotic prophylaxis. World J. Urol. 2021, 39, 3861–3866. [Google Scholar] [CrossRef] [PubMed]
- Jahnen, M.; Amiel, T.; Kirchoff, F.; Büchler, J.W.; Herkommer, K.; Rothe, K.; Meissner, V.H.; Gschwend, J.E.; Lunger, L. Cotrimoxazole and targeted antibiotic prophylaxis for transrectal prostate biopsy: A single-center study. World J. Urol. 2024, 42, 260. [Google Scholar] [CrossRef] [PubMed]
- Elshal, A.M.; Atwa, A.M.; El-Nahas, A.R.; El-Ghar, M.A.; Gaber, A.; Elsawy, E.; Hashem, A.; Farag, Y.; Farg, H.; Elsorougy, A. Chemoprophylaxis during transrectal prostate needle biopsy: Critical analysis through randomized clinical trial. World J. Urol. 2018, 36, 1845–1852. [Google Scholar] [CrossRef]
- Bhanji, Y.; Allaway, M.J.; Gorin, M.A. Recent advances and current role of transperineal prostate biopsy. Urol. Clin. N. Am. 2021, 48, 25–33. [Google Scholar] [CrossRef]
- Thomson, A.; Li, M.; Grummet, J.; Sengupta, S. Transperineal prostate biopsy: A review of technique. Transl. Androl. Urol. 2020, 9, 3009. [Google Scholar] [CrossRef]
- Pooli, A.; Johnson, D.C.; Shirk, J.; Markovic, D.; Sadun, T.Y.; Sisk Jr, A.E.; Mohammadian Bajgiran, A.; Afshari Mirak, S.; Felker, E.R.; Hughes, A.K. Predicting pathological tumor size in prostate cancer based on multiparametric prostate magnetic resonance imaging and preoperative findings. J. Urol. 2021, 205, 444–451. [Google Scholar] [CrossRef]
- Triquell, M.; Regis, L.; Winkler, M.; Valdés, N.; Cuadras, M.; Celma, A.; Planas, J.; Morote, J.; Trilla, E. Multiparametric MRI for staging of prostate cancer: A multicentric analysis of predictive factors to improve identification of extracapsular extension before radical prostatectomy. Cancers 2022, 14, 3966. [Google Scholar] [CrossRef] [PubMed]
- Kuru, T.H.; Fütterer, J.J.; Schiffmann, J.; Porres, D.; Salomon, G.; Rastinehad, A.R. Transrectal ultrasound (US), contrast-enhanced US, real-time elastography, HistoScanning, magnetic resonance imaging (MRI), and MRI-US fusion biopsy in the diagnosis of prostate cancer. Eur. Urol. Focus 2015, 1, 117–126. [Google Scholar] [CrossRef] [PubMed]
- Szewczyk-Bieda, M.; Wei, C.; Coll, K.; Gandy, S.; Donnan, P.; Ragupathy, S.K.A.; Singh, P.; Wilson, J.; Nabi, G. A multicentre parallel-group randomised trial assessing multiparametric MRI characterisation and image-guided biopsy of prostate in men suspected of having prostate cancer: MULTIPROS study protocol. Trials 2019, 20, 638. [Google Scholar] [CrossRef] [PubMed]
- Turkbey, B.; Rosenkrantz, A.B.; Haider, M.A.; Padhani, A.R.; Villeirs, G.; Macura, K.J.; Tempany, C.M.; Choyke, P.L.; Cornud, F.; Margolis, D.J. Prostate imaging reporting and data system version 2.1: 2019 update of prostate imaging reporting and data system version 2. Eur. Urol. 2019, 76, 340–351. [Google Scholar] [CrossRef] [PubMed]
- Klotz, L.; Chin, J.; Black, P.C.; Finelli, A.; Anidjar, M.; Bladou, F.; Mercado, A.; Levental, M.; Ghai, S.; Chang, S.D. Comparison of multiparametric magnetic resonance imaging–targeted biopsy with systematic transrectal ultrasonography biopsy for biopsy-naive men at risk for prostate cancer: A phase 3 randomized clinical trial. JAMA Oncol. 2021, 7, 534–542. [Google Scholar] [CrossRef]
- Kasivisvanathan, V.; Stabile, A.; Neves, J.B.; Giganti, F.; Valerio, M.; Shanmugabavan, Y.; Clement, K.D.; Sarkar, D.; Philippou, Y.; Thurtle, D. Magnetic resonance imaging-targeted biopsy versus systematic biopsy in the detection of prostate cancer: A systematic review and meta-analysis. Eur. Urol. 2019, 76, 284–303. [Google Scholar] [CrossRef]
- Porpiglia, F.; Manfredi, M.; Mele, F.; Cossu, M.; Bollito, E.; Veltri, A.; Cirillo, S.; Regge, D.; Faletti, R.; Passera, R. Diagnostic pathway with multiparametric magnetic resonance imaging versus standard pathway: Results from a randomized prospective study in biopsy-naïve patients with suspected prostate cancer. Eur. Urol. 2017, 72, 282–288. [Google Scholar] [CrossRef]
- Tonttila, P.P.; Lantto, J.; Pääkkö, E.; Piippo, U.; Kauppila, S.; Lammentausta, E.; Ohtonen, P.; Vaarala, M.H. Prebiopsy Multiparametric Magnetic Resonance Imaging for Prostate Cancer Diagnosis in Biopsy-naive Men with Suspected Prostate Cancer Based on Elevated Prostate-specific Antigen Values: Results from a Randomized Prospective Blinded Controlled Trial. Eur. Urol. 2016, 69, 419–425. [Google Scholar] [CrossRef]
- Preisser, F.; Cooperberg, M.R.; Crook, J.; Feng, F.; Graefen, M.; Karakiewicz, P.I.; Klotz, L.; Montironi, R.; Nguyen, P.L.; D’Amico, A.V. Intermediate-risk prostate cancer: Stratification and management. Eur. Urol. Oncol. 2020, 3, 270–280. [Google Scholar] [CrossRef]
- Valerio, M.; Donaldson, I.; Emberton, M.; Ehdaie, B.; Hadaschik, B.A.; Marks, L.S.; Mozer, P.; Rastinehad, A.R.; Ahmed, H.U. Detection of clinically significant prostate cancer using magnetic resonance imaging–ultrasound fusion targeted biopsy: A systematic review. Eur. Urol. 2015, 68, 8–19. [Google Scholar] [CrossRef]
- Pezelj, I.; Pirša, M.; Svaguša, I.; Nikles, S.; Tomić, M.; Knežević, M.; Tomašković, I.; Krušlin, B. Comparison of Grading Accuracy of Prostate Cancer in Samples Acquired by a Targeted and Systemic Prostate Biopsy. Acta Clin. Croat. 2022, 61 (Suppl. S3), 28–31. [Google Scholar] [CrossRef] [PubMed]
- Overland, M.R.; Washington III, S.L.; Carroll, P.R.; Cooperberg, M.R.; Herlemann, A. Active surveillance for intermediate-risk prostate cancer: Yes, but for whom? Curr. Opin. Urol. 2019, 29, 605–611. [Google Scholar] [CrossRef] [PubMed]
- Li, P.; You, S.; Nguyen, C.; Wang, Y.; Kim, J.; Sirohi, D.; Ziembiec, A.; Luthringer, D.; Lin, S.-C.; Daskivich, T. Genes involved in prostate cancer progression determine MRI visibility. Theranostics 2018, 8, 1752. [Google Scholar] [CrossRef] [PubMed]
- Stavrinides, V.; Giganti, F.; Trock, B.; Punwani, S.; Allen, C.; Kirkham, A.; Freeman, A.; Haider, A.; Ball, R.; McCartan, N. Five-year outcomes of magnetic resonance imaging–based active surveillance for prostate cancer: A large cohort study. Eur. Urol. 2020, 78, 443–451. [Google Scholar] [CrossRef]
- Nakanishi, Y.; Ito, M.; Fukushima, H.; Yokoyama, M.; Kataoka, M.; Ikuta, S.; Sakamoto, K.; Takemura, K.; Suzuki, H.; Tobisu, K.-i. Who can avoid systematic biopsy without missing clinically significant prostate cancer in men who undergo magnetic resonance imaging-targeted biopsy? Clin. Genitourin. Cancer 2019, 17, e664–e671. [Google Scholar] [CrossRef]
- Derigs, F.; Kowalewski, K.F.; Hartung, F.O.; Waldbillig, F.; Neuberger, M.; von Hardenberg, J.; Westhoff, N. A Matched-pair Analysis Comparing Systematic Prostate Biopsy by Conventional Transrectal Ultrasound-guidance Versus Software-based Predefined 3D-Guidance. Urology 2023, 177, 128–133. [Google Scholar] [CrossRef]
- Ristau, B.T.; Chen, D.Y.T.; Ellis, J.; Malhotra, A.; DeMora, L.; Parsons, R.B.; Milestone, B.; Brody, M.; Viterbo, R.; Greenberg, R.; et al. Defining Novel and Practical Metrics to Assess the Deliverables of Multiparametric Magnetic Resonance Imaging/Ultrasound Fusion Prostate Biopsy. J. Urol. 2018, 199, 969–975. [Google Scholar] [CrossRef]
- Shin, T.; Smyth, T.B.; Ukimura, O.; Ahmadi, N.; de Castro Abreu, A.L.; Oishi, M.; Mimata, H.; Gill, I.S. Detection of prostate cancer using magnetic resonance imaging/ultrasonography image-fusion targeted biopsy in African-American men. BJU Int. 2017, 120, 233–238. [Google Scholar] [CrossRef]
- Vourganti, S.; Rastinehad, A.; Yerram, N.; Nix, J.; Volkin, D.; Hoang, A.; Turkbey, B.; Gupta, G.N.; Kruecker, J.; Linehan, W.M.; et al. Multiparametric magnetic resonance imaging and ultrasound fusion biopsy detect prostate cancer in patients with prior negative transrectal ultrasound biopsies. J. Urol. 2012, 188, 2152–2157. [Google Scholar] [CrossRef]
- Ber, Y.; Segal, N.; Tamir, S.; Benjaminov, O.; Yakimov, M.; Sela, S.; Halstauch, D.; Baniel, J.; Kedar, D.; Margel, D. A noninferiority within-person study comparing the accuracy of transperineal to transrectal MRI-US fusion biopsy for prostate-cancer detection. Prostate Cancer Prostatic Dis. 2020, 23, 449–456. [Google Scholar] [CrossRef]
- Rai, B.P.; Mayerhofer, C.; Somani, B.K.; Kallidonis, P.; Nagele, U.; Tokas, T. Magnetic resonance imaging/ultrasound fusion-guided transperineal versus magnetic resonance imaging/ultrasound fusion-guided transrectal prostate biopsy—A systematic review. Eur. Urol. Oncol. 2021, 4, 904–913. [Google Scholar] [CrossRef] [PubMed]
- Rastinehad, A.R.; Turkbey, B.; Salami, S.S.; Yaskiv, O.; George, A.K.; Fakhoury, M.; Beecher, K.; Vira, M.A.; Kavoussi, L.R.; Siegel, D.N.; et al. Improving detection of clinically significant prostate cancer: Magnetic resonance imaging/transrectal ultrasound fusion guided prostate biopsy. J. Urol. 2014, 191, 1749–1754. [Google Scholar] [CrossRef]
- Borkowetz, A.; Platzek, I.; Toma, M.; Laniado, M.; Baretton, G.; Froehner, M.; Koch, R.; Wirth, M.; Zastrow, S. Comparison of systematic transrectal biopsy to transperineal magnetic resonance imaging/ultrasound-fusion biopsy for the diagnosis of prostate cancer. BJU Int. 2015, 116, 873–879. [Google Scholar] [CrossRef]
- Eklund, M.; Jäderling, F.; Discacciati, A.; Bergman, M.; Annerstedt, M.; Aly, M.; Glaessgen, A.; Carlsson, S.; Grönberg, H.; Nordström, T. MRI-Targeted or Standard Biopsy in Prostate Cancer Screening. N. Engl. J. Med. 2021, 385, 908–920. [Google Scholar] [CrossRef] [PubMed]
- Deniffel, D.; Perlis, N.; Ghai, S.; Girgis, S.; Healy, G.M.; Fleshner, N.; Hamilton, R.; Kulkarni, G.; Toi, A.; van der Kwast, T.; et al. Prostate biopsy in the era of MRI-targeting: Towards a judicious use of additional systematic biopsy. Eur. Radiol. 2022, 32, 7544–7554. [Google Scholar] [CrossRef]
- Barrett, T.; de Rooij, M.; Giganti, F.; Allen, C.; Barentsz, J.O.; Padhani, A.R. Quality checkpoints in the MRI-directed prostate cancer diagnostic pathway. Nat. Rev. Urol. 2023, 20, 9–22. [Google Scholar] [CrossRef]
- Borkowetz, A.; Hadaschik, B.; Platzek, I.; Toma, M.; Torsev, G.; Renner, T.; Herout, R.; Baunacke, M.; Laniado, M.; Baretton, G.; et al. Prospective comparison of transperineal magnetic resonance imaging/ultrasonography fusion biopsy and transrectal systematic biopsy in biopsy-naïve patients. BJU Int. 2018, 121, 53–60. [Google Scholar] [CrossRef] [PubMed]
- Hakozaki, Y.; Matsushima, H.; Kumagai, J.; Murata, T.; Masuda, T.; Hirai, Y.; Oda, M.; Kawauchi, N.; Yokoyama, M.; Homma, Y. A prospective study of magnetic resonance imaging and ultrasonography (MRI/US)-fusion targeted biopsy and concurrent systematic transperineal biopsy with the average of 18-cores to detect clinically significant prostate cancer. BMC Urol. 2017, 17, 117. [Google Scholar] [CrossRef]
- Tang, Y.; Liu, Z.; Tang, L.; Zhang, R.; Lu, Y.; Liang, J.; Zou, Z.; Zhou, C.; Wang, Y. Significance of MRI/Transrectal Ultrasound Fusion Three-Dimensional Model-Guided, Targeted Biopsy Based on Transrectal Ultrasound-Guided Systematic Biopsy in Prostate Cancer Detection: A Systematic Review and Meta-Analysis. Urol. Int. 2018, 100, 57–65. [Google Scholar] [CrossRef]
- Krausewitz, P.; Schmeller, H.; Luetkens, J.; Dabir, D.; Ellinger, J.; Ritter, M.; Conrad, R. Prospective analysis of pain expectancy and experience during MR-fusion prostate biopsy: Does reality match patients’ expectancy? World J. Urol. 2022, 40, 2239–2244. [Google Scholar] [CrossRef]
- Mottet, N.; van den Bergh, R.C.; Briers, E.; Van den Broeck, T.; Cumberbatch, M.G.; De Santis, M.; Fanti, S.; Fossati, N.; Gandaglia, G.; Gillessen, S. EAU-EANM-ESTRO-ESUR-SIOG guidelines on prostate cancer—2020 update. Part 1: Screening, diagnosis, and local treatment with curative intent. Eur. Urol. 2021, 79, 243–262. [Google Scholar] [CrossRef]
- Williams, C.; Ahdoot, M.; Daneshvar, M.A.; Hague, C.; Wilbur, A.R.; Gomella, P.T.; Shih, J.; Khondakar, N.; Yerram, N.; Mehralivand, S.; et al. Why does magnetic resonance imaging-targeted biopsy miss clinically significant cancer? J. Urol. 2022, 207, 95–107. [Google Scholar] [CrossRef] [PubMed]
- Westhoff, N.; Baeßler, B.; von Hardenberg, J.; Hetjens, S.; Porubsky, S.; Siegel, F.; Martini, T.; Michel, M.S.; Attenberger, U.; Ritter, M. Systematic prostate biopsy still matters: A comprehensive analysis of MRI/TRUS-fusion targeted prostate biopsies across different indications. In Urologic Oncology: Seminars and Original Investigations; Elsevier: Amsterdam, The Netherlands, 2019. [Google Scholar]
- Westhoff, N.; Haumann, H.; Kriegmair, M.C.; Von Hardenberg, J.; Budjan, J.; Porubsky, S.; Michel, M.S.; Honeck, P.; Ritter, M. Association of training level and outcome of software-based image fusion-guided targeted prostate biopsies. World J. Urol. 2019, 37, 2119–2127. [Google Scholar] [CrossRef]
- Tomašković, I.; Pezelj, I.; Bolanča Čulo, K.; Novosel, L.; Nikles, S.; Tomić, M.; Reljić, A.; Katušić, J.; Knežević, M.; Pirša, M. Diagnostic value of cognitive-registration multiparametric magnetic resonance guided biopsy for the detection of prostate cancer after initial negative biopsy. Acta Clin. Croat. 2018, 57 (Suppl. 1), 40–45. [Google Scholar] [PubMed]
- Moore, C.M.; Kasivisvanathan, V.; Eggener, S.; Emberton, M.; Fütterer, J.J.; Gill, I.S.; Grubb Iii, R.L.; Hadaschik, B.; Klotz, L.; Margolis, D.J. Standards of reporting for MRI-targeted biopsy studies (START) of the prostate: Recommendations from an International Working Group. Eur. Urol. 2013, 64, 544–552. [Google Scholar] [CrossRef] [PubMed]
- Oerther, B.; Engel, H.; Nedelcu, A.; Schlett, C.L.; Grimm, R.; von Busch, H.; Sigle, A.; Gratzke, C.; Bamberg, F.; Benndorf, M. Prediction of upgrade to clinically significant prostate cancer in patients under active surveillance: Performance of a fully automated AI-algorithm for lesion detection and classification. Prostate 2023, 83, 871–878. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).