Effect of Flexible Sacrum Position on Maternal and Neonatal Outcomes in Public Health Facilities, Amhara Regional State, Ethiopia: A Quasi-Experimental Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design, Setting and Period
Sample Size Determination
- The women in the FSP were allowed to change position among the FSP (standing, kneeling, squatting, all four, seat birth and lateral positions);
- For laboring women to change among the above-listed FSP positions, they were allowed to have a companion with them to assist when standing, walking, squatting and on birth seat position.
- Continuous follow-up and labor support by the trained midwives.
- The trained midwives applied different pain relief methods and perineal support: different types of perineal support methods were applied in different FSP positions to reduce risk of perineal tear. All the above intervention strategies were applied to the intervention group only, because it needs by its nature to have safe labor and delivery services. To apply the intervention, equipments used were mattresses (for all four positions, kneeling, sometimes for squatting position), seats for birth seat position (for laboring mothers and the midwives attending labor in birth seat position), and screen sheets (to separate mothers in different types of birth position).
2.2. Outcome Ascertainment
2.3. Data Quality Control, Data Collection Tools and Procedures
2.4. Data Analysis
3. Results
3.1. Socio-Demographic Characteristics of the Study Participants
3.2. Flexible Sacrum Birth Positions used at the Time of Birth
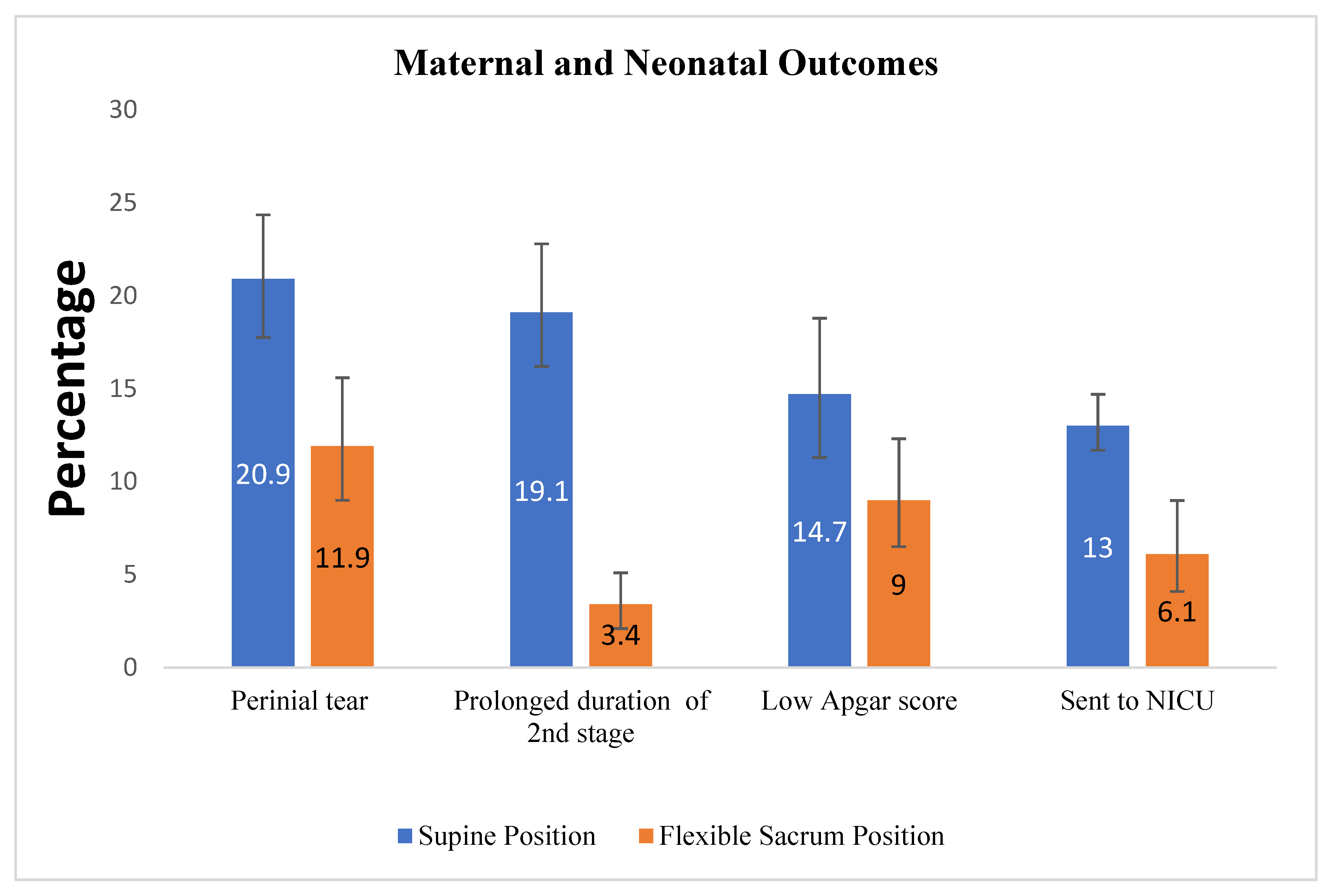
3.3. Maternal and Neonatal Outcomes in the Intervention Group Compared to the Control Group
3.4. Effect of Flexible Sacrum Position on Maternal and Neonatal Outcomes
4. Discussion
5. Conclusions
6. Clinical Implication and Recommendation
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Declercq, E.R.; Sakala, C.; Corry, M.P.; Applebaum, S. Listening to mothers II: Report of the second national US survey of women’s childbearing experiences. J. Perinat. Educ. 2007, 16, 9–14. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Olson, R.; Olson, C.; Cox, N.S. Maternal birthing positions and perineal injury. J. Fam. Pract. 1990, 30, 553–557. [Google Scholar] [PubMed]
- Gupta, J.K.; Sood, A.; Hofmeyr, G.J.; Vogel, J.P. Position in the second stage of labour for women without epidural anaesthesia. Cochrane Database Syst. Rev. 2017, 5, Cd002006. [Google Scholar] [CrossRef]
- Kemp, E.; Kingswood, C.J.; Kibuka, M.; Thornton, J.G. Position in the second stage of labour for women with epidural anaesthesia. Cochrane Database Syst. Rev. 2013, 1, CD008070. [Google Scholar]
- Lindgren, H.E.; Brink, Å.; Klingberg-Allvin, M. Fear causes tears-perineal injuries in home birth settings. A Swedish interview study. BMC Pregnancy Childbirth 2011, 11, 6. [Google Scholar] [CrossRef] [Green Version]
- World Health Organization. Making Pregnancy Safer: The Critical Role of the Skilled Attendant: A Joint Statement by WHO, ICM and FIGO; World Health Organization: Geneva, Switzerland, 2004.
- Jowitt, M. Dynamic Positions in Birth; Pinter Martin: London, UK, 2014. [Google Scholar]
- Walsh, D. Evidence and Skills for Normal Labour and Birth: A Guide for Midwives; Routledge: London, UK, 2011. [Google Scholar]
- Coppen, R. Birthing Positions: What Do Women Want? Do Midwives Know Best? Quay Books: Salisbury, UK, 2005. [Google Scholar]
- Dundes, L. The evolution of maternal birthing position. Am. J. Public Health 1987, 77, 636–641. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Johanson, R.; Newburn, M.; Macfarlane, A. Has the medicalisation of childbirth gone too far. BMJ 2002, 324, 892–895. [Google Scholar] [CrossRef] [Green Version]
- Adachi, K.S.M.; Usui, A. The relationship between the parturient’s positions and perceptions of labor pain intensity. Nurs. Res. 2003, 52, 47–51. [Google Scholar] [CrossRef]
- de Jonge, A.; Rijnders, M.E.; van Diem, M.T.; Scheepers, P.L.; Lagro-Janssen, A.L. Are there inequalities in choice of birthing position? Sociodemographic and labour factors associated with the supine position during the second stage of labour. Midwifery 2009, 25, 439–448. [Google Scholar] [CrossRef]
- De Jonge, A.; Van Diem, M.T.; Scheepers, P.L.H.; Buitendijk, S.E.; Lagro-Janssen, A.L.M. Risk of perineal damage is not a reason to discourage a sitting birthing position: A secondary analysis. Int. J. Clin. Pract. 2010, 64, 611–618. [Google Scholar] [CrossRef]
- BgO, G.M. Puerperal women’s perceptions on vertical and horizontal deliveries. Rev. Lat. Am. Enfermagem. 2009, 17, 153–159. [Google Scholar]
- Lugina, H.M.R.; Smith, H. Mobility and maternal position during childbirth in Tanzania: An exploratory study at four government hospitals. BMC Pregnancy Childbirth. 2004, 4, 3. [Google Scholar] [CrossRef] [Green Version]
- Thilagavathy, G. Maternal Birthing Position and Outcome of Labor; The Journal of Family Welfare: Mumbai, India, 2012. [Google Scholar]
- Nieuwenhuijze, M.; Jonge, A.; Korstjens, I.; Lagro-Jansse, T. Factors influencing the fulfillment of women’s preferences for birthing positions during second stage of labor. J. Psychosom. Obstet. Gynecol. 2012, 33, 25–31. [Google Scholar] [CrossRef] [PubMed]
- Schirmer, J.; Fustinoni, S.M.; Basile, A.L.d.O. Perineal outcomes on the left lateral versus vertical semi-sitting birth positions: A randomized study. Acta Paul. Enferm. 2011, 24, 745–750. [Google Scholar] [CrossRef] [Green Version]
- Thies-Lagergren, L.; Kvist, L.J.; Christensson, K.; Hildingsson, I. Striving for scientific stringency: A re-analysis of a randomised controlled trial considering first-time mothers’ obstetric outcomes in relation to birth position. BMC Pregnancy Childbirth 2012, 12, 135. [Google Scholar] [CrossRef] [Green Version]
- McPherson, K.C.; Beggs, A.D.; Sultan, A.H.; Thakar, R. Can the risk of obstetric anal sphincter injuries (OASIs) be predicted using a risk-scoring system? BMC Res. Notes 2014, 7, 471. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hutton, E.K.; Cappelletti, A.; Reitsma, A.H.; Simioni, J.; Horne, J.; McGregor, C.; Ahmed, R.J. Outcomes associated with planned place of birth among women with low-risk pregnancies. CMAJ 2016, 188, E80–E90. [Google Scholar] [CrossRef] [Green Version]
- De Jong, P.; Johanson, R.; Baxen, P.; Adrians, V.; Van der Westhuisen, S.; Jones, P. Randomised trial comparing the upright and supine positions for the second stage of labour. BJOG 1997, 104, 567–571. [Google Scholar] [CrossRef]
- Walker, C.R.T.; Herranz, A.; Espinosa, J.A.; Sánchez, E.; Espuña-Pons, M. Alternative model of birth to reduce the risk of assisted vaginal delivery and perineal trauma. Int. Urogynecol. J. 2012, 23, 1249–1256. [Google Scholar] [CrossRef]
- Simkin, P.P.; O’hara, M. Nonpharmacologic relief of pain during labor: Systematic reviews of five methods. Am. J. Obstet. Gynecol. 2002, 186, S131–S159. [Google Scholar] [CrossRef]
- Meyvis, I.; Van Rompaey, B.; Goormans, K.; Truijen, S.; Lambers, S.; Mestdagh, E.; Mistiaen, W. Maternal position and other variables: Effects on perineal outcomes in 557 births. Birth 2012, 39, 115–120. [Google Scholar] [CrossRef] [PubMed]
- Smith, L.A.; Price, N.; Simonite, V.; Burns, E.E. Incidence of and risk factors for perineal trauma: A prospective observational study. BMC Pregnancy Childbirth 2013, 13, 59. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zang, Y.; Lu, H.; Zhao, Y.; Huang, J.; Ren, L.; Li, X. Effects of flexible sacrum positions during the second stage of labour on maternal and neonatal outcomes: A systematic review and meta-analysis. J. Clin. Nurs. 2020, 29, 3154–3169. [Google Scholar] [CrossRef] [PubMed]
- WHO Guidelines Approved by the Guidelines Review Committee. In WHO Recommendations: Intrapartum Care for a Positive Childbirth Experience; World Health Organization: Geneva, Switzerland, 2018.
- Berta, M.; Lindgren, H.; Christensson, K.; Mekonnen, S.; Adefris, M. Effect of maternal birth positions on duration of second stage of labor: Systematic review and meta-analysis. BMC Pregnancy Childbirth 2019, 19, 466. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dabral, A.; Pawar, P.; Bharti, R.; Kumari, A.; Batra, A.; Arora, R. Upright kneeling position during second stage of labor: A pilot study. Int. J. Reprod. Contracept. Obst. Gynecol. 2018, 7, 401–407. [Google Scholar] [CrossRef]
- Argaw, M.; Mesfin, Y.; Demissie, E. Birth-Related Perineal Tear and Its Associated Factors Among Mothers Who Delivered in Atat Hospital. Int. J. Childbirth 2022, 12, 107–113. [Google Scholar] [CrossRef]
- Reis, V.; Deller, B.; Catherine Carr, C.; Smith, J. Respectful Maternity Care; USAID: Washington, DC, USA, 2012.
- World Health Organization. Standards for Improving Quality of Maternal and Newborn Care in Health Facilities; World Health Organization: Geneva, Switzerland, 2016.
- Sheferaw, E.D.; Bazant, E.; Gibson, H.; Fenta, H.B.; Ayalew, F.; Belay, T.B.; Worku, M.M.; Kebebu, A.E.; Woldie, S.A.; Kim, Y.M.; et al. Respectful maternity care in Ethiopian public health facilities. Reprod. Health 2017, 14, 60. [Google Scholar] [CrossRef]
- Asefa, A.B.D. Status of respectful and non-abusive care during facility-based childbirth in a hospital and health centers in Addis Ababa, Ethiopia. Reprod. Health 2015, 12, 33. [Google Scholar] [CrossRef] [Green Version]
- Edqvist, M.H.I.; Mollberg, M.; Lundgren, I.; Lindgren, H. Midwives’ Management during the Second Stage of Labor in Relation to Second-Degree Tears-An Experimental Study. Birth 2017, 44, 86–94. [Google Scholar] [CrossRef] [Green Version]
- Daniilidis, A.; Markis, V.; Tzafetas, M.; Loufopoulos, P.; Hatzis, P.; Vrachnis, N.; Dinas, K. Third degree perineal lacerations-How, why and when? A review analysis. Open J. Obstet. Gynecol. 2012, 2, 304. [Google Scholar] [CrossRef] [Green Version]
- No, G.T.G. The management of third-and fourth-degree perineal tears. MIDIRS 2015, 2, 9. [Google Scholar]
- Shorten, A.; Donsante, J.; Shorten, B. Birth position, accoucheur, and perineal outcomes: Informing women about choices for vaginal birth. Birth 2002, 29, 18–27. [Google Scholar] [CrossRef] [PubMed]
- Caughey, A.B.; Cahill, A.G.; Guise, J.-M.; Rouse, D.J.; Obstetricians, A. Safe prevention of the primary cesarean delivery. Am. J. Obstet. Gynecol. 2014, 210, 179–193. [Google Scholar] [CrossRef] [PubMed]
- Gudayu, T.W. Proportion and factors associated with low fifth minute Apgar score among singleton newborn babies in Gondar University Referral Hospital; North West Ethiopia. Afr. Health Sci. 2017, 17, 1–6. [Google Scholar] [CrossRef]
- Apgar, V. A proposal for a new method of evaluation of the newborn. Classic Papers Crit. Care 1952, 32, 97. [Google Scholar]
- Apgar, V. Further observations on the newborn scoring system. Am. J. Dis. Child. 1962, 104, 419–428. [Google Scholar] [CrossRef]
- Casey, B.M.; McIntire, D.D.; Leveno, K.J. The continuing value of the Apgar score for the assessment of newborn infants. N. Engl. J. Med. 2001, 344, 467–471. [Google Scholar] [CrossRef]
- Creswell, J.W. Educational Research: Planning, Conducting, and Evaluating Quantitative; Prentice Hall Upper: Saddle River, NJ, USA, 2002. [Google Scholar]
- He, S.J.H.; Qian, X.; Garner, P. Women’s experience of episiotomy: A qualitative study from China. BMJ Open 2020, 10, e033354. [Google Scholar] [CrossRef]
- Soong, B.B.M. Maternal position at midwife-attended birth and perineal trauma: Is there an association? Birth 2005, 32, 164–169. [Google Scholar] [CrossRef]
- Mayanja, R.; Chakura, A.; Mubiru, M.; Masembe, S.; Nkonwa, I.; Njagi, J.; Ngonzi, J. Association between Duration of Second Stage of Labour and Perinatal Outcomes among Mothers admitted in Labour at Mbarara Regional Referral Hospital, Uganda. ASRJETS 2016, 25, 112–130. [Google Scholar]
- Yousuf, J.; Ayalew, M.; Seid, F. Maternal health beliefs, attitudes and practices among Ethiopian Afar. Exchange 2011, 1, 12–15. [Google Scholar]
- Mushtari, F.H.S. Perceptions on birth positions among midwives and obstetricians at malalai maternity hospital and badakhshan provincial hospital, Afghanistan. J. Midwifery Women’s Health 2011, 56, 528. [Google Scholar] [CrossRef]
- Zhang, H.Y.; Shu, R.; Zhao, N.N.; Lu, Y.J.; Chen, M.; Li, Y.X.; Cai, W.Z. Comparing maternal and neonatal outcomes between hands-and-knees delivery position and supine position. Int. J. Nurs. Sci. 2016, 3, 178–184. [Google Scholar] [CrossRef] [Green Version]
- Gupta, J.K.; Sood, A.; Hofmeyr, G.J.; Vogel, J.P. Position in the second stage of labour for women without epidural anaesthesia. Cochrane Database Syst. Rev. 2012, 5, CD002006. [Google Scholar] [CrossRef]
- Elvander, C.A.M.; Thies-Lagergren, L.; Cnattingius, S.; Stephansson, O. Birth position and obstetric anal sphincter injury: A population-based study of 113 000 spontaneous births. BMC Pregnancy Childbirth 2015, 15, 252. [Google Scholar] [CrossRef] [Green Version]
- World Health Organization. WHO Recommendations on Intrapartum Care for a Positive Childbirth Experience; World Health Organization: Geneva, Switzerland, 2018.
- Moraloglu, O.; Kansu-Celik, H.; Tasci, Y.; Karakaya, B.K.; Yilmaz, Y.; Cakir, E.; Yakut, H.I. The influence of different maternal pushing positions on birth outcomes at the second stage of labor in nulliparous women. J. Matern. Neonatal Med. 2017, 30, 245–249. [Google Scholar] [CrossRef]
- Mirzakhani, K.; Karimi, F.Z.; Mohamadzadeh Vatanchi, A.; Feroz Zaidi, F. The effect of maternal position on maternal, fetal and neonatal outcomes: A systematic review. J. Midwifery Reprod. Health 2020, 8, 1988–2004. [Google Scholar]
- Humphrey, M.; Hounslow, D.; Morgan, S.; Wood, C. The influence of maternal posture at birth on the fetus. BJOG 1974, 29, 392. [Google Scholar] [CrossRef]
- Gizzo, S.; Di Gangi, S.; Noventa, M.; Bacile, V.; Zambon, A.; Nardelli, G.B. Women’s choice of positions during labour: Return to the past or a modern way to give birth? A cohort study in Italy. BioMed Res. Int. 2014, 2014, 638093. [Google Scholar] [CrossRef]



| Variables | Control Group (N = 360) | Intervention Group (N = 688) | |
|---|---|---|---|
| Age | 15–24 years | 125 (34.7%) | 240 (34.9%) |
| 25–34 years | 190 (52.8%) | 361 (52.5%) | |
| 35–54 years | 45 (12.5%) | 87 (12.6%) | |
| Residence | Urban Rural | 257 (71.4%) 103 (28.6%) | 473 (68.8%) 215 (31.3%) |
| Type of health facility | Hospital | 280 (77.8%) | 542 (78.8%) |
| Health center | 80 (22.2%) | 146 (21.2%) | |
| Marital status | Married | 347 (96.4%) | 648 (94.2%) |
| Single | 13 (3.6%) | 40 (5.8%) | |
| Religion | Orthodox | 331 (91.9%) | 621 (90.3%) |
| Muslim | 29 (8.1%) | 67 (9.7%) | |
| Educational status | Unable to read and write | 108 (30.0%) | 200 (29.1%) |
| Able to read and write | 40 (28.8%) | 99 (71.2%) | |
| Grade 1–8 | 81 (36.3%) | 142 (63.7%) | |
| Grade 9–12 | 88 (31.9%) | 188 (68.1%) | |
| Diploma and above | 43 (42.2%) | 59 (57.8%) | |
| Occupation | Housewife | 230 (63.9%) | 463 (67.3%) |
| Daily laborer | 22 (6.1%) | 47 (6.8%) | |
| Private | 68 (18.9%) | 93 (13.5%) | |
| Government employee | 40 (11.1%) | 85 (12.4%) | |
| Wealth Index | Very poor | 66 (18.3%) | 144 (20.9%) |
| Poor | 75 (20.8%) | 134 (19.5%) | |
| Middle | 72 (20%) | 137 (19.9%) | |
| Rich | 77 (21.4%) | 134 (19.5%) | |
| Very rich | 70 (19.4%) | 139 (19.9%) | |
| Variables | Control Group (N = 360) | Intervention Group (N = 688) | |
|---|---|---|---|
| Gravidity | 1 | 162 (45.0%) | 312 (45.3%) |
| 2–4 | 162 (45.0%) | 300 (43.6%) | |
| ≥5 | 36 (10%) | 76 (11.1%) | |
| Parity | 1 | 167 (46.4%) | 334 (48.5%) |
| ≥2 | 193 (53.6%) | 354 (51.5%) | |
| Number ANC follow-up | 1–3 | 122 (37.8%) | 263 (41.2%) |
| 4 | 201 (62.2%) | 375 (58.8%) | |
| BMI of mothers | <18.4 kg/m2 | 8 (2.2%) | 37 (5.4%) |
| 18.5–24.99 kg/m2 | 281 (78.1%) | 515 (74.9%) | |
| 25–29.99 kg/m2 | 63 (17.5%) | 116 (16.9%) | |
| >30 kg/m2 | 8 (2.2%) | 20 (2.9%) | |
| Intervention Group N = 378 (%) | Control Group N = 592 (%) | RR (95%, CI) | ||
|---|---|---|---|---|
| Perineal tear | Yes | 45 (11.9%) | 124 (20.9%) | 0.57 (0.41, 0.78) * |
| No | 333 (88.1%) | 468 (79.1%) | 1 | |
| APGAR score | <7 (Low APGAR score) | 60 (15.6%) | 168 (28.3%) | 0.61 (0.42, 0.89) * |
| 7 and above | 318 (84.4%) | 424 (71.7%) | 1 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Badi, M.B.; Abebe, S.M.; Weldetsadic, M.A.; Christensson, K.; Lindgren, H. Effect of Flexible Sacrum Position on Maternal and Neonatal Outcomes in Public Health Facilities, Amhara Regional State, Ethiopia: A Quasi-Experimental Study. Int. J. Environ. Res. Public Health 2022, 19, 9637. https://doi.org/10.3390/ijerph19159637
Badi MB, Abebe SM, Weldetsadic MA, Christensson K, Lindgren H. Effect of Flexible Sacrum Position on Maternal and Neonatal Outcomes in Public Health Facilities, Amhara Regional State, Ethiopia: A Quasi-Experimental Study. International Journal of Environmental Research and Public Health. 2022; 19(15):9637. https://doi.org/10.3390/ijerph19159637
Chicago/Turabian StyleBadi, Marta Berta, Solomon Mekonnen Abebe, Mulat Adefris Weldetsadic, Kyllike Christensson, and Helena Lindgren. 2022. "Effect of Flexible Sacrum Position on Maternal and Neonatal Outcomes in Public Health Facilities, Amhara Regional State, Ethiopia: A Quasi-Experimental Study" International Journal of Environmental Research and Public Health 19, no. 15: 9637. https://doi.org/10.3390/ijerph19159637
APA StyleBadi, M. B., Abebe, S. M., Weldetsadic, M. A., Christensson, K., & Lindgren, H. (2022). Effect of Flexible Sacrum Position on Maternal and Neonatal Outcomes in Public Health Facilities, Amhara Regional State, Ethiopia: A Quasi-Experimental Study. International Journal of Environmental Research and Public Health, 19(15), 9637. https://doi.org/10.3390/ijerph19159637






