The Main Changes in Pregnancy—Therapeutic Approach to Musculoskeletal Pain
Abstract
:1. Introduction
2. Physiological and Anatomical Changes of Pregnancy
2.1. The Main Changes That Occur at the Organ Level
2.2. Musculoskeletal Changes
2.2.1. Lower Back Pain
2.2.2. Pelvic Pain
2.2.3. Joint Pain
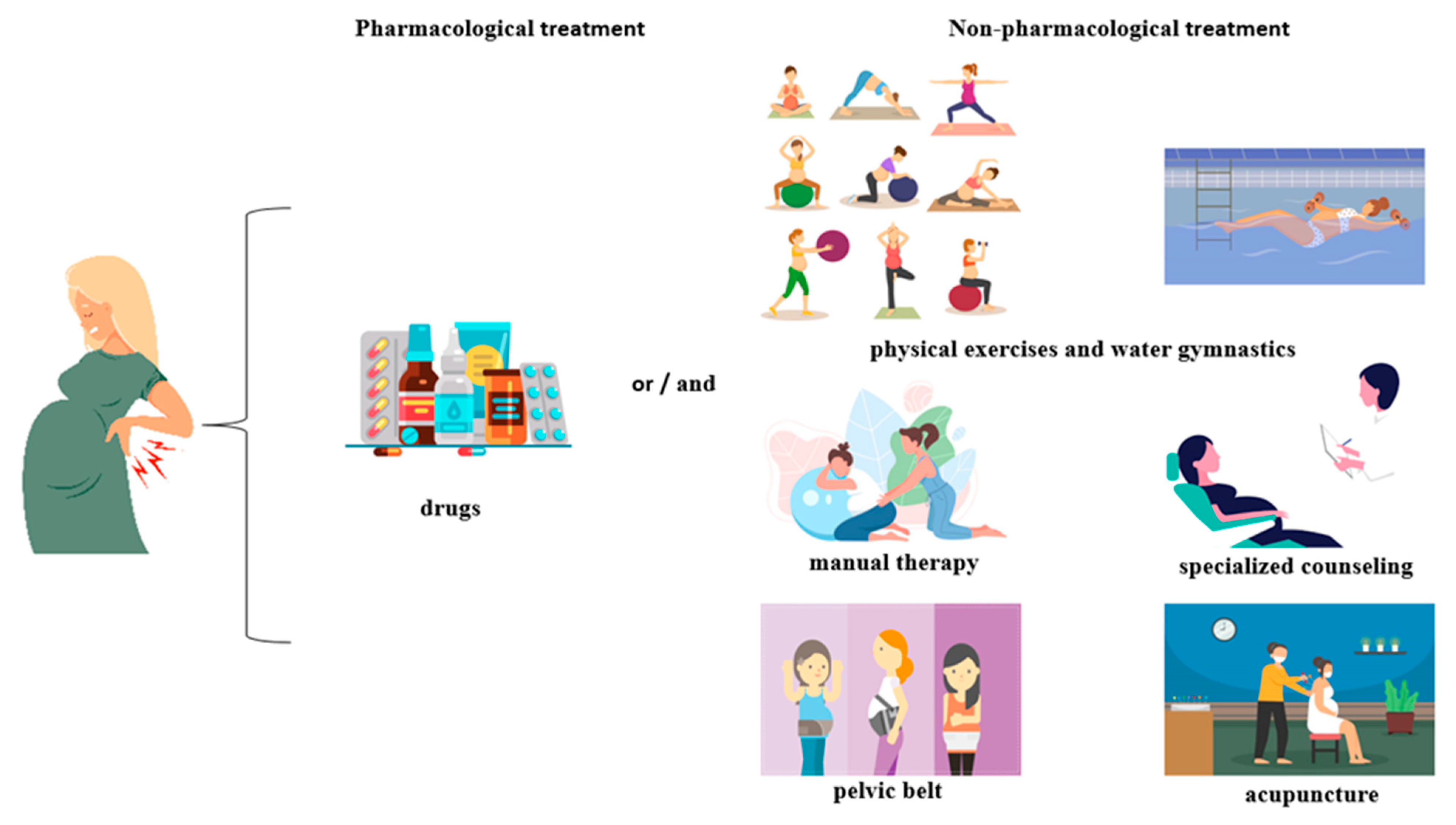
3. Treatment of Musculoskeletal Pain with Medication
3.1. Non-Opioid Medications
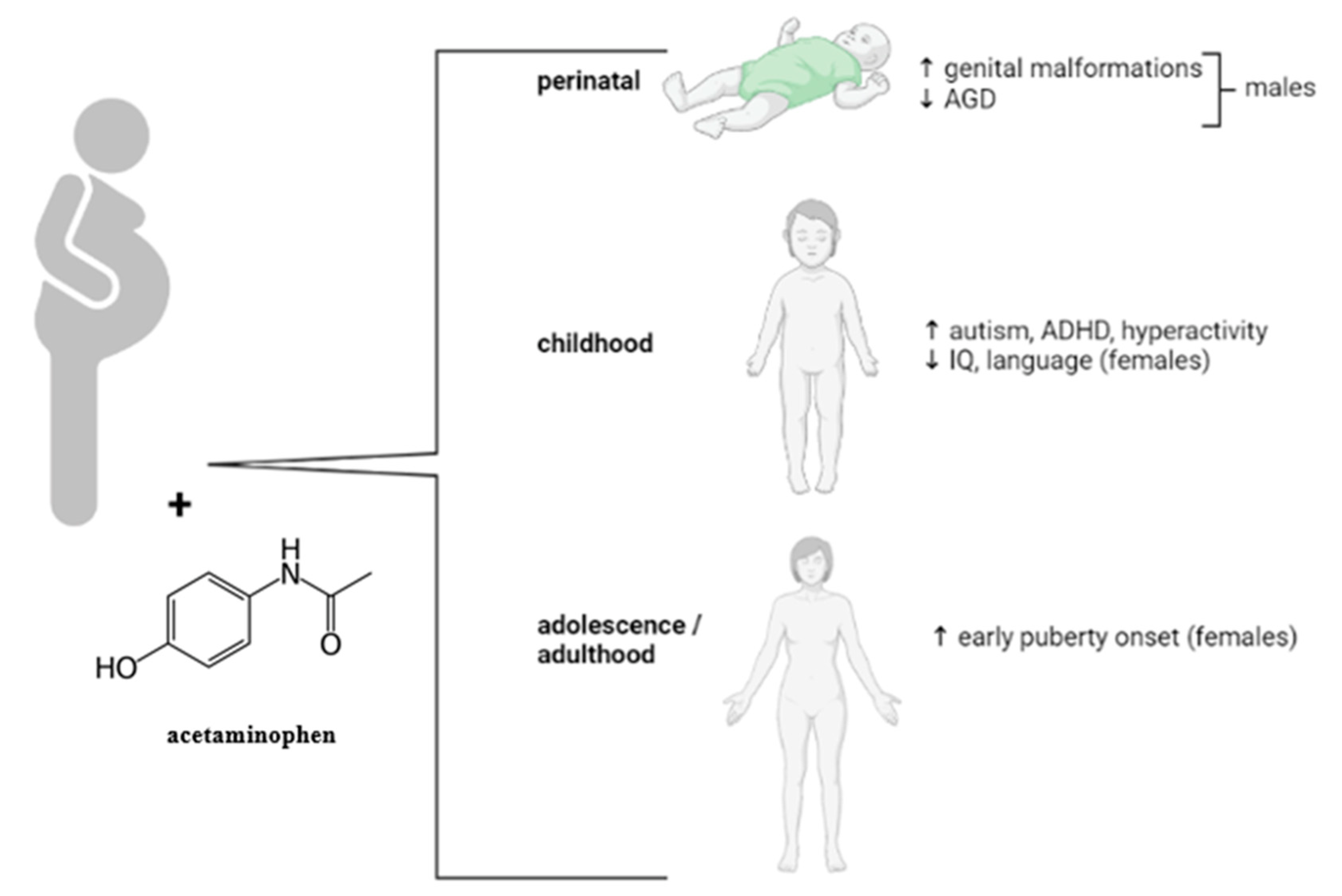
3.1.1. Paracetamol (Acetaminophen)
3.1.2. Non-Steroidal Anti-Inflammatory Agents
3.2. Opioid Medications
3.3. Transdermal Therapies
4. Treatment of Musculoskeletal Pain by Alternative and Complementary Methods
4.1. Physical Exercises and Water Gymnastics
4.2. Manual Therapy
4.3. Pelvic Belt
4.4. Acupuncture
4.5. Electrotherapy
4.6. The Benefits of Physiotherapy
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Pascual, Z.N.; Langaker, M.D. Physiology, pregnancy. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2022. [Google Scholar]
- Bhatia, P.; Chhabra, S. Physiological and anatomical changes of pregnancy: Implications for anaesthesia. Indian J. Anaesth. 2018, 62, 651–657. [Google Scholar] [CrossRef] [PubMed]
- Kesikburun, S.; Güzelküçük, Ü.; Fidan, U.; Demir, Y.; Ergün, A.; Tan, A.K. Musculoskeletal pain and symptoms in pregnancy: A descriptive study. Ther. Adv. Musculoskelet. Dis. 2018, 10, 229–234. [Google Scholar] [CrossRef] [PubMed]
- Williamson, C.S. Nutrition in pregnancy. Nutr. Bull. 2006, 31, 28–59. [Google Scholar] [CrossRef]
- Zaadstra, B.M.; Seidell, J.C.; Van Noord, P.A.; te Velde, E.R.; Habbema, J.D.; Vrieswijk, B.; Karbaat, J. Fat and female fecundity: Prospective study of effect of body fat distribution on conception rates. BMJ 1993, 306, 484–487. [Google Scholar] [CrossRef]
- Vanstone, M.; Kandasamy, S.; Giacomini, M.; DeJean, D.; McDonald, S.D. Pregnant women’s perceptions of gestational weight gain: A systematic review and meta-synthesis of qualitative research. Matern. Child Nutr. 2017, 13, e12374. [Google Scholar] [CrossRef]
- Bang, S.W.; Lee, S.S. The factors affecting pregnancy outcomes in the second trimester pregnant women. Nutr. Res. Pract. 2009, 3, 134–140. [Google Scholar] [CrossRef]
- Londero, A.P.; Rossetti, E.; Pittini, C.; Cagnacci, A.; Driul, L. Maternal age and the risk of adverse pregnancy outcomes: A retrospective cohort study. BMC Pregnancy Childbirth 2019, 19, 261. [Google Scholar] [CrossRef]
- Artal, R.; O’Toole, M. Guidelines of the American College of Obstetricians and Gynecologists for exercise during pregnancy and the postpartum period. Br. J. Sports Med. 2003, 37, 6–12. [Google Scholar] [CrossRef]
- Robson, S.C.; Hunter, S.; Boys, R.J.; Dunlop, W. Serial study of factors influencing changes in cardiac output during human pregnancy. Am. J. Physiol. 1989, 256, H1060–H1065. [Google Scholar] [CrossRef]
- Palmer, S.K.; Zamudio, S.; Coffin, C.; Parker, S.; Stamm, E.; Moore, L.G. Quantitative estimation of human uterine artery blood flow and pelvic blood flow redistribution in pregnancy. Obstet. Gynecol. 1992, 80, 1000–1006. [Google Scholar]
- Katz, M.; Sokal, M.M. Skin perfusion in pregnancy. Am. J. Obstet. Gynecol. 1980, 137, 30–33. [Google Scholar] [CrossRef]
- Cheung, K.L.; Lafayette, R.A. Renal physiology of pregnancy. Adv. Chronic Kidney Dis. 2013, 20, 209–214. [Google Scholar] [CrossRef]
- Kinsella, S.M.; Lohmann, G. Supine hypotensive syndrome. Obstet. Gynecol. 1994, 83, 774–788. [Google Scholar]
- Lanni, S.M.; Tillinghast, J.; Silver, H.M. Hemodynamic changes and baroreflex gain in the supine hypotensive syndrome. Am. J. Obstet. Gynecol. 2002, 187, 1636–1641. [Google Scholar] [CrossRef]
- Whitehead, E.M.; Smith, M.; Dean, Y.; O’Sullivan, G. An evaluation of gastric emptying times in pregnancy and the puerperium. Anaesthesia 1993, 48, 53–57. [Google Scholar] [CrossRef]
- Shah, S.; Nathan, L.; Singh, R.; Fu, Y.S.; Chaudhuri, G. E2 and not P4 increases NO release from NANC nerves of the gastrointestinal tract: Implications in pregnancy. Am. J. Physiol.-Regul. Integr. Comp. Physiol. 2001, 280, R1546–R1554. [Google Scholar] [CrossRef]
- Hu, H.; Pasca, I. Management of complex cardiac issues in the pregnant patient. Crit. Care Clin. 2016, 32, 97–107. [Google Scholar] [CrossRef]
- Gaiser, R. Physiologic changes of pregnancy. In Chestnut’s Obstetric Anesthesia: Principles and Practice, 5th ed.; Chestnut, D.H., Wng, C.A., Tsen, L.C., Ngan Kee, W.D., Beilin, Y., Mhyre, J.M., Eds.; Elsevier Saunders: Philadelphia, PA, USA, 2014; pp. 15–38. [Google Scholar]
- Soma-Pillay, P.; Nelson-Piercy, C.; Tolppanen, H.; Mebazaa, A. Physiological changes in pregnancy. Cardiovasc. J. Afr. 2016, 27, 89–94. [Google Scholar] [CrossRef]
- LoMauro, A.; Aliverti, A. Respiratory physiology of pregnancy: Physiology masterclass. Breathe 2015, 11, 297–301. [Google Scholar] [CrossRef]
- Stirrat, G.M. Pregnancy and immunity. BMJ 1994, 308, 1385–1386. [Google Scholar] [CrossRef]
- Burrows, R.F.; Kelton, J.G. Incidentally detected thrombocytopenia in healthy mothers and their infants. N. Engl. J. Med. 1988, 319, 142–145. [Google Scholar] [CrossRef] [PubMed]
- Thabah, M.; Ravindran, V. Musculoskeletal problems in pregnancy. Rheumatol. Int. 2015, 35, 581–587. [Google Scholar] [CrossRef] [PubMed]
- Smith, M.W.; Marcus, P.S.; Wurtz, L.D. Orthopedic issues in pregnancy. Obstet. Gynecol. Surv. 2008, 63, 103–111. [Google Scholar] [CrossRef] [PubMed]
- Borg-Stein, J.; Dugan, S.A. Musculoskeletal disorders of pregnancy, delivery and postpartum. Phys. Med. Rehabil. Clin. N. Am. 2007, 18, 459–476. [Google Scholar] [CrossRef]
- Sumilo, D.; Kurinczuk, J.J.; Redshaw, M.E.; Gray, R. Prevalence and impact of disability in women who had recently given birth in the UK. BMC Pregnancy Childbirth 2012, 12, 31. [Google Scholar] [CrossRef]
- Imaging Tests for Musculoskeletal Disorders and Muscle Damage. Available online: https://www.envrad.com/imaging-tests-musculoskeletal-disorders-muscle-damage/ (accessed on 26 July 2022).
- Test and Treatment Topics. Available online: https://www.radiologyinfo.org/en/test-treatment (accessed on 26 July 2022).
- Mack, K.A.; Jones, C.M.; Paulozzi, L.J. Vital signs: Overdoses of prescription opioid pain relievers and other drugs among women—United States, 1999–2010. Morb. Mortal. Wkly. Rep. 2013, 62, 537–542. [Google Scholar]
- Fast, A.; Shapiro, D.; Ducommun, E.J.; Friedmann, L.W.; Bouklas, T.; Floman, Y. Low-back pain in pregnancy. Spine 1987, 12, 368–371. [Google Scholar] [CrossRef]
- Wang, S.M.; Dezinno, P.; Maranets, I.; Berman, M.R.; Caldwell-Andrews, A.A.; Kain, Z.N. Low back pain during pregnancy: Prevalence, risk factors, and outcomes. Obstet. Gynecol. 2004, 104, 65–70. [Google Scholar] [CrossRef]
- Sabino, J.; Grauer, J.N. Pregnancy and low back pain. Curr. Rev. Musculoskelet. Med. 2008, 1, 137–141. [Google Scholar] [CrossRef]
- Katonis, P.; Kampouroglou, A.; Aggelopoulos, A.; Kakavelakis, K.; Lykoudis, S.; Makrigiannakis, A.; Alpantaki, K. Pregnancy-related low back pain. Hippokratia 2011, 15, 205–210. [Google Scholar]
- Germann, C.; Kroismayr, D.; Brunner, F.; Pfirrmann, C.W.A.; Sutter, R.; Zubler, V. Influence of pregnancy/childbirth on long-term bone marrow edema and subchondral sclerosis of sacroiliac joints. Skeletal. Radiol. 2021, 50, 1617–1628. [Google Scholar] [CrossRef]
- Šimac, D.V.; Vujaklija, D.V.; Mirić, F.; Novak, S. Transitory bone marrow oedema of the hip in pregnant patient with antiphospholipid syndrome: A case report. Egypt. Rheumatol. 2021, 43, 209–212. [Google Scholar] [CrossRef]
- Agten, C.A.; Zubler, V.; Zanetti, M.; Binkert, C.A.; Kolokythas, O.; Prentl, E.; Buck, F.M.; Pfirrmann, C.W.A. Postpartum bone marrow edema at the sacroiliac joints may mimic sacroiliitis of axial spondyloarthritis on MRI. Am. J. Roentgenol. 2018, 211, 1306–1312. [Google Scholar] [CrossRef]
- Wu, W.H.; Meijer, O.G.; Uegaki, K.; Mens, J.M.A.; van Dieen, J.H.; Wuisman, P.I.J.M.; Ostgaard, H.C. Pregnancy-related pelvic girdle pain (PPP), I: Terminology, clinical presentation, and prevalence. Eur. Spine J. 2004, 13, 575–589. [Google Scholar] [CrossRef]
- Keriakos, R.; Bhatta, S.R.; Morris, F.; Mason, S.; Buckley, S. Pelvic girdle pain during pregnancy and puerperium. J. Obstet. Gynaecol. 2011, 31, 572–780. [Google Scholar] [CrossRef]
- Vleeming, A.; Albert, H.B.; Östgaard, H.C.; Sturesson, B.; Stuge, B. European guidelines for the diagnosis and treatment of pelvic girdle pain. Eur. Spine J. 2008, 17, 794–819. [Google Scholar] [CrossRef]
- Walters, C.; West, S.; Nippita, T.A. Pelvic girdle pain in pregnancy. Aust. J. Gen. Pract. 2018, 47, 439–443. [Google Scholar] [CrossRef]
- Paslaru, F.G.; Giovani, A.; Iancu, G.; Panaitescu, A.; Peltecu, G.; Gorgan, R.M. Methods of delivery in pregnant women with lumbar disc herniation: A narrative review of general management and case report. J. Med. Life 2020, 13, 517–522. [Google Scholar] [CrossRef]
- Silman, A.; Kay, A.; Brennan, P. Timing of pregnancy in relation to the onset of rheumatoid arthritis. Arthritis Rheum. 1992, 35, 152–155. [Google Scholar] [CrossRef]
- Shah, S.; Banh, E.T.; Koury, K.; Bhatia, G.; Nandi, R.; Gulur, P. Pain management in pregnancy: Multimodal approaches. Pain Res. Treat. 2015, 2015, 987483. [Google Scholar] [CrossRef]
- Choi, H.J.; Lee, J.C.; Lee, Y.J.; Lee, E.B.; Shim, S.S.; Park, J.S.; Jun, J.K.; Song, Y.W. Prevalence and clinical features of arthralgia/arthritis in healthy pregnant women. Rheumatol. Int. 2008, 28, 1111–1115. [Google Scholar] [CrossRef]
- Descatha, A.; Dale, A.M.; Franzblau, A.; Coomes, J.; Evanoff, B. Comparison of research case definitions for carpal tunnel syndrome. Scand. J. Work Environ. Health 2011, 37, 298–306. [Google Scholar] [CrossRef]
- Mondelli, M.; Rossi, S.; Monti, E.; Aprile, I.; Caliandro, P.; Pazzaglia, C.; Romano, C.; Padua, L. Long term follow-up of carpal tunnel syndrome during pregnancy: A cohort study and review of the literature. Electromyogr. Clin. Neurophysiol. 2007, 47, 259–271. [Google Scholar]
- Zaghw, A.; Koronfel, M.; Podgorski, E.; Siddiqui, S.; Valliani, A.; Karmakar, A.; Khan, J. Pain management for pregnant women in the opioid crisis era. In Pain Management in Special Circumstances; Shallik, N.A., Ed.; IntechOpen: London, UK, 2018. [Google Scholar] [CrossRef]
- Roberto Díaz, R.; Lopera Rivera, A. Manejo del dolor no obstétrico durante el embarazo. Artículo de revisión. Rev. Colomb. Anestesiol. 2012, 40, 213–223. [Google Scholar] [CrossRef]
- Rathmell, J.P.; Viscomi, C.M.; Ashburn, M.A. Management of nonobstetric pain during pregnancy and lactation. Anesth. Analg. 1997, 85, 1074–1087. [Google Scholar] [CrossRef] [PubMed]
- Food and Drug Administration. Content and format of labeling for human prescription drug and biological products; requirements for pregnancy and lactation labeling. Final rule. Fed. Regist. 2014, 79, 72063–72103. [Google Scholar]
- Acetaminophen Information. Available online: https://www.fda.gov/drugs/information-drug-class/acetaminophen-information (accessed on 16 May 2022).
- Purdue Pharma, L.P. OxyContin. Prescribing Information. Available online: www.accessdata.fda.gov/drugsatfda_docs/label/2010/022272lbl.pdf (accessed on 16 May 2022).
- APP Pharmaceuticals, LLC. Xylocaine. Prescribing Information. Available online: www.accessdata.fda.gov/drugsatfda_docs/label/2010/006488s074lbl.pdf (accessed on 16 May 2022).
- Pfizer Laboratories Div Pfizer Inc. Dexamethasone Sodium Phosphate. Available online: http://www.drugs.com/pro/dexamethasone-sodium-phosphate.html (accessed on 16 May 2022).
- Roxane Laboratories, Inc. Codeine Sulfate. Prescribing Information. Available online: http://www.drugs.com/pro/codeine-sulfate.html (accessed on 16 May 2022).
- Abbott Laboratories. Vicodin. Prescribing Information. Available online: http://www.drugs.com/pro/vicodin.html# (accessed on 16 May 2022).
- TEVA Pharmaceuticals USA Inc. Diclofenac. Prescribing Information. Available online: http://www.drugs.com/pro/diclofenac.html (accessed on 16 May 2022).
- Polygen Pharmaceuticals LLC. Ibuprofen. Prescribing Information. Available online: http://www.drugs.com/pro/ibuprofen.html (accessed on 16 May 2022).
- Hospira, I. Naloxone. Prescribing Information. Available online: http://www.drugs.com/pro/naloxone.html (accessed on 16 May 2022).
- H.J. Harkins Company, Inc. Ketoprofen Prescribing Information. Available online: http://www.drugs.com/pro/ketoprofen.html (accessed on 16 May 2022).
- Pfizer. Celecoxib, Capsules. Medication Guide. Available online: www.fda.gov/downloads/Drugs/DevelopmentApprovalProcess/DevelopmentResources/UCM162532.pdf (accessed on 16 May 2022).
- Roxane Laboratories, Inc. Naproxen. Prescribing Information. Available online: http://www.drugs.com/pro/naproxen.html (accessed on 16 May 2022).
- Lachman Consultant Services, Inc. Tramadol. Attachment, C. Available online: www.fda.gov/ohrms/dockets/dailys/04/sep04/090804/04p-0405-cp00001-04-Attachment-C-vol1.pdf (accessed on 16 May 2022).
- Teva Pharmaceuticals USA, Inc. Piroxicam. Prescribing Information. Available online: http://www.drugs.com/pro/piroxicam.html (accessed on 16 May 2022).
- Himprit Pharmachem Pvt, Ltd. Aspirine. Prescribing Information. Available online: http://www.drugs.com/pro/aspirin.html (accessed on 16 May 2022).
- West-Ward Pharmaceutical Corp. Ergotamine and Caffeine. Prescribing Information. Available online: http://www.drugs.com/pro/ergotamine-and-caffeine.html (accessed on 16 May 2022).
- Bauer, A.Z.; Swan, S.H.; Kriebel, D.; Liew, Z.; Taylor, H.S.; Bornehag, C.G.; Andrade, A.M.; Olsen, J.; Jensen, R.H.; Mitchell, R.T.; et al. Paracetamol use during pregnancy—A call for precautionary action. Nat. Rev. Endocrinol. 2021, 17, 757–766. [Google Scholar] [CrossRef]
- Rebordosa, C.; Kogevinas, M.; Horváth-Puhó, E.; Nørgård, B.; Morales, M.; Czeizel, A.E.; Vilstrup, H.; Sørensen, H.T.; Olsen, J. Acetaminophen use during pregnancy: Effects on risk for congenital abnormalities. Am. J. Obstet. Gynecol. 2008, 198, 178.e1–178.e7. [Google Scholar] [CrossRef]
- Rebordosa, C.; Kogevinas, M.; Bech, B.H.; Sørensen, H.T.; Olsen, J. Use of acetaminophen during pregnancy and risk of adverse pregnancy outcomes. Int. J. Epidemiol. 2009, 38, 706–714. [Google Scholar] [CrossRef]
- Cooper, M.; Langley, K.; Thapar, A. Antenatal acetaminophen use and attention-deficit/hyperactivity disorder: An interesting observed association but too early to infer causality. JAMA Pediatr. 2014, 168, 306–307. [Google Scholar] [CrossRef]
- Kristensen, D.M.; Hass, U.; Lesné, L.; Lottrup, G.; Jacobsen, P.R.; Desdoits-Lethimonier, C.; Boberg, J.; Petersen, J.H.; Toppari, J.; Jensen, T.K.; et al. Intrauterine exposure to mild analgesics is a risk factor for development of male reproductive disorders in human and rat. Hum. Reprod. 2011, 26, 235–244. [Google Scholar] [CrossRef] [PubMed]
- Snijder, C.A.; Kortenkamp, A.; Steegers, E.A.; Jaddoe, V.W.; Hofman, A.; Hass, U.; Burdorf, A. Intrauterine exposure to mild analgesics during pregnancy and the occurrence of cryptorchidism and hypospadia in the offspring: The Generation R Study. Hum. Reprod. 2012, 27, 1191–1201. [Google Scholar] [CrossRef] [PubMed]
- Lind, D.V.; Main, K.M.; Kyhl, H.B.; Kristensen, D.M.; Toppari, J.; Andersen, H.R.; Andersen, M.S.; Skakkebæk, N.E.; Jensen, T.K. Maternal use of mild analgesics during pregnancy associated with reduced anogenital distance in sons: A cohort study of 1027 mother-child pairs. Hum. Reprod. 2017, 32, 223–231. [Google Scholar] [CrossRef] [PubMed]
- Fisher, B.G.; Thankamony, A.; Hughes, I.A.; Ong, K.K.; Dunger, D.B.; Acerini, C.L. Prenatal paracetamol exposure is associated with shorter anogenital distance in male infants. Hum. Reprod. 2016, 31, 2642–2650. [Google Scholar] [CrossRef]
- Ernst, A.; Brix, N.; Lauridsen, L.L.B.; Olsen, J.; Parner, E.T.; Liew, Z.; Olsen, L.H.; Ramlau-Hansen, C.H. Acetaminophen (paracetamol) exposure during pregnancy and pubertal development in boys and girls from a nationwide puberty cohort. Am. J. Epidemiol. 2019, 188, 34–46. [Google Scholar] [CrossRef]
- Feldkamp, M.L.; Meyer, R.E.; Krikov, S.; Botto, L.D. Acetaminophen use in pregnancy and risk of birth defects: Findings from the National Birth Defects Prevention Study. Obstet. Gynecol. 2010, 115, 109–115. [Google Scholar] [CrossRef]
- Lind, J.N.; Tinker, S.C.; Broussard, C.S.; Reefhuis, J.; Carmichael, S.L.; Honein, M.A.; Olney, R.S.; Parker, S.E.; Werler, M.M.; National Birth Defects Prevention Study. Maternal medication and herbal use and risk for hypospadias: Data from the National Birth Defects Prevention Study, 1997–2007. Pharmacoepidemiol. Drug Saf. 2013, 22, 783–793. [Google Scholar] [CrossRef]
- Interrante, J.D.; Ailes, E.C.; Lind, J.N.; Anderka, M.; Feldkamp, M.L.; Werler, M.M.; Taylor, L.G.; Trinidad, J.; Gilboa, S.M.; Broussard, C.S.; et al. Risk comparison for prenatal use of analgesics and selected birth defects, National Birth Defects Prevention Study 1997–2011. Ann. Epidemiol. 2017, 27, 645–653. [Google Scholar] [CrossRef]
- Avella-Garcia, C.B.; Julvez, J.; Fortuny, J.; Rebordosa, C.; García-Esteban, R.; Galán, I.R.; Tardón, A.; Rodríguez-Bernal, C.L.; Iñiguez, C.; Andiarena, A.; et al. Acetaminophen use in pregnancy and neurodevelopment: Attention function and autism spectrum symptoms. Int. J. Epidemiol. 2016, 45, 1987–1996. [Google Scholar] [CrossRef]
- Liew, Z.; Ritz, B.; Virk, J.; Olsen, J. Maternal use of acetaminophen during pregnancy and risk of autism spectrum disorders in childhood: A Danish national birth cohort study. Autism Res. 2016, 9, 951–958. [Google Scholar] [CrossRef]
- Ji, Y.; Azuine, R.E.; Zhang, Y.; Hou, W.; Hong, X.; Wang, G.; Riley, A.; Pearson, C.; Zuckerman, B.; Wang, X. Association of cord plasma biomarkers of in utero acetaminophen exposure with risk of attention-deficit/hyperactivity disorder and autism spectrum disorder in childhood. JAMA Psychiatry 2020, 77, 180–189. [Google Scholar] [CrossRef]
- Thompson, J.M.; Waldie, K.E.; Wall, C.R.; Murphy, R.; Mitchell, E.A.; ABC study group. Associations between acetaminophen use during pregnancy and ADHD symptoms measured at ages 7 and 11 years. PLoS ONE 2014, 9, e108210. [Google Scholar] [CrossRef]
- Leppert, B.; Havdahl, A.; Riglin, L.; Jones, H.J.; Zheng, J.; Smith, G.D.; Tilling, K.; Thapar, A.; Reichborn-Kjennerud, T.; Stergiakouli, E. Association of maternal neurodevelopmental risk alleles with early-life exposures. JAMA Psychiatry 2019, 76, 834–842. [Google Scholar] [CrossRef]
- Ystrom, E.; Gustavson, K.; Brandlistuen, R.E.; Knudsen, G.P.; Magnus, P.; Susser, E.; Davey Smith, G.; Stoltenberg, C.; Surén, P.; Håberg, S.E.; et al. Prenatal exposure to acetaminophen and risk of ADHD. Pediatrics 2017, 140, e20163840. [Google Scholar] [CrossRef]
- Ji, Y.; Riley, A.W.; Lee, L.C.; Hong, X.; Wang, G.; Tsai, H.J.; Mueller, N.T.; Pearson, C.; Thermitus, J.; Panjwani, A.; et al. Maternal biomarkers of acetaminophen use and offspring attention deficit hyperactivity disorder. Brain Sci. 2018, 8, 127. [Google Scholar] [CrossRef]
- Tovo-Rodrigues, L.; Schneider, B.C.; Martins-Silva, T.; Del-Ponte, B.; Loret de Mola, C.; Schuler-Faccini, L.; Vianna, F.S.L.; Munhoz, T.N.; Entiauspe, L.; Silveira, M.F.; et al. Is intrauterine exposure to acetaminophen associated with emotional and hyperactivity problems during childhood? Findings from the 2004 Pelotas birth cohort. BMC Psychiatry 2018, 18, 368. [Google Scholar] [CrossRef]
- Liew, Z.; Kioumourtzoglou, M.A.; Roberts, A.L.; O’Reilly, É.J.; Ascherio, A.; Weisskopf, M.G. Use of negative control exposure analysis to evaluate confounding: An example of acetaminophen exposure and attention-deficit/hyperactivity disorder in Nurses’ Health Study II. Am. J. Epidemiol. 2019, 188, 768–775. [Google Scholar] [CrossRef]
- Chen, M.-H.; Pan, T.-L.; Wang, P.-W.; Hsu, J.-W.; Huang, K.-L.; Su, T.-P.; Li, C.-T.; Lin, W.-C.; Tsai, S.-J.; Chen, T.-J.; et al. Prenatal exposure to acetaminophen and the risk of attention-deficit/hyperactivity disorder: A nationwide study in Taiwan. J. Clin. Psychiatry 2019, 80, 18m12612. [Google Scholar] [CrossRef]
- Baker, B.H.; Lugo-Candelas, C.; Wu, H.; Laue, H.E.; Boivin, A.; Gillet, V.; Aw, N.; Rahman, T.; Lepage, J.-F.; Whittingstall, K.; et al. Association of prenatal acetaminophen exposure measured in meconium with risk of attention-deficit/hyperactivity disorder mediated by frontoparietal network brain connectivity. JAMA Pediatr. 2020, 174, 1073–1081. [Google Scholar] [CrossRef]
- Ofori, B.; Oraichi, D.; Blais, L.; Rey, E.; Bérard, A. Risk of congenital anomalies in pregnant users of non-steroidal antiinflammatory drugs: A nested case-control study. Birth Defects Res. Part B Dev. Reprod. Toxicol. 2006, 77, 268–279. [Google Scholar] [CrossRef]
- Nielsen, G.L.; Sørensen, H.T.; Larsen, H.; Pedersen, L. Risk of adverse birth outcome and miscarriage in pregnant users of non-steroidal anti-inflammatory drugs: Population based observational study and case-control study. BMJ 2001, 322, 266–270. [Google Scholar] [CrossRef] [PubMed]
- Li, D.K.; Liu, L.; Odouli, R. Exposure to non-steroidal anti-inflammatory drugs during pregnancy and risk of miscarriage: Population based cohort study. BMJ 2003, 327, 368. [Google Scholar] [CrossRef] [PubMed]
- Hardy, J.B. The collaborative perinatal project: Lessons and legacy. Ann. Epidemiol. 2003, 13, 303–311. [Google Scholar] [CrossRef]
- Livshits, A.; Seidman, D.S. Role of non-steroidal anti-inflammatory drugs in gynecology. Pharmaceuticals 2010, 3, 2082–2089. [Google Scholar] [CrossRef]
- Le Duc, K.; Gilliot, S.; Baudelet, J.B.; Mur, S.; Boukhris, M.R.; Domanski, O.; Odou, P.; Storme, L. Case report: Persistent pulmonary hypertension of the newborn and narrowing of the ductus arteriosus after topical use of non-steroidal anti-inflammatory during pregnancy. Front. Pharmacol. 2021, 12, 756056. [Google Scholar] [CrossRef]
- Shintaku, K.; Hori, S.; Satoh, H.; Tsukimori, K.; Nakano, H.; Fujii, T.; Taketani, Y.; Ohtani, H.; Sawada, Y. Prediction and evaluation of fetal toxicity induced by NSAIDs using transplacental kinetic parameters obtained from human placental perfusion studies. Br. J. Clin. Pharmacol. 2012, 73, 248–256. [Google Scholar] [CrossRef]
- Arruza Gómez, L.; Corredera Sánchez, A.; Montalvo Montes, J.; de Marco Guilarte, E.; Moro Serrano, M. Cierre intrauterino del conducto arterial en probable relación con la ingesta materna de metamizol durante el tercer trimestre de gestación [Intrauterine closure of the ductus arteriosus probably associated with the taking of metamizole during the third trimester]. An. Pediatr. 2008, 68, 626–627. [Google Scholar] [CrossRef]
- da Silva Dal Pizzol, T.; Schüler-Faccini, L.; Mengue, S.S.; Fischer, M.I. Dipyrone use during pregnancy and adverse perinatal events. Arch. Gynecol. Obstet. 2009, 279, 293–297. [Google Scholar] [CrossRef]
- Bar-Oz, B.; Clementi, M.; Di Giantonio, E.; Greenberg, R.; Beer, M.; Merlob, P.; Arnon, J.; Ornoy, A.; Zimmerman, D.M.; Berkovitch, M. Metamizol (dipyrone, optalgin) in pregnancy, is it safe? A prospective comparative study. Eur. J. Obstet. Gynecol. Reprod. Biol. 2005, 119, 176–179. [Google Scholar] [CrossRef]
- Sharpe, C.R.; Franco, E.L.; Brazilian Wilms’ Tumor Study Group. Use of dipyrone during pregnancy and risk of Wilms’ tumor. Epidemiology 1996, 7, 533–535. [Google Scholar] [CrossRef]
- Ives, T.J.; Tepper, R.S. Drug use in pregnancy and lactation. Prim. Care 1990, 17, 623–645. [Google Scholar] [CrossRef]
- van Montfort, P.; Scheepers, H.C.J.; van Dooren, I.V.A.; Meertens, L.J.E.; Zelis, M.; Zwaan, I.M.; Spaanderman, M.E.A.; Smits, L.J.M. Low-dose-aspirin usage among women with an increased preeclampsia risk: A prospective cohort study. Acta Obstet. Gynecol. Scand. 2020, 99, 875–883. [Google Scholar] [CrossRef]
- American Society of Anesthesiologists Task Force on Chronic Pain Management; American Society of Regional Anesthesia and Pain Medicine. Practice guidelines for chronic pain management: An updated report by the American Society of Anesthesiologists Task Force on Chronic Pain Management and the American Society of Regional Anesthesia and Pain Medicine. Anesthesiology 2010, 112, 810–833. [Google Scholar] [CrossRef]
- Kakko, J.; Heilig, M.; Sarman, I. Buprenorphine and methadone treatment of opiate dependence during pregnancy: Comparison of fetal growth and neonatal outcomes in two consecutive case series. Drug Alcohol Depend. 2008, 96, 69–78. [Google Scholar] [CrossRef]
- Hagmeyer, K.O.; Mauro, L.S.; Mauro, V.F. Meperidine-related seizures associated with patient-controlled analgesia pumps. Ann. Pharmacother. 1993, 27, 29–32. [Google Scholar] [CrossRef]
- Cohen, R.S. Fentanyl transdermal analgesia during pregnancy and lactation. J. Hum. Lact. 2009, 25, 359–361. [Google Scholar] [CrossRef]
- Peck, J.; Urits, I.; Peoples, S.; Foster, L.; Malla, A.; Berger, A.A.; Cornett, E.M.; Kassem, H.; Herman, J.; Kaye, A.D.; et al. Comprehensive review of over the counter treatment for chronic low back pain. Pain Ther. 2021, 10, 69–80. [Google Scholar] [CrossRef]
- Lalkhen, A.; Grady, K. Non-obstetric pain in pregnancy. Rev. Pain 2008, 1, 10–14. [Google Scholar] [CrossRef]
- Geneen, L.J.; Moore, R.A.; Clarke, C.; Martin, D.; Colvin, L.A.; Smith, B.H. Physical activity and exercise for chronic pain in adults: An overview of Cochrane Reviews. Cochrane Database Syst. Rev. 2017, 4, CD011279. [Google Scholar] [CrossRef]
- Thompson, P.D.; Franklin, B.A.; Balady, G.J.; Blair, S.N.; Corrado, D.; Estes, N.M., III; Fulton, J.E.; Gordon, N.F.; Haskell, W.L.; Link, M.S. Exercise and acute cardiovascular events placing the risks into perspective: A scientific statement from the American Heart Association Council on Nutrition, Physical Activity, and Metabolism and the Council on Clinical Cardiology. Circulation 2007, 115, 2358–2368. [Google Scholar] [CrossRef]
- Mogren, I.M. Previous physical activity decreases the risk of low back pain and pelvic pain during pregnancy. Scand. J. Public Health 2005, 33, 300–306. [Google Scholar] [CrossRef]
- Kihlstrand, M.; Stenman, B.; Nilsson, S.; Axelsson, O. Water-gymnastics reduced the intensity of back/low back pain in pregnant women. Acta Obstet. Gynecol. Scand. 1999, 78, 180–185. [Google Scholar]
- Elden, H.; Ladfors, L.; Olsen, M.F.; Ostgaard, H.C.; Hagberg, H. Effects of acupuncture and stabilising exercises as adjunct to standard treatment in pregnant women with pelvic girdle pain: Randomised single blind controlled trial. BMJ 2005, 330, 761. [Google Scholar] [CrossRef]
- Wedenberg, K.; Moen, B.; Norling, A. A prospective randomized study comparing acupuncture with physiotherapy for low-back and pelvic pain in pregnancy. Acta Obstet. Gynecol. Scand. 2000, 79, 331–335. [Google Scholar]
- George, J.W.; Skaggs, C.D.; Thompson, P.A.; Nelson, D.M.; Gavard, J.A.; Gross, G.A. A randomized controlled trial comparing a multimodal intervention and standard obstetrics care for low back and pelvic pain in pregnancy. Am. J. Obstet. Gynecol. 2013, 208, 295. [Google Scholar] [CrossRef] [PubMed]
- Kordi, R.; Abolhasani, M.; Rostami, M.; Hantoushzadeh, S.; Mansournia, M.A.; Vasheghani-Farahani, F. Comparison between the effect of lumbopelvic belt and home based pelvic stabilizing exercise on pregnant women with pelvic girdle pain; a randomized controlled trial. J. Back Musculoskelet. Rehabil. 2013, 26, 133–139. [Google Scholar] [CrossRef] [PubMed]
- Nilsson-Wikmar, L.; Holm, K.; Oijerstedt, R.; Harms-Ringdahl, K. Effect of three different physical therapy treatments on pain and activity in pregnant women with pelvic girdle pain: A randomized clinical trial with 3, 6, and 12 months follow-up postpartum. Spine 2005, 30, 850–856. [Google Scholar] [CrossRef] [PubMed]
- Stafne, S.N.; Salvesen, K.A.; Romundstad, P.R.; Stuge, B.; Morkved, S. Does regular exercise during pregnancy influence lumbopelvic pain? A randomized controlled trial. Acta Obstet. Gynecol. Scand. 2012, 91, 552–559. [Google Scholar] [CrossRef] [PubMed]
- Kashanian, M.; Akbari, Z.; Alizadeh, M.H. The effect of exercise on back pain and lordosis in pregnant women. Int. J. Gynaecol. Obstet. 2009, 107, 160–161. [Google Scholar] [CrossRef]
- Eggen, M.H.; Stuge, B.; Mowinckel, P.; Jensen, K.S.; Hagen, K.B. Can supervised group exercises including ergonomic advice reduce the prevalence and severity of low back pain and pelvic girdle pain in pregnancy? A randomized controlled trial. Phys. Ther. 2012, 92, 781–790. [Google Scholar] [CrossRef]
- Kluge, J.; Hall, D.; Louw, Q.; Theron, G.; Grove, D. Specific exercises to treat pregnancy-related low back pain in a South African population. Int. J. Gynaecol. Obstet. 2011, 113, 187–191. [Google Scholar] [CrossRef]
- Gutke, A.; Sjodahl, J.; Oberg, B. Specific muscle stabilizing as home exercises for persistent pelvic girdle pain after pregnancy: A randomized, controlled clinical trial. J. Rehabil. Med. 2010, 42, 929–935. [Google Scholar] [CrossRef]
- Chaudry, S.; Rashid, F.; Shah, S.I.H. Effectiveness of core stabilization exercises along with postural correction in postpartum back pain. Rawal Med. J. 2013, 38, 256–259. [Google Scholar]
- Garshasbi, A.; Faghih Zadeh, S. The effect of exercise on the intensity of low back pain in pregnant women. Int. J. Gynaecol. Obstet. 2005, 88, 271–275. [Google Scholar] [CrossRef]
- Gutke, A.; Betten, C.; Degerskär, K.; Pousette, S.; Olsén, M.F. Treatments for pregnancy-related lumbopelvic pain: A systematic review of physiotherapy modalities. Acta Obstet. Gynecol. Scand. 2015, 94, 1156–1167. [Google Scholar] [CrossRef]
- Elden, H.; Ostgaard, H.C.; Fagevik-Olsen, M.; Ladfors, L.; Hagberg, H. Treatments of pelvic girdle pain in pregnant women: Adverse effects of standard treatment, acupuncture and stabilising exercises on the pregnancy, mother, delivery and the fetus/neonate. BMC Complement. Altern. Med. 2008, 8, 34. [Google Scholar] [CrossRef]
- Mens, J.M.; Snijders, C.J.; Stam, H.J. Diagonal trunk muscle exercises in peripartum pelvic pain: A randomized clinical trial. Phys. Ther. 2000, 80, 1164–1173. [Google Scholar] [CrossRef]
- Granath, A.B.; Hellgren, M.S.; Gunnarsson, R.K. Water aerobics reduces sick leave due to low back pain during pregnancy. J. Obstet. Gynecol. Neonatal Nurs. 2006, 35, 465–471. [Google Scholar] [CrossRef]
- Khorsan, R.; Hawk, C.; Lisi, A.J.; Kizhakkeveettil, A. Manipulative therapy for pregnancy and related conditions: A systematic review. Obs. Gynecol. Surv. 2009, 64, 416–427. [Google Scholar] [CrossRef]
- Stuber, K.J.; Wynd, S.; Weis, C.A. Adverse events from spinal manipulation in the pregnant and postpartum periods: A critical review of the literature. Chiropr. Man. Ther. 2012, 20, 8. [Google Scholar] [CrossRef]
- Aldabe, D.; Milosavljevic, S.; Bussey, M.D. Is pregnancy related pelvic girdle pain associated with altered kinematic, kinetic and motor control of the pelvis? A systematic review. Eur. Spine J. 2012, 21, 1777–1787. [Google Scholar] [CrossRef] [PubMed]
- Brosseau, L.; Wells, G.A.; Poitras, S.; Tugwell, P.; Casimiro, L.; Novikov, M.; Loew, L.; Sredic, D.; Clément, S.; Gravelle, A.; et al. Ottawa Panel evidence-based clinical practice guidelines on therapeutic massage for low back pain. J. Bodyw. Mov. 2012, 16, 424–455. [Google Scholar] [CrossRef] [PubMed]
- Elden, H.; Ostgaard, H.C.; Glantz, A.; Marciniak, P.; Linner, A.C.; Olsen, M.F. Effects of craniosacral therapy as adjunct to standard treatment for pelvic girdle pain in pregnant women: A multicenter, single blind, randomized controlled trial. Acta Obstet. Gynecol. Scand. 2013, 92, 775–782. [Google Scholar] [CrossRef]
- Licciardone, J.C.; Buchanan, S.; Hensel, K.L.; King, H.H.; Fulda, K.G.; Stoll, S.T. Osteopathic manipulative treatment of back pain and related symptoms during pregnancy: A randomized controlled trial. Am. J. Obstet. Gynecol. 2010, 202, 43. [Google Scholar] [CrossRef] [PubMed]
- American Osteopathic Association. Osteopathic Medicine and Your Health. Available online: http://www.osteopathic.org/osteopathic-health/treatment/Pages/default.aspx (accessed on 22 May 2022).
- Hensel, K.L.; Buchanan, S.; Brown, S.K.; Rodriguez, M.; Cruser, D.A. Pregnancy research on osteopathic manipulation optimizing treatment effects: The PROMOTE study. Am. J. Obstet. Gynecol. 2015, 212, 108. [Google Scholar] [CrossRef] [PubMed]
- Depledge, J.; McNair, P.J.; Keal-Smith, C.; Williams, M. Management of symphysis pubis dysfunction during pregnancy using exercise and pelvic support belts. Phys. Ther. 2005, 85, 1290–1300. [Google Scholar] [CrossRef]
- Kalus, S.M.; Kornman, L.H.; Quinlivan, J.A. Managing back pain in pregnancy using a support garment: A randomised trial. BJOG Int. J. Obstet. Gynaecol. 2007, 115, 68–75. [Google Scholar] [CrossRef]
- Kvorning, N.; Holmberg, C.; Grennert, L.; Aberg, A.; Akeson, J. Acupuncture relieves pelvic and low-back pain in late pregnancy. Acta Obstet. Gynecol. Scand. 2004, 83, 246–250. [Google Scholar] [CrossRef]
- Wang, S.M.; Dezinno, P.; Lin, E.C.; Lin, H.; Yue, J.J.; Berman, M.R.; Braveman, F.; Kain, Z.N. Auricular acupuncture as a treatment for pregnant women who have low back and posterior pelvic pain: A pilot study. Am. J. Obstet. Gynecol. 2009, 201, 271. [Google Scholar] [CrossRef]
- Elden, H.; Hagberg, H.; Olsen, M.F.; Ladfors, L.; Ostgaard, H.C. Regression of pelvic girdle pain after delivery: Follow-up of a randomised single blind controlled trial with different treatment modalities. Acta Obstet. Gynecol. Scand. 2008, 87, 201–208. [Google Scholar] [CrossRef]
- Ternov, N.K.; Grennert, L.; Aberg, A.; Algotsson, L.; Akeson, J. Acupuncture for lower back and pelvic pain in late pregnancy: A retrospective report on 167 consecutive cases. Pain Med. 2001, 2, 204–207. [Google Scholar] [CrossRef]
- Oxford Health NHS. TENS Machine in Pregnancy. Available online: https://www.oxfordhealth.nhs.uk/wp-content/uploads/2014/08/OP-100.15-TENS-machine-in-pregnancy.pdf (accessed on 17 June 2022).
- Behailu Kribet. Transcutaneous Electrical Nerve Stimulation during Pregnancy: The Electric Field in the Fetal Brain. Available online: https://bkibret.com/tens-during-pregnancy (accessed on 17 June 2022).
- Keskin, E.A.; Onur, O.; Keskin, H.L.; Gumus, I.I.; Kafali, H.; Turhan, N. Transcutaneous electrical nerve stimulation improves low back pain during pregnancy. Gynecol. Obstet. Investig. 2012, 74, 76–83. [Google Scholar] [CrossRef]
- Njogu, A.; Qin, S.; Chen, Y.; Hu, L.; Luo, Y. The effects of transcutaneous electrical nerve stimulation during the first stage of labor: A randomized controlled trial. BMC Pregnancy Childbirth 2021, 21, 164. [Google Scholar] [CrossRef]
- Nascimento, S.L.; Surita, F.G.; Cecatti, J.G. Physical exercise during pregnancy. Curr. Opin. Obstet. Gynecol. 2012, 24, 387–394. [Google Scholar] [CrossRef]
- Barakat, R.; Cordero, Y.; Coteron, J.; Luaces, M.; Montejo, R. Exercise during pregnancy improves maternal glucose screen at 24–28 weeks: A randomised controlled trial. Br. J. Sports Med. 2012, 46, 656–661. [Google Scholar] [CrossRef]
- de Barros, M.C.; Lopes, M.A.; Francisco, R.P.; Sapienza, A.D.; Zugaib, M. Resistance exercise and glycemic control in women with gestational diabetes mellitus. Am. J. Obstet. Gynecol. 2010, 203, 556. [Google Scholar] [CrossRef]
- Mason, L.; Roe, B.; Wong, H.; Davies, J.; Bamber, J. The role of antenatal pelvic floor muscle exercises in prevention of postpartum stress incontinence: A randomised controlled trial. J. Clin. Nurs. 2010, 19, 2777–2786. [Google Scholar] [CrossRef]
- Ko, P.C.; Liang, C.C.; Chang, S.D.; Lee, J.T.; Chao, A.S.; Cheng, P.J. A randomized controlled trial of antenatal pelvic floor exercises to prevent and treat urinary incontinence. Int. Urogynecol. J. 2011, 22, 17–22. [Google Scholar] [CrossRef]
- Robledo-Colonia, A.F.; Sandoval-Restrepo, N.; Mosquera-Valderrama, Y.F.; Escobar-Hurtado, C.; Ramírez-Vélez, R. Aerobic exercise training during pregnancy reduces depressive symptoms in nulliparous women: A randomised trial. J. Physiother. 2012, 58, 9–15. [Google Scholar] [CrossRef]
- Vallim, A.L.; Osis, M.J.; Cecatti, J.G.; Baciuk, É.P.; Silveira, C.; Cavalcante, S.R. Water exercises and quality of life during pregnancy. Reprod. Health 2011, 8, 14. [Google Scholar] [CrossRef]
- Barakat, R.; Pelaez, M.; Montejo, R.; Luaces, M.; Zakynthinaki, M. Exercise during pregnancy improves maternal health perception: A randomized controlled trial. Am. J. Obstet. Gynecol. 2011, 204, 402. [Google Scholar] [CrossRef] [PubMed]




| Classification | Definition | Examples | References |
|---|---|---|---|
| Category A | Controlled studies in pregnant women have not shown a risk to the fetus. | - | |
| Category B | Animal studies have not shown toxic effects on the fetus, but there are no controlled clinical trials in humans. Animal studies have shown toxic effects but have not been confirmed in studies in pregnant women. | Acetaminophen | [52,53,54,55] |
| Oxycodone | |||
| Lidocaine | |||
| Dexamethasone | |||
| Category C | Animal studies have shown teratogenic risk, but no controlled studies have been performed in pregnant women. | Piroxicam | [56,57,58,59,60,61,62,63,64,65] |
| Codeine | |||
| Hydrocodone | |||
| Diclofenac | |||
| Ibuprofen | |||
| Naloxone | |||
| Ketoprofen | |||
| Celecoxib | |||
| Naproxen | |||
| Tramadol | |||
| Category D | Positive evidence of fetal risk but their use is accepted, the benefit of the mother outweighs the risk of the fetus. | Acetyl salicylic acid | [66] |
| Category X | Studies in both animals and humans have shown fetal malformations or no evidence. The risks outweigh the benefits, they are contraindicated in pregnancy. | Ergot derivatives | [67] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fiat, F.; Merghes, P.E.; Scurtu, A.D.; Almajan Guta, B.; Dehelean, C.A.; Varan, N.; Bernad, E. The Main Changes in Pregnancy—Therapeutic Approach to Musculoskeletal Pain. Medicina 2022, 58, 1115. https://doi.org/10.3390/medicina58081115
Fiat F, Merghes PE, Scurtu AD, Almajan Guta B, Dehelean CA, Varan N, Bernad E. The Main Changes in Pregnancy—Therapeutic Approach to Musculoskeletal Pain. Medicina. 2022; 58(8):1115. https://doi.org/10.3390/medicina58081115
Chicago/Turabian StyleFiat, Felicia, Petru Eugen Merghes, Alexandra Denisa Scurtu, Bogdan Almajan Guta, Cristina Adriana Dehelean, Narcis Varan, and Elena Bernad. 2022. "The Main Changes in Pregnancy—Therapeutic Approach to Musculoskeletal Pain" Medicina 58, no. 8: 1115. https://doi.org/10.3390/medicina58081115
APA StyleFiat, F., Merghes, P. E., Scurtu, A. D., Almajan Guta, B., Dehelean, C. A., Varan, N., & Bernad, E. (2022). The Main Changes in Pregnancy—Therapeutic Approach to Musculoskeletal Pain. Medicina, 58(8), 1115. https://doi.org/10.3390/medicina58081115








