Abstract
Study Design: Retrospective review. Objective: Auricular hematomas are generally associated with sports-related injuries, with studies predominantly in white populations and high neighborhood socioeconomic status (NSES) compared to our county. A previous population-based study of trauma patients in our county, Shelby County, Tennessee, shows that those who live in high vs low NSES experienced socioeconomic variation in injury. We aim to determine if differences exist in clinical management and outcomes in this population. Methods: Patients from two hospital systems diagnosed with auricular hematomas from 2008–2023 were reviewed retrospectively. Inclusion criteria included adequate follow-up, clinical description of the hematoma, and comment on any complications or recurrence. Results: 48 patients, with a median age of 28 (range: 0–83), with the most common etiology being assault/non-accidental trauma (NAT) at 41.7%, equally distributed across all NSES (p = 0.30), with one sports-related injury. Facial trauma consults were associated with lower recurrence rates, 25% vs 62.5% (p = 0.003) and were less likely to be placed for self-pay patients (p = 0.019). Bolster placement resulted in lower recurrence rates, 23.3% compared to 58.3% (p = 0.030). Conclusions: Higher rates of assault/NAT etiologies existed in our population, independent of NSES. Our study reiterates the importance of facial trauma consultation and bolster usage to reduce recurrence.
Introduction
An auricular hematoma is a collection of blood underneath the perichondrium of the ear. Auricular hematomas are generally associated with sports-related injuries in high-risk contact sports, with a higher incidence in males [1,2,3,4]. There is also an association with impact trauma and assault. Notably, auricular hematomas in young children (<1 year), or bilateral auricular hematomas, without any explanation of trauma should raise concern for non-accidental trauma and trigger subsequent workup [5,6,7]. Less commonly, spontaneous hematomas can occur and primarily are described in case reports—due to its rarity there is a possibility of initial misdiagnosis due to a lack of an inciting event [8].
While generally an uncommon occurrence, the workup, management, and surveillance of this entity is important due to long-term cosmetic and occasionally functional concerns. Known complications without prompt management include infection, necrosis, and long-standing blood loss to the ear cartilage, which can result in cauliflower ear due to neocartilage formation with potential for hearing loss [9]. Recent publications show a wide range of recurrence rates from 5.6% up to 45.8%, showing lower recurrence rates with bolster placement and with management by a specialist such as an otolaryngologist [1,2,10,11,12].
Previous studies predominantly have been completed in white populations and high neighborhood socioeconomic status (NSES), or did not evaluate or report for NSES [1,2,10,12]. A previous population-based study of all trauma patients our own Shelby County, Tennessee shows that those who live in high NSES vs low NSES experienced socioeconomic variation in injury; penetrating injury rates were 20 times higher for persons living in the lowest NSES compared to those living in the highest NSES [13]. However, NSES had no association with in-hospital mortality [13].
Facial trauma injuries have higher incidence in lower socioeconomic groups. A previous study on mandibular fractures showed that up to 80% of their mandibular fracture patient population fell into the bottom five socioeconomic deciles [14].
The purpose of this study is to determine if differences exist in clinical management and outcomes in our distinct patient population in a retrospective cohort review over a 15-year experience.
Methods
Study Design and Data Source
We performed an Institutional Review Board approved (#22-08963-XP) retrospective chart review of patients from two hospitals systems: one system with six hospital locations including a level one trauma center and the other system with a single location functioning as a level one trauma center.
Study Population Selection
Each hospital database was queried for patients diagnosed inpatient and outpatient with auricular hematomas from January 1, 2008–January 1, 2023. Inclusion criteria included adequate follow-up, a clinical description of the hematoma, and comment on any complications or recurrence. Adequate follow-up includes evaluation and comment on the auricular hematoma seven or more days from initial presentation, based on recurrence timeframes given from prior studies [1,8]. One of the two institutions did not implement fully integrated electronic health record (EHR) until July 2019, disqualifying most patients in that hospital prior to that date from meeting inclusion criteria.
Given timeframe of our data analysis, we retrieved the following codes from both International Classification of Diseases, Ninth Revision (ICD-9) and International Classification of Diseases, 10th Revision (ICD-10): 380.31, H61.102, H61.121, H61.122, H61.191, H61.192, H61.193, H61.199, H61.891, H61.892, H61.893, H61.899, H61.90, H61.91, H61.92, H61.93, M95.10, M95.11, M95.12, S00.431A, S00.432A, S00.432D, and S00.439A.
Data on age, race, ethnicity, insurance type, zip code, admission date, encounter type, and diagnosis code were included.
Data Elements and Chart Review
The authors conducted a retrospective chart review. Data manually extracted during chart review included mechanism of injury, associated injuries, consult, consult to facial trauma team, prior aspiration or I&D attempt, I&D, bolster, bolster material, mattress suture, drainage location: bedside or operating room (OR), antibiotics given, other treatments, follow-up location, complications, recurrence, repeat drainage, cauliflower ear, infection, and other complications. Individuals with a previous history of cauliflower ear were excluded from the calculation of the incidence of cauliflower ear when there was no worsening of the deformity. Bolster, mattress suture, and drainage location information were only obtained if an aspiration or I&D event took place, and bolster material information was only collected for those with a bolster placed. Mechanisms of injury were grouped into the following categories: “Animal/ Bug Bite,” “Assault/NAT,” “Blow by object,” “Fall,” “MVC/Ped Struck,” “Piercing,” “Sport,” and “Unknown/ Spontaneous.” Patients were flagged as trauma patients for “Assault/NAT,” “Falls,” “MVC/Ped Struck,” and “Blow by Object.”
ZIP Code Tabulation Areas (ZCTAs) from the United States Census Bureau were used to identify the average household income and poverty percentage of the area, alongside income quintiles, based on the 2021 American Community 5-year survey [15]. High poverty area flags were assigned if >20% of the population lived in poverty. Low-NSES flags were assigned to areas with a median income in the bottom two income quintiles based on the most recently released 2021 income limits and mean income data (lowest quintile upper limit $28,007 and second quintile $28,008–55,000). Those meeting poverty threshold qualify for federal resources and by including both flags, we hope to also account for a high-risk population that falls into a low-income range without the same access to federal resources. ZCTAS were also used to flag areas with an uninsured rate higher than the 2021 national average uninsured rate as reported by the United States Census Bureau [16].
Outcomes
Primary outcome was recurrence rate at follow-up. Secondary outcomes included repeat drainage, cauliflower ear, infection, and cosmetic complications, which includes cauliflower ear, pressure necrosis, and hearing loss from meatal narrowing. Associations between social determinants of health and facial trauma consults were also tested.
Statistical Analysis
Statistical analysis was completed using SPSS (IBM, Armonk, NY). Pearson’s chi-squared test (or Fisher’s exact test if any expected count was <5) was used for testing association between two factors (p ≤.05). All odds ratios are reported as the point estimate and the 95% confidence interval.
Results
Demographics and Case Characteristics
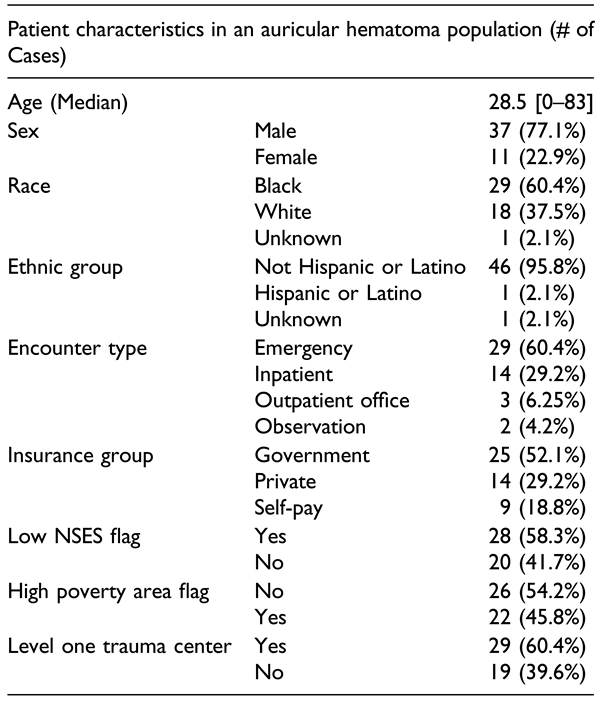
A total of 48 patients were included in our study with a median age of 28.5, ranging from 0–83 years of age (Table 1). Our patients primarily identified as male sex (77.1%) and black (60.4%). The majority of encounters took place in a hospital setting with 54.2% being emergency visits and 60.4% of the patients were seen at one of the two level one trauma centers included on our study.

Table 1.
Patient Demographics and Social Determinants of Health for 48 Auricular Hematoma Cases.
In terms of social determinants of health, the majority of our patients were government insured (52.1%) followed by private insurance (29.2%). The lowest percentage were self-pay patients (18.8%). When compared to the national average of insured patients, 85.4% of our patients lived in an area with a higher uninsured rate. 58.3% of patients lived in a low neighborhood socioeconomic status (NSES) area and 45.8% lived in a high poverty rate area.
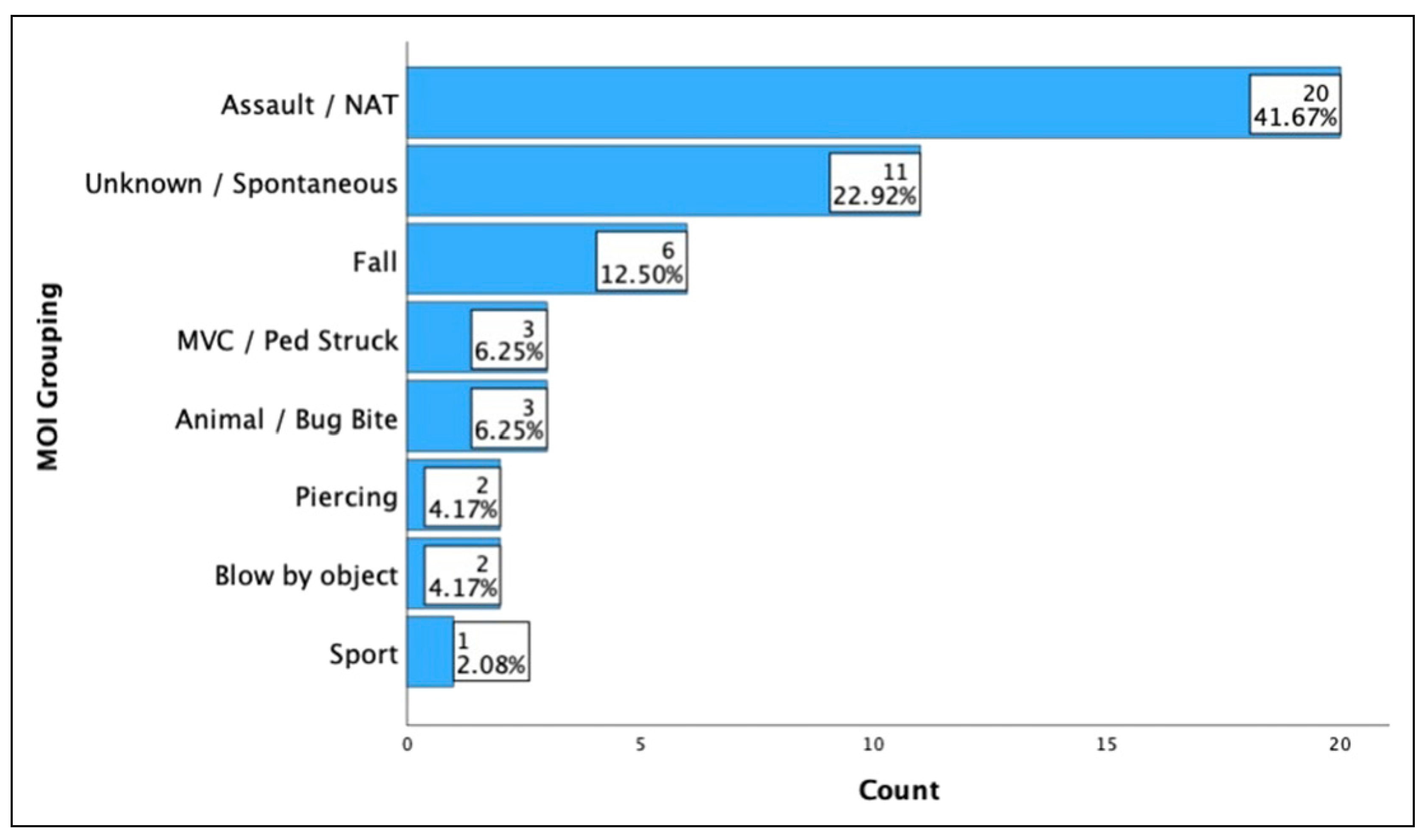
The most common etiology of injury was assault/nonaccidental trauma (NAT) at 41.7% and was equally distributed across all NSES (p = .30) (Figure 1). The second most common etiology was unknown/spontaneous (22.9%), followed by falls (12.5%), MVC/ped struck (6.25%), animal/bug bite (6.25%), piercing (4.2%), and blow by object (4.2%). There was only one sport related injury (2.1%). Only 46% of our patients had a reliable timeline from injury to accumulation given our large NAT and unknown/spontaneous populations, with the median timeframe being 0 days [range: 0–3] after initial injury. Overall, 62.5% of our patients were flagged as trauma patients.
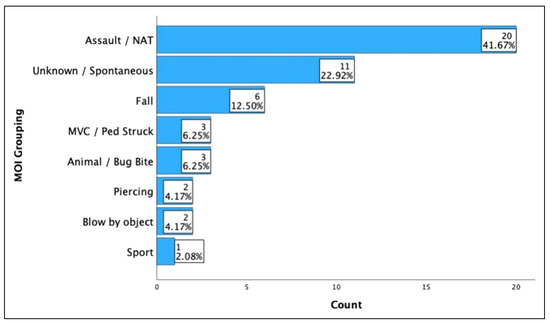
Figure 1.
Volume of auricular hematomas cases by mechanism of injury grouping.
Treatment and Outcome Data
Our patients had an overall recurrence rate of 37.5%. In total, 85.4% underwent an incision and drainage (I&D) procedure and of those with an I&D procedure, 80% were drained at bedside and 73.2% had bolsters placed.
In total, 62.5% of all patients received a bolster (70% with Xeroform, 20% with dental rolls, and 10% unspecified). Overall, 8.3% of all patients had mattress sutures placed. These therapies only took place when a facial trauma consult was ordered, with a bolster and/or mattress suture placement rate of 93.8% for patients with a consult.
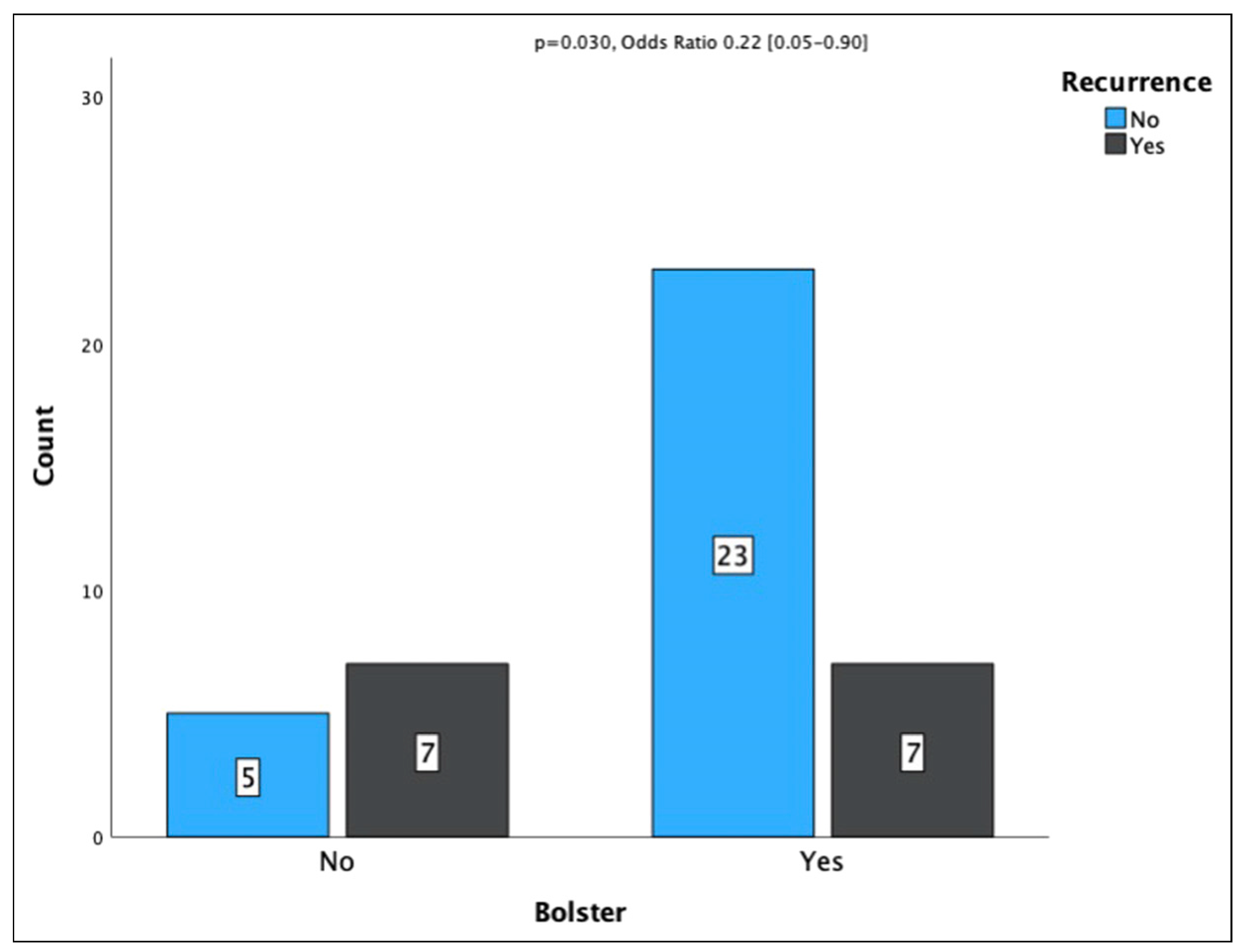
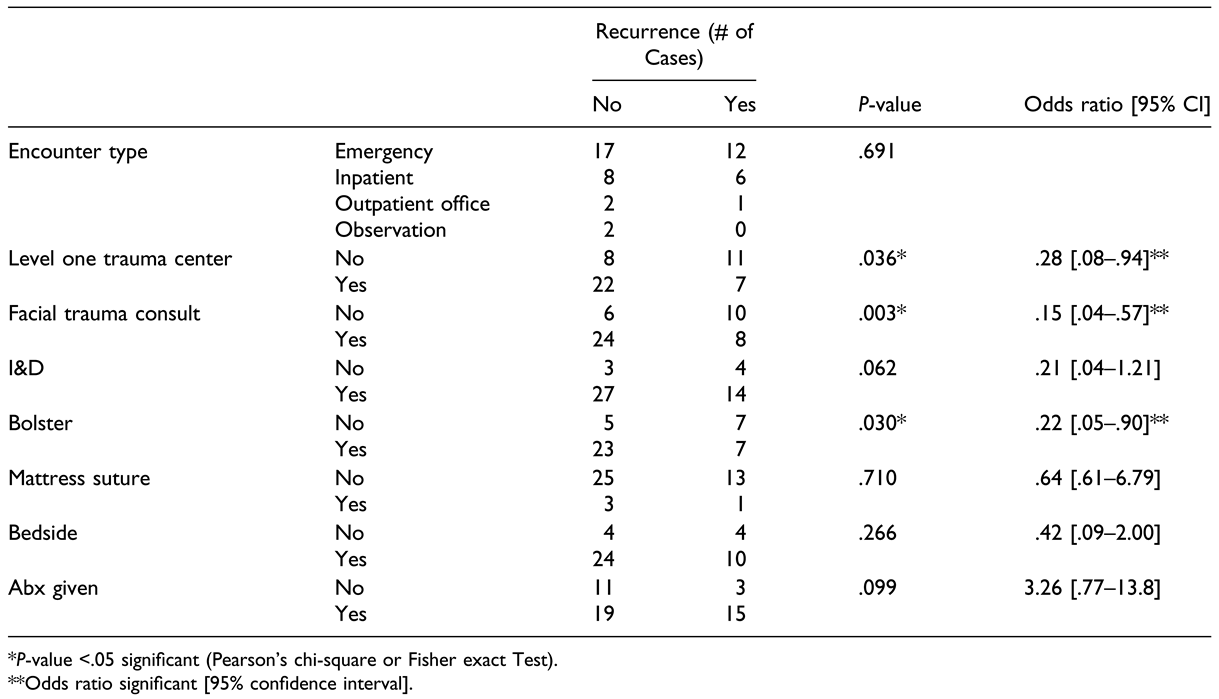
For those with interventions, median time to recurrence was 2 days [range: 0–6]. Three cases did not have a clearly documented timeframe to recurrence. Facial trauma consults resulted in lower rates of recurrence, 25.0% vs 62.5% (p = .003, OR .15 [.04-.57], Table 2). Bolster placement resulted in lower rates of recurrence, 23.3% compared to 58.3% (p = .030, OR .22 [.05-.90]), Figure 2). Individuals that were seen at one of the two level one trauma centers in the study had a lower rate of recurrence, 24.1% vs 57.9% (p = .036, OR .036 [.08-.94]). Patients that identified as black had a recurrence rate of 41.4% compared to 38.9% in patients that identified as white with no significant difference in recurrence rate (p = .866, OR .902 [.27–3.00]).

Table 2.
Chi-Squared Testing and Odds Ratios for Auricular Hematoma Recurrence Rate.
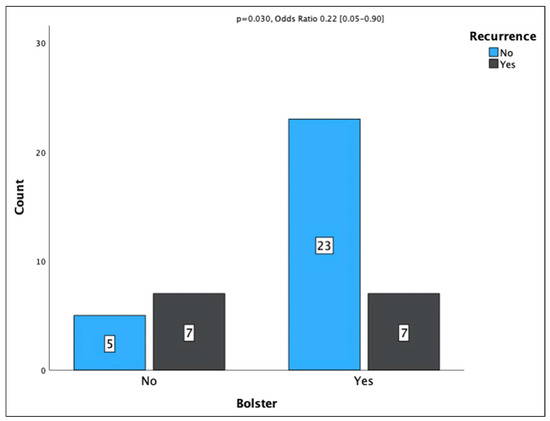
Figure 2.
Recurrence rate with bolster placement.
Encounter type, I&D, bolster type, horizontal mattress sutures, drainage location, or antibiotics did not have a statistically significant difference on recurrence rate (Table 2). There were no other significant results for recurrence.
In total, 19.1% of our patients had an infection and there were no statistically significant associations, including no association with antibiotics given (p = .173).
Overall, 34.0% of our patients required a repeat drainage of their hematoma. An association between repeat drainage and mechanism of injury (MOI) grouping was statistically significant (p = .045, Fisher Exact Test). All patients with a MOI of blow by object and piercing required repeat drainage. Repeat drainage for the other groups were as follows: assault/NAT (31.6%), MVC/Ped struck (33.3%), and unknown/spontaneous (45.5%). Fall, animal/bug bite, and sport etiologies did not require repeat drainage. There were no other statistically significant associations with repeat drainage.
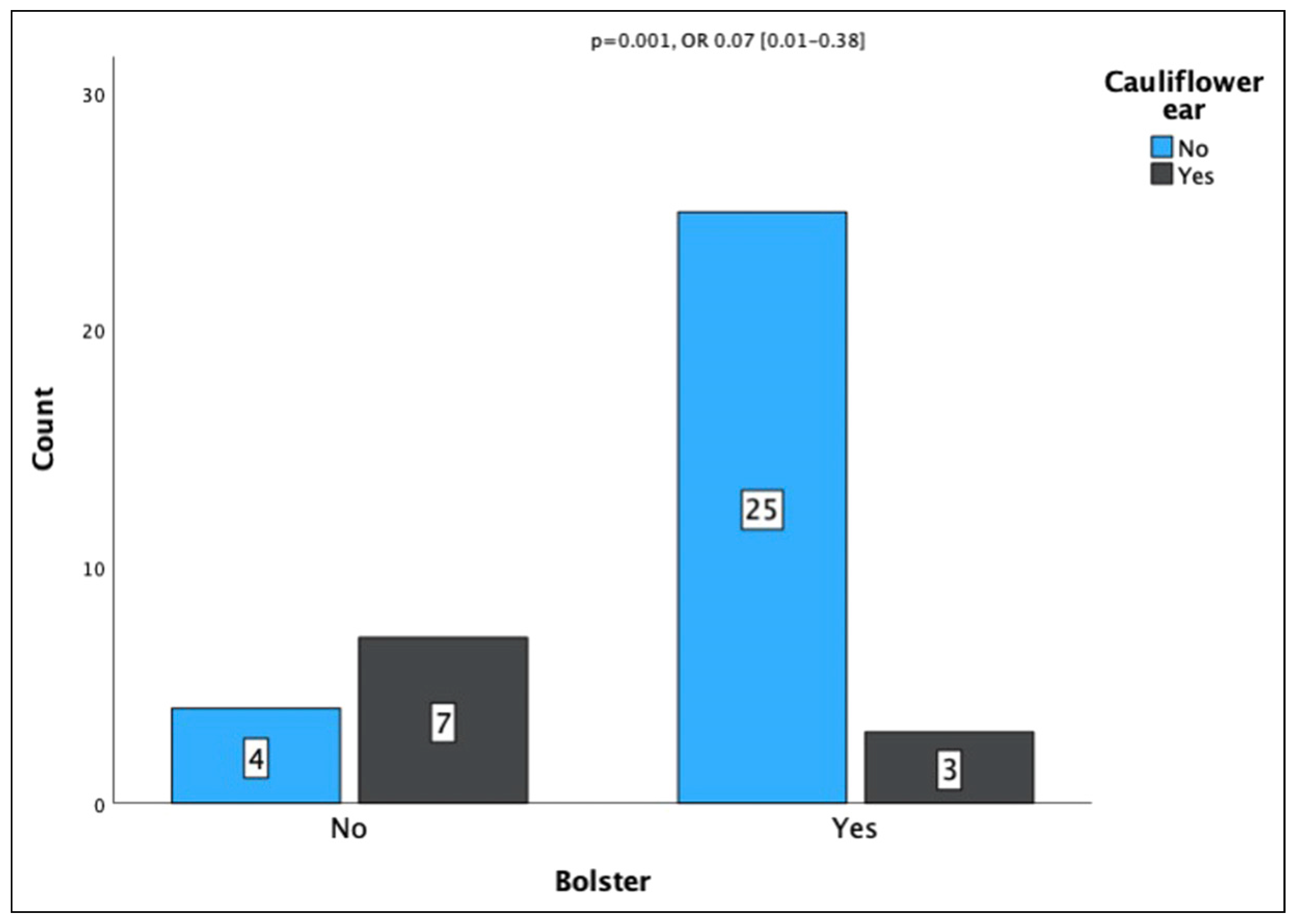
The overall incidence of cauliflower ear was 27.1%. One case was excluded due to a prior history of bilateral cauliflower ear with baseline description of the ear, and two of the cases were excluded due to lack of description of the shape of the auricle at the repeat visit. The incidence of cauliflower ears was reduced for patients at a level one trauma center, 7.1% vs 64.7% (p=<.001, OR .04 [.01–.24]), and for those with an associated injury, 13.6% vs 43.5% (p = .027 OR .21 [.05–.89]). Facial trauma consult was associated with a decreased incidence of cauliflower ear, 13.3% vs 60.0% (p = .001, OR .10 [.02–.45]). Bolster placement was associated with a reduced incidence of cauliflower ear, 10.7% vs 63.4% (p = .001, OR .07 [.01–.38], Figure 3). Material of bolster was not statistically significant (p = .052); however, use of Xeroform was associated with decreased odds of cauliflower ear (OR .18 [.07–.44]). There were no other factors associated with incidence of cauliflowers ears that were statistically significant. We did not have any instances of pressure necrosis; therefore, our cosmetic complication rate is the same population as cauliflower ears.
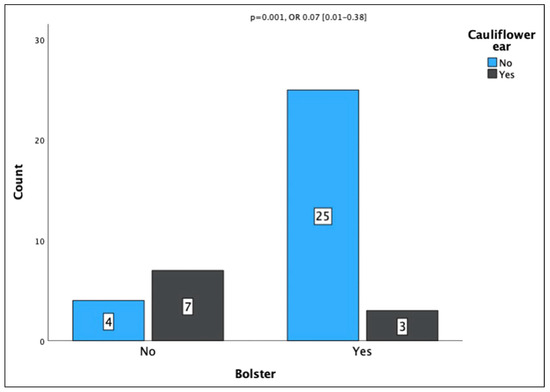
Figure 3.
Incidence of cauliflower ear with bolster placement.
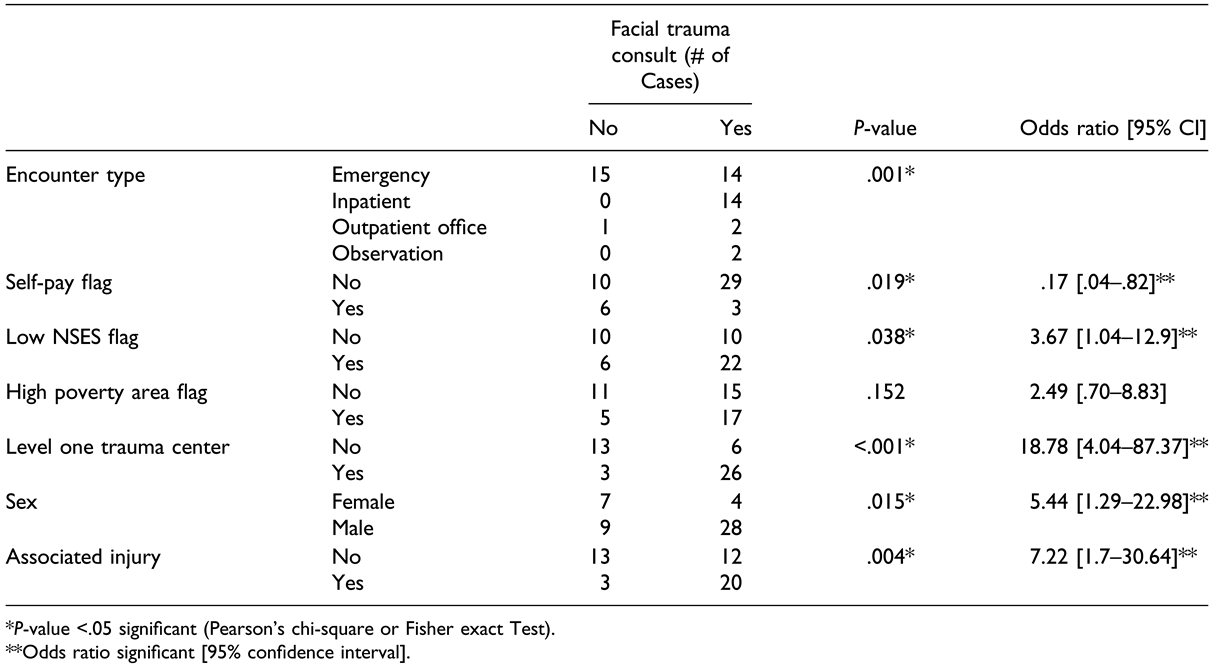
Facial trauma consults were placed for 66.7% of the patients and there were numerous variables associated with a consult being placed. As mentioned previously, facial trauma consults resulted in lower rates of recurrence, and were less likely to be placed for self-pay patients, where 33.3% of self-pay patients had a consulted compared to 74.4% of insured patients (p = .019, OR .17 [.04–.82], Table 3). In terms of follow-up location, 66.7% of the self-pay patients followed up in the emergency department. 65.8% of the insured patients followed up in an outpatient office setting.

Table 3.
Chi-Squared Testing and Odds Ratios for Consults to a Facial Trauma Specialist.
Females were less likely to have a facial trauma consult, 36.3% vs 75.7% (p = .015, OR 5.44 [1.29–22.98]). Individuals at a level one trauma center were more likely to receive a consult, 89.7% vs 31.5% (p=<.001, OR 18.78 [4.04–87.37]. Lastly, those with associated injuries were more likely to receive a facial trauma consult, 87.0% vs 48.0% (p = .004, OR 7.22 [1.70–30.64]). Notably, eleven patients had associated facial trauma injuries, with eight receiving facial trauma consults (72.7%). Of those eight consults, all consults explicitly requested management of the auricular hematomas.
Patients that lived in a low NSES area were more likely to have a facial trauma consult placed (p = .038, OR 3.67 [1.03–12.9], Table 3). There was no statistical significance regarding facial trauma consults being placed for race, ethnicity, or high poverty areas (Table 3).
Given the association between low NSES and facial trauma consultation, we conducted a subgroup analysis to test for similar associations with facial trauma consultation. In the low NSES subgroup, we again showed an association with level one trauma centers, 90% vs 50% (p = .038, OR 9.00 [1.20–67.42] and bolster placement, 100% vs 0% (p < .001). The association between sex (p = .091) and associated injury (p = .141) were no longer significant.
No other statistically significant outcomes associations were found with patients from low NSES areas. However, patients from a low NSES had improved non-statistically significant outcomes across the board, except for infection rates, where low NSES rate was 25.9% vs 10% (p = .17).
Discussion
Consistent with previous studies, our study further supports that there is a decreased recurrence rate and incidence of complications for patients managed by a facial trauma specialist and with bolster placement.
Our overall complication rate of 37.5% was comparable to other studies that looked at both specialist and non-specialist management and a mixed inpatient and outpatient setting, where those ranged from 23.7%–46% [1,10,12]. Another study had a recurrence rate of 18.0%, with management by otolaryngologist in an outpatient setting [11]. The study demonstrating the lowest recurrence rate of 5.6% was done in a young population of wrestlers, with strict inclusion criteria, managed by otolaryngologists in an outpatient setting with controlled follow-up, limiting external validity outside of this population [2].
We had a predominantly emergency and inpatient population with a wide range of presentation timelines and acuity levels of patients with associated injuries. Although we did not show a statistically significant result in encounter type, we only had three patients present to an outpatient clinic for their initial management and would need more volume to better test this association; however, a previous study has previously shown that admission to the hospital did not decrease recurrence rates [12]. Consistent with all data, there are likely confounding variables, that is, acuity of injury, timeline to presentation, patient access to care and compliance, etc., that are difficult to adjust for given low volumes and subjectivity; nevertheless, these could be beneficial in determining outcomes such as recurrence rate in an outpatient vs emergency presentations.
Compared to previous studies on auricular hematomas, our population had a higher rate of assault/non-accidental trauma (NAT), with only one sports related case of auricular hematomas. Unlike a previous study done in our trauma population and in the mandibular fracture population, there was no significant association between type of injury and socioeconomic status [13,14]. Similar to previous studies done in this trauma population, our patients had no statistically significant differences in primary outcomes [13]. The one difference was patients from a low NSES area were more likely to have a facial consult placed; however, self-pay patients were less likely to get a facial trauma consult. It is worth noting that patients from a low NSES had better outcomes across the board, except for infection rates. Given the high-volume of trauma patients seen in our area and the trauma pathways implemented in our institutions, this could serve as a safeguard for more vulnerable patient populations.
Placing facial trauma consultation and being a recipient of a bolster correlated with insurance status. Self-pay patients had statistically significant lower rate of facial trauma consults. The patient population in this study had a substantially higher uninsured rate than the general population, where our rate was 18.8% vs 8.6% nationally reported in 2021 [16]. We also had a larger prevalence of government insured patients than privately insured patients, where the private health insurance coverage at the national level was 66.0% compared to 29.2% in our subset of patients.
Care at a level one trauma center was consistently associated with improved outcomes, including lower rates of recurrence and cauliflower ears. There also was a higher rate of facial trauma consults being placed. Given the rarity of auricular hematomas, it is crucial for emergency and primary care providers to promptly recognizing not only the appearance of an auricular hematoma, but also the importance of consulting a specialist for proper management. With notably improvement in outcomes with a facial consult being placed, as well as the costs associated with following up in an emergency department vs outpatient office setting, facial trauma specialists should make a conscious effort to be available for patients, including sufficient follow-up [14,17].
Antibiotics usage was not associated with a decreased rate of infection, which is consistent with previous studies [1,12]. Guidelines note that antibiotic use is left to the discretion of the physician, with consideration of a splint in place due to risk of systemic infection and toxic shock [17]. Regarding drainage location, bedside vs operating room, there were no statistically significant differences in any of the outcome metrics, which is consistent with a previous study done in the United States [1].
Our study had several notable limitations. This was a retrospective review which limits available data to prior documentation and coding within the electronic health record (EHR). We performed several broad ICD code searches and two-person manual extraction to maximize the accuracy of patients included and excluded in this study. One hospital system’s EHR was only available from 2019– 2023 which limited the number of patients included in the study. Therefore, this study had a significant number of patients at one of the two hospital systems excluded due to the lack of records. For the hospital system with six locations, only four out of six hospitals have otolaryngology/ facial trauma coverage, which could have biased the patients receiving a facial trauma consult. This could have contributed to the better outcomes associated with presentation to the level one trauma centers as these both have facial trauma coverage. Trauma patients are frequently transferred for facial trauma evaluation in our system and encounters were captured in our database at the final hospital location with facial trauma services. This would reduce the rate of consultation rates at outside hospital; furthermore, we reiterate that this increases external validity. As with most trauma populations, our study was limited by low rates of patient follow-up. This places some limitations on the power of our study, as it would most publications of this nature. Low volumes place further restrictions on the types of statistically analyses available for subgroups in our population, such as those with associated injuries. Even in patients who completed acute follow-up, a majority of patients did not continue with long-term follow-up to further assess outcome.
Conclusions
Higher rates of assault/NAT etiologies existed in our population, independent of neighborhood socioeconomic status. Our study reiterates the importance of facial trauma consultation and bolster usage to reduce recurrence and cauliflower ear.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Acknowledgments
Thank you to those involved with the data extraction process: Shannon Williams and Dusty Griffith at Regional One Hospital and Manasa Mallampaty at Methodist Healthcare. The authors included each contributed substantially to this research as per the guidelines of the International Committee of Medical Journal Editors (ICMJE).
Conflicts of Interest
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Dalal, P.J.; Purkey, M.R.; Price, C.P.E.; Sidle, D.M. Risk factors for auricular hematoma and recurrence after drainage. Laryngoscope 2020, 130, 628–631. [Google Scholar] [CrossRef] [PubMed]
- Brickman, K.; Adams, D.Z.; Akpunonu, P.; Adams, S.S.; Zohn, S.F.; Guinness, M. Acute management of auricular hematoma: a novel approach and retrospective review. Clin J Sport Med. 2013, 23, 321–323. [Google Scholar] [CrossRef]
- Greywoode, J.D.; Pribitkin, E.A.; Krein, H. Management of auricular hematoma and the cauliflower ear. Facial Plast Surg. 2010, 26, 451–455. [Google Scholar]
- Kakarala, K.; Kieff, D.A. Bolsterless management for recurrent auricular hematomata. Laryngoscope 2012, 122, 1235–1237. [Google Scholar] [CrossRef]
- Manning, S.C.; Casselbrant, M.; Lammers, D. Otolaryngologic manifestations of child abuse. Int J Pediatr Otorhinolaryngol. 1990, 20, 7–16. [Google Scholar] [CrossRef] [PubMed]
- Steele, B.D.; Brennan, P.O. A prospective survey of patients with presumed accidental ear injury presenting to a paediatric accident and emergency department. Emerg Med J. 2002, 19, 226–228. [Google Scholar] [CrossRef] [PubMed]
- Mathur, S.; Clarke, R.; John, C.M. Spontaneous’ auricular haematoma: a rare differential diagnosis of NAI. Acta Paediatr. 2009, 98, 928. [Google Scholar] [CrossRef] [PubMed]
- Mohseni, M.; Szymanski, T. Acute non-traumatic spontaneous auricular hematoma. Am J Case Rep. 2019, 20, 204–206. [Google Scholar] [CrossRef] [PubMed]
- Muller, R.V. Facial Trauma: Soft Tissue Injuries. Plastic Surgery, Volume 3: Craniofacial, Head and Neck Surgery and Pediatric Plastic Surgery; Elsevier: Amsterdam, The Netherlands, 2018. [Google Scholar]
- Choung, Y.H.; Park, K.; Choung, P.H.; Oh, J.H. Simple compressive method for treatment of auricular haematoma using dental silicone material. J Laryngol Otol. 2005, 119, 27–31. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Giles, W.C.; Iverson, K.C.; King, J.D.; Hill, F.C.; Woody, E.A.; Bouknight, A.L. Incision and drainage followed by mattress suture repair of auricular hematoma. Laryngoscope. 2007, 117, 2097–2099. [Google Scholar] [CrossRef] [PubMed]
- Vijendren, A.; Coates, M.; Smith, ME; et al. Management of pinna haematoma study (MaPHaeS): A multicentre retrospective observational study. Clin Otolaryngol. 2017, 42, 1252–1258. [Google Scholar] [CrossRef] [PubMed]
- Zarzaur, B.L.; Croce, M.A.; Fabian, T.C.; Fischer, P.; Magnotti, L.J. A population-based analysis of neighborhood socioeconomic status and injury admission rates and in-hospital mortality. J Am Coll Surg. 2010, 211, 216–223. [Google Scholar] [CrossRef] [PubMed]
- Goodfellow, M.; Burns, A. Relation between facial fractures and socioeconomic deprivation in the north east of England. Br J Oral Maxillofac Surg. 2019, 57, 255–259. [Google Scholar] [CrossRef] [PubMed]
- U.S. Census Bureau. Historical Income Tables: Household; U.S. Department of Commerce: Washington, DC, USA. Available online: https:// data.census.gov/.
- U.S. Census Bureau. Health insurance coverage in the United States. 2021. Available online: https://data.census.gov/.
- Krogmann, R.J.; Jamal, Z.; King, K.C. Auricular Hematoma. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2023. [Google Scholar]
© 2024 by the author. The Author(s) 2024.