Effects of Different Calcium Silicate Cements on the Inflammatory Response and Odontogenic Differentiation of Lipopolysaccharide-Stimulated Human Dental Pulp Stem Cells
Abstract
:1. Introduction
2. Materials and Methods
2.1. Preparation of Material Extracts
2.2. Cell Isolation and Culture
2.3. LPS Stimulation
2.4. Cell Viability Test
2.5. Enzyme-Linked Immunosorbent Assay
2.6. Quantitative Real-Time Polymerase Chain Reaction (qPCR)
2.7. Alizarin Red S (ARS) Staining
2.8. Inductively Coupled Plasma Mass Spectrometry (ICP-MS)
2.9. Statistical Analysis
3. Results
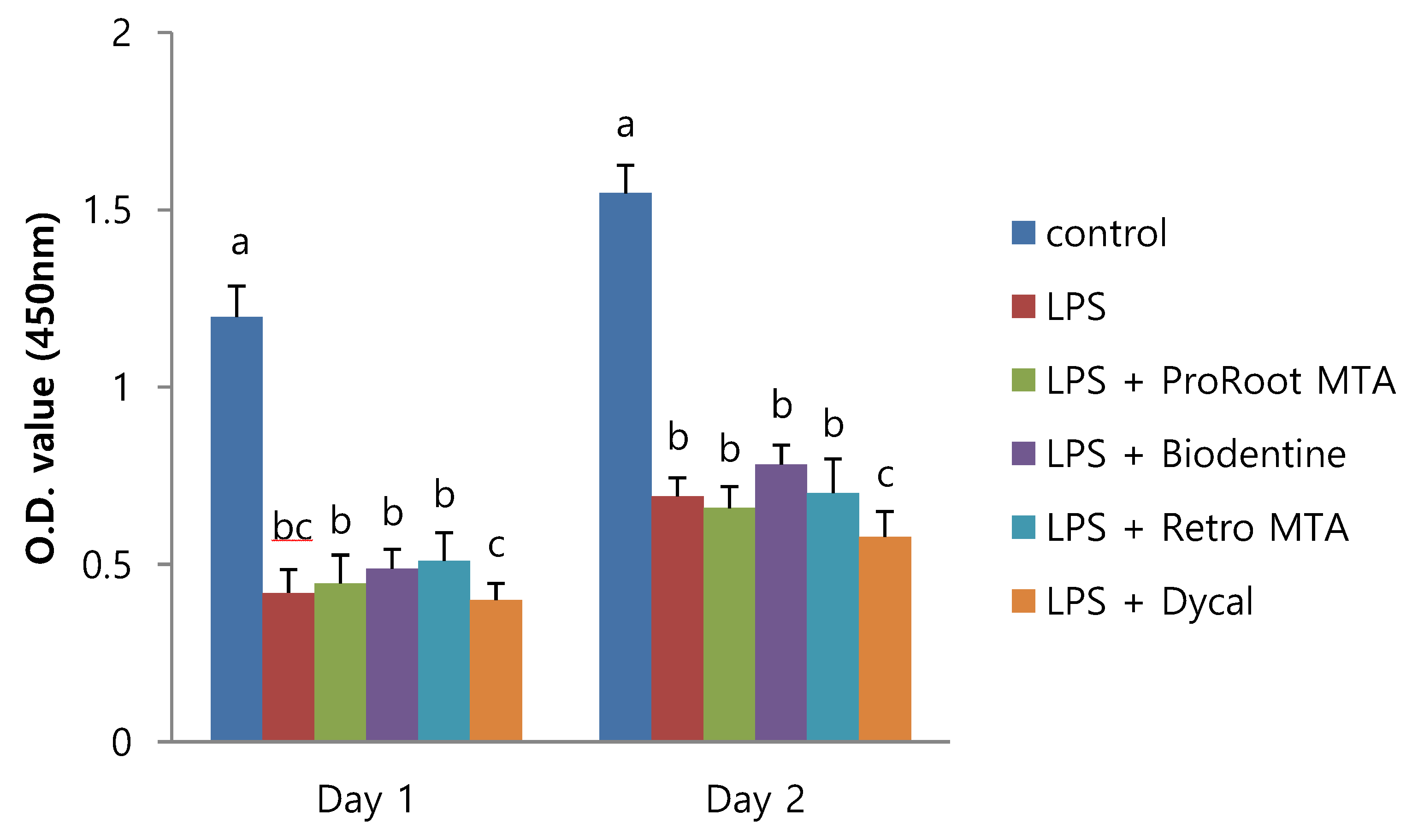
3.1. Effect of Different CSCs on Cell Viability of LDPSCs
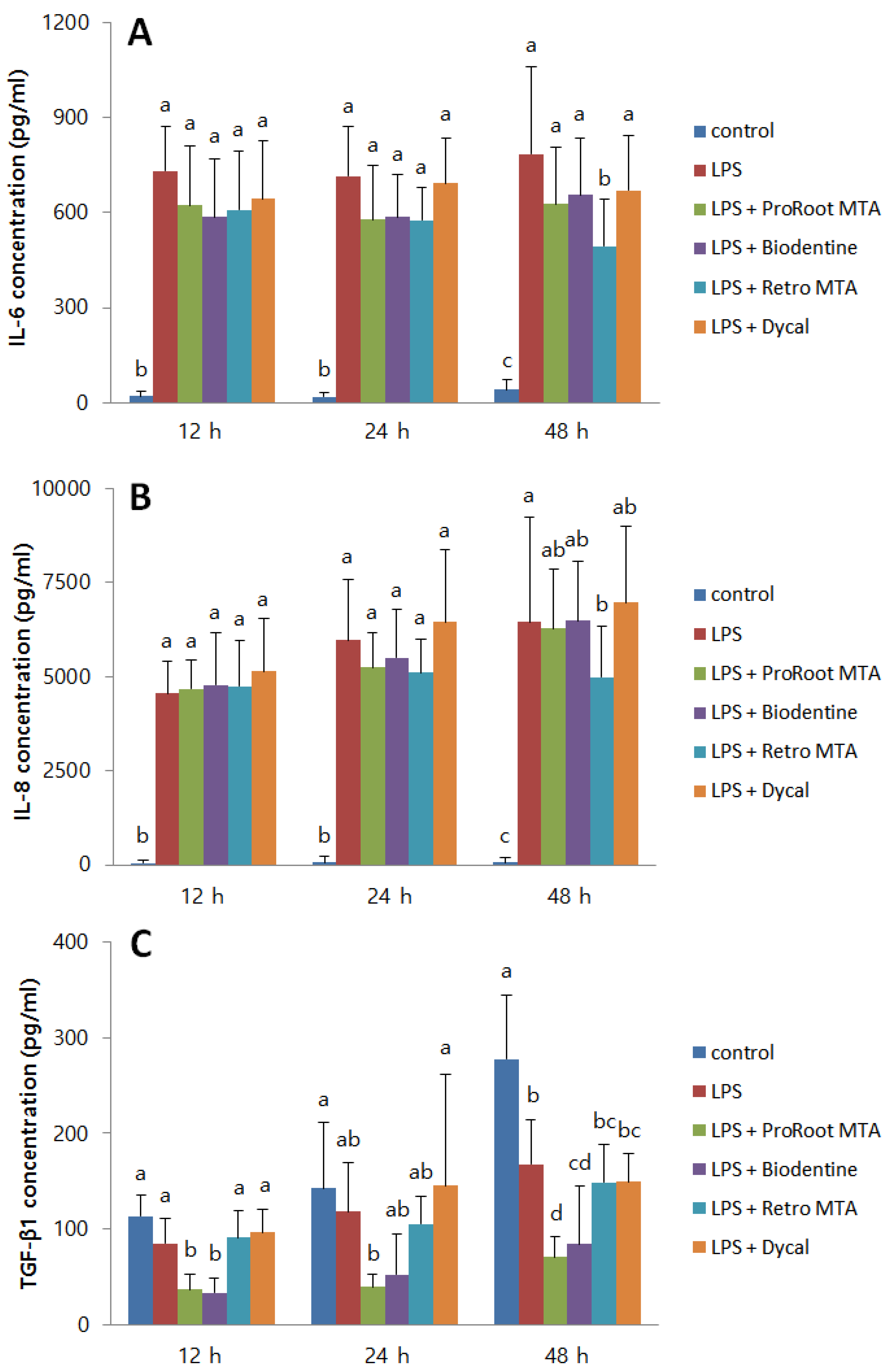
3.2. Effect of Different CSCs on the Inflammatory Responses of LDPSCs
3.3. Effect of Different CSCs on the Odontogenic Differentiation of LDPSCs
3.4. Si and Ca Ion Concentrations from Material Extract Medium
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Parirokh, M.; Torabinejad, M.; Dummer, P.M.H. Mineral trioxide aggregate and other bioactive endodontic cements: An updated overview—Part I: Vital pulp therapy. Int. Endod. J. 2018, 51, 177–205. [Google Scholar] [CrossRef]
- Torabinejad, M.; Parirokh, M. Mineral trioxide aggregate: A comprehensive literature review—Part II: Leakage and biocompatibility investigations. J. Endod. 2010, 36, 190–202. [Google Scholar] [CrossRef]
- Parirokh, M.; Torabinejad, M. Mineral trioxide aggregate: A comprehensive literature review—Part III: Clinical applications, drawbacks, and mechanism of action. J. Endod. 2010, 36, 400–413. [Google Scholar] [CrossRef]
- Sequeira, D.B.; Seabra, C.M.; Palma, P.J.; Cardoso, A.L.; Peca, J.; Santos, J.M. Effects of a New Bioceramic Material on Human Apical Papilla Cells. J. Funct. Biomater. 2018, 9, 74. [Google Scholar] [CrossRef]
- Awawdeh, L.; Al-Qudah, A.; Hamouri, H.; Chakra, R.J. Outcomes of Vital Pulp Therapy Using Mineral Trioxide Aggregate or Biodentine: A Prospective Randomized Clinical Trial. J. Endod. 2018, 44, 1603–1609. [Google Scholar] [CrossRef]
- Cho, S.Y.; Seo, D.G.; Lee, S.J.; Lee, J.; Lee, S.J.; Jung, I.Y. Prognostic factors for clinical outcomes according to time after direct pulp capping. J. Endod. 2013, 39, 327–331. [Google Scholar] [CrossRef]
- Li, Z.; Cao, L.; Fan, M.; Xu, Q. Direct Pulp Capping with Calcium Hydroxide or Mineral Trioxide Aggregate: A Meta-analysis. J. Endod. 2015, 41, 1412–1417. [Google Scholar] [CrossRef]
- Min, K.S.; Park, H.J.; Lee, S.K.; Park, S.H.; Hong, C.U.; Kim, H.W.; Lee, H.H.; Kim, E.C. Effect of mineral trioxide aggregate on dentin bridge formation and expression of dentin sialoprotein and heme oxygenase-1 in human dental pulp. J. Endod. 2008, 34, 666–670. [Google Scholar] [CrossRef]
- Baume, L.J. Diagnosis of diseases of the pulp. Oral Surg. Oral Med. Oral Pathol. 1970, 29, 102–116. [Google Scholar] [CrossRef]
- Garfunkel, A.; Sela, J.; Ulmansky, M. Dental pulp pathosis. Clinicopathologic correlations based on 109 cases. Oral Surg. Oral Med. Oral Pathol. 1973, 35, 110–117. [Google Scholar] [CrossRef]
- Seltzer, S.; Bender, I.B.; Ziontz, M. The dynamics of pulp inflammation: Correlations between diagnostic data and actual histologic findings in the pulp. Oral Surg. Oral Med. Oral Pathol. 1963, 16, 846–871. [Google Scholar] [CrossRef]
- Ricucci, D.; Loghin, S.; Siqueira, J.F., Jr. Correlation between clinical and histologic pulp diagnoses. J. Endod. 2014, 40, 1932–1939. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.; Lee, S.; Jung, H.S.; Kim, S.Y.; Shin, S.J.; Kang, M.K.; Kim, E. Evaluation of the Biodistribution of Human Dental Pulp Stem Cells Transplanted into Mice. J. Endod. 2018, 44, 592–598. [Google Scholar] [CrossRef] [PubMed]
- Aguilar, P.; Linsuwanont, P. Vital pulp therapy in vital permanent teeth with cariously exposed pulp: A systematic review. J. Endod. 2011, 37, 581–587. [Google Scholar] [CrossRef]
- Brizuela, C.; Ormeno, A.; Cabrera, C.; Cabezas, R.; Silva, C.I.; Ramirez, V.; Mercade, M. Direct Pulp Capping with Calcium Hydroxide, Mineral Trioxide Aggregate, and Biodentine in Permanent Young Teeth with Caries: A Randomized Clinical Trial. J. Endod. 2017, 43, 1776–1780. [Google Scholar] [CrossRef]
- Mente, J.; Geletneky, B.; Ohle, M.; Koch, M.J.; Friedrich Ding, P.G.; Wolff, D.; Dreyhaupt, J.; Martin, N.; Staehle, H.J.; Pfefferle, T. Mineral trioxide aggregate or calcium hydroxide direct pulp capping: An analysis of the clinical treatment outcome. J. Endod. 2010, 36, 806–813. [Google Scholar] [CrossRef]
- Chang, S.W.; Bae, W.J.; Yi, J.K.; Lee, S.; Lee, D.W.; Kum, K.Y.; Kim, E.C. Odontoblastic Differentiation, Inflammatory Response, and Angiogenic Potential of 4 Calcium Silicate-based Cements: Micromega MTA, ProRoot MTA, RetroMTA, and Experimental Calcium Silicate Cement. J. Endod. 2015, 41, 1524–1529. [Google Scholar] [CrossRef] [PubMed]
- Kang, C.M.; Hwang, J.; Song, J.S.; Lee, J.H.; Choi, H.J.; Shin, Y. Effects of Three Calcium Silicate Cements on Inflammatory Response and Mineralization-Inducing Potentials in a Dog Pulpotomy Model. Materials 2018, 11, 899. [Google Scholar] [CrossRef]
- Asgary, S.; Eghbal, M.J.; Ghoddusi, J.; Yazdani, S. One-year results of vital pulp therapy in permanent molars with irreversible pulpitis: An ongoing multicenter, randomized, non-inferiority clinical trial. Clin. Oral Investig. 2013, 17, 431–439. [Google Scholar] [CrossRef]
- Taha, N.A.; Khazali, M.A. Partial Pulpotomy in Mature Permanent Teeth with Clinical Signs Indicative of Irreversible Pulpitis: A Randomized Clinical Trial. J. Endod. 2017, 43, 1417–1421. [Google Scholar] [CrossRef]
- Nagaoka, S.; Tokuda, M.; Sakuta, T.; Taketoshi, Y.; Tamura, M.; Takada, H.; Kawagoe, M. Interleukin-8 gene expression by human dental pulp fibroblast in cultures stimulated with Prevotella intermedia lipopolysaccharide. J. Endod. 1996, 22, 9–12. [Google Scholar] [CrossRef]
- Tokuda, M.; Sakuta, T.; Fushuku, A.; Torii, M.; Nagaoka, S. Regulation of interleukin-6 expression in human dental pulp cell cultures stimulated with Prevotella intermedia lipopolysaccharide. J. Endod. 2001, 27, 273–277. [Google Scholar] [CrossRef]
- Widbiller, M.; Eidt, A.; Wolflick, M.; Lindner, S.R.; Schweikl, H.; Hiller, K.A.; Buchalla, W.; Galler, K.M. Interactive effects of LPS and dentine matrix proteins on human dental pulp stem cells. Int. Endod. J. 2018, 51, 877–888. [Google Scholar] [CrossRef]
- Horst, O.V.; Tompkins, K.A.; Coats, S.R.; Braham, P.H.; Darveau, R.P.; Dale, B.A. TGF-β1 Inhibits TLR-mediated odontoblast responses to oral bacteria. J. Dent. Res. 2009, 88, 333–338. [Google Scholar] [CrossRef] [PubMed]
- Piattelli, A.; Rubini, C.; Fioroni, M.; Tripodi, D.; Strocchi, R. Transforming growth factor-beta 1 (TGF-beta 1) expression in normal healthy pulps and in those with irreversible pulpitis. Int. Endod. J. 2004, 37, 114–119. [Google Scholar] [CrossRef] [PubMed]
- Kim, D.H.; Jang, J.H.; Lee, B.N.; Chang, H.S.; Hwang, I.N.; Oh, W.M.; Kim, S.H.; Min, K.S.; Koh, J.T.; Hwang, Y.C. Anti-inflammatory and mineralization effects of proroot MTA and endocem MTA in studies of human and rat dental pulps in vitro and in vivo. J. Endod. 2018, 44, 1534–1541. [Google Scholar] [CrossRef] [PubMed]
- Lai, W.Y.; Kao, C.T.; Hung, C.J.; Huang, T.H.; Shie, M.Y. An evaluation of the inflammatory response of lipopolysaccharide-treated primary dental pulp cells with regard to calcium silicate-based cements. Int. J. Oral Sci. 2014, 6, 94–98. [Google Scholar] [CrossRef] [Green Version]
- Shie, M.Y.; Chang, H.C.; Ding, S.J. Effects of altering the Si/Ca molar ratio of a calcium silicate cement on in vitro cell attachment. Int. Endod. J. 2012, 45, 337–345. [Google Scholar] [CrossRef] [PubMed]
- Barry, M.A.; Eastman, A. Endonuclease activation during apoptosis: The role of cytosolic Ca2+ and pH. Biochem. Biophys. Res. Commun. 1992, 186, 782–789. [Google Scholar] [CrossRef]
- Shie, M.Y.; Ding, S.J.; Chang, H.C. The role of silicon in osteoblast-like cell proliferation and apoptosis. Acta Biomater. 2011, 7, 2604–2614. [Google Scholar] [CrossRef]
- Chen, M.; Hu, D.N.; Pan, Z.; Lu, C.W.; Xue, C.Y.; Aass, I. Curcumin protects against hyperosmoticity-induced IL-1beta elevation in human corneal epithelial cell via MAPK pathways. Exp. Eye Res. 2010, 90, 437–443. [Google Scholar] [CrossRef]
- Lee, M.; Kang, C.M.; Song, J.S.; Shin, Y.; Kim, S.; Kim, S.O.; Choi, H.J. Biological efficacy of two mineral trioxide aggregate (MTA)-based materials in a canine model of pulpotomy. Dent. Mater. J. 2017, 36, 41–47. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- An, S.; Gao, Y.; Ling, J.; Wei, X.; Xiao, Y. Calcium ions promote osteogenic differentiation and mineralization of human dental pulp cells: Implications for pulp capping materials. J. Mater. Sci. Mater. Med. 2012, 23, 789–795. [Google Scholar] [CrossRef] [PubMed]
- An, S.; Gao, Y.; Huang, Y.; Jiang, X.; Ma, K.; Ling, J. Short-term effects of calcium ions on the apoptosis and onset of mineralization of human dental pulp cells in vitro and in vivo. Int. J. Mol. Med. 2015, 36, 215–221. [Google Scholar] [CrossRef] [Green Version]
- Gandolfi, M.G.; Siboni, F.; Botero, T.; Bossu, M.; Riccitiello, F.; Prati, C. Calcium silicate and calcium hydroxide materials for pulp capping: Biointeractivity, porosity, solubility and bioactivity of current formulations. J. Appl. Biomater. Funct. Mater. 2015, 13, 43–60. [Google Scholar] [CrossRef] [PubMed]
- Natale, L.C.; Rodrigues, M.C.; Xavier, T.A.; Simoes, A.; de Souza, D.N.; Braga, R.R. Ion release and mechanical properties of calcium silicate and calcium hydroxide materials used for pulp capping. Int. Endod. J. 2015, 48, 89–94. [Google Scholar] [CrossRef]
- Tran, X.V.; Gorin, C.; Willig, C.; Baroukh, B.; Pellat, B.; Decup, F.; Opsahl Vital, S.; Chaussain, C.; Boukpessi, T. Effect of a calcium-silicate-based restorative cement on pulp repair. J. Dent Res. 2012, 91, 1166–1171. [Google Scholar] [CrossRef] [PubMed]



© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chung, M.; Lee, S.; Chen, D.; Kim, U.; Kim, Y.; Kim, S.; Kim, E. Effects of Different Calcium Silicate Cements on the Inflammatory Response and Odontogenic Differentiation of Lipopolysaccharide-Stimulated Human Dental Pulp Stem Cells. Materials 2019, 12, 1259. https://doi.org/10.3390/ma12081259
Chung M, Lee S, Chen D, Kim U, Kim Y, Kim S, Kim E. Effects of Different Calcium Silicate Cements on the Inflammatory Response and Odontogenic Differentiation of Lipopolysaccharide-Stimulated Human Dental Pulp Stem Cells. Materials. 2019; 12(8):1259. https://doi.org/10.3390/ma12081259
Chicago/Turabian StyleChung, Minsun, Sukjoon Lee, Dongzi Chen, Ukseong Kim, Yaelim Kim, Sunil Kim, and Euiseong Kim. 2019. "Effects of Different Calcium Silicate Cements on the Inflammatory Response and Odontogenic Differentiation of Lipopolysaccharide-Stimulated Human Dental Pulp Stem Cells" Materials 12, no. 8: 1259. https://doi.org/10.3390/ma12081259
APA StyleChung, M., Lee, S., Chen, D., Kim, U., Kim, Y., Kim, S., & Kim, E. (2019). Effects of Different Calcium Silicate Cements on the Inflammatory Response and Odontogenic Differentiation of Lipopolysaccharide-Stimulated Human Dental Pulp Stem Cells. Materials, 12(8), 1259. https://doi.org/10.3390/ma12081259




