Biological and Chemo-Physical Features of Denture Resins
Abstract
:1. Introduction
1.1. Background
1.2. Aim
- Does dental resin material feature influence predictability of the rehabilitation in patients who have dentures? Are dental resin material characteristics influenced by composition in denture?
2. Materials and Methods
2.1. Protocol and Registration
2.2. Eligibility Criteria
- Scientific articles concerning the dental materials of removable prostheses.
- Scientific articles containing information on dental resins.
- Scientific articles concerning chemical–physical and biological interface information on dental acrylic resins.
- Resins used for other purposes or in other areas of medicine.
- Items not accessible, with missing or incomplete dates.
- Articles not in English.
- Short articles, theses, or letters.
2.3. Information Sources
2.4. Search
2.5. Study Selection
2.6. Data Collection Process
2.7. Data Items
- Adequate mechanical and chemical characteristics: they should have high elasticity and resistance as they should bear the weight of the chewing load or the stresses of the buccal liquids.
- High chemical stability.
- Good aesthetic characteristics: the color and translucency should be similar to natural tissue (it is important that the color is maintained over time).
- Insolubility in buccal fluids and absorption of these in the least amount possible.
- Low density, particularly total prostheses should be light and reproduce at the same time all the morphological details.
- High softening temperature, such as not to generate deformations of the prosthesis in the oral cavity.
- Synthetic resins for prosthetic bases: They are used in mobile prostheses for their characteristics, in fact their main component is polymethyl-methacrylate.
- Resins for relining of mobile prostheses: The soft tissues underlying the prosthetic bases tend to undergo changes in shape over time due to the slow reabsorption of the underlying bone tissue. It is therefore necessary to change the shape of the surface of the resin prosthesis that comes into contact with the mucosa to maintain adequate adhesion. For this operation, resins similar to the previous ones need to be used, but they need to be able to perfectly adapt to achieve the desired purpose.
- Resins for repair of mobile prostheses: Despite the constant stresses that prostheses undergo during normal chewing functions, relatively few fractures occur in the mouth; this is often due to too thin bases and too deep or acute frenum measurements.
- Artificial resins: These are similar in composition to those for prosthetic bases but contain a greater concentration of substances that increase their wear resistance and the weight of the chewing load (the part of the teeth that is fixed to the resin base, however, contains a lower amount of these substances in order to allow a correct union with the resin of the base itself).
- Resins for fixed prosthesis crowns and bridges: For this use, various types of resins are available that have a wide range of colors similar to natural teeth, heat-cured acrylic resins, thermopolymerizable vinyl-acrylic copolymers, modified acrylic resins, acrylic resins with reinforcing substances, and composite resins based on the Bowen monomer [32,33,34].
2.8. Risk of Bias
2.9. Summary Measures
- ◦
- Author and year—author and year of publication;
- ◦
- Type of study—type of manuscript (article, Randomized Clinical Trials (RCT), review, etc.);
- ◦
- Sample size and type—sample size and type of performed analysis (in vitro, in vivo, in silico etc);
- ◦
- Intervention/method—type of group subdivision and features;
- ◦
- Main outcomes—intervention on single specimens and type of evaluated outcomes;
- ◦
- Main results—main results of the single study;
- ◦
- Statistical analysis—statistical data regarding outcomes.
- ◦
- Biological features—only biological outcomes, host tissue or cell implications.
- ◦
- Microbiological features—microbiological outcomes, bacteria, fungi or virus.
- ◦
- Physical features—physical, mechanical, chemical properties.
- ◦
- Other—other outcomes, in this case, only one result evaluated “patient acceptability”.
2.10. Synthesis of Results
2.11. Additional Analysis
- Liquid: methacrylate, tetramethylene, dimethacrylate.
- Powder: dibenzoyl peroxide, methyl methacrylate (does not contain cadmium).
3. Results
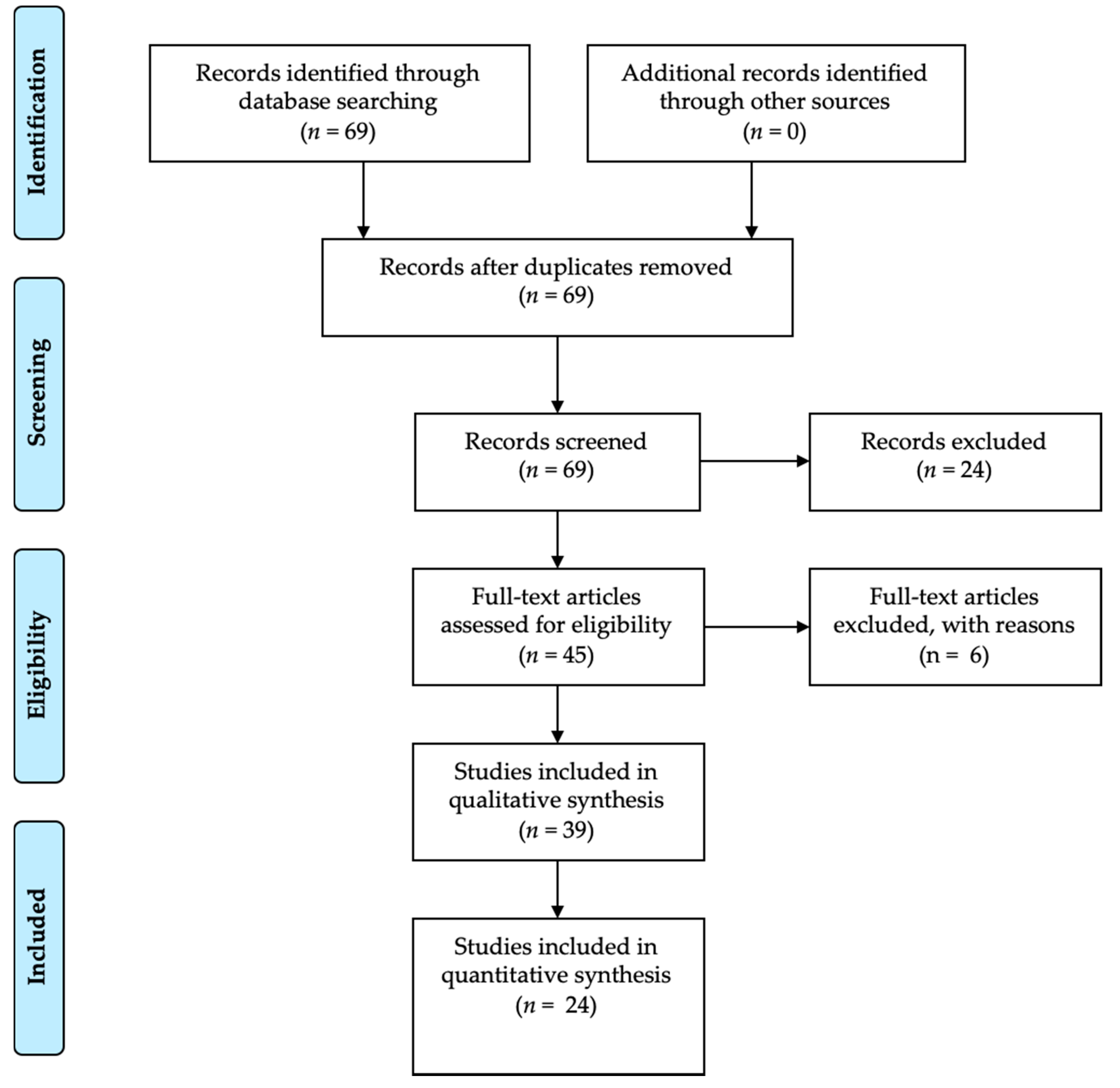
3.1. Study Selection
3.2. Study Characteristics
3.3. Risk of Bias
3.4. Results of Individual Studies
3.5. Synthesis of Results
3.5.1. Microbiological Properties
3.5.2. Biological Properties
3.5.3. Physical Properties
3.6. Additional Analysis
4. Discussion
4.1. Summary of Evidence
4.1.1. Microbiological Properties
4.1.2. Biological Properties
4.1.3. Physical Properties
4.2. Limitations
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Poole, D.F.; Newman, H.N. Dental plaque and oral health. Nature 1971, 234, 329–331. [Google Scholar] [CrossRef]
- Makin, S. Searching for digital technology’s effects on well-Being. Nature 2018, 563, S138–S140. [Google Scholar] [CrossRef]
- Hodson, R. Digital revolution. Nature 2018, 563, S131. [Google Scholar] [CrossRef] [PubMed]
- Diesendorf, M. The mystery of declining tooth decay. Nature 1986, 322, 125–129. [Google Scholar] [CrossRef]
- Pihlstrom, B.L.; Michalowicz, B.S.; Johnson, N.W. Periodontal diseases. Lancet 2005, 366, 1809–1820. [Google Scholar] [CrossRef] [Green Version]
- Bjertness, E.; Hansen, B.F.; Berseth, G.; Gronnesby, J.K. Oral hygiene and periodontitis in young adults. Lancet 1993, 342, 1170–1171. [Google Scholar] [CrossRef]
- El-Assal, G.S. Ancient Egyptian medicine. Lancet 1972, 2, 272–274. [Google Scholar] [CrossRef]
- Ortiz, C.; Boyce, M.C. Materials science. Bioinspired structural materials. Science 2008, 319, 1053–1054. [Google Scholar] [CrossRef]
- Rueggeberg, F.A. From vulcanite to vinyl, a history of resins in restorative dentistry. J. Prosthet. Dent. 2002, 87, 364–379. [Google Scholar] [CrossRef] [PubMed]
- Hensten-Pettersen, A. Skin and mucosal reactions associated with dental materials. Eur. J. Oral Sci. 1998, 106, 707–712. [Google Scholar] [PubMed]
- Godovalov, A.P.; Stepanov, M.S.; Yakovlev, M.V.; Kobzarenko, E.E.; Batog, K.A. Determination of biofilm forming activity of microorganisms on synthetic polymeric materials. Klin. Lab. Diagn. 2019, 64, 758–761. [Google Scholar] [CrossRef] [PubMed]
- Fugolin, A.P.; Dobson, A.; Mbiya, W.; Navarro, O.; Ferracane, J.L.; Pfeifer, C.S. Use of (meth)acrylamides as alternative monomers in dental adhesive systems. Dent. Mater. 2019, 35, 686–696. [Google Scholar] [CrossRef] [PubMed]
- Nagireddi, S.; Katiyar, V.; Uppaluri, R. Pd(II) adsorption characteristics of glutaraldehyde cross-Linked chitosan copolymer resin. Int. J. Biol. Macromol. 2017, 94, 72–84. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Via, B.K.; Pan, Y.; Cheng, Q.; Guo, H.; Auad, M.L.; Taylor, S. Preparation and Characterization of Epoxy Resin Cross-Linked with High Wood Pyrolysis Bio-Oil Substitution by Acetone Pretreatment. Polymers (Basel) 2017, 9, 106. [Google Scholar] [CrossRef] [Green Version]
- Marenzi, G.; Impero, F.; Scherillo, F.; Sammartino, J.C.; Squillace, A.; Spagnuolo, G. Effect of Different Surface Treatments on Titanium Dental Implant Micro-Morphology. Materials (Basel) 2019, 12, 733. [Google Scholar] [CrossRef] [Green Version]
- Cervino, G.; Fiorillo, L.; Arzukanyan, A.V.; Spagnuolo, G.; Cicciù, M. Dental restorative digital workflow: Digital smile design from aesthetic to function. Dent. J. 2019, 7, 30. [Google Scholar] [CrossRef] [Green Version]
- Cicciù, M.; Risitano, G.; Lo Giudice, G.; Bramanti, E. Periodontal health and caries prevalence in patients affected by Parkinson’s Disease. Parkinson’s Disease 2012, 541908. [Google Scholar] [CrossRef]
- Di Salle, A.; Spagnuolo, G.; Conte, R.; Procino, A.; Peluso, G.; Rengo, C. Effects of various prophylactic procedures on titanium surfaces and biofilm formation. J. Periodontal. Implant Sci. 2018, 48, 373–382. [Google Scholar] [CrossRef]
- Cervino, G.; Fiorillo, L.; Spagnuolo, G.; Bramanti, E.; Laino, L.; Lauritano, F.; Cicciù, M. Interface between MTA and dental bonding agents: Scanning electron microscope evaluation. J. Int. Soc. Prev. Community Dent. 2017, 7, 64–68. [Google Scholar] [CrossRef]
- Cicciù, M.; Bramanti, E.; Cecchetti, F.; Scappaticci, L.; Guglielmino, E.; Risitano, G. Fem and Von Mises analyses of different dental implant shapes for masticatory load distribution. ORAL Implantol. 2014, 7, 1–10. [Google Scholar]
- Spagnuolo, G.; Ametrano, G.; D’Antò, V.; Formisano, A.; Simeone, M.; Riccitiello, F.; Amato, M.; Rengo, S. Microcomputed tomography analysis of mesiobuccal orifices and major apical foramen in first maxillary molars. Open Dent. J. 2012, 6, 118–125. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Patini, R.; Gallenzi, P.; Spagnuolo, G.; Cordaro, M.; Cantiani, M.; Amalfitano, A.; Arcovito, A.; Calla, C.; Mingrone, G.; Nocca, G. Correlation Between Metabolic Syndrome, Periodontitis and Reactive Oxygen Species Production. Open Dent. J. 2017. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vojdani, M.; Giti, R. Polyamide as a Denture Base Material: A Literature Review. J. Dent. (Shiraz) 2015, 16, 1–9. [Google Scholar]
- Nandal, S.; Ghalaut, P.; Shekhawat, H.; Gulati, M.S. New Era in Denture Base Resins: A Review. Dent. J. Adv. Stud. 2013, 1, 136–143. [Google Scholar] [CrossRef] [Green Version]
- Hutton, B.; Salanti, G.; Caldwell, D.M.; Chaimani, A.; Schmid, C.H.; Cameron, C.; Ioannidis, J.P.; Straus, S.; Thorlund, K.; Jansen, J.P.; et al. The PRISMA extension statement for reporting of systematic reviews incorporating network meta-Analyses of health care interventions: Checklist and explanations. Ann. Intern. Med. 2015, 162, 777–784. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tian, J.H.; Ge, L.; Li, L. The PRISMA Extension Statement. Ann. Intern. Med. 2015, 163, 566. [Google Scholar] [CrossRef]
- Liu, H.; Zhou, X.; Yu, G.; Sun, X. The effects of the PRISMA statement to improve the conduct and reporting of systematic reviews and meta-Analyses of nursing interventions for patients with heart failure. Int. J. Nurs. Pract. 2019. [Google Scholar] [CrossRef]
- Dioguardi, M.; Perrone, D.; Troiano, G.; Laino, L.; Ardito, F.; Lauritano, F.; Cicciù, M.; Lo Muzio, L. Cytotoxicity evaluation of five different dual-Cured resin cements used for fiber posts cementation. Int. J. Clin. Exp. Med. 2015, 8, 9327–9333. [Google Scholar]
- Neppelenbroek, K.H.; Kurokawa, L.A.; Procópio, A.L.F.; Pegoraro, T.A.; Hotta, J.; Mello Lima, J.F.; Urban, V.M. Hardness and surface roughness of enamel and base layers of resin denture teeth after long-Term repeated chemical disinfection. J. Contemp. Dent. Pract. 2015, 16, 54–60. [Google Scholar] [CrossRef]
- Pavarina, A.C.; Vergani, C.E.; Machado, A.L.; Giampaolo, E.T.; Teraoka, M.T. The effect of disinfectant solutions on the hardness of acrylic resin denture teeth. J. Oral Rehabil. 2003, 30, 749–752. [Google Scholar] [CrossRef]
- Pero, A.C.; Scavassin, P.M.; Nunes, É.M.; Policastro, V.B.; Giro, G.; Compagnoni, M.A. Bond Strength of Artificial Teeth Attached to a Microwave-Polymerized Denture Base Resin after Immersion in Disinfectant Solutions. J. Prosthodont. 2016, 25, 576–579. [Google Scholar] [CrossRef] [PubMed]
- Mumoli, N.; Busoni, A.; Cei, M. A swallowed denture. Lancet 2009, 373, 1890. [Google Scholar] [CrossRef]
- Rossi, T.; Laine, J.; Eerola, E.; Kotilainen, P.; Peltonen, R. Denture carriage of methicillin-resistant Staphylococcus aureus. Lancet 1995, 345, 1577. [Google Scholar] [CrossRef]
- Tsunoda, A.; Kanazawa, H.; Ishige, T.; Kishimoto, S. A missing denture. Lancet 2004, 364, 1884. [Google Scholar] [CrossRef]
- Higgins, J.P.; Altman, D.G.; Gotzsche, P.C.; Juni, P.; Moher, D.; Oxman, A.D.; Savovic, J.; Schulz, K.F.; Weeks, L.; Sterne, J.A. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. Bmj 2011, 343, d5928. [Google Scholar] [CrossRef] [Green Version]
- Higgins, J.P.T.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.A. (Eds.) Assessing Risk of Bias in Included Studies. In Cochrane Handbook for Systematic Reviews of Interventions; Version 5.1.0; John Wiley & Sons: Auckland, New Zealand, 2008. [Google Scholar] [CrossRef]
- Bachelet, V.C.; Pardo-Hernandez, H. Quality of reporting and risk of bias of randomized clinical trials published in Spanish and Latin American journals. Medwave 2019, 19, e7573. [Google Scholar] [CrossRef]
- Bacali, C.; Baldea, I.; Moldovan, M.; Carpa, R.; Olteanu, D.E.; Filip, G.A.; Nastase, V.; Lascu, L.; Badea, M.; Constantiniuc, M.; et al. Flexural strength, biocompatibility, and antimicrobial activity of a polymethyl methacrylate denture resin enhanced with graphene and silver nanoparticles. Clin. Oral Investig. 2019. [Google Scholar] [CrossRef]
- Alfaifi, A.A.; Lin, W.S.; Aldhaian, B.A.; Levon, J.A.; Gregory, R.L. Impact of caffeine on metabolic activity and biofilm formation of Candida albicans on acrylic denture resin in the presence of nicotine. J. Prosthet. Dent. 2019. [Google Scholar] [CrossRef]
- Al-Thobity, A.M.; Gad, M.; ArRejaie, A.; Alnassar, T.; Al-Khalifa, K.S. Impact of Denture Cleansing Solution Immersion on Some Properties of Different Denture Base Materials: An In Vitro Study. J. Prosthodont. 2019, 28, 913–919. [Google Scholar] [CrossRef]
- Somkuwar, S.; Mishra, S.K.; Agrawal, B.; Choure, R. Comparison of the flexural strength of polymethyl methacrylate resin reinforced with multiwalled carbon nanotubes and processed by conventional water bath technique and microwave polymerization. J. Indian Prosthodont. Soc. 2017, 17, 332–339. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.H.; Jun, S.K.; Kim, S.C.; Okubo, C.; Lee, H.H. Investigation of the cytotoxicity of thermoplastic denture base resins. J. Adv. Prosthodont. 2017, 9, 453–462. [Google Scholar] [CrossRef] [Green Version]
- Wagner, D.A.; Pipko, D.J. The effect of repeated microwave irradiation on the dimensional stability of a specific acrylic denture resin. J. Prosthodont. 2015, 24, 25–31. [Google Scholar] [CrossRef] [PubMed]
- De Sousa Porta, S.R.; de Lucena-Ferreira, S.C.; da Silva, W.J.; Del Bel Cury, A.A. Evaluation of sodium hypochlorite as a denture cleanser: a clinical study. Gerodontology 2015, 32, 260–266. [Google Scholar] [CrossRef] [PubMed]
- Wang, R.; Tao, J.; Yu, B.; Dai, L. Characterization of multiwalled carbon nanotube-polymethyl methacrylate composite resins as denture base materials. J. Prosthet. Dent. 2014, 111, 318–326. [Google Scholar] [CrossRef] [PubMed]
- Akalın-Evren, B.; Kulak-Özkan, Y.; Ozcan, M.; Kadir, T. Candida albicans adhesion on reinforced polymethylmethacrylate denture resin: effect of fibre architecture and exposure to saliva. Gerodontology 2014, 31, 194–201. [Google Scholar] [CrossRef] [PubMed]
- Mansour, M.M.; Wagner, W.C.; Chu, T.M. Effect of mica reinforcement on the flexural strength and microhardness of polymethyl methacrylate denture resin. J. Prosthodont. 2013, 22, 179–183. [Google Scholar] [CrossRef]
- So, Y.C.; Tsoi, J.K.-H.; Matinlinna, J.P. A New Approach to Cure and Reinforce Cold-Cured Acrylics. Silicon 2012, 4, 209–220. [Google Scholar] [CrossRef] [Green Version]
- Monteiro, D.R.; Gorup, L.F.; Takamiya, A.S.; de Camargo, E.R.; Filho, A.C.; Barbosa, D.B. Silver distribution and release from an antimicrobial denture base resin containing silver colloidal nanoparticles. J. Prosthodont. 2012, 21, 7–15. [Google Scholar] [CrossRef]
- Ladha, K.; Shah, D. An in-vitro evaluation of the flexural strength of heat-Polymerized poly (methyl methacrylate) denture resin reinforced with fibers. J. Indian Prosthodont. Soc. 2011, 11, 215–220. [Google Scholar] [CrossRef]
- Fan, C.; Chu, L.; Rawls, H.R.; Norling, B.K.; Cardenas, H.L.; Whang, K. Development of an antimicrobial resin--a pilot study. Dent. Mater. 2011, 27, 322–328. [Google Scholar] [CrossRef]
- Zortuk, M.; Kılıc, K.; Uzun, G.; Ozturk, A.; Kesim, B. The effect of different fiber concentrations on the surface roughness of provisional crown and fixed partial denture resin. Eur. J. Dent. 2008, 2, 185–190. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Puri, G.; Berzins, D.W.; Dhuru, V.B.; Raj, P.A.; Rambhia, S.K.; Dhir, G.; Dentino, A.R. Effect of phosphate group addition on the properties of denture base resins. J. Prosthet. Dent. 2008, 100, 302–308. [Google Scholar] [CrossRef] [Green Version]
- Faot, F.; Garcia, R.C.; Del Bel Cury, A.A. Fractographic analysis, accuracy of fit and impact strength of acrylic resin. Braz Oral Res. 2008, 22, 334–339. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, S.K.; Heo, S.J.; Koak, J.Y.; Lee, J.H.; Lee, Y.M.; Chung, D.J.; Lee, J.I.; Hong, S.D. A biocompatibility study of a reinforced acrylic-based hybrid denture composite resin with polyhedraloligosilsesquioxane. J. Oral Rehabil. 2007, 34, 389–395. [Google Scholar] [CrossRef] [PubMed]
- Tacir, I.H.; Kama, J.D.; Zortuk, M.; Eskimez, S. Flexural properties of glass fibre reinforced acrylic resin polymers. Aust. Dent J. 2006, 51, 52–56. [Google Scholar] [CrossRef] [Green Version]
- Kimoto, S.; Kobayashi, N.; Kobayashi, K.; Kawara, M. Effect of bench cooling on the dimensional accuracy of heat-Cured acrylic denture base material. J. Dent. 2005, 33, 57–63. [Google Scholar] [CrossRef]
- Pesci-Bardon, C.; Fosse, T.; Madinier, I.; Serre, D. In vitro new dialysis protocol to assay the antiseptic properties of a quaternary ammonium compound polymerized with denture acrylic resin. Lett. Appl. Microbiol. 2004, 39, 226–231. [Google Scholar] [CrossRef]
- Uzun, G.; Keyf, F. The effect of fiber reinforcement type and water storage on strength properties of a provisional fixed partial denture resin. J. Biomater. Appl. 2003, 17, 277–286. [Google Scholar] [CrossRef]
- Keyf, F.; Uzun, G.; Mutlu, M. The effects of HEMA-monomer and air atmosphere treatment of glass fibre on the transverse strength of a provisional fixed partial denture resin. J. Oral Rehabil. 2003, 30, 1142–1148. [Google Scholar] [CrossRef]
- John, J.; Gangadhar, S.A.; Shah, I. Flexural strength of heat-polymerized polymethyl methacrylate denture resin reinforced with glass, aramid, or nylon fibers. J. Prosthet. Dent. 2001, 86, 424–427. [Google Scholar] [CrossRef]
- Riccitiello, F.; De Luise, A.; Conte, R.; D’Aniello, S.; Vittoria, V.; Di Salle, A.; Calarco, A.; Peluso, G. Effect of resveratrol release kinetic from electrospun nanofibers on osteoblast and osteoclast differentiation. Eur. Polym. J. 2018, 99, 289–297. [Google Scholar] [CrossRef]
- Guarnieri, R.; Grande, M.; Ippoliti, S.; Iorio-Siciliano, V.; Riccitiello, F.; Farronato, D. Influence of a Laser-Lok surface on immediate functional loading of implants in single-tooth replacement: Three-year results of a prospective randomized clinical study on soft tissue response and esthetics. Int. J. Periodontics Restor. Dent. 2015, 35, 864–875. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- De Santis, R.; Gloria, A.; Russo, T.; D’Amora, U.; Varriale, A.; Veltri, M.; Balleri, P.; Mollica, F.; Riccitiello, F.; Ambrosio, L. Reverse engineering of mandible and prosthetic framework: Effect of titanium implants in conjunction with titanium milled full arch bridge prostheses on the biomechanics of the mandible. J. Biomech. 2014, 47, 3825–3829. [Google Scholar] [CrossRef] [Green Version]
- D’Antò, V.; Eckhardt, A.; Hiller, K.A.; Spagnuolo, G.; Valletta, R.; Ambrosio, L.; Schmalz, G.; Schweikl, H. The influence of Ni(II) on surface antigen expression in murine macrophages. Biomaterials 2009, 30, 1492–1501. [Google Scholar] [CrossRef]
- Krifka, S.; Petzel, C.; Bolay, C.; Hiller, K.A.; Spagnuolo, G.; Schmalz, G.; Schweikl, H. Activation of stress-regulated transcription factors by triethylene glycol dimethacrylate monomer. Biomaterials 2011, 32, 1787–1795. [Google Scholar] [CrossRef]
- Eckhardt, A.; Müller, P.; Hiller, K.A.; Krifka, S.; Bolay, C.; Spagnuolo, G.; Schmalz, G.; Schweikl, H. Influence of TEGDMA on the mammalian cell cycle in comparison with chemotherapeutic agents. Dental Mater. 2010, 26, 232–241. [Google Scholar] [CrossRef]
- Spagnuolo, G.; Desiderio, C.; Rivieccio, V.; Amato, M.; Rossetti, D.V.; D’Antò, V.; Schweikl, H.; Lupi, A.; Rengo, S.; Nocca, G. In vitro cellular detoxification of triethylene glycol dimethacrylate by adduct formation with N-acetylcysteine. Dental Mater. 2013, 29, e153–e160. [Google Scholar] [CrossRef]
- Castrogiovanni, P.; Trovato, F.M.; Szychlinska, M.A.; Nsir, H.; Imbesi, R.; Musumeci, G. The importance of physical activity in osteoporosis. From the molecular pathways to the clinical evidence. Histol. Histopathol. 2016, 31, 1183–1194. [Google Scholar] [CrossRef]
- Fiorillo, L.; Musumeci, G. TMJ Dysfunction and Systemic Correlation. J. Funct. Morphol. Kinesiol. 2020, 5, 20. [Google Scholar] [CrossRef] [Green Version]
- Ametrano, G.; D’Antò, V.; Di Caprio, M.P.; Simeone, M.; Rengo, S.; Spagnuolo, G. Effects of sodium hypochlorite and ethylenediaminetetraacetic acid on rotary nickel-Titanium instruments evaluated using atomic force microscopy. Int. Endod. J. 2011, 44, 203–209. [Google Scholar] [CrossRef]
- Spagnuolo, G.; Ametrano, G.; D’Antò, V.; Rengo, C.; Simeone, M.; Riccitiello, F.; Amato, M. Effect of autoclaving on the surfaces of TiN-Coated and conventional nickel-titanium rotary instruments. Int. Endod. J. 2012, 45, 1148–1155. [Google Scholar] [CrossRef] [PubMed]
- Sambataro, S.; Bocchieri, S.; Cervino, G.; La Bruna, R.; Cicciù, A.; Innorta, M.; Torrisi, B.; Cicciù, M. Correlations between Malocclusion and Postural Anomalies in Children with Mixed Dentition. J. Funct. Morphol. Kinesiol. 2019, 4, 45. [Google Scholar] [CrossRef] [Green Version]
- Tan, C.-M.; Tsoi, J.K.-H.; Seneviratne, C.J.; Matinlinna, J.P. Evaluation of the Candida albicans removal and mechanical properties of denture acrylics cleaned by a low-Cost powered toothbrush. J. Prosthodont. Res. 2014, 58, 243–251. [Google Scholar] [CrossRef] [PubMed]
- Cervino, G.; Montanari, M.; Santonocito, D.; Nicita, F.; Baldari, R.; De Angelis, C.; Storni, G.; Fiorillo, L. Comparison of Two Low-Profile Prosthetic Retention System Interfaces: Preliminary Data of an In Vitro Study. Prosthesis 2019, 1, 54–60. [Google Scholar] [CrossRef] [Green Version]
- Cicciù, M. Prosthesis: New Technological Opportunities and Innovative Biomedical Devices. Prosthesis 2019, 1, 1. [Google Scholar] [CrossRef] [Green Version]
- Fiorillo, L.; D’Amico, C.; Turkina, A.Y.; Nicita, F.; Amoroso, G.; Risitano, G. Endo and Exoskeleton: New Technologies on Composite Materials. Prosthesis 2020, 2, 1–9. [Google Scholar] [CrossRef] [Green Version]
- Scrascia, R.; Fiorillo, L.; Gaita, V.; Secondo, L.; Nicita, F.; Cervino, G. Implant-Supported Prosthesis for Edentulous Patient Rehabilitation. From Temporary Prosthesis to Definitive with a New Protocol: A Single Case Report. Prosthesis 2020, 2, 10–24. [Google Scholar] [CrossRef] [Green Version]
- Bramanti, E.; Matacena, G.; Cecchetti, F.; Arcuri, C.; Cicciù, M. Oral health-related quality of life in partially edentulous patients before and after implant therapy: A 2-year longitudinal study. ORAL Implantol. 2013, 6, 37–42. [Google Scholar] [CrossRef]
- De Stefano, R. Psychological Factors in Dental Patient Care: Odontophobia. Medicina 2019, 55, 678. [Google Scholar] [CrossRef] [Green Version]
- Fiorillo, L.; Cervino, G.; De Stefano, R.; Iannello, G.; Cicciù, M. Socio-economic behaviours on dental profession: an in Italy google trends investigation. In Minerva Stomatol; Minerva Medica Edition: Turin, Italy, 2020. [Google Scholar] [CrossRef]
- Militi, A.; Cicciu, M.; Sambataro, S.; Bocchieri, S.; Cervino, G.; De Stefano, R.; Fiorillo, L. Dental occlusion and sport performance. In Minerva Stomatol; Minerva Medica Edition: Turin, Italy, 2020. [Google Scholar] [CrossRef]
- Bettencourt, A.F.; Neves, C.B.; de Almeida, M.S.; Pinheiro, L.M.; Oliveira, S.A.; Lopes, L.P.; Castro, M.F. Biodegradation of acrylic based resins: A review. Dent. Mater. 2010, 26, e171–e180. [Google Scholar] [CrossRef]
- Consani, R.L.; Mesquita, M.F.; de Arruda Nobilo, M.A.; Henriques, G.E. Influence of simulated microwave disinfection on complete denture base adaptation using different flask closure methods. J. Prosthet. Dent. 2007, 97, 173–178. [Google Scholar] [CrossRef] [PubMed]
- Nicholson, W.J. Titanium Alloys for Dental Implants: A Review. Prosthesis 2020, 2, 100–116. [Google Scholar] [CrossRef]




| Author and Year | Type of Study | Sample Size and Type | Intervention/Method | Main Outcomes | Main Results | Statistical Analysis |
|---|---|---|---|---|---|---|
| Bacali et al. [38] 2019 | Original Article | In vitro study | Auto-polymerizing acrylic resin loaded with 1 wt% (weight) G-AgNp (graphene-Ag nanoparticles) (test1) and 2 wt% G-AgNp (test 2) | Methyl methacrylate monomer (MMA) release; cell (dysplastic oral keratinocytes (DOK) and dental pulp stem cells) viability; oxidative stress and inflammatory response of DOK; antibacterial activity | MMA concentration reached high levels when immersed in chloroform; cell viability displayed a decrease; pro inflammatory molecules (as TNF- α) decreased; antibacterial properties against Gram + bacteria | No significant results of cells viability (p = 0.472); significant reduction in TNF- α levels p = 0.016 and p = 0.104 (for test 1 and 2 respectively); significant antibacterial properties for test 1 and test 2 (p < 0.05); significantly improved flexural strength (P < 0.05) |
| Alfaifi et al. [39] 2019 | Original Article | 240 acrylic resin specimens; in vitro study | Candida albicans metabolic activity (group 1); C. albicans biofilm attachment (group 2) | After nicotine and caffeine administration: C. albicans metabolic activity; C. albicans biofilm attachment | The presence of 8mg/mL of nicotine increased the metabolic activity and biofilm formation of C. albicans | Significant p < 0.05 |
| Al-Thobity et al. [40] 2019 | 81 resin specimens; in vitro study | Heat-polymerized (HP) denture base material (group 1); auto-polymerized (AP) denture base material (group 2); visible-light-polymerized (VLP) denture base (group 3) | Denture cleansing solution application, the distilled water group (DWG), Corega group (CG), Renew group (RG): flexural strength; color changes; surface roughness | Color change detected was in the VLP resin treated with Corega and Renew; increased roughness of all denture resin groups after immersion in Corega; reduction in flexural strength in the HP resin after immersion in Corega. | Statistically significant color change p < 0.05; significant increase in the surface roughness p < 0.05; flexural strength reduction p < 0.05 | |
| Somkuwar et al. [41] | Original article | 180 acrylic resins specimen; in vitro study | Polymethyl methacrylate resin reinforced with 0.025% multiwalled carbon nanotubes (MWCNTs) (group 1); polymethyl methacrylate resin reinforced with 0.050% MWCNTs | conventional water bath groups and microwave group: flexural strength | The mean flexural strength of specimens cured by water bath technique was 95.563 MPa and microwave technique was 118.416 MPa. High percentage of multiwalled carbon nanotubes present better flexural strength | Better flexural strength on microwave group p < 0.05; better flexural strength on high MWCNTs groups p < 0.05 |
| Lee et al. [42] 2017 | Original article | Six thermoplastic resin materials; in vitro study | Three polyamide materials (Smile tone, ST; valplast, VP; and Luciton FRS, LF), two acrylic materials (Acrytone, AT; and Acryshot, AS), and one polypropylene resin material (Unigum, UG), heat-polymerized acrylic resin (Vertex RS, RS) (control) | Extracts and culture with immortalized human oral keratinocytes (IHOKs) or mouse fibroblasts: cytotoxicity | VP at 70° extract and AT at 121° extract showed lower cytotoxicity | p < 0.05 |
| Wagner et al. [43] 2017 | Original article | 20 dentures; in vitro study | PMMA (poly(methyl methacrylate)) acrylic resin | Microwave irradiation at 700W and 420W: dimensional stability | Denture experienced a linear dimensional change of approximately 3% | Significant at p < 0.05 |
| De Sousa Porta et al. [44] 2014 | Original article | 15 participants; clinical study | Acrylic resin dentures | 0.5% NaOCl for 3 min over 90 days: biofilm formation, color stability, surface roughness, patient acceptability | Reduction in microorganism and C. albicans; no difference in color and roughness; increased level of patient satisfaction | Significant microorganism reduction p = 0.001; color p = 0.68; roughness p = 0.47 |
| Wang et al. [45] 2014 | Original Article | In vitro study | Acrylic resin dentures loaded with 0.5, 1, 2 wt% multiwalled carbon nanotubes | Flexural strength | 2 wt% MWCNT-loaded dentures showed not beneficial results | Worst mechanical properties on 2 wt% MWCNT-loaded dentures |
| Akalin-Evren et al. [46] 2014 | Original Article | 48 denture base resins; in vitro study | Denture base resin reinforced with E-glass fiber-reinforced composites (FRC) | Treated with saliva or distilled water; C. albicans adhesion | C. albicans adhesion did not show differences | Not significant p = 0.436 |
| Mansour et al. [47] 2013 | Original Article | 199 denture bases; in vitro study | Wet ground muscovite mica and Lucitone 199 original shade denture base resin: (A) control group with 0 vol% mica, (B) 10 vol% W200 mica, (C) 20 vol% W200 mica, (D) 10 vol% P66 mica, (E) 20 vol% P66 mica. | The mica was silane treated in a solution of 3-methacryloxypropyl trimethoxysilane, ethanol, and water, and then dried; flexural strength and microhardness | The flexural strength of the control group 77–94%. No significant differences were found within the four mica groups. Microhardnesses of the 20% mica groups were 33–26%. | Flexural strength higher in control than mica p ≤ 0.05. Microhardness of the C group was higher than control (p ≤ 0.05). |
| So et al. [48] 2012 | Original Article | 50 specimens; in vitro study | Cold cured PMMA with 0%, 2%, 3%, 5% E-glass fibers with and without post-curing microwave at 800 w for 3 min | Water storage for 7,14 and 30 days; Flexural strength, maximum load on the load-deflection curve | The group with 3% fiber and microwave treatment, and the groups with 5% fiber increase in the flexural strength values compared with the control group | Flexural strength on 3% and 5% E-glass fiber(p = 0.003 and p ≤ 0.003) |
| Monteiro et al. [49] 2011 | Original Article | Denture resin; in vitro study | Denture base resin containing silver colloidal nanoparticles in different concentration 0.05, 0.5, and 5 vol% silver colloidal | Specimens were stored in deionized water at 37 °C for 7, 15, 30, 60 and 120 days; silver distribution and release | Silver was not detected in deionized water; silver distribution and dispersion was improved with lower silver concentration | / |
| Ladha et al. [50] 2011 | Original Article | 160 resin specimens; in vitro study | Conventional PMMA denture resin; unidirectional stick (S) glass fiber reinforced-PMMA denture resin; woven stick net (SN) glass fiber-reinforced PMMA denture resin; nylon fiber-reinforced PMMA denture resin | Each group was stored in dry and wet conditions; flexural strength | Glass fiber reinforcements enhanced flexural strength of heat cured PMMA denture | Significant enhanced flexural strength in glass fiber-reinforced group |
| Fan et al. [51] 2011 | Original article | In vitro study | Light-cure denture resins with Ag benzoate of various concentration (0, 0.002, 0.02, 0.1, 0.15 and 0.2%); chemical-cure systems with Ag benzoate various concentration (0, 0.002, 0.02, 0.1, 0.15 and 0.2%) | Resin hardness, silver release, antibacterial activity | Hardness was unaffected by Ag benzoate, and silver was released only at a concentration higher than 0.1% | / |
| Zortuk et al. [52] 2008 | Original article | 48 specimens; in vitro study | Auto-polymerizing acrylic resin (no fiber); auto-polymerizing acrylic resin with glass fiber (0.5%); auto-polymerizing acrylic resin with glass fiber (1%); auto-polymerizing acrylic resin with glass fiber (2%) | Surface specimens polishing; surface roughness (Ra) | Difference in resin surface roughness with different concentrations of fiber | p < 0.001 |
| Puri et al. [53] 2008 | Original article | In vitro study | PMMA resin Lucitone 199; PMMA resin with ethylene glycol methacrylate phosphate (EGMP) 10%; PMMA resin with ethylene glycol methacrylate phosphate (EGMP) 15%; PMMA resin with ethylene glycol methacrylate phosphate (EGMP) 15% + cross linking agent; PMMA resin with ethylene glycol methacrylate phosphate (EGMP) 20% | Impact strength, fracture toughness, wettability, resin bonding ability | Hydrophilicity was increased increasing EGMP concentrations, with no other differences between groups | Improved hydrophilicity p = 0.039 |
| Faot et al. [54] 2008 | Original Article | In vitro study | Microwave acrylic resin polymerized with 3 min at 360 W, 4-min pause, and 3 min at 810 W (Control); microwave acrylic resin polymerized with an alternative cycle (AC) of 6 min at 630 W | Accuracy of fit at 0 time and at 30 days, impact strength test (Charpy method), fractographic analysis | No difference in outcomes between groups, denture bases showed a better fit after 30-days of storage in water | Better fit after 30 days in water p < 0.05 |
| Kim et al. [55] 2007 | Original Article | In vitro study | Reinforced acrylic-based hybrid denture composite resin with polyhedraloligosilsesquioxane (POSS) (group 1); heat-polymerized acrylic denture base resin (group 2); auto-polymerized acrylic denture base resin (group 3); direct relining acrylic denture base resin (group 4) | Biocompatibility, mutagenesis | POSS showed improved biocompatibility and lower mutagenicity. | Group 1 showed less cytotoxicity (p < 0.05); group 4 showed the highest cytotoxicity (p < 0.05) |
| Tacir et al. [56] 2006 | Original article | 80 specimens; in vitro study | Conventional heat-polymerized acrylic resin (group 1); Heat-polymerized acrylic resin with glass fibers (10–15μm thick and 5mm long) (group 2); microwaved Shera-Med MW 2000 (Dental-Werkstoffe, Lemförde, Germany) PMMA in a polycarbonate flask (group 3); microwaved Shera-Med MW 2000 (Dental-Werkstoffe, Lemförde, Germany) PMMA in a polycarbonate flask with glass fibers (10–15μm thick and 5mm long) (group 4) | Flexural strength | Group 2 presented better fracture resistance but less flexural strength | p < 0.05 |
| Kimoto et al. [57] 2005 | Original article | In vitro study | Rapid cooling after heat polymerization (group 1); bench cooling after heath polymerization (group 2) | Denture strain | Bench cooling for the heat-cured denture reduced the strain | p < 0.05 |
| Pesci-Bardon et al. [58] 2004 | Original article | 216 specimens; in vitro study | Acrylic resin discs added with Poly 202063A and large volumes of microbial inoculum (45 mL) (group 1); acrylic resin discs added with Poly 202063A and microbial inoculum (600 microL) (group 2); Acrylic resin discs added with Poly 202063A and sterile buffer (600 microL) (group 3) | Antiseptic properties | A bactericidal effect against Escherichia coli and Staphylococcus aureus. A dose-dependent fungistatic effect was observed against C. albicans. | bactericidal effect p = 0.012; antifungal effect p = 0.003 |
| Uzun et al. [59] 2003 | Original article | 16 specimens; in vitro study | Pre-treated epoxy resin-coated glass fibers, with aramid fibers, or with no fibers | Immediately and at 30-days water storage; transverse strength, maximal deflection, modulus of elasticity | No differences in strength and deflection values in immediate group and 30 days group | Aramid fiber and without fiber (p = 0.574), glass fiber and without fiber (p = 0.065) in the immediate group |
| Keyf et al. [60] 2003 | Original article | 36 specimens; In vitro study | Auto-polymerizing acrylic resin with hydroxyethyl-methacrylate (HEMA) treated glass fiber: (group A) discharge power of 15 W and flowrate 15 min, 60 mL min; (group B) 20 W, 10 (group C) 15 W, 15 min, 60 mL min)1; (group D) 20 W, 15 min, 60 mL min)1; (group E) untreated; (group F) without fiber | Load of fracture, transverse strength, deflection, modulus of elasticity | Transverse strength and maximal deflection were different between groups, not for modulus of elasticity | Transverse strength p = 0.006, deflection p = 0.039, elasticity modulus p = 0.491 |
| John et al. [61] 2001 | Original Article | ten specimens; in vitro study | No fiber reinforced-acrylic resin (control); acrylic resin reinforced with glass fibers (test 1); acrylic resin reinforced with aramid (test 2) acrylic resin reinforced with nylon fibers (test 3) | Flexural strength | All reinforced test groups showed better results on flexural strength; glass fiber showed the highest flexural strength | Test 2 had the best result (p < 0.001) |
| Study | Random Sequence Generation | Allocation Concealment | Blinding of Participants and Personnel | Blinding of Outcome Assessment | Incomplete Outcome Data | Selective Reporting | Other Sources of Bias | Overall | Weight |
|---|---|---|---|---|---|---|---|---|---|
| Bacali et al. [38] 2019 | High | Low | High | High | Low | Low | Low | Low | / |
| Alfaifi et al. [39] 2019 | High | Low | High | High | Low | Low | Low | Low | 240 acrylic resin specimens |
| Al-Thobity et al. [40] 2019 | High | Low | High | High | Low | Low | Low | Low | 81 resin specimens |
| Somkuwar et al. [41] 2017 | High | Low | High | High | Low | Low | Low | Low | 180 acrylic resin specimens |
| Lee et al. [42] 2017 | High | Low | High | High | Low | Low | Low | Low | Six thermoplastic resin materials |
| Wagner et al. [43] 2015 | High | Low | High | High | Low | Low | Low | Low | 20 dentures |
| De Sousa Porta et al. [44] 2014 | High | Low | High | High | Low | Low | Low | Low | 15 participants |
| Wang et al. [45] 2014 | High | Low | High | High | Low | Low | Low | Low | / |
| Akalin-Evren et al. [46] 2014 | High | Low | High | High | Low | Low | Low | Low | 48 denture base resins |
| Mansour et al. [47] 2013 | High | Low | High | High | Low | Low | Low | Low | / |
| So et al. [48] | High | Low | High | High | Low | Low | Low | Low | 50 specimens |
| Monteiro et al. [49] 2011 | High | Low | High | High | Low | Low | Low | Low | 199 denture bases |
| Ladha et al. [50] 2011 | High | Low | High | High | Low | Low | Low | Low | Denture resins |
| Fan et al. [51] 2011 | High | Low | High | High | Low | Low | Low | Low | 160 resin specimens |
| Zortuk et al. [52] 2008 | High | Low | High | High | Low | Low | Low | Low | / |
| Puri et al. [53] 2008 | High | Low | High | High | Low | Low | Low | Low | 48 specimens |
| Faot et al. [54] 2008 | High | Low | High | High | Low | Low | Low | Low | / |
| Kim et al. [55] 2007 | High | Low | High | High | Low | Low | Low | Low | / |
| Tacir et al. [56] 2006 | High | Low | High | High | Low | Low | Low | Low | / |
| Kimoto et al. [57] 2005 | High | Low | High | High | Low | Low | Low | Low | 80 specimens |
| Pesci-Bardon et al. [58] 2004 | High | Low | High | High | Low | Low | Low | Low | / |
| Uzun et al. [59] 2003 | High | Low | High | High | Low | Low | Low | Low | 216 specimens |
| Keyf et al. [60] 2003 | High | Low | High | High | Low | Low | Low | Low | 16 specimens |
| John et al. [61] 2001 | High | Low | High | High | Low | Low | Low | Low | 36 specimens |
| Individual Studies Outcomes | |
|---|---|
| Biological features | Cell viability; oxidative stress and inflammatory response; cytotoxicity; silver distribution and release; biocompatibility, mutagenesis. |
| Microbiological features | Antibacterial activity; C. albicans metabolic activity; C. albicans biofilm attachment; biofilm formation; antiseptic properties. |
| Physical features | Flexural strength; color changes; surface roughness; dimensional stability; color stability, microhardness; impact strength, fracture toughness, wettability, resin bonding ability; fractographic analysis; denture strain; transverse strength, maximal deflection, modulus of elasticity; load of fracture; maximum load on the load-deflection curve. |
| Other | Patient acceptability. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cervino, G.; Cicciù, M.; Herford, A.S.; Germanà, A.; Fiorillo, L. Biological and Chemo-Physical Features of Denture Resins. Materials 2020, 13, 3350. https://doi.org/10.3390/ma13153350
Cervino G, Cicciù M, Herford AS, Germanà A, Fiorillo L. Biological and Chemo-Physical Features of Denture Resins. Materials. 2020; 13(15):3350. https://doi.org/10.3390/ma13153350
Chicago/Turabian StyleCervino, Gabriele, Marco Cicciù, Alan Scott Herford, Antonino Germanà, and Luca Fiorillo. 2020. "Biological and Chemo-Physical Features of Denture Resins" Materials 13, no. 15: 3350. https://doi.org/10.3390/ma13153350
APA StyleCervino, G., Cicciù, M., Herford, A. S., Germanà, A., & Fiorillo, L. (2020). Biological and Chemo-Physical Features of Denture Resins. Materials, 13(15), 3350. https://doi.org/10.3390/ma13153350









