Polydopamine Linking Substrate for AMPs: Characterisation and Stability on Ti6Al4V
Abstract
:1. Introduction
2. Materials and Methods
2.1. Peptide Design
2.2. Peptide Synthesis, Purification
2.3. Peptide Characterisation
2.3.1. High-Pressure Liquid Chromatography
2.3.2. Mass Spectrometry
2.3.3. Minimum Inhibitory Concentration (MIC) Values of Peptides
2.4. Sample Preparation
2.5. Topography of Coating
2.6. Fluorescence Microscopy
2.7. Scanning Electron Microscopy
2.8. Coating Stability
2.9. Dynamic Contact Angle Analysis
2.10. Cell Culture Studies
3. Results
3.1. Antimicrobial Characterisation
3.2. Polymerisation of Dopamine
3.3. Fluorescence Microscopy
3.4. Peptide Release Studies
3.5. Wettability of the Surface
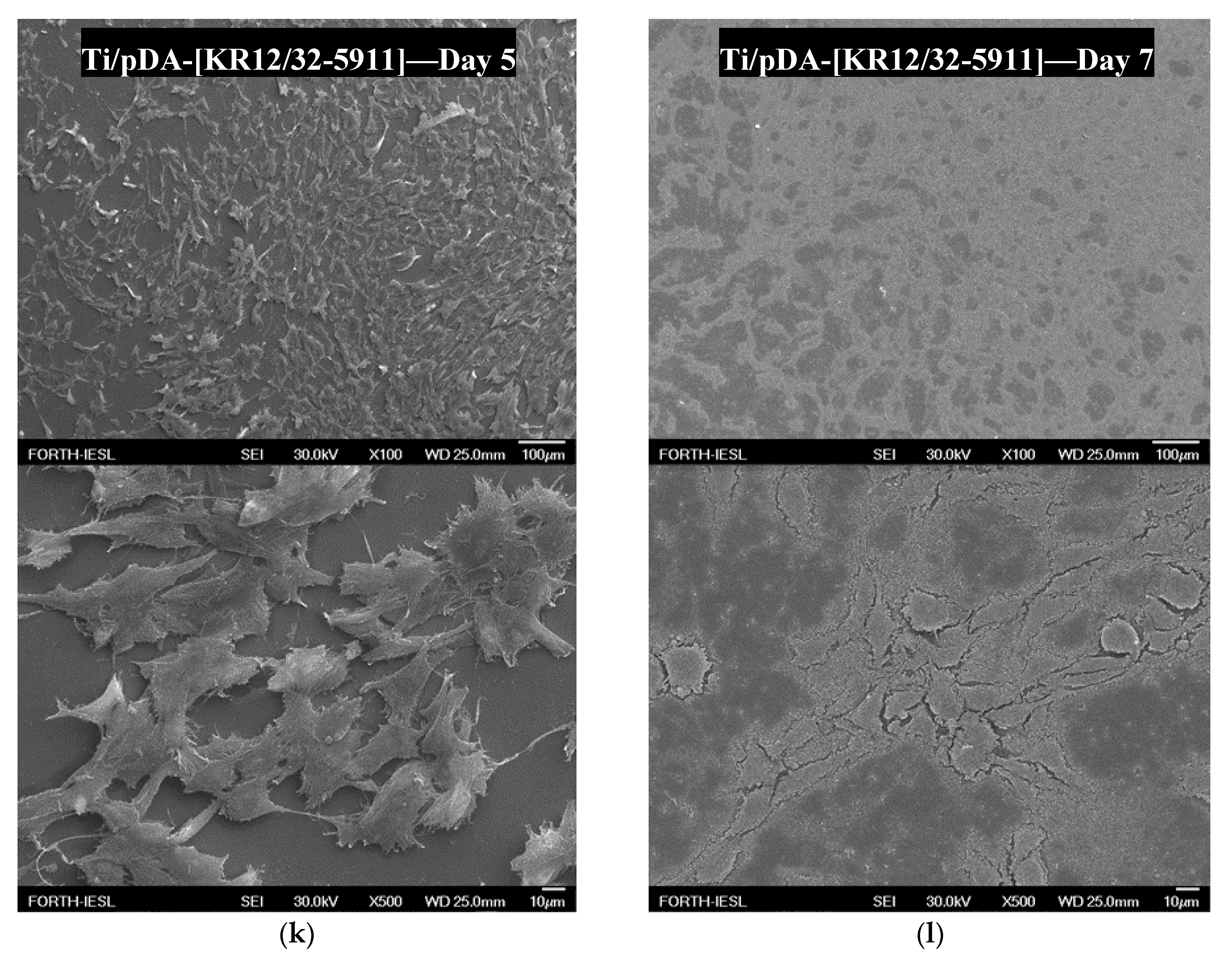
3.6. Cell Studies
4. Discussion
4.1. Peptide MIC Characterisation
4.2. Polydopamine Coating of Ti6Al4V
4.3. Peptide Attachment to Polydopamine
4.4. Wettability of the Surface
4.5. Cell Culture Studies
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Cloutier, M.; Mantovani, D.; Rosei, F. Antibacterial Coatings: Challenges, Perspectives, and Opportunities. Trends Biotechnol. 2015, 33, 637–652. [Google Scholar] [CrossRef]
- Goodman, S.B.; Yao, Z.; Keeney, M.; Yang, F. The future of biologic coatings for orthopaedic implants. Biomaterials 2013, 34, 3174–3183. [Google Scholar] [CrossRef] [Green Version]
- Romanò, C.L.; Scarponi, S.; Gallazzi, E.; Romanò, D.; Drago, L. Antibacterial coating of implants in orthopaedics and trauma: A classification proposal in an evolving panorama. J. Orthop. Surg. Res. 2015, 10, 157. [Google Scholar] [CrossRef] [Green Version]
- Geetha, M.; Singh, A.K.; Asokamani, R.; Gogia, K.A. Ti based biomaterials, the ultimate choice for orthopaedic implants—A review. Prog. Mater. Sci. 2009, 54, 397–425. [Google Scholar] [CrossRef]
- Bauer, J.; Siala, W.; Tulkens, P.M.; Van Bambeke, F. A combined pharmacodynamic quantitative and qualitative model reveals the potent activity of daptomycin and delafloxacin against Staphylococcus aureus biofilms. Antimicrob. Agents Chemother. 2013, 57, 2726–2737. [Google Scholar] [CrossRef] [Green Version]
- Mishra, B.; Wang, G. Titanium surfaces immobilised with the major antimicrobial fragment FK-16 of human cathelicidin LL-37 are potent against multiple antibiotic-resistant bacteria. Biofouling 2017, 33, 544–555. [Google Scholar] [CrossRef] [PubMed]
- Stigter, M.; Bezemer, J.; De Groot, K.; Layrolle, P. Incorporation of different antibiotics into carbonated hydroxyapatite coatings on titanium implants, release and antibiotic efficacy. J. Control. Release 2004, 99, 127–137. [Google Scholar] [CrossRef]
- Rathbone, C.R.; Cross, J.D.; Brown, K.V.; Murray, C.; Wenke, J.C. Effect of various concentrations of antibiotics on osteogenic cell viability and activity. J. Orthop. Res. 2011, 29, 1070–1074. [Google Scholar] [CrossRef]
- Mor, A. Peptide-based antibiotics: A potential answer to raging antimicrobial resistance. Drug Dev. Res. 2000, 50, 440–447. [Google Scholar] [CrossRef]
- Alves, D.; Olívia Pereira, M. Mini-review: Antimicrobial peptides and enzymes as promising candidates to functionalise biomaterial surfaces. Biofouling 2014, 30, 483–499. [Google Scholar] [CrossRef]
- Bazaka, K.; Jacob, M.V.; Chrzanowski, W.; Ostrikov, K. Anti-bacterial surfaces: Natural agents, mechanisms of action, and plasma surface modification. RSC Adv. 2015, 5, 48739–48759. [Google Scholar] [CrossRef] [Green Version]
- Zasloff, M. Antimicrobial peptides of multicellular organisms. Nature 2002, 415, 389–395. [Google Scholar] [CrossRef] [PubMed]
- Guilhelmelli, F.; Vilela, N.; Albuquerque, P.; Derengowski, L.D.S.; Pereira, I.S.; Kyaw, C.M. Antibiotic development challenges: The various mechanisms of action of antimicrobial peptides and of bacterial resistance. Front. Microbiol. 2013, 4, 353. [Google Scholar] [CrossRef] [Green Version]
- Fjell, C.D.; Hiss, J.A.; Hancock, R.E.W.; Schneider, G. Designing antimicrobial peptides: Form follows function. Nat. Rev. Drug Discov. 2011, 11, 37–51. [Google Scholar] [CrossRef]
- Lazzaro, B.P.; Zasloff, M.; Rolff, J. Antimicrobial peptides: Application informed by evolution. Science 2020, 368, eaau5480. [Google Scholar] [CrossRef]
- Jacob, B.; Park, I.-S.; Bang, J.-K.; Shin, S.Y. Short KR-12 analogs designed from human cathelicidin LL-37 possessing both antimicrobial and antiendotoxic activities without mammalian cell toxicity. J. Pept. Sci. 2013, 19, 700–707. [Google Scholar] [CrossRef]
- Jia, L.; Han, F.; Wang, H.; Zhu, C.; Guo, Q.; Li, J.; Zhao, Z.; Zhang, Q.; Zhu, X.; Li, B. Polydopamine-assisted surface modification for orthopaedic implants. J. Orthop. Transl. 2019, 17, 82–95. [Google Scholar] [CrossRef]
- Zhu, Y.; Liu, D.; Wang, X.; He, Y.; Luan, W.; Qi, F.; Ding, J. Polydopamine-mediated covalent functionalisation of collagen on a titanium alloy to promote biocompatibility with soft tissues J. Mater. Chem. B 2019, 7, 2019–2031. [Google Scholar] [CrossRef]
- Wang, Y.; Qi, H.; Miron, R.J.; Zhang, Y. Modulating macrophage polarisation on titanium implant surface by poly(dopamine)-assisted immobilisation of IL4. Clin. Implant Dent. Relat. Res. 2019, 21, 977–986. [Google Scholar] [CrossRef]
- Kokubo, T.; Takadama, H. How useful is SBF in predicting in vivo bone bioactivity? Biomaterials 2006, 27, 2907–2915. [Google Scholar] [CrossRef]
- Ribeiro, M.; Monteiro, F.J.; Ferraz, M.P. Infection of orthopedic implants with emphasis on bacterial adhesion process and techniques used in studying bacterial-material interactions. Biomaterials 2013, 2, 176–194. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Levison, M.E.; Levison, J.H. Pharmacokinetics and Pharmacodynamics of Antibacterial Agents. Infect. Dis. Clin. N. A. 2009, 23, 791–815. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wong, J.H.; Łęgowska, A.; Rolka, K.; Ng, T.B.; Hui, M.; Cho, C.H.; Lam, W.W.L.; Au, S.W.-N.; Gu, O.W.; Wan, D.C.C. Effects of cathelicidin and its fragments on three key enzymes of HIV-1. Peptides 2011, 32, 1117–1122. [Google Scholar] [CrossRef]
- Overhage, J.; Campisano, A.; Bains, M.; Torfs, E.C.W.; Rehm, B.H.A.; Hancock, R.E.W. Human Host Defense Peptide LL-37 Prevents Bacterial Biofilm Formation. Infect. Immun. 2008, 76, 4176–4182. [Google Scholar] [CrossRef] [Green Version]
- Barlow, P.G.; Svoboda, P.; Mackellar, A.; Nash, A.A.; York, I.A.; Pohl, J.; Davidson, D.J.; Donis, R.O. Antiviral Activity and Increased Host Defense against Influenza Infection Elicited by the Human Cathelicidin LL-37. PLoS ONE 2011, 6, e25333. [Google Scholar] [CrossRef]
- Davidson, D.J.; Currie, A.J.; Reid, G.S.D.; Bowdish, D.M.E.; MacDonald, K.L.; Ma, R.C.; Hancock, R.E.W.; Speert, D.P. The Cationic Antimicrobial Peptide LL-37 Modulates Dendritic Cell Differentiation and Dendritic Cell-Induced T Cell Polarization. J. Immunol. 2004, 172, 1146–1156. [Google Scholar] [CrossRef] [Green Version]
- Koczulla, R.; Von Degenfeld, G.; Kupatt, C.; Krötz, F.; Zahler, S.; Gloe, T.; Issbrücker, K.; Unterberger, P.; Zaiou, M.; Lebherz, C.; et al. An angiogenic role for the human peptide antibiotic LL-37/hCAP-18. J. Clin. Investig. 2003, 111, 1665–1672. [Google Scholar] [CrossRef]
- Duplantier, A.J.; Van Hoek, M.L. The Human Cathelicidin Antimicrobial Peptide LL-37 as a Potential Treatment for Polymicrobial Infected Wounds. Front. Immunol. 2013, 4, 1–14. [Google Scholar] [CrossRef] [Green Version]
- Dutta, D.; Kumar, N.; Willcox, M.D.P. Antimicrobial activity of four cationic peptides immobilised to poly-hydroxyethylmethacrylate. Biofouling 2016, 32, 429–438. [Google Scholar] [CrossRef]
- Alfieri, M.L.; Panzella, L.; Oscurato, S.L.; Salvatore, M.; Avolio, R.; Errico, M.E.; Maddalena, P.M.; Napolitano, A.; D’Ischia, M. The Chemistry of Polydopamine Film Formation: The Amine-Quinone Interplay. Biomimetics 2018, 3, 26. [Google Scholar] [CrossRef] [Green Version]
- Kim, J.H.; Lee, M.; Park, C.B. Polydopamine as a Biomimetic Electron Gate for Artificial Photosynthesis. Angew. Chem. Int. Ed. 2014, 53, 6364–6368. [Google Scholar] [CrossRef] [PubMed]
- Dreyer, D.R.; Miller, D.J.; Freeman, B.D.; Paul, D.R.; Bielawski, C.W. Perspectives on poly(dopamine). Chem. Sci. 2013, 4, 3796. [Google Scholar] [CrossRef]
- Lee, H.; Dellatore, S.M.; Miller, W.M.; Messersmith, P.B. Mussel-Inspired Surface Chemistry for Multifunctional Coatings. Science 2007, 318, 426–430. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jiang, J.; Zhu, L.; Zhu, L.; Zhu, B.; Xu, Y. Surface Characteristics of a Self-Polymerised Dopamine Coating Deposited on Hydrophobic Polymer Films. Langmuir 2011, 27, 14180–14187. [Google Scholar] [CrossRef] [PubMed]
- Zhang, W.; Yang, F.K.; Han, Y.; Gaikwad, R.; Leonenko, Z.; Zhao, B. Surface and Tribological Behaviors of the Bioinspired Polydopamine Thin Films under Dry and Wet Conditions. Biomacromolecules 2013, 14, 394–405. [Google Scholar] [CrossRef] [PubMed]
- Bernsmann, F.; Ponche, A.; Ringwald, C.; Hemmerle, J.; Raya, J.; Bechinger, B.; Voegel, J.C.; Schaaf, P.; Ball, V. Characterisation of Dopamine−Melanin Growth on Silicon Oxide. J. Phys. Chem. C 2009, 113, 8234–8242. [Google Scholar] [CrossRef]
- Lynge, M.E.; Van Der Westen, R.; Postma, A.; Städler, B. Polydopamine-a nature-inspired polymer coating for biomedical science. Nanoscale 2011, 3, 4916. [Google Scholar] [CrossRef]
- Shin, Y.M.; Jun, I.; Lee, J.Y.; Rhim, T.; Shin, H. Bio-inspired Immobilization of Cell-Adhesive Ligands on Electrospun Nanofibrous Patches for Cell Delivery. Macromol. Mater. Eng. 2012, 298, 555–564. [Google Scholar] [CrossRef]
- Li, H.; Cui, D.; Cai, H.; Zhang, L.; Chen, X.; Sun, J.; Chao, Y. Use of surface plasmon resonance to investigate lateral wall deposition kinetics and properties of polydopamine films. Biosens. Bioelectron. 2013, 41, 809–814. [Google Scholar] [CrossRef]
- Lee, H.J.; Koo, A.N.; Lee, S.W.; Lee, M.H.; Lee, S.C. Catechol-functionalised adhesive polymer nanoparticles for controlled local release of bone morphogenetic protein-2 from titanium surface. J. Control. Release 2013, 170, 198–208. [Google Scholar] [CrossRef]
- Ku, S.H.; Ryu, J.; Hong, S.K.; Lee, H.; Park, C.B. General functionalisation route for cell adhesion on non-wetting surfaces. Biomaterials 2010, 31, 2535–2541. [Google Scholar] [CrossRef] [PubMed]
- Ponsonnet, L.; Reybier, K.; Jaffrezic, N.; Comte, V.; Lagneau, C.; Lissac, M.; Martelet, C. Relationship between surface properties (roughness, wettability) of titanium and titanium alloys and cell behaviour. Mater. Sci. Eng. C 2003, 23, 551–560. [Google Scholar] [CrossRef]
- Nijhuis, A.W.G.; Van den Beucken, J.J.J.P.; Boerman, O.C.; Jansen, J.A.; Leeuwenburgh, S.C.G. 1-Step Versus 2-Step Immobilisation of Alkaline Phosphatase and Bone Morphogenetic Protein-2 onto Implant Surfaces Using Polydopamine. Tissue Eng. Part C Methods 2013, 19, 610–619. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liu, X.; Chu, P.K.; Ding, C. Surface modification of titanium, titanium alloys, and related materials for biomedical applications. Mater. Sci. Eng. R Rep. 2004, 47, 49–121. [Google Scholar] [CrossRef] [Green Version]
- Luo, R.; Tang, L.; Zhong, S.; Yang, Z.; Wang, J.; Weng, Y.; Tu, Q.; Jiang, C.; Huang, N. In Vitro Investigation of Enhanced Hemocompatibility and Endothelial Cell Proliferation Associated with Quinone-Rich Polydopamine Coating. ACS Appl. Mater. Interfaces 2013, 5, 1704–1714. [Google Scholar] [CrossRef]
- Jun, I.-K.; Jang, J.-H.; Kim, H.-W.; Kim, H.-E. Recombinant osteopontin fragment coating on hydroxyapatite for enhanced osteoblast-like cell responses. J. Mater. Sci. 2005, 40, 2891–2895. [Google Scholar] [CrossRef]











| Peptide | Sequence | Length of Sequence | Net Charge | Charge Density | Mean Hydrophobicity [H] | Helical Hydrophobic |
|---|---|---|---|---|---|---|
| KR12 | KRIVQRIKDFLR | 12 aa | +4 | 0.33 | 0.193 | 0.782 |
| KR12/32 | KIRVQRIKDFLR | 12 aa | +4 | 0.33 | 0.193 | 0.429 |
| KR12-5911 | KRIVRIKFR | 9 aa | +5 | 0.56 | 0.178 | 0.395 |
| KR12/32-5911 | KIRVRIKFR | 9 aa | +5 | 0.56 | 0.178 | 0.092 |
| Peptide | Theoretical Molecular Weight (g/mol) | Molecular Weight M Measured by MS (g/mol) | Purity Calculated by HPLC (%) |
|---|---|---|---|
| KR12 | 1572 | M = 1574 [M + 2H]2+ = 788 [M + Na + H]2+ = 799 | 95 |
| 5(6)-FAM-labelled KR12 | 1904 | M = 1903 [M + 2H]2+ = 952 | 95 |
| KR12/32 | 1572 | M = 1572 [M + 2H]2+ = 787 [M + 3H]3+ = 525 | 99 |
| 5(6)-FAM-labelled KR12/32 | 1904 | M = 1903 [M + H]+ = 1904 [M + 2H]2+ = 952 | 95 |
| KR12-5911 | 1216 | M = 1215 [M + 2H]2+ = 609 | 97 |
| 5(6)-FAM-labelled KR12-5911 | 1548 | M = 1547 [M + H]+ = 1549 [M + 2H]2+ = 775 | 95 |
| KR12/32-5911 | 1216 | M = 1215 [M + 2H]2+ = 609 | 98 |
| 5(6)-FAM-labelled KR12/32-5911 | 1548 | M = 1547 [M + 2H]2+ = 775 | 96 |
| KR12 | 1572 | M = 1574 [M + 2H]2+ = 788 [M + Na + H]2+ = 799 | 95 |
| 5(6)-FAM-labelled KR12 | 1904 | M = 1903 [M + 2H]2+ = 952 | 95 |
| Sequence | MIC Values (μM) | |||
|---|---|---|---|---|
| E. coli (I364) | P. aeruginosa (PAO1) | S. aureus (F77) | Geometric Mean | |
| KR12 | 2 | 2 | 8 | 4.0 |
| KR12/32 | 4 | 4 | 32 | 13.33 |
| KR12-5911 | 0.5 | 2 | 8 | 3.5 |
| KR12/32-5911 | 4 | 4 | 2 | 3.33 |
| LL-37 [14] | 8 | 8 | 4 | 6.67 |
| Time of Immersion | 24 h | 48 h | 72 h | 96 h |
|---|---|---|---|---|
| Coating thickness measured by ellipsometry (nm) | 10.2 ± 1.1 | 32.8 ± 1.1 | 52.4 ± 7.0 | 54.7 ± 6.4 |
| Coating thickness measured by AFM (nm) | 10.3 ± 0.5 | 34.1 ± 2.0 | 55.4 ± 9.0 | 57.1 ± 6.8 |
| 5(6)-FAM-KR12 | pDA-5(6)-FAM-KR12 | pDA-5(6)-FAM-KR12/32 | pDA-5(6)-FAM-KR12-5911 | pDA-5(6)-FAM-KR12/32-5911 | |
|---|---|---|---|---|---|
| Fluorescence intensity (FI) | 868 ± 144 | 1204 ± 37 | 1198 ± 44 | 1227 ± 42 | 1189 ± 52 |
| Surface | Contact Angle at Steady Volume of the Droplet |
|---|---|
| Mirror polished Ti6Al4V | 65.4° ± 1.6 |
| Ti6Al4V coated with pDA | 59.0° ± 1.2 |
| Ti6Al4V coated with pDA and peptide KR12 | 57.7° ± 0.9 |
| Ti6Al4V coated with pDA and peptide KR12/32 | 57.5° ± 0.7 |
| Ti6Al4V coated with pDA and peptide KR12-5911 | 55.6° ± 1.1 |
| Ti6Al4V coated with pDA and peptide KR12/32-5911 | 56.3° ± 0.5 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Trzcińska, Z.; Bruggeman, M.; Ijakipour, H.; Hodges, N.J.; Bowen, J.; Stamboulis, A. Polydopamine Linking Substrate for AMPs: Characterisation and Stability on Ti6Al4V. Materials 2020, 13, 3714. https://doi.org/10.3390/ma13173714
Trzcińska Z, Bruggeman M, Ijakipour H, Hodges NJ, Bowen J, Stamboulis A. Polydopamine Linking Substrate for AMPs: Characterisation and Stability on Ti6Al4V. Materials. 2020; 13(17):3714. https://doi.org/10.3390/ma13173714
Chicago/Turabian StyleTrzcińska, Zuzanna, Marc Bruggeman, Hanieh Ijakipour, Nikolas J. Hodges, James Bowen, and Artemis Stamboulis. 2020. "Polydopamine Linking Substrate for AMPs: Characterisation and Stability on Ti6Al4V" Materials 13, no. 17: 3714. https://doi.org/10.3390/ma13173714
APA StyleTrzcińska, Z., Bruggeman, M., Ijakipour, H., Hodges, N. J., Bowen, J., & Stamboulis, A. (2020). Polydopamine Linking Substrate for AMPs: Characterisation and Stability on Ti6Al4V. Materials, 13(17), 3714. https://doi.org/10.3390/ma13173714







