Margin Integrity of Bulk-Fill Composite Restorations in Primary Teeth
Abstract
1. Introduction
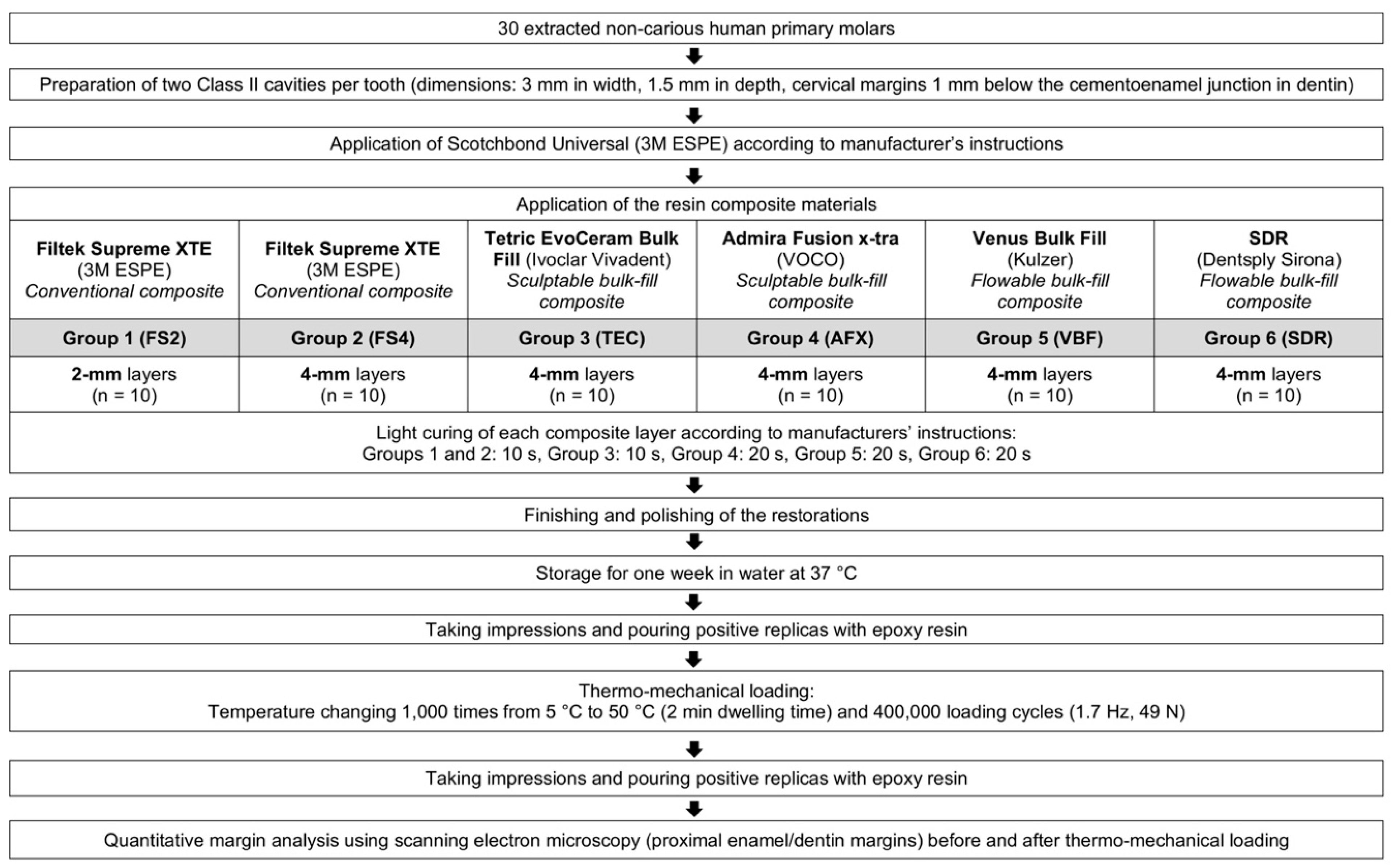
2. Materials and Methods
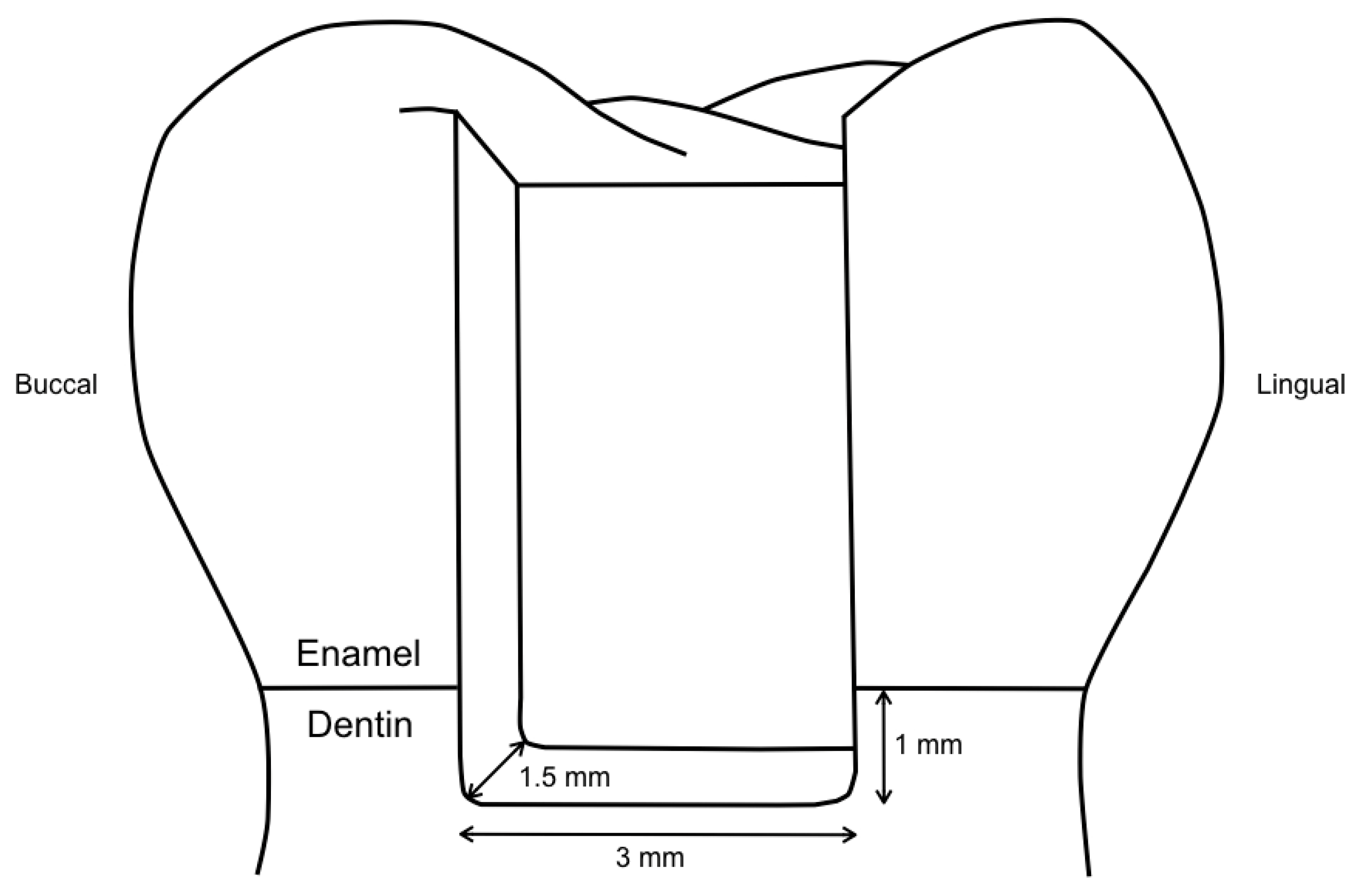
2.1. Specimen Preparation
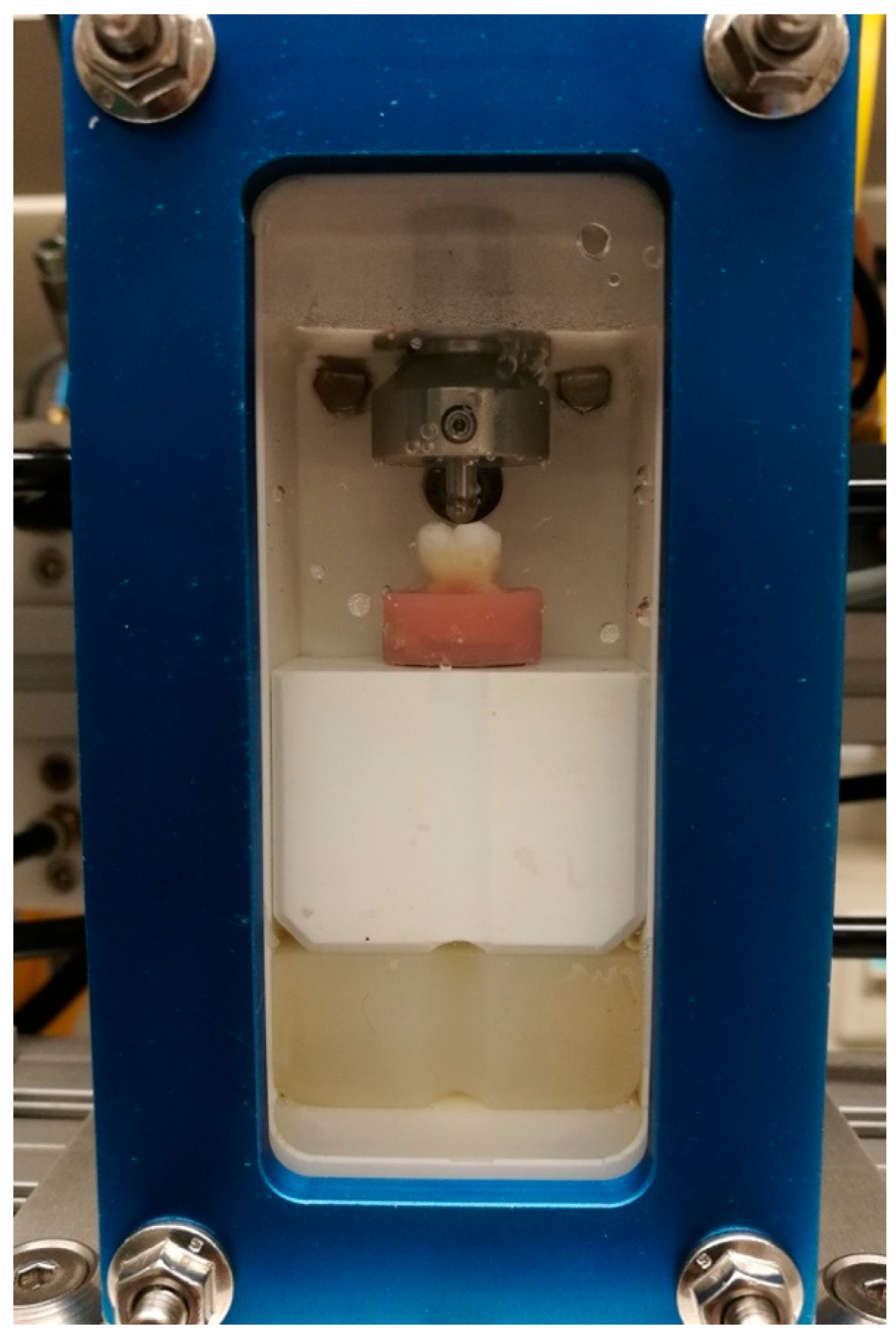
2.2. Thermo-Mechanical Loading
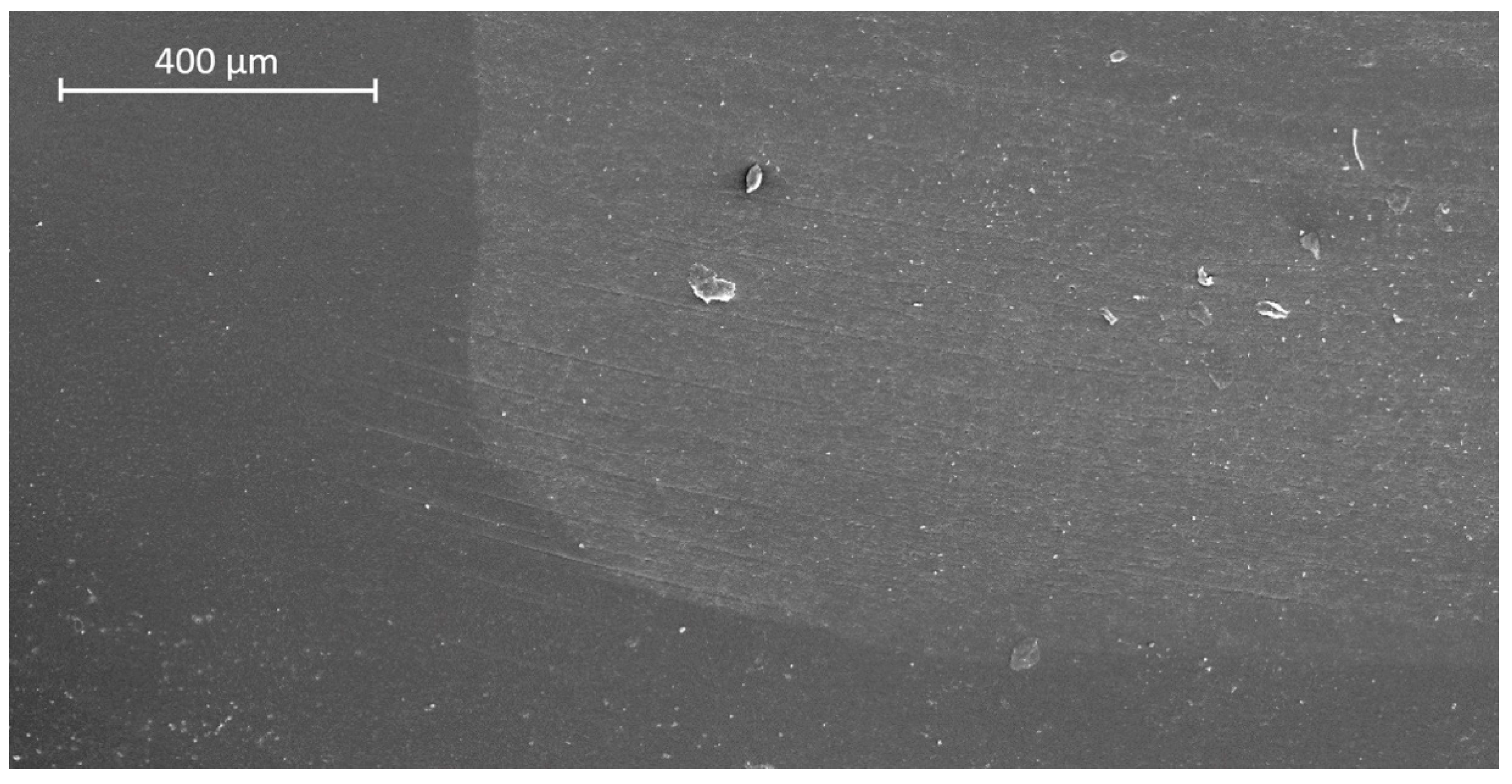
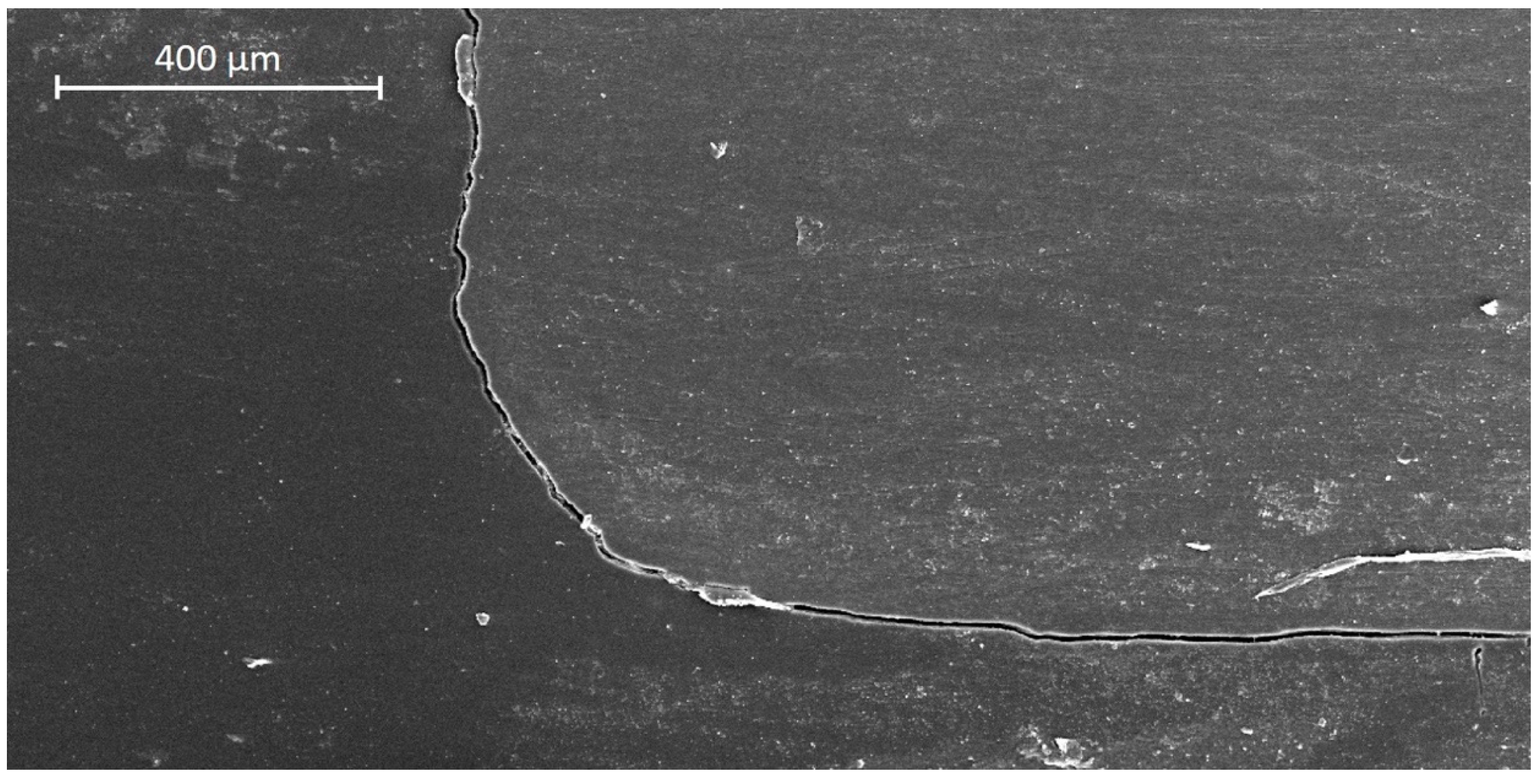
2.3. Assessment of Margin Integrity
2.4. Statistical Analysis
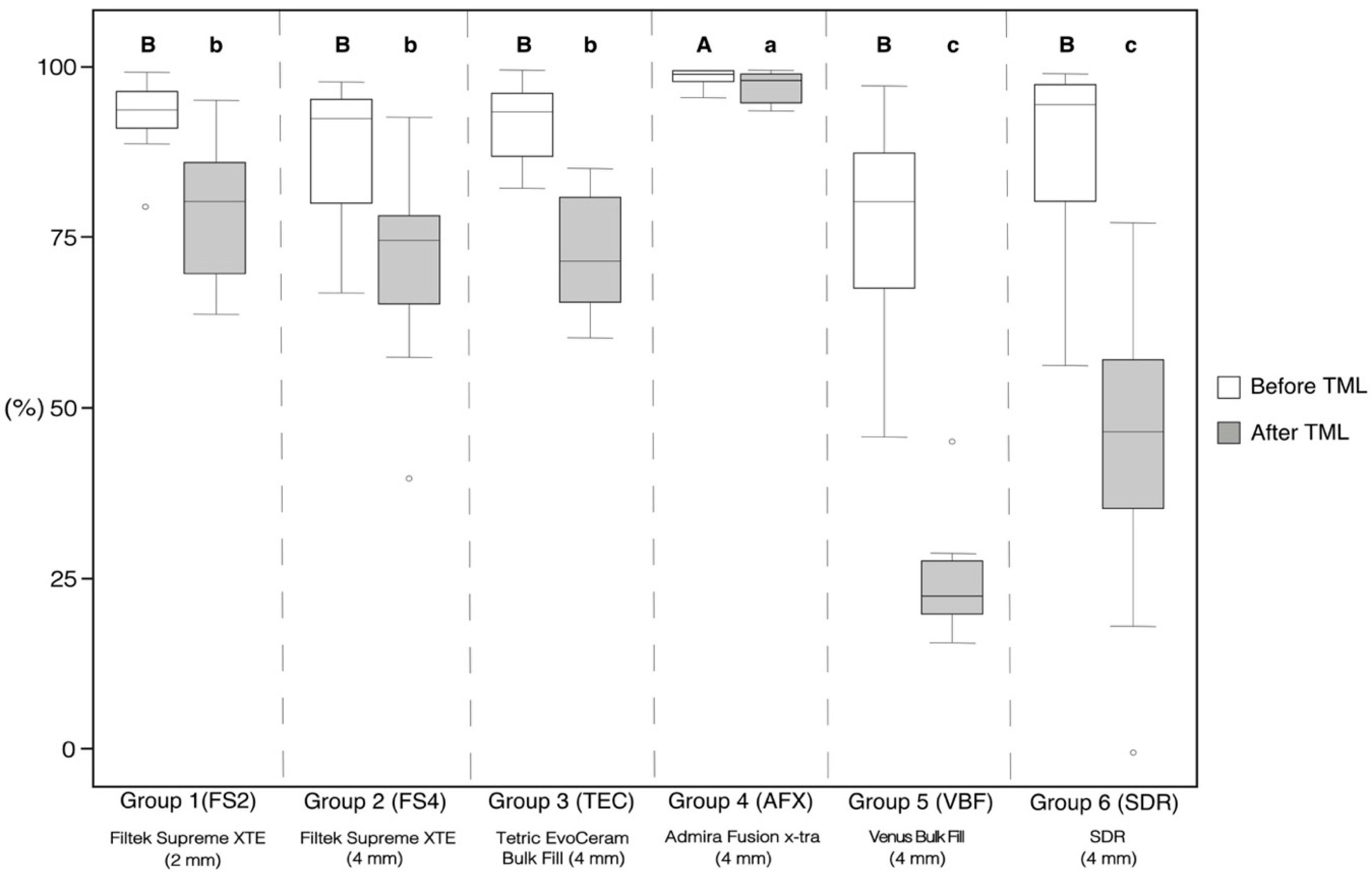
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Lazaridou, D.; Belli, R.; Krämer, N.; Petschelt, A.; Lohbauer, U. Dental materials for primary dentition: Are they suitable for occlusal restorations? A two-body wear study. Eur. Arch. Paediatr. Dent. 2015, 16, 165–172. [Google Scholar] [CrossRef] [PubMed]
- Chisini, L.A.; Collares, K.; Cademartori, M.G.; de Oliveira, L.J.C.; Conde, M.C.M.; Demarco, F.F.; Corrêa, M.B. Restorations in primary teeth: A systematic review on survival and reasons for failures. Int. J. Paediatr. Dent. 2018, 28, 123–139. [Google Scholar] [CrossRef] [PubMed]
- Davidson, C.L.; Feilzer, A.J. Polymerization shrinkage and polymerization shrinkage stress in polymer-based restoratives. J. Dent. 1997, 25, 435–440. [Google Scholar] [CrossRef]
- Carvalho, R.M.; Pereira, J.C.; Yoshiyama, M.; Pashley, D.H. A review of polymerization contraction: The influence of stress development versus stress relief. Oper. Dent. 1996, 21, 17–24. [Google Scholar] [PubMed]
- Peutzfeldt, A.; Asmussen, E. Determinants of in vitro gap formation of resin composites. J. Dent. 2004, 32, 109–115. [Google Scholar] [CrossRef]
- Park, J.; Chang, J.; Ferracane, J.; Lee, I.B. How should composite be layered to reduce shrinkage stress: Incremental or bulk filling? Dent. Mater. 2008, 24, 1501–1505. [Google Scholar] [CrossRef] [PubMed]
- Tauböck, T.T.; Feilzer, A.J.; Buchalla, W.; Kleverlaan, C.J.; Krejci, I.; Attin, T. Effect of modulated photo-activation on polymerization shrinkage behavior of dental restorative resin composites. Eur. J. Oral Sci. 2014, 122, 293–302. [Google Scholar] [CrossRef]
- Tarle, Z.; Attin, T.; Marovic, D.; Andermatt, L.; Ristic, M.; Tauböck, T.T. Influence of irradiation time on subsurface degree of conversion and microhardness of high-viscosity bulk-fill resin composites. Clin. Oral Investig. 2015, 19, 831–840. [Google Scholar] [CrossRef]
- Alrahlah, A.; Silikas, N.; Watts, D.C. Post-cure depth of cure of bulk fill dental resin-composites. Dent. Mater. 2014, 30, 149–154. [Google Scholar] [CrossRef]
- Tauböck, T.T.; Marovic, D.; Zeljezic, D.; Steingruber, A.D.; Attin, T.; Tarle, Z. Genotoxic potential of dental bulk-fill resin composites. Dent. Mater. 2017, 33, 788–795. [Google Scholar] [CrossRef]
- Dieckmann, P.; Mohn, D.; Zehnder, M.; Attin, T.; Tauböck, T.T. Light transmittance and polymerization of bulk-fill composite materials doped with bioactive micro-fillers. Materials 2019, 12, 4087. [Google Scholar] [CrossRef] [PubMed]
- Ilie, N.; Hickel, R. Investigations on a methacrylate-based flowable composite based on the SDR technology. Dent. Mater. 2011, 27, 348–355. [Google Scholar] [CrossRef] [PubMed]
- Marovic, D.; Tauböck, T.T.; Attin, T.; Panduric, V.; Tarle, Z. Monomer conversion and shrinkage force kinetics of low-viscosity bulk-fill resin composites. Acta Odontol. Scand. 2015, 73, 474–480. [Google Scholar] [CrossRef] [PubMed]
- Tauböck, T.T.; Jäger, F.; Attin, T. Polymerization shrinkage and shrinkage force kinetics of high- and low-viscosity dimethacrylate- and ormocer-based bulk-fill resin composites. Odontology 2019, 107, 103–110. [Google Scholar] [CrossRef]
- Moorthy, A.; Hogg, C.H.; Dowling, A.H.; Grufferty, B.F.; Benetti, A.R.; Fleming, G.J. Cuspal deflection and microleakage in premolar teeth restored with bulk-fill flowable resin-based composite base materials. J. Dent. 2012, 40, 500–505. [Google Scholar] [CrossRef]
- Politi, I.; McHugh, L.E.J.; Al-Fodeh, R.S.; Fleming, G.J.P. Modification of the restoration protocol for resin-based composite (RBC) restoratives (conventional and bulk fill) on cuspal movement and microleakage score in molar teeth. Dent. Mater. 2018, 34, 1271–1277. [Google Scholar] [CrossRef]
- Roggendorf, M.J.; Kramer, N.; Appelt, A.; Naumann, M.; Frankenberger, R. Marginal quality of flowable 4-mm base vs. conventionally layered resin composite. J. Dent. 2011, 39, 643–647. [Google Scholar] [CrossRef]
- De Assis, F.S.; Lima, S.N.; Tonetto, M.R.; Bhandi, S.H.; Pinto, S.C.; Malaquias, P.; Loguercio, A.D.; Bandéca, M.C. Evaluation of bond strength, marginal integrity, and fracture strength of bulk- vs. incrementally-filled restorations. J. Adhes. Dent. 2016, 18, 317–323. [Google Scholar]
- Heintze, S.D.; Monreal, D.; Peschke, A. Marginal quality of Class II composite restorations placed in bulk compared to an incremental technique: Evaluation with SEM and stereomicroscope. J. Adhes. Dent. 2015, 17, 147–154. [Google Scholar]
- Van Dijken, J.W.V.; Pallesen, U. Bulk-filled posterior resin restorations based on stress-decreasing resin technology: A randomized, controlled 6-year evaluation. Eur. J. Oral Sci. 2017, 125, 303–309. [Google Scholar] [CrossRef]
- Heck, K.; Manhart, J.; Hickel, R.; Diegritz, C. Clinical evaluation of the bulk fill composite QuiXfil in molar class I and II cavities: 10-year results of a RCT. Dent. Mater. 2018, 34, e138–e147. [Google Scholar] [CrossRef] [PubMed]
- Veloso, S.R.M.; Lemos, C.A.A.; de Moraes, S.L.D.; do Egito Vasconcelos, B.C.; Pellizzer, E.P.; de Melo Monteiro, G.Q. Clinical performance of bulk-fill and conventional resin composite restorations in posterior teeth: A systematic review and meta-analysis. Clin. Oral Investig. 2019, 23, 221–233. [Google Scholar] [CrossRef] [PubMed]
- García Marí, L.; Climent Gil, A.; LLena Puy, C. In vitro evaluation of microleakage in Class II composite restorations: High-viscosity bulk-fill vs. conventional composites. Dent. Mater. J. 2019, 38, 721–727. [Google Scholar] [CrossRef] [PubMed]
- Patel, M.C.; Bhatt, R.K.; Makwani, D.A.; Dave, L.D.; Raj, V.S. Comparative evaluation of marginal seal integrity of three bulk-fill composite materials in Class II cavities: An in vitro study. Adv. Hum. Biol. 2018, 8, 201–205. [Google Scholar]
- Eltoum, N.A.; Bakry, N.S.; Talaat, D.M.; Elshabrawy, S.M. Microleakage evaluation of bulk-fill composite in class II restorations of primary molars. Alex. Dent. J. 2019, 44, 111–116. [Google Scholar] [CrossRef]
- Krejci, I.; Reich, T.; Lutz, F.; Albertoni, M. An in vitro test procedure for evaluating dental restoration systems. 1. A computer-controlled mastication simulator. Schweiz. Monatsschr. Zahnmed. 1990, 100, 953–960. [Google Scholar]
- Krejci, I.; Planinic, M.; Stavridakis, M.; Bouillaguet, S. Resin composite shrinkage and marginal adaptation with different pulse-delay light curing protocols. Eur. J. Oral Sci. 2005, 113, 531–536. [Google Scholar] [CrossRef]
- Groddeck, S.; Attin, T.; Tauböck, T.T. Effect of cavity contamination by blood and hemostatic agents on marginal adaptation of composite restorations. J. Adhes. Dent. 2017, 19, 259–264. [Google Scholar]
- Frankenberger, R.; Hehn, J.; Hajtó, J.; Krämer, N.; Naumann, M.; Koch, A.; Roggendorf, M.J. Effect of proximal box elevation with resin composite on marginal quality of ceramic inlays in vitro. Clin. Oral Investig. 2013, 17, 177–183. [Google Scholar] [CrossRef]
- Campos, E.A.; Ardu, S.; Lefever, D.; Jasse, F.F.; Bortolotto, T.; Krejci, I. Marginal adaptation of class II cavities restored with bulk-fill composites. J. Dent. 2014, 42, 575–581. [Google Scholar] [CrossRef]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2015; Available online: https://www.R-project.org/ (accessed on 6 March 2020).
- Wickham, H. ggplot2: Elegant Graphics for Data Analysis; Springer-Verlag: New York, NY, USA, 2016. [Google Scholar]
- Wagner, A.; Wendler, M.; Petschelt, A.; Belli, R.; Lohbauer, U. Bonding performance of universal adhesives in different etching modes. J. Dent. 2014, 42, 800–807. [Google Scholar] [CrossRef] [PubMed]
- Fu, J.; Saikaew, P.; Kawano, S.; Carvalho, R.M.; Hannig, M.; Sano, H.; Selimovic, D. Effect of air-blowing duration on the bond strength of current one-step adhesives to dentin. Dent. Mater. 2017, 33, 895–903. [Google Scholar] [CrossRef] [PubMed]
- Michelotti, G.; Niedzwiecki, M.; Bidjan, D.; Dieckmann, P.; Deari, S.; Attin, T.; Tauböck, T.T. Silane effect of universal adhesive on the composite–composite repair bond strength after different surface pretreatments. Polymers 2020, 12, 950. [Google Scholar] [CrossRef] [PubMed]
- Lawson, N.C.; Robles, A.; Fu, C.C.; Lin, C.P.; Sawlani, K.; Burgess, J.O. Two-year clinical trial of a universal adhesive in total-etch and self-etch mode in non-carious cervical lesions. J. Dent. 2015, 43, 1229–1234. [Google Scholar] [CrossRef]
- Zanatta, R.F.; Silva, T.M.; Esper, M.; Bresciani, E.; Gonçalves, S.; Caneppele, T. Bonding performance of simplified adhesive systems in noncarious cervical lesions at 2-year follow-up: A double-blind randomized clinical trial. Oper. Dent. 2019, 44, 476–487. [Google Scholar] [CrossRef]
- Lenzi, T.L.; Pires, C.W.; Soares, F.Z.M.; Raggio, D.P.; Ardenghi, T.M.; de Oliveira Rocha, R. Performance of universal adhesive in primary molars after selective removal of carious tissue: An 18-month randomized clinical trial. Pediatr. Dent. 2017, 39, 371–376. [Google Scholar]
- Papadogiannis, D.; Dimitriadi, M.; Zafiropoulou, M.; Gaintantzopoulou, M.D.; Eliades, G. Universal adhesives: Setting characteristics and reactivity with dentin. Materials 2019, 12, 1720. [Google Scholar] [CrossRef]
- Wegehaupt, F.J.; Tauböck, T.T.; Attin, T. Durability of the anti-erosive effect of surfaces sealants under erosive abrasive conditions. Acta Odontol. Scand. 2013, 71, 1188–1194. [Google Scholar] [CrossRef]
- Leprince, J.G.; Palin, W.M.; Vanacker, J.; Sabbagh, J.; Devaux, J.; Leloup, G. Physico-mechanical characteristics of commercially available bulk-fill composites. J. Dent. 2014, 42, 993–1000. [Google Scholar] [CrossRef]
- Wegehaupt, F.J.; Tauböck, T.T.; Attin, T.; Belibasakis, G.N. Influence of light-curing mode on the cytotoxicity of resin-based surface sealants. BMC Oral Health 2014, 14, 48. [Google Scholar] [CrossRef][Green Version]
- Wiegand, A.; Credé, A.; Tschammler, C.; Attin, T.; Tauböck, T.T. Enamel wear by antagonistic restorative materials under erosive conditions. Clin. Oral Investig. 2017, 21, 2689–2693. [Google Scholar] [CrossRef] [PubMed]
- Par, M.; Spanovic, N.; Tauböck, T.T.; Attin, T.; Tarle, Z. Degree of conversion of experimental resin composites containing bioactive glass 45S5: The effect of post-cure heating. Sci. Rep. 2019, 9, 17245. [Google Scholar] [CrossRef] [PubMed]
- Totiam, P.; Gonzalez-Cabezas, C.; Fontana, M.R.; Zero, D.T. A new in vitro model to study the relationship of gap size and secondary caries. Caries Res. 2007, 41, 467–473. [Google Scholar] [CrossRef] [PubMed]
- Aggarwal, V.; Logani, A.; Jain, V.; Shah, N. Effect of cyclic loading on marginal adaptation and bond strength in direct vs. indirect class II MO composite restorations. Oper. Dent. 2008, 33, 587–592. [Google Scholar] [CrossRef] [PubMed]
- Correia, A.; Andrade, M.R.; Tribst, J.; Borges, A.; Caneppele, T. Influence of bulk-fill restoration on polymerization shrinkage stress and marginal gap formation in Class V restorations. Oper. Dent. 2020, 45, E207–E216. [Google Scholar] [CrossRef]
- Bucuta, S.; Ilie, N. Light transmittance and micro-mechanical properties of bulk fill vs. conventional resin based composites. Clin. Oral Investig. 2014, 18, 1991–2000. [Google Scholar] [CrossRef] [PubMed]
- Manhart, J.; Hickel, R. Bulk-fill-composites. Modern application technique of direct composites for posterior teeth. Swiss Dent. J. 2014, 124, 19–37. [Google Scholar]
- Wolter, H.; Storch, W.; Ott, H. New inorganic/organic copolymers (ORMOCERs) for dental applications. Mater. Res. Soc. Symp. Proc. 1994, 346, 143–149. [Google Scholar] [CrossRef]
- Pick, B.; Pelka, M.; Belli, R.; Braga, R.R.; Lohbauer, U. Tailoring of physical properties in highly filled experimental nanohybrid resin composites. Dent. Mater. 2011, 27, 664–669. [Google Scholar] [CrossRef]
- Sharma, S.; Padda, B.K.; Choudhary, V. Comparative evaluation of residual monomer content and polymerization shrinkage of a packable composite and an ormocer. J. Conserv. Dent. 2012, 15, 161–165. [Google Scholar] [CrossRef]
- Rullman, I.; Patyna, M.; Janssen, B.; Willershausen, B. Determination of polymerization shrinkage of different composites using a photoelastic method. Am. J. Dent. 2017, 30, 16–22. [Google Scholar] [PubMed]
- Lu, H.; Stansbury, J.W.; Bowman, C.N. Towards the elucidation of shrinkage stress development and relaxation in dental composites. Dent. Mater. 2004, 20, 979–986. [Google Scholar] [CrossRef] [PubMed]
- Ilie, N.; Bucuta, S.; Draenert, M. Bulk-fill resin-based composites: An in vitro assessment of their mechanical performance. Oper. Dent. 2013, 38, 618–625. [Google Scholar] [CrossRef] [PubMed]
- Par, M.; Marovic, D.; Attin, T.; Tarle, Z.; Tauböck, T.T. The effect of rapid high-intensity light-curing on micromechanical properties of bulk-fill and conventional resin composites. Sci. Rep. 2020, 10, 10560. [Google Scholar] [CrossRef] [PubMed]
- Ferracane, J.L. Hygroscopic and hydrolytic effects in dental polymer networks. Dent. Mater. 2006, 22, 211–222. [Google Scholar] [CrossRef]
- Alshali, R.Z.; Salim, N.A.; Satterthwaite, J.D.; Silikas, N. Post-irradiation hardness development, chemical softening, and thermal stability of bulk-fill and conventional resin-composites. J. Dent. 2015, 43, 209–218. [Google Scholar] [CrossRef]
- Lima, A.F.; Soares, G.P.; Vasconcellos, P.H.; Ambrosano, G.M.; Marchi, G.M.; Lovadino, J.R.; Aguiar, F.H. Effect of surface sealants on microleakage of Class II restorations after thermocycling and long-term water storage. J. Adhes. Dent. 2011, 13, 249–254. [Google Scholar]
- Gerula-Szymańska, A.; Kaczor, K.; Lewusz-Butkiewicz, K.; Nowicka, A. Marginal integrity of flowable and packable bulk fill materials used for class II restorations–A systematic review and meta-analysis of in vitro studies. Dent. Mater. J. 2020, 39, 335–344. [Google Scholar] [CrossRef]

| Composite | Manufacturer | LOT | Composition | Filler Content (wt%/vol%) |
|---|---|---|---|---|
| Filtek Supreme XTE | 3M ESPE, St. Paul, MN, USA | N959768 | Matrix: Bis-GMA, Bis-EMA, UDMA, TEGDMA, PEGDMA Filler: Silica/zirconia filler | 78.5/63.3 |
| Tetric EvoCeram Bulk Fill | Ivoclar Vivadent, Schaan, Liechtenstein | W07641 | Matrix: Bis-GMA, Bis-EMA, UDMA Filler: Ba-Al-Si-glass, YbF3, spherical mixed oxide, PPF (monomer, glass filler and ytterbium fluoride) | 81 (including 17% PPF)/61 |
| Admira Fusion x-tra | VOCO, Cuxhaven, Germany | 1824538 | Matrix: Ormocer matrix Filler: SiO2, glass ceramics | 84/69 |
| Venus Bulk Fill | Heraeus Kulzer, Hanau, Germany | K010207 | Matrix: UDMA, Bis-EMA Filler: Ba-Al-F-Si-glass, SiO2, YbF3 | 65/38 |
| SDR | Dentsply Sirona, Konstanz, Germany | 1806000680 | Matrix: Modified UDMA, Bis-EMA, TEGDMA Filler: Ba-Al-F-B-Si-glass, Sr-Al-F-Si-glass | 68/45 |
| Enamel | Dentin | |||
|---|---|---|---|---|
| Before TML | After TML | Before TML | After TML | |
| Group 1: FS2 | 92.5 (5.9) AB | 85.3 (8.4) B | 94.9 (5.8) AB | 69.5 (21.1) B |
| Group 2: FS4 | 89.5 (10.1) AB | 76.9 (13.5) B | 85.6 (20.0) B | 62.4 (27.6) BC |
| Group 3: TEC | 93.0 (6.5) AB | 82.6 (10.2) B | 91.0 (8.7) B | 59.0 (19.5) BC |
| Group 4: AFX | 98.1 (2.3) A | 97.3 (3.1) A | 100.0 (0.0) A | 97.7 (4.8) A |
| Group 5: VBF | 74.6 (21.9) B | 32.6 (16.1) C | 84.0 (12.0) B | 16.5 (8.4) D |
| Group 6: SDR | 90.7 (11.3) AB | 48.1 (29.6) C | 84.5 (18.8) B | 35.7 (29.4) CD |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Paganini, A.; Attin, T.; Tauböck, T.T. Margin Integrity of Bulk-Fill Composite Restorations in Primary Teeth. Materials 2020, 13, 3802. https://doi.org/10.3390/ma13173802
Paganini A, Attin T, Tauböck TT. Margin Integrity of Bulk-Fill Composite Restorations in Primary Teeth. Materials. 2020; 13(17):3802. https://doi.org/10.3390/ma13173802
Chicago/Turabian StylePaganini, Alina, Thomas Attin, and Tobias T. Tauböck. 2020. "Margin Integrity of Bulk-Fill Composite Restorations in Primary Teeth" Materials 13, no. 17: 3802. https://doi.org/10.3390/ma13173802
APA StylePaganini, A., Attin, T., & Tauböck, T. T. (2020). Margin Integrity of Bulk-Fill Composite Restorations in Primary Teeth. Materials, 13(17), 3802. https://doi.org/10.3390/ma13173802





