Effect of Cleaning Protocol on Bond Strength between Resin Composite Cement and Three Different CAD/CAM Materials
Abstract
:1. Introduction
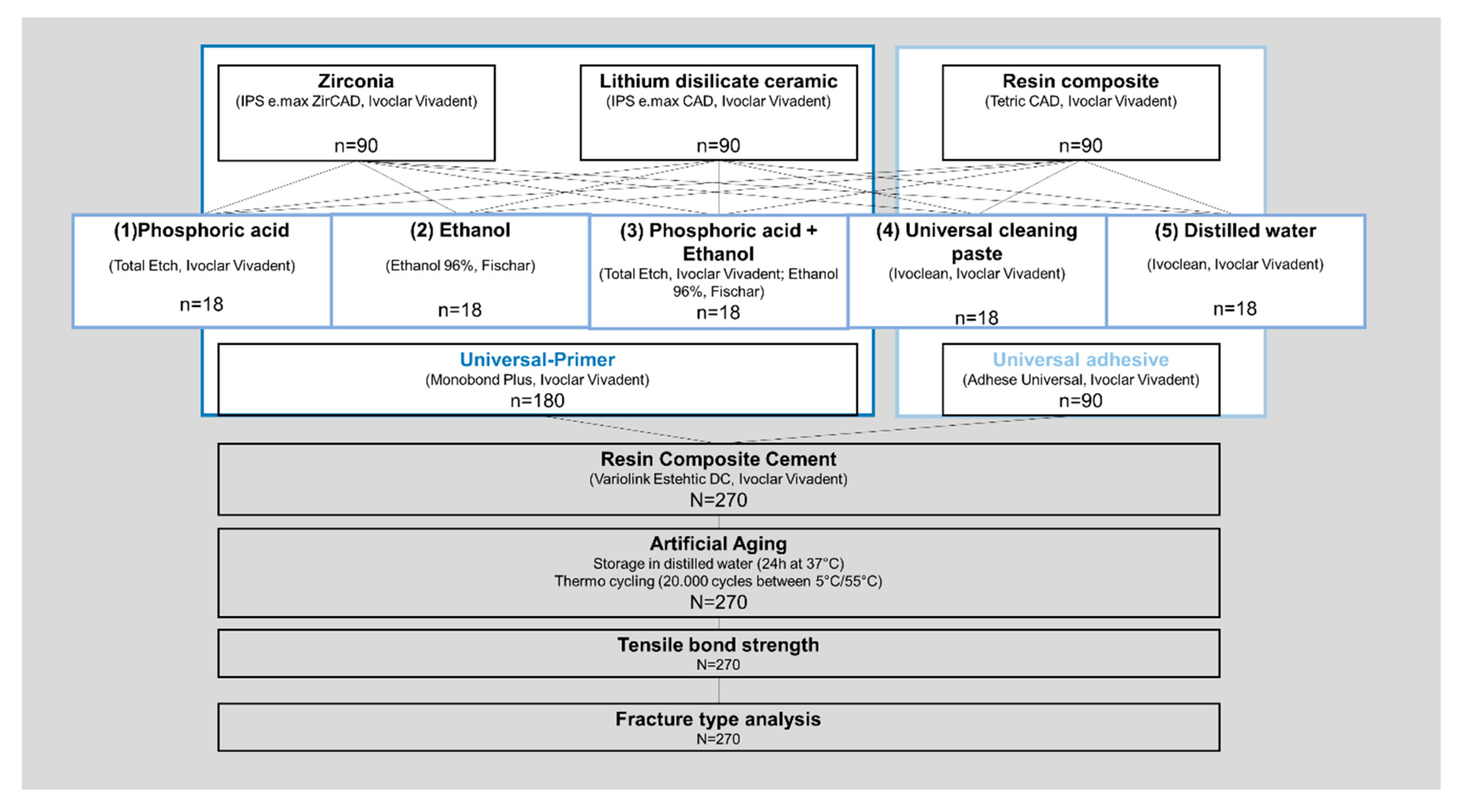
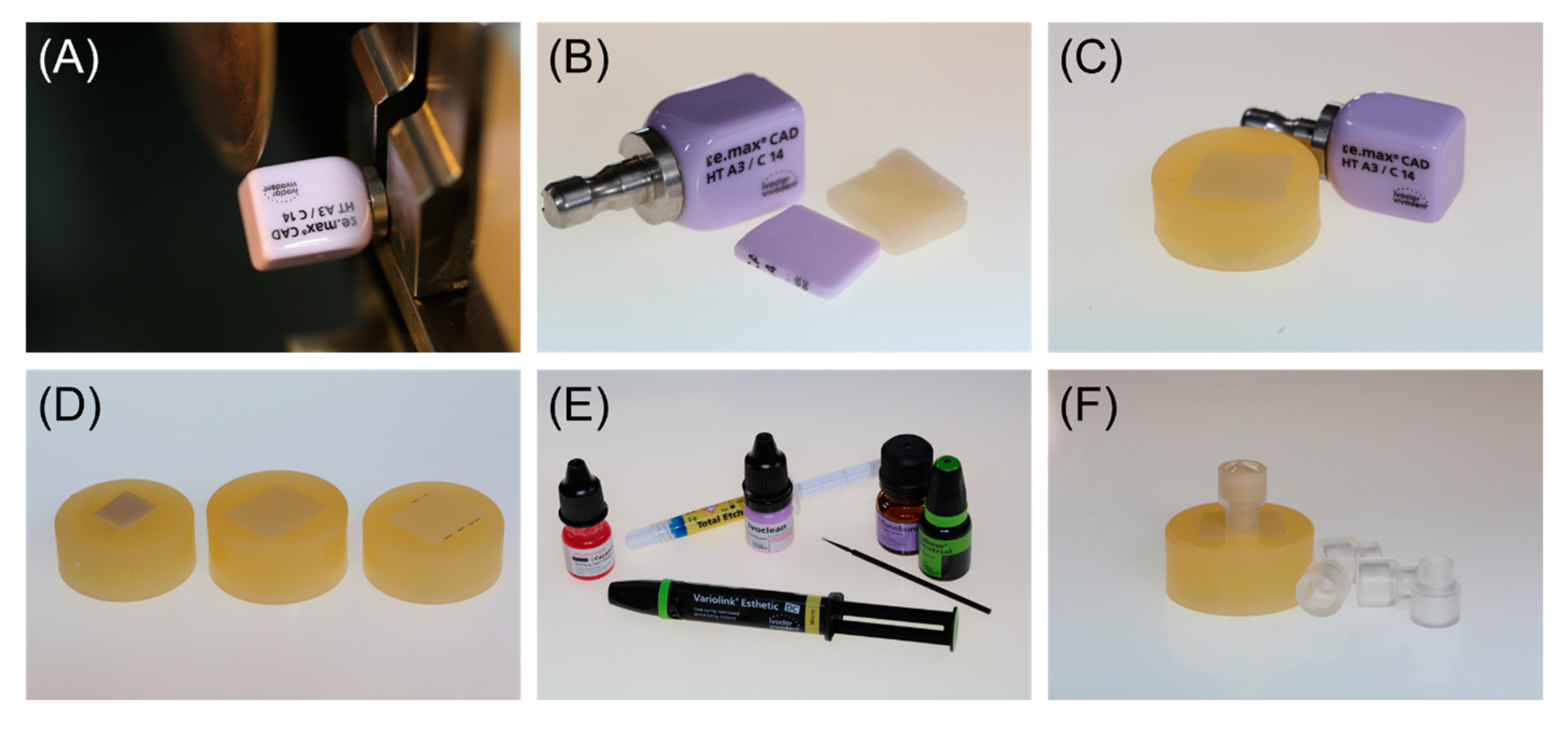
2. Materials and Methods
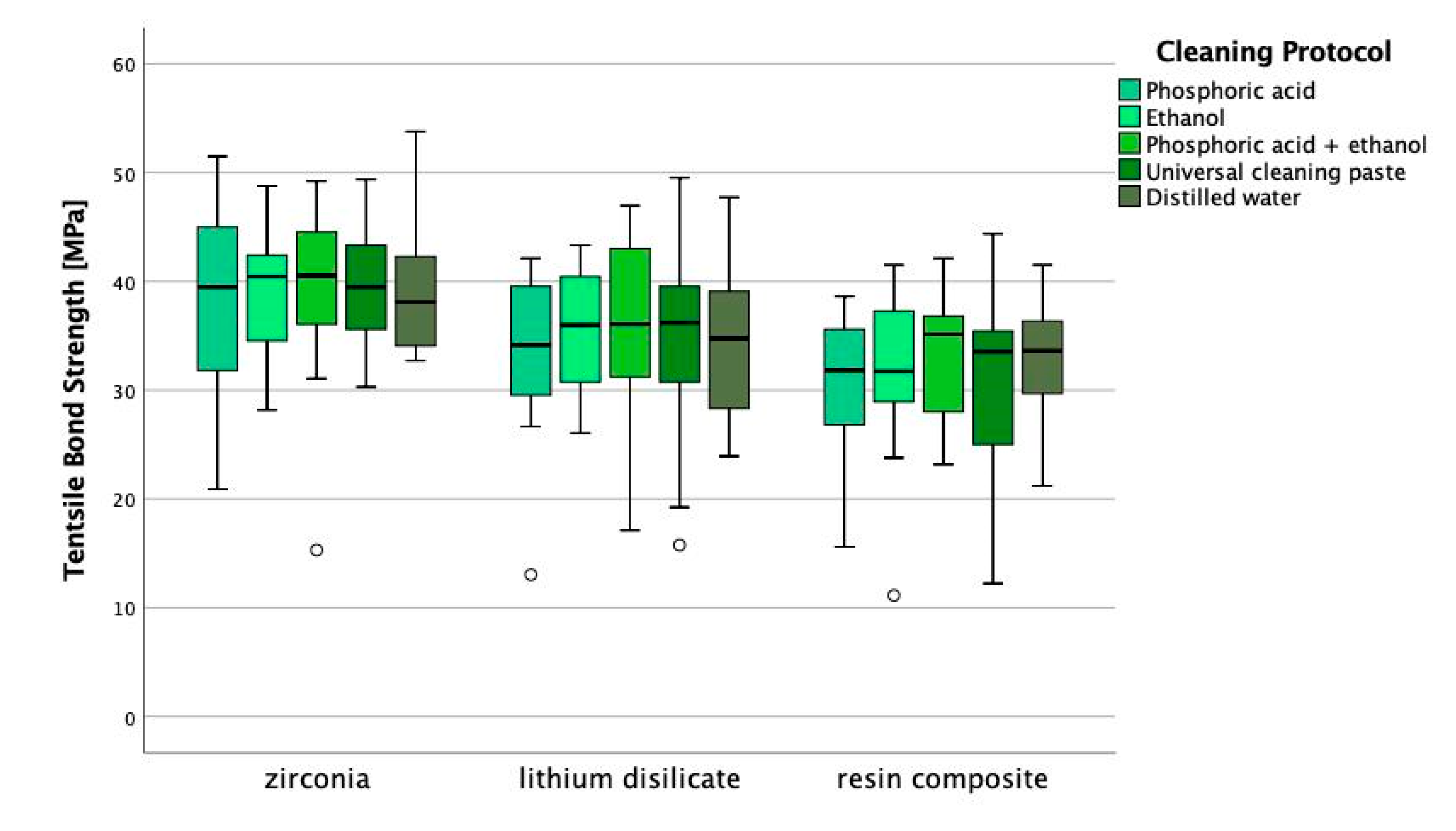
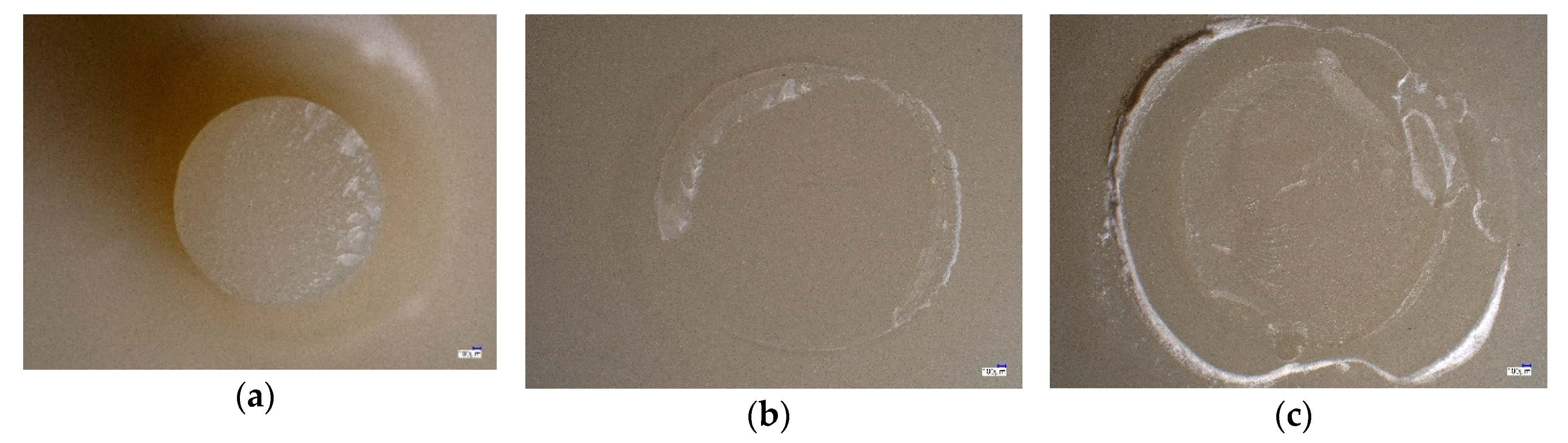
3. Results
4. Discussions
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Spitznagel, F.A.; Boldt, J. Gierthmuehlen PC. CAD/CAM Ceramic Restorative Materials for Natural Teeth. J. Dent. Res. 2018, 97, 1082–1091. [Google Scholar] [CrossRef]
- Tian, T.; Tsio, J.K.-H.; Matinlinna, J.P.; Burrow, M.F. Aspects of bonding between resin luting cements and glass ceramic materials. Dent. Mater. 2014, 30, 147–162. [Google Scholar] [CrossRef]
- Frankenberger, R.; Hermann, V.E.; Krech, M.; Krämer, N.; Reich, S.; Braun, A.; Roggendorf, M. Adhesive luting of new CAD/CAM materials. Int. J. Comput. Dent. 2015, 18, 9–20. [Google Scholar] [PubMed]
- Özcan, M.; Bernasconi, M. Adhesion to zirconia used for dental restorations: A systematic review and meta-analysis. J. Adhes. Dent. 2015, 17, 7–26. [Google Scholar] [PubMed]
- Kern, M. Bonding to oxide ceramics-laboratory testing versus clinical outcome. Dent. Mater. 2015, 31, 8–14. [Google Scholar] [CrossRef] [PubMed]
- Nejat, A.H.; Lee, J.; Shah, S.; Lin, C.P.; Kulkarni, P.; Chavali, R.; Lawson, N.C. Retention of CAD/CAM resin composite crowns following different bonding protocols. Am. J. Dent. 2018, 31, 97–102. [Google Scholar]
- Klosa, K.; Meyer, G.; Kern, M. Clinically used adhesive ceramic bonding methods: A survey in 2007, 2011 and in 2015. Clin. Oral. Investig. 2016, 20, 1691–1698. [Google Scholar] [CrossRef]
- Klosa, K.; Warnecke, H.; Kern, M. Effectiveness of protecting a zirconia bonding surface against contaminations using a newly developed protective lacquer. Dent. Mater. 2014, 30, 785–792. [Google Scholar] [CrossRef]
- Aladag, A.; Elter, B.; Cömlekoglu, E.; Kanat, B.; Sonugelen, M.; Kesercioglu, A.; Özcan, M. Effect of different cleaning regimes on the adhesion of resin to saliva-contaminated ceramics. J. Prosthodont. 2015, 24, 136–145. [Google Scholar] [CrossRef] [Green Version]
- Attia, A.; Lehmann, F.; Kern, M. Influence of surface conditioning and cleaning methods on resin bonding to zirconia ceramic. Dent. Mater. 2011, 27, 207–213. [Google Scholar] [CrossRef] [PubMed]
- Chen, L.; Suh, B.I.; Kim, J.; Tay, F.R. Evaluation of silica-coating techniques for zirconia bonding. Am. J. Dent. 2011, 24, 79–84. [Google Scholar] [PubMed]
- Lung, C.Y.; Liu, D.; Matinlinna, J.P. Silica coating of zirconia by silicon nitride hydrolysis on adhesion promotion of resin to zirconia. Mater. Sci. Eng. C Mater. Biol. Appl. 2015, 46, 103–110. [Google Scholar] [CrossRef] [PubMed]
- Cattani Lorente, M.; Scherrer, S.S.; Richard, J.; Demellayer, R.; Amez-Droz, M.; Wiskott, H.W. Surface roughness and EDS characterization of a Y-TZP dental ceramic treated with the CoJetTM Sand. Dent. Mater. 2010, 26, 1035–1042. [Google Scholar] [CrossRef] [PubMed]
- Yi, Y.A.; Ahn, J.S.; Park, Y.J.; Jun, S.H.; Lee, I.B.; Cho, B.H.; Son, H.H.; Seo, D.G. The effect of sandblasting and different primers on shear bond strength between yttria-tetragonal zirconia polycrystal ceramic and a self-adhesive resin cement. Oper. Dent. 2015, 40, 63–71. [Google Scholar] [CrossRef] [PubMed]
- Nishigawa, G.; Maruo, Y.; Irie, M.; Oka, M.; Yoshihara, K.; Minagi, S.; Nagaoka, N.; Yoshida, Y.; Suzuki, K. Ultrasonic cleaning of silica-coated zirconia influences bond strength between zirconia and resin luting material. Dent. Mater. J. 2008, 27, 842–848. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Attia, A.; Kern, M. Long-term resin bonding to zirconia ceramic with new universal primer. J. Prosthet. Dent. 2011, 106, 319–327. [Google Scholar] [CrossRef]
- Takahashi, A. The effect of different cleaning agents on saliva contamination for bonding performance of zirconia ceramics. Dent. Mater. 2018, 37, 734–739. [Google Scholar] [CrossRef] [Green Version]
- Moura, D.M.D.; Araujo, A.M.M.; Souza, K.B.; Verissimo, A.H.; Tribst, J.P.M.; Souza, R.O.A.E. Hydrofluoric acid concentration, time and use of phosphoric acid on the bond strength of feldspathic ceramics. Braz. Oral. Res. 2020, 34, e018. [Google Scholar] [CrossRef]
- Güth, J.F.; Stawarczyk, B.; Edelhoff, D.; Liebermann, A. Zirconia and its novel compositions: What do clinicians need to know? Quintessence Int. 2019, 50, 512–520. [Google Scholar]
- Yang, B.; Lange-Jansen, H.C.; Scharnberg, M.; Wolfart, S.; Lugwig, K.; Adelung, R.; Kern, M. Influence of saliva contamination on zirconia ceramic bonding. Dent. Mater. 2008, 4, 508–513. [Google Scholar] [CrossRef]
- Feitosa, S.A.; Patel, D.; Borges, A.L.; Alshehri, E.Z.; Bottino, M.A.; Özcan, M.; Valandro, L.F.; Bottino, M.C. Effect of cleaning methods on saliva-contaminated zirconia: An evaluation of resin bond durability. Oper. Dent. 2015, 40, 163–171. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Phark, J.H.; Duarte, S., Jr.; Kahn, H.; Blatz, M.B.; Sadan, A. Influence of contamination and cleaning on bond strength to modified zirconia. Dent. Mater. 2009, 25, 1541–1550. [Google Scholar] [CrossRef] [PubMed]
- Yoshida, K. Influence of cleaning methods on resin bonding to saliva contaminated zirconia. J. Esthet. Restor. Dent. 2018, 30, 259–264. [Google Scholar] [CrossRef] [PubMed]
- Bähr, N.; Keul, C.; Edelhoff, D.; Eichberger, M.; Roos, M.; Gernet, W.; Stawarczyk, B. Effect of different adhesives combined with two resin composite cements on shear bond strength to polymeric CAD/CAM materials. Dent. Mater. J. 2013, 32, 492–501. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yu, H.; Özcan, M.; Yoshida, K.; Cheng, H.; Sawase, T. Bonding to industrial indirect composite blocks: A systematic review and meta analysis. Dent. Mater. 2020, 36, 19–134. [Google Scholar] [CrossRef]
- Yang, B.; Scharnberg, M.; Wolfart, S.; Quaas, A.C.; Ludwig, K.; Adelung, R.; Kern, M. Influence of contamination on bonding to zirconia ceramic. J. Biomed. Mater. Res. B Appl. Biomater. 2007, 81, 283–290. [Google Scholar] [CrossRef]
- Nejatidanesh, F.; Savabi, O.; Savabi, G.; Razavi, M. Effect of cleaning methods on retentive values of saliva-contaminated implant-supported zirconia copings. Clin. Oral. Implants Res. 2018, 29, 530–536. [Google Scholar] [CrossRef]
- Lima, R.B.W.; Barreto, S.C.; Hajhamid, B.; de Souza, G.M.; de Goes, M.F. Effect of cleaning protocol on silica deposition and silica-mediated bonding to Y-TZP. Dent. Mater. 2019, 35, 1603–1613. [Google Scholar] [CrossRef]
- Noronha, M.D.S.; Fronza, B.M.; André, C.B.; de Castro, E.F.; Soto-Montero, J.; Price, R.B.; Giannini, M. Effect of zirconia decontamination protocols on bond strength and surface wettability. J. Esthet. Restor. Dent. 2020, 32, 521–529. [Google Scholar] [CrossRef]
- Al-Dobaei, E.; Al-Akhali, M.; Polonskyi, O.; Strunskus, T.; Wille, S.; Kern, M. Influence of Cleaning Methods on Resin Bonding to Contaminated Translucent 3Y-TZP ceramic. J. Adhes. Dent. 2020, 22, 383–391. [Google Scholar]
- Klosa, K.; Wolfart, S.; Lehmann, F.; Wenz, H.J.; Kern, M. The effect of storage conditions, contamination modes and cleaning procedures on the resin bond strength to lithium disilicate ceramic. J. Adhes. Dent. 2009, 11, 127–135. [Google Scholar] [PubMed]
- Nikolaus, F.; Wolkewitz, M.; Hahn, P. Bond strength of composite resin to glass ceramic after saliva contamination. Clin. Oral. Investig. 2013, 17, 751–755. [Google Scholar] [CrossRef] [PubMed]
- Yoshida, K. Influence of cleaning methods on the bond strength of resin cement to saliva-contaminated lithium disilicate ceramic. Clin. Oral. Investig. 2020, 24, 2091–2097. [Google Scholar] [CrossRef] [PubMed]
- Bijelic-Donova, J.; Flett, A.; Lassila, L.V.J.; Vallittu, P.K. Immediate repair bond strength of fiber-reinforced composite after saliva or water contamination. J. Adhes. Dent. 2018, 20, 205–212. [Google Scholar] [PubMed]
| Material | Product Name | Manufacturer | Chemical Composition | Lot No. |
|---|---|---|---|---|
| Lithium disilicate glass-ceramic | IPS e.max CAD HT | Ivoclar Vivadent; Schaan, Liechtenstein | Lithium disilicate glass-ceramic (LS2) Silicate-based glass-ceramic | X25830 |
| Zirconia | IPS e.max ZirCAD LT | Ivoclar Vivadent; Schaan, Liechtenstein | ZrO2 88.0–95.5 wt.% Y2O3 > 4.5 ≤ 6.0 wt.% HfO2 ≤ 5.0 wt.% Al2O3 ≤ 1.0 wt.% Other oxides ≤1 wt.% | X17186 |
| Resin composite | Tetric CAD | Ivoclar Vivadent; Schaan, Liechtenstein | Cross-linked dimethacrylate inorganic filler particles | X12627 |
| Hydrofluoric acid | IPS Ceramic Etching Gel | Ivoclar Vivadent; Schaan, Liechtenstein | <5 wt.% hydrofluoric acid | W14921 |
| Phosphoric acid | Total Etch | Ivoclar Vivadent; Schaan, Liechtenstein | 37 wt.% phosphoric acid in water, thickening agent, color pigments | X51245 |
| Cleaning paste | Ivoclean | Ivoclar Vivadent; Schaan, Liechtenstein | Dispersion of metal oxide particles in water | X47350 |
| Universal primer | Monobond Plus | Ivoclar Vivadent; Schaan, Liechtenstein | Alcohol solution of silane methacrylate, phosphoric acid methacrylate and sulphide methacrylate | X51129 |
| Universal adhesive | Adhese Universal | Ivoclar Vivadent; Schaan, Liechtenstein | methacrylates, ethanol, water, highly dispersed silicon dioxide, initiators and stabilizers | X41517 |
| Resin composite cement | Variolink Esthetic DC | Ivoclar Vivadent; Schaan, Liechtenstein | Monomer matrix: urethane dimethacrylate, and further methacrylate monomers; inorganic fillers: ytterbium trifluoride and spheroid mixed oxide; initiators: stabilizers, pigments | X41008 |
| Material | Start Temperature (°C) | End Temperature (°C) | Heating/Cooling Rate (°C/min) | Holding Time (min) |
|---|---|---|---|---|
| IPS e.max Zir CAD | 20 | 900 | 10 | 30 |
| 900 | 1500 | 3.3 | 120 | |
| 1500 | 900 | 10 | --- | |
| 900 | 300 | 8.3 | --- | |
| IPS e.max CAD | 550 | 550 | 0 | 6 |
| 550 | 820 | 90 | 1 | |
| 820 | 840 | 30 | 7 | |
| 840 | 700 | --- | --- |
| Material | Cleaning Protocol | Tensile Bond Strength (MPa) | ||
|---|---|---|---|---|
| Mean ± SD | 95% CI | Min/Median/Max | ||
| IPS e.max Zir CAD | Total Etch | 37.5 ± 9.2 | 32.8;42.1 | 20.9/39.5/51.5 |
| Total Etch + Ethanol | 39.1 ± 7.6 | 35.1;42.9 | 15.3/40.5/49.2 | |
| Ethanol | 38.9 ± 5.6 * | 36.0;41.7 | 28.2/40.4/48.8 | |
| Ivoclean | 39.6 ± 4.7 | 37.1;42.0 | 30.3/39.5/49.4 | |
| Distilled Water | 39.2 ± 5.6 | 36.3;42.1 | 32.7/38.1/53.8 | |
| IPS e.max CAD | Total Etch | 33.5 ± 7.1 | 29.9;37.1 | 13.0/34.2/42.1 |
| Total Etch + Ethanol | 35.8 ± 7.6 | 31.9;39.6 | 17.1/36.1/47.0 | |
| Ethanol | 35.4 ± 5.4 | 32.5;38.1 | 26.1/36.0/43.3 | |
| Ivoclean | 34.0 ± 9.0 | 29.3;38.4 | 15.8/36.2/49.5 | |
| Distilled Water | 35.2 ± 7.4 | 31.4;39.0 | 23.9/34.8/47.7 | |
| Tetric CAD | Total Etch | 31.1 ± 6.0 | 27.9;34.1 | 15.6/31.8/38.6 |
| Total Etch + Ethanol | 33.3 ± 5.7 | 30.3;36.2 | 23.2/35.1/42.1 | |
| Ethanol | 31.7 ± 7.3 | 28.0;35.4 | 11.1/31.7/41.5 | |
| Ivoclean | 30.8 ± 7.7 | 26.8;34.7 | 12.2/33.6/44.4 | |
| Distilled Water | 32.5 ± 5.1 | 29.8;35.1 | 21.2/33.6/41.5 | |
| Material | Cleaning Protocol | Fracture Type | ||
|---|---|---|---|---|
| Adhesive | Cohesive | Mixed | ||
| IPS e.max Zir CAD | Total Etch | 0 (0;19) | 100 (80;100) | 0 (0;19) |
| Total Etch + Ethanol | 0 (0;19) | 100 (80;100) | 0 (0;19) | |
| Ethanol | 0 (0;19) | 100 (80;100) | 0 (0;19) | |
| Ivoclean | 0 (0;19) | 100 (80;100) | 0 (0;19) | |
| Distilled Water | 0 (0;19) | 100 (80;100) | 0 (0;19) | |
| IPS e.max CAD | Total Etch | 11 (1;35) | 89 (64;99) | 0 (0;19) |
| Total Etch + Ethanol | 0 (0;19) | 100 (80;100) | 0 (0;19) | |
| Ethanol | 0 (0;19) | 100 (80;100) | 0 (0;19) | |
| Ivoclean | 6 (0;28) | 94 (71;99) | 0 (0;19) | |
| Distilled Water | 0 (0;19) | 100 (80;100) | 0 (0;19) | |
| Tetric CAD | Total Etch | 11 (1;35) | 89 (64;99) | 0 (0;19) |
| Total Etch + Ethanol | 0 (0;19) | 100 (80;100) | 0 (0;19) | |
| Ethanol | 0 (0;19) | 94 (71;99) | 6 (0;28) | |
| Ivoclean | 0 (0;19) | 100 (71;99) | 6 (0;28) | |
| Distilled Water | 0 (0;19) | 100 (80;100) | 0 0 (0;19) | |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lümkemann, N.; Schönhoff, L.M.; Buser, R.; Stawarczyk, B. Effect of Cleaning Protocol on Bond Strength between Resin Composite Cement and Three Different CAD/CAM Materials. Materials 2020, 13, 4150. https://doi.org/10.3390/ma13184150
Lümkemann N, Schönhoff LM, Buser R, Stawarczyk B. Effect of Cleaning Protocol on Bond Strength between Resin Composite Cement and Three Different CAD/CAM Materials. Materials. 2020; 13(18):4150. https://doi.org/10.3390/ma13184150
Chicago/Turabian StyleLümkemann, Nina, Lisa Marie Schönhoff, Ramona Buser, and Bogna Stawarczyk. 2020. "Effect of Cleaning Protocol on Bond Strength between Resin Composite Cement and Three Different CAD/CAM Materials" Materials 13, no. 18: 4150. https://doi.org/10.3390/ma13184150






