Influence of Different Surface Pretreatments on Shear Bond Strength of an Adhesive Resin Cement to Various Zirconia Ceramics
Abstract
:1. Introduction
2. Materials and Methods
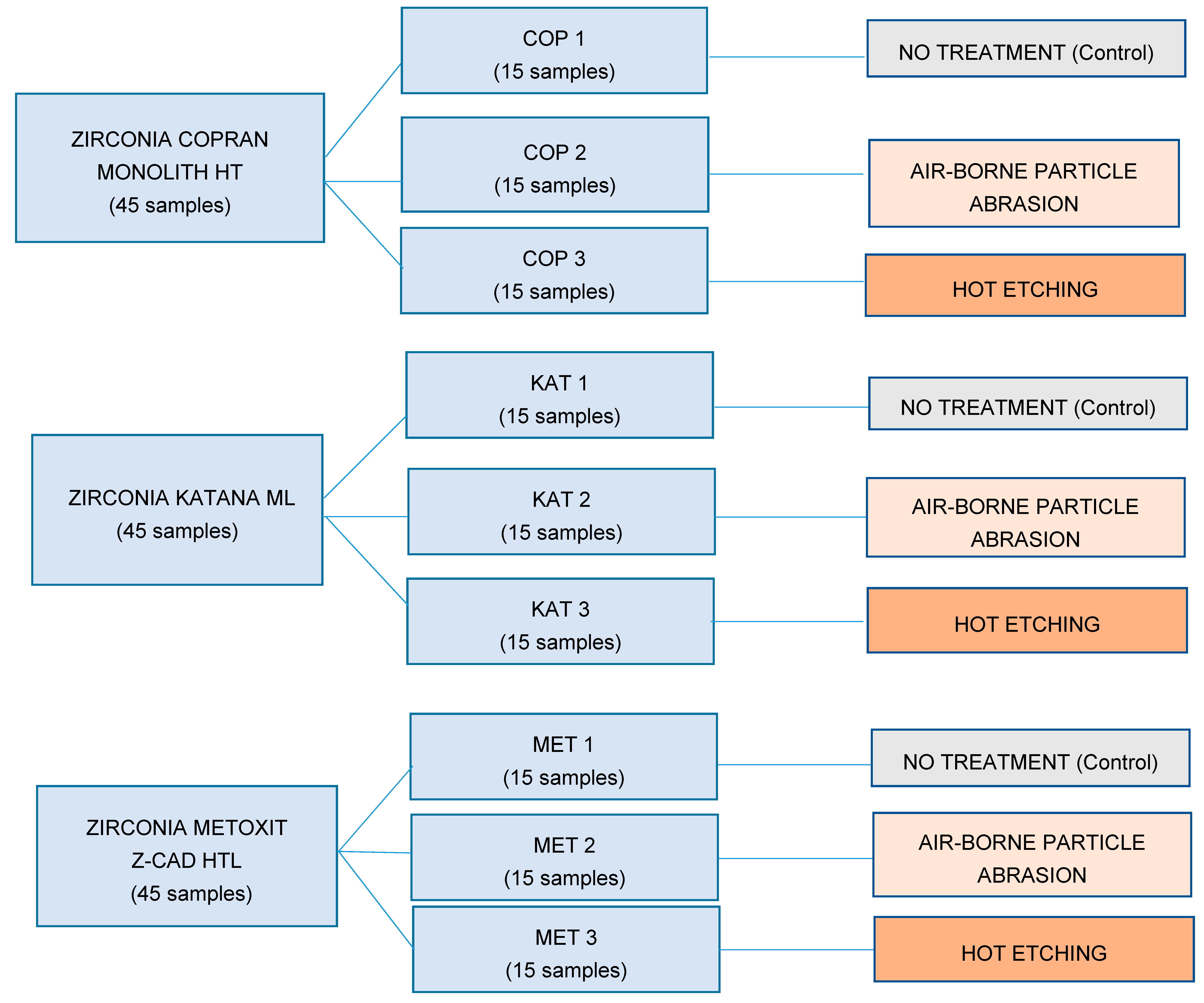
2.1. Specimen Preparation
- -
- Groups COP 1, KAT 1, and MET 1: no treatment (control groups). The cementation surfaces remained unaltered and unchanged after the manufacturing process [21];
- -
- Groups COP 2, KAT 2, and MET 2: ABPA (Base 1 Plus, Dentalfarm, Torino, Italia) with aluminum dioxide particles with 50-μm particle size at 0.3 MPa for 20 s at a distance of 10 mm perpendicular to the sample’s surface; subsequently, samples were rinsed with an air/water vaporizer (Minivapor.86, Effegi Brega, Sarmato, Italia) for 10 s and finally air-dried [22];
- -
- Groups COP 3, KAT 3, and MET 3: immersion in an experimental corrosive solution of HCl–FeCl3 (800 mL of hydrochloric acid HCl and 5 mL of ferric chloride FeCl3) for 10 min at a temperature of 100 °C, subsequently washed with 90% CH3OH methanol and finally air-dried [17].
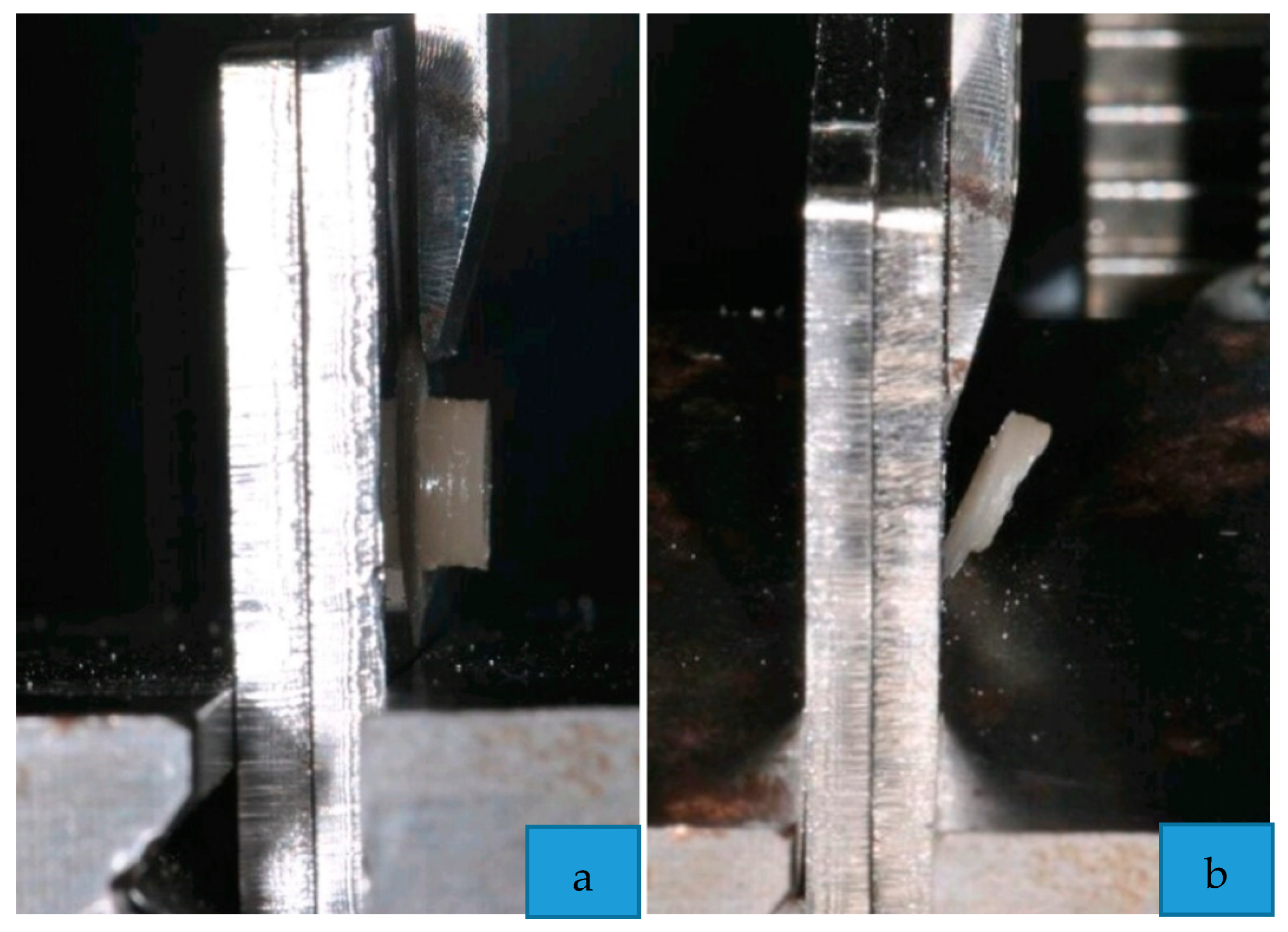
2.2. Shear Bond Strength Testing
2.3. Statistical Analysis
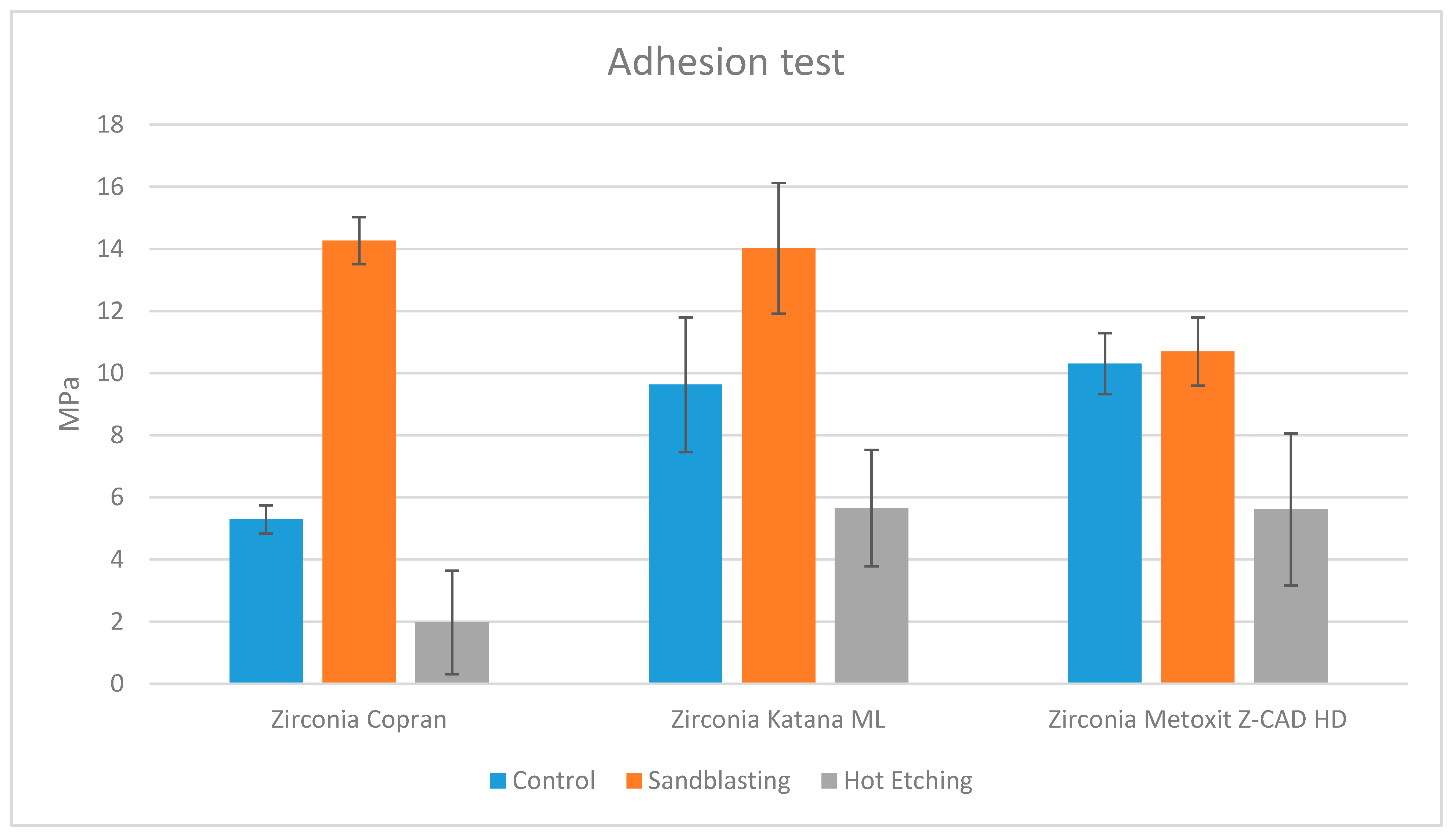
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Giordano, R. Materials for chairside CAD/CAM-produced restorations. J. Am. Dent. Assoc. 2006, 137, 14S–21S. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, J.-F.; Migonney, V.; Ruse, N.D.; Sadoun, M. Resin composite blocks via high-pressure high-temperature polymerization. Dent. Mater. 2012, 28, 529–534. [Google Scholar] [CrossRef] [PubMed]
- Coldea, A.; Swain, M.V.; Thiel, N. Mechanical properties of polymer-infiltrated-ceramic-network materials. Dent. Mater. 2013, 29, 419–426. [Google Scholar] [CrossRef] [PubMed]
- Luthardt, R.; Holzhüter, M.; Sandkuhl, O.; Herold, V.; Schnapp, J.; Kuhlisch, E.; Walter, M. Reliability and properties of ground Y-TZP-zirconia ceramics. J. Dent. Res. 2002, 81, 487–491. [Google Scholar] [CrossRef]
- Manicone, P.F.; Iommetti, P.R.; Raffaelli, L. An overview of zirconia ceramics: Basic properties and clinical applications. J. Dent. 2007, 35, 819–826. [Google Scholar] [CrossRef]
- Eschbach, S.; Wolfart, S.; Bohlsen, F.; Kern, M. Clinical evaluation of all-ceramic posterior three-unit FDPs made of In-Ceram Zirconia. Int. J. Prosthodont. 2009, 22, 490–492. [Google Scholar]
- Schmitt, J.; Holst, S.; Wichmann, M.; Reich, S.; Gollner, M.; Hamel, J. Zirconia posterior fixed partial dentures: a prospective clinical 3-year follow-up. Int. J. Prosthodont. 2009, 22, 597–603. [Google Scholar]
- Özkurt, Z.; Kazazoğlu, E. Clinical Success of Zirconia in Dental Applications. J. Prosthodont. 2010, 19, 64–68. [Google Scholar] [CrossRef]
- Colombo, M.; Poggio, C.; Lasagna, A.; Chiesa, M.; Scribante, A. Vickers Micro-Hardness of New Restorative CAD/CAM Dental Materials: Evaluation and Comparison after Exposure to Acidic Drink. Materials 2019, 12, 1246. [Google Scholar] [CrossRef] [Green Version]
- Guazzato, M.; Albakry, M.; Ringer, S.P.; Swain, M.V. Strength, fracture toughness and microstructure of a selection of all- ceramic materials. Part II. Zirconia-based dental ceramics. Dent. Mater. 2004, 20, 449–456. [Google Scholar] [CrossRef]
- Raigrodski, A.J. Contemporary materials and technologies for all- ceramic fixed partial dentures: a review of the literature. J. Prosthet. Dent. 2004, 92, 557–562. [Google Scholar] [CrossRef] [PubMed]
- Blatz, M.B.; Chiche, G.; Holst, S.; Sadan, A. Influence of surface treatment and simulated aging on bond strengths of luting agents to zirconia. Quintessence Int 2007, 38, 745–753. [Google Scholar] [PubMed]
- Atsu, S.S.; Kilicarslan, M.A.; Kucukesmen, H.C.; Aka, P.S. Effect of zirconium-oxide ceramic surface treatments on the bond strength to adhesive resin. J. Prosthet. Dent. 2006, 95, 430–436. [Google Scholar] [CrossRef] [PubMed]
- Derand, T.; Molin, M.; Kvam, K. Bond strength of com-posite luting cement to zirconia ceramic surfaces. Dent. Materials 2005, 21, 1158–1162. [Google Scholar] [CrossRef]
- Janda, R.; Roulet, J.-F.; Wulf, M.; Tiller, H.-J. A new adhesive technology for all-ceramics. Dent. Mater. 2003, 19, 567–573. [Google Scholar] [CrossRef]
- Raigrodski, M.N.; Kleverlaan, C.J.; Feilzer, A.J. Selective infiltration-etching technique for a strong and durable bond of resin cements to zirconia-based materials. J. Prosthet. Dent. 2007, 98, 379–388. [Google Scholar]
- Ferrari, M.; Cagidiaco, M.; Borracchini, A.; Bertelli, E. Evaluation of a chemical etching solution for nickel-chromium-beryllium and chromium-cobalt alloys. J. Prosthet. Dent. 1989, 62, 516–521. [Google Scholar] [CrossRef]
- Casucci, A.; Osorio, E.; Osorio, R.; Monticelli, F.; Toledano, M.; Mazzitelli, C.; Ferrari, M. Influence of different surface treatments on surface zirconia frameworks. J. Dent. 2009, 37, 891–897. [Google Scholar] [CrossRef]
- Kern, M.; Barloi, A.; Yang, B. Surface conditioning influences zirconia ceramic bonding. J. Dent. Res. 2009, 88, 817–822. [Google Scholar] [CrossRef]
- Wegner, S.M.; Kern, M. Long-term resin bond strength to zirconia ceramic. J Adhes Dent 2000, 2, 139–147. [Google Scholar]
- Augusti, D.; Re, D.; Augusti, G.; Merlati, G.; Barabanti, N.; Cerutti, A. I pretrattamenti di superficie del biossido di zirconio nella cementazione adesiva: studio in vitro. Dentista Moderno. 2010, 9, 134–150. [Google Scholar]
- Ahn, J.-S.; Yi, Y.-A.; Lee, Y.; Seo, D.-G. Shear Bond Strength of MDP-Containing Self-Adhesive Resin Cement and Y-TZP Ceramics: Effect of Phosphate Monomer-Containing Primers. BioMed Res. Int. 2015, 2015, 1–6. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ceci, M.; Pigozzo, M.; Scribante, A.; Beltrami, R.; Colombo, M.; Chiesa, M.; Poggio, C. Effect of glycine pretreatment on the shear bond strength of a CAD/CAM resin nano ceramic material to dentin. J. Clin. Exp. Dent. 2016, 8, e146–e152. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Beltrami, R.; Chiesa, M.; Scribante, A.; Allegretti, J.; Poggio, C. Comparison of shear bond strength of universal adhesives on etched and nonetched enamel. J. Appl. Biomater. Funct. Mater. 2016, 14, 78–83. [Google Scholar] [CrossRef] [Green Version]
- Al-Dohan, H.M.; Yaman, P.; Dennison, J.B.; Razzoog, M.E.; Lang, B. Shear strength of core veneer interface in bi-layered ceramics. J. Prosthet. Dent. 2004, 91, 349–355. [Google Scholar] [CrossRef]
- Scribante, A.; Contreras-Bulnes, R.; Montasser, M.A.; Vallittu, P.K. Orthodontics: Bracket Materials, Adhesives Systems, and Their Bond Strength. BioMed Res. Int. 2016, 2016, 1–3. [Google Scholar] [CrossRef]
- Colombo, M.; Beltrami, R.; Chiesa, M.; Poggio, C.; Scribante, A. Shear bond strength of one-step self-etch adhesives to dentin: Evaluation of NaOCl pretreatment. J. Clin. Exp. Dent. 2018, 10, e127–e133. [Google Scholar] [CrossRef] [Green Version]
- Gargari, M.; Gloria, F.; Cappello, A.; Ottria, L. Strength of zirconia fixed partial dentures: review of the literature. Oral. Implantol. 2010, 3, 15–24. [Google Scholar]
- Tinschert, J.; Natt, G.; Mautsch, W.; Augthun, M.; Spiekermann, H. Fracture resistance of lithium disilicate-, alumina-, and zirconia-based three-unit fixed partial dentures: a laboratory study. Int. J. Prosthodont. 2001, 14, 231–238. [Google Scholar]
- Mota, Y.A.; Cotes, C.; Carvalho, R.F.; Machado, J.P.B.; Leite, F.P.P.; Souza, R.O.A.; Özcan, M. Monoclinic phase transformation and mechanical durability of zirconia ceramic after fatigue and autoclave aging. J. Biomed. Mater. Res. B Appl. Biomater. 2017, 105, 1972–1977. [Google Scholar] [CrossRef] [Green Version]
- Tsukakoshi, M.; Shinya, A.; Gomi, H.; Lassila, L.V.; Vallittu, P.K.; Shinya, A. Effects of dental adhesive cement and surface treatment on bond strength and leakage of zirconium oxide ceramics. Dent. Mater. J. 2008, 27, 159–171. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aboushelib, M.N.; Mirmohamadi, H.; Matinlinna, J.P.; Kukk, E.; Ounsi, H.F.; Salameh, Z. Innovations in bonding to zirconia-based materials. Part II: Focusing on chemical interactions. Dent. Mater. 2009, 25, 989–993. [Google Scholar] [CrossRef] [PubMed]
- Kosmač, T.; Oblak, C.; Jevnikar, P.; Funduk, N.; Marion, L. The effect of surface grinding and sandblasting on flexural strength and reliability of Y-TZP zirconia ceramic. Dent. Mater. 1999, 15, 426–433. [Google Scholar] [CrossRef]
- Guazzato, M.; Proos, K.; Quach, L.; Swain, M.V. Strength, reliability and mode of fracture of bilayered porcelain/zirconia (Y-TZP) dental ceramics. Biomaterials 2004, 25, 5045–5052. [Google Scholar] [CrossRef] [PubMed]
- Aboushelib, M.N.; Matinlinna, J.P.; Salameh, Z.; Ounsi, H. Innovations in bonding to zirconia-based materials: Part I. Dent. Mater. 2008, 24, 1268–1272. [Google Scholar] [CrossRef]
- Nagaoka, N.; Yoshihara, K.; Feitosa, V.P.; Tamada, Y.; Irie, M.; Yoshida, Y.; Van Meerbeek, B.; Hayakawa, S. Chemical interaction mechanism of 10-MDP with zirconia. Sci. Rep. 2017, 7, 45563. [Google Scholar] [CrossRef] [Green Version]
- Kern, M. Bonding to oxide ceramics—Laboratory testing versus clinical outcome. Dent. Mater. 2015, 31, 8–14. [Google Scholar] [CrossRef]
- Blatz, M.B.; Vonderheide, M.; Conejo, J. The Effect of Resin Bonding on Long-Term Success of High-Strength Ceramics. J Dent Res. 2018, 97, 132–139. [Google Scholar] [CrossRef]
- Kern, M.; Passia, N.; Sasse, M.; Yazigi, C. Ten-year outcome of zirconia ceramic cantilever resin-bonded fixed dental prostheses and the influence of the reasons for missing incisors. J. Dent. 2017, 65, 51–55. [Google Scholar] [CrossRef]
- Le, M.; Larsson, C.; Papia, E. Bond strength between MDP-based cement and translucent zirconia. Dent. Mater. J. 2019, 38, 480–489. [Google Scholar] [CrossRef] [Green Version]
- Nishigawa, G.; Maruo, Y.; Irie, M.; Maeda, N.; Yoshihara, K.; Nagaoka, N.; Matsumoto, T.; Minagi, S. Various Effects of Sandblasting of Dental Restorative Materials. PLoS ONE 2016, 11, e0147077. [Google Scholar] [CrossRef] [PubMed]
- Sawada, T.; Spintzyk, S.; Schille, C.; Zöldföldi, J.; Paterakis, A.; Schweizer, E.; Stephan, I.; Rupp, F.; Geis-Gerstorfer, J. Influence of Pre-Sintered Zirconia Surface Conditioning on Shear Bond Strength to Resin Cement. Materials 2016, 9, 518. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Attia, A.; Lehmann, F.; Kern, M. Influence of surface conditioning and cleaning methods on resin bonding to zirconia ceramic. Dent. Mater. 2011, 27, 207–213. [Google Scholar] [CrossRef] [PubMed]
- Scribante, A.; Sfondrini, M.F.; Fraticelli, D.; Daina, P.; Tamagnone, A.; Gandini, P. The Influence of No-Primer Adhesives and Anchor Pylons Bracket Bases on Shear Bond Strength of Orthodontic Brackets. BioMed Res. Int. 2013, 2013, 1–6. [Google Scholar] [CrossRef]
- Poggio, C.; Scribante, A.; Della Zoppa, F.; Colombo, M.; Beltrami, R.; Chiesa, M. Shear bond strength of one-step self-etch adhesives to enamel: Effect of acid pretreatment. Dent. Traumatol. 2014, 30, 43–48. [Google Scholar] [CrossRef]
- Pereira, P.; Yamada, T.; Inokoshi, S.; Burrow, M.; Sano, H.; Tagami, J. Adhesion of resin-modified glass ionomer cements using resin bonding systems. J. Dent. 1998, 26, 479–485. [Google Scholar] [CrossRef]

| Product | Chemical Composition (wt.%) * | Technical Data * | Manufacturer (Lot No.) |
|---|---|---|---|
| Copran Zirconia Monolith HT | Zirconium dioxide (balance), yttrium oxide (5.15–5.55), aluminium oxide (0.03–0.07), iron hydroxide (0–0.01), other (0–0.02) a | Density (g/cm3): 6.09 a Flexural strength (MPa): 1100 a Translucency (%): 20 b | Whitepeaks Dental Solutions GmbH & Co. KG, Wesel, Germany (IM1024A2) |
| Katana ML Zirconia | Zirconium dioxide (86.21), yttrium oxide (10.95), aluminium oxide (0.16), hafnium dioxide (2.41) b | Density (g/cm3): 6.00 a Flexural Strength (MPa): 1125 a Fracture Strength (MPa√m): 5 a Translucency (%): 31 a Grain size (μm): 0.6 b | Kuraray Noritake Dental Inc., Tokyo, Japan (DDZHM) |
| Metoxit Z-CAD HTL Zirconia | Zirconium dioxide (92.72), yttrium oxide (5.35), hafnium dioxide (1.88), alluminium oxide (0.05), other (≤ 0.05) a | Density (g/cm3): 6.08 a Flexural Strength (MPa): > 1100 a Translucency (%): 41 a Grain size (μm): < 0.4 a | Metoxit AG, Thayngen Switzerland (409800) |
| Product | Description | Chemical Composition * | Manufacturer (Lot No.) |
|---|---|---|---|
| G-CEM Link Force TM | Dual-cure adhesive luting cement with barium fillers (size of 300 nm, 62 vol.% rate) | Paste A: bis-GMA, urethanedimethacrylate, dimethacrylate, barium glass, initiator, pigments. Paste B: bis-MEPP, urethanedimethacrylate, dimethacrylate, barium glass, initiator. | GC Corporation, Tokyo, Japan (1803271) |
| G-Multi PRIMER | Universal primer for adhesive cementation | Ethanol, MDP, MDTP, silane, methacrylate monomer | GC Corporation, Tokyo, Japan (1806051) |
| Group | Zirconia Type | Condition | Mean | SD | Min | Median | Max |
|---|---|---|---|---|---|---|---|
| COP 1 | Copran Monolith HT | Control | 5.27 a | 0.75 | 4.23 | 5.79 | 5.84 |
| COP 2 | Copran Monolith HT | Air-borne particle abrasion (APBA) | 14.33 b | 2.35 | 10.12 | 14.34 | 19.22 |
| COP 3 | Copran Monolith HT | Hot etching | 1.95 c | 0.85 | 1.07 | 1.87 | 2.86 |
| KAT 1 | Katana ML | Control | 9.64 d | 0.88 | 8.56 | 9.67 | 10.70 |
| KAT 2 | Katana ML | Air-borne particle abrasion | 14.29 b | 2.56 | 10.66 | 14.01 | 18.43 |
| KAT 3 | Katana ML | Hot etching | 5.71 a | 0.86 | 4.42 | 5.66 | 7.04 |
| MET 1 | Metoxit Z-CAD HTL | Control | 10.34 d | 1.61 | 7.95 | 10.38 | 12.66 |
| MET 2 | Metoxit Z-CAD HTL | Air-borne particle abrasion | 11.07 d | 1.89 | 7.34 | 10.92 | 14.20 |
| MET 3 | Metoxit Z-CAD HTL | Hot etching | 5.53 a | 1.70 | 2.15 | 5.66 | 9.08 |
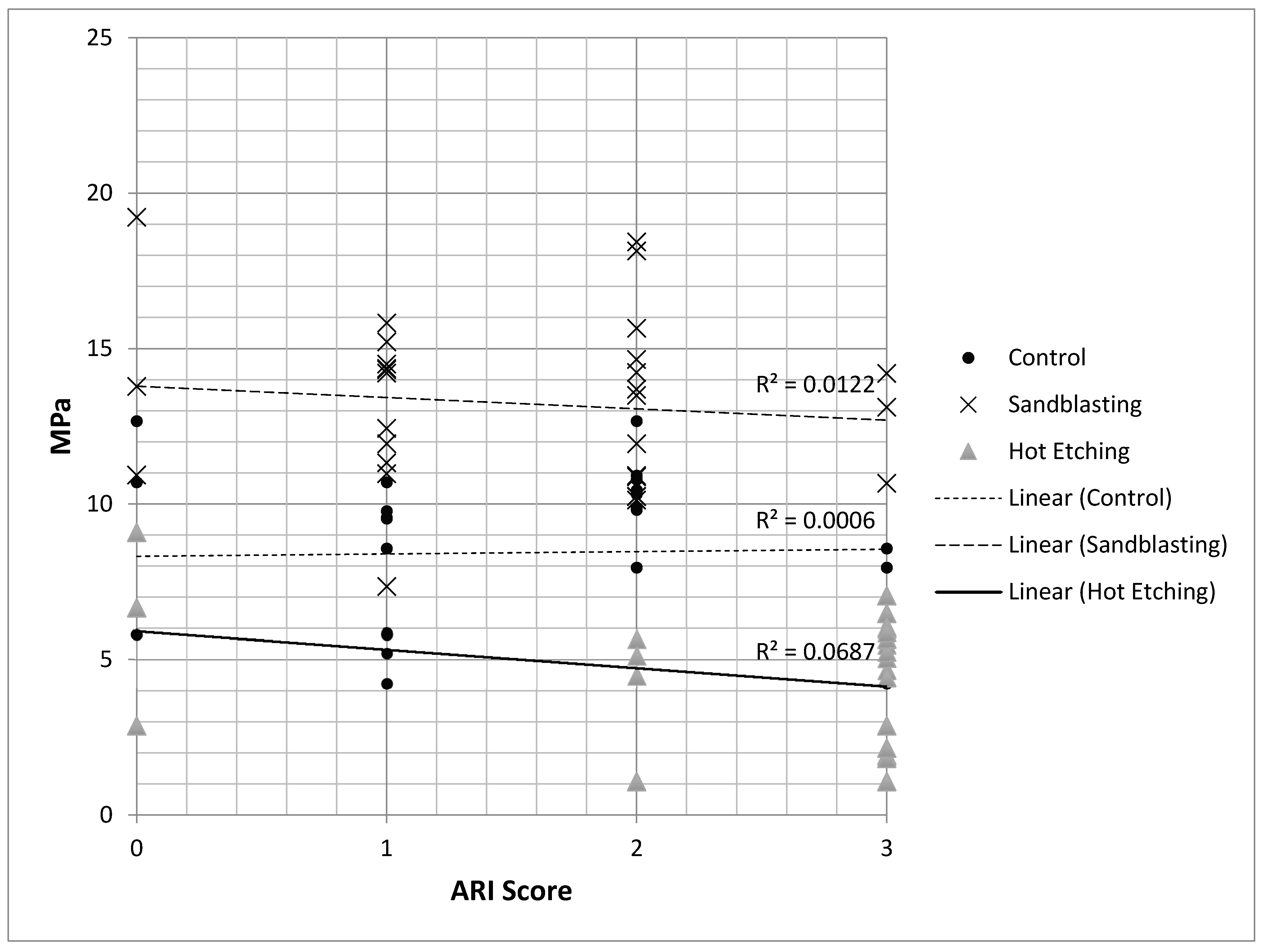
| Group | Zirconia Type | Condition | ARI = 0 | ARI = 1 | ARI = 2 | ARI = 3 |
|---|---|---|---|---|---|---|
| COP 1 | Copran Monolith HT | Control | 10.00 | 80.00 | 0.00 | 10.00 |
| COP 2 | Copran Monolith HT | ABPA | 10.00 | 70.00 | 10.00 | 10.00 |
| COP 3 | Copran Monolith HT | Hot etching | 10.00 | 0.00 | 10.00 | 80.00 |
| KAT 1 | Katana ML | Control | 20.00 | 60.00 | 10.00 | 10.00 |
| KAT 2 | Katana ML | ABPA | 10.00 | 10.00 | 70.00 | 10.00 |
| KAT 3 | Katana ML | Hot etching | 10.00 | 0.00 | 10.00 | 80.00 |
| MET 1 | Metoxit Z-CAD HTL | Control | 10.00 | 0.00 | 80.00 | 10.00 |
| MET 2 | Metoxit Z-CAD HTL | ABPA | 10.00 | 30.00 | 50.00 | 10.00 |
| MET 3 | Metoxit Z-CAD HTL | Hot etching | 10.00 | 0.00 | 20.00 | 70.00 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Colombo, M.; Gallo, S.; Padovan, S.; Chiesa, M.; Poggio, C.; Scribante, A. Influence of Different Surface Pretreatments on Shear Bond Strength of an Adhesive Resin Cement to Various Zirconia Ceramics. Materials 2020, 13, 652. https://doi.org/10.3390/ma13030652
Colombo M, Gallo S, Padovan S, Chiesa M, Poggio C, Scribante A. Influence of Different Surface Pretreatments on Shear Bond Strength of an Adhesive Resin Cement to Various Zirconia Ceramics. Materials. 2020; 13(3):652. https://doi.org/10.3390/ma13030652
Chicago/Turabian StyleColombo, Marco, Simone Gallo, Sara Padovan, Marco Chiesa, Claudio Poggio, and Andrea Scribante. 2020. "Influence of Different Surface Pretreatments on Shear Bond Strength of an Adhesive Resin Cement to Various Zirconia Ceramics" Materials 13, no. 3: 652. https://doi.org/10.3390/ma13030652
APA StyleColombo, M., Gallo, S., Padovan, S., Chiesa, M., Poggio, C., & Scribante, A. (2020). Influence of Different Surface Pretreatments on Shear Bond Strength of an Adhesive Resin Cement to Various Zirconia Ceramics. Materials, 13(3), 652. https://doi.org/10.3390/ma13030652







