Single-Crown, Short and Ultra-Short Implants, in Association with Simultaneous Internal Sinus Lift in the Atrophic Posterior Maxilla: A Three-Year Retrospective Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Inclusion Criteria
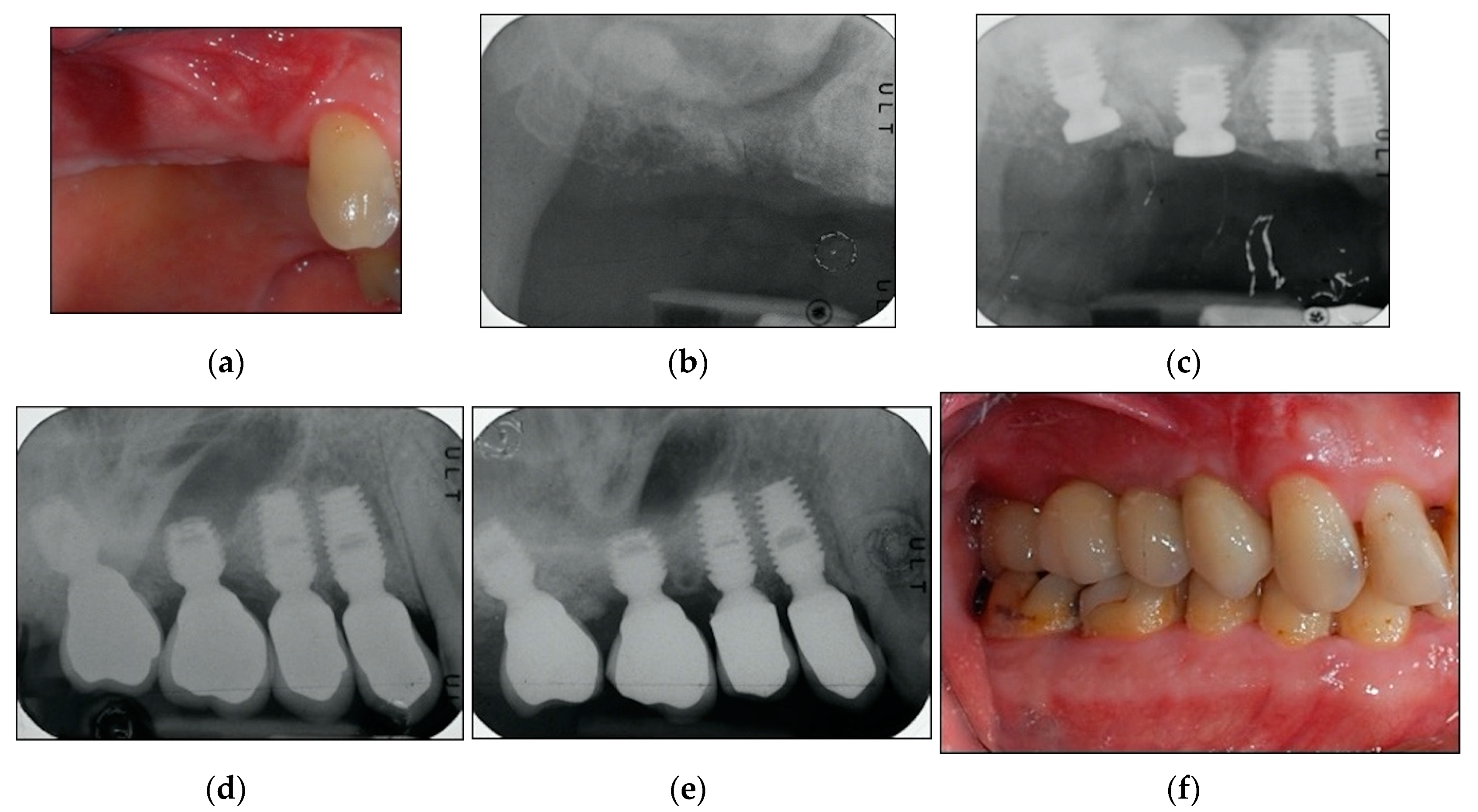
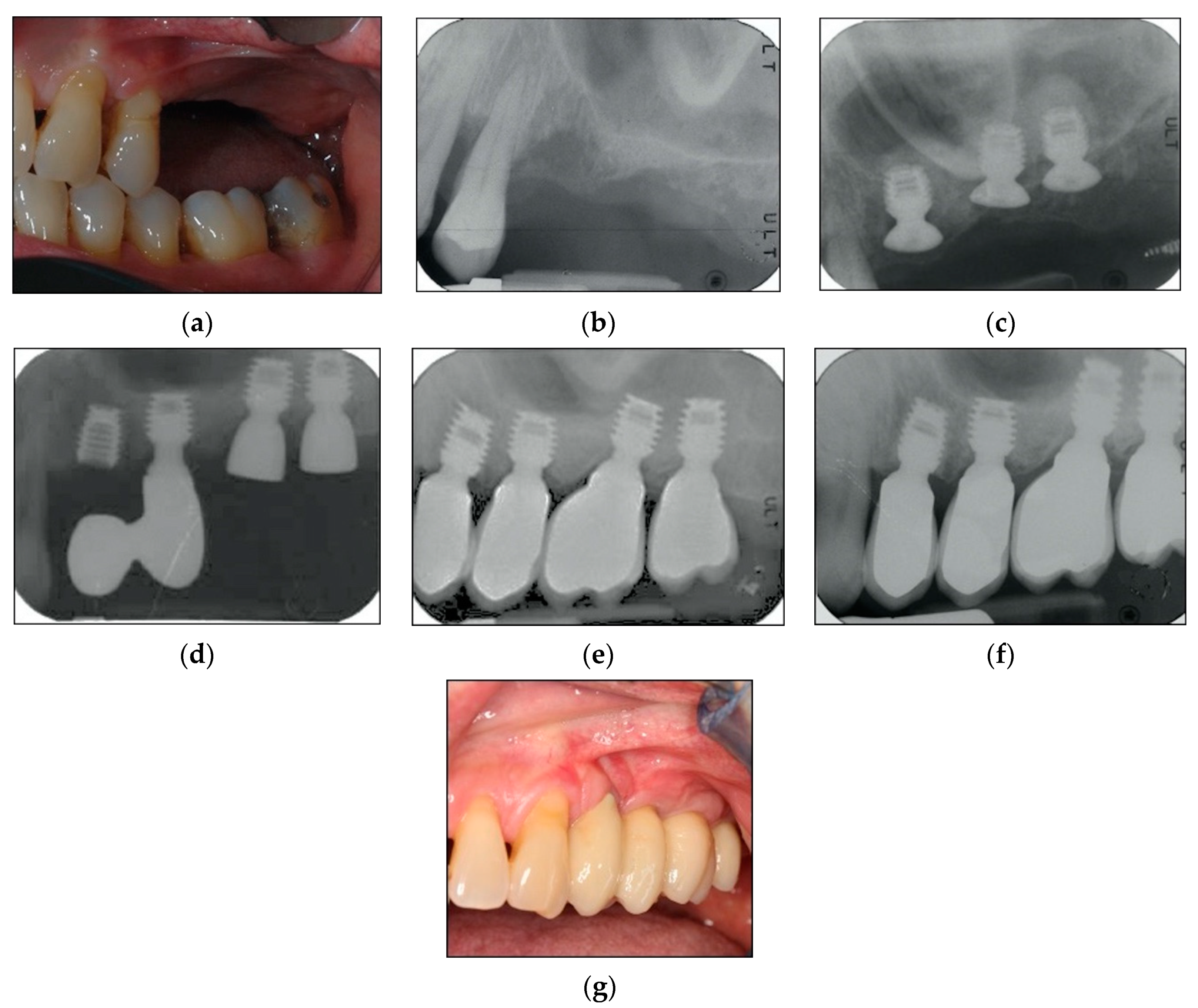
2.2. Surgical Protocol
2.3. Prosthetic Protocol and Follow-Up Evaluation
2.4. Study Variables and Outcomes
2.5. Statistical Analysis
3. Results
3.1. Demographics
3.2. Implant Survival
3.3. Radiographic Bone Levels
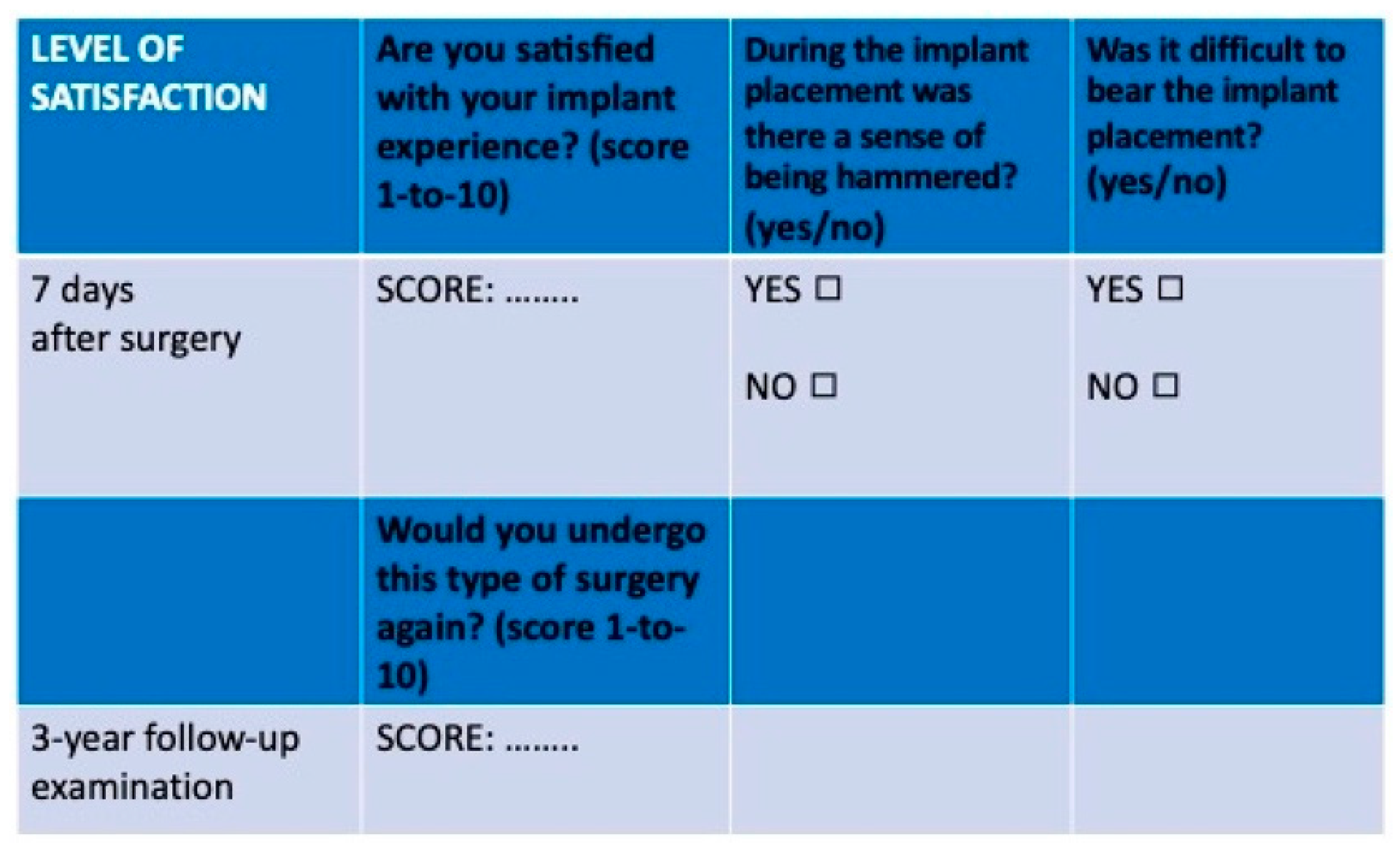
3.4. Patients’ Level of Satisfaction
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
Abbreviations
| RCBH | Residual crestal bone height |
| OSFE | Osteotome sinus floor elevation |
| ISL | Internal sinus lift technique |
| ASA | American Society of Anesthesiologists |
| CBCT | Cone beam computed tomography |
| CIR | Crown-to-implant ratio |
| IAI | Implant-abutment interface |
| CBL | Crestal bone level |
| F-BIC | First bone-to-implant contact |
| ∆-CBL | Average bone loss |
| ∆F-BIC | Average apical shift of the first bone-to-implant contact point position |
| SFL | Sinus floor level |
| av | Average |
| IBHG | Intra-sinus bone height gain |
| BPPV | Benign paroxysmal positional vertigo |
| SD | Standard deviation |
| iqr | Interquartile range |
References
- Chand, A.; Ronghe, B.; Byakod, G.; Lathi, A.A.; Muglikar, S. Relationship between inferior wall of maxillary sinus and maxillary posterior teeth using cone-beam computed tomography in healthy and chronic periodontitis patients. J. Indian Soc. Periodontol. 2017, 21, 466–472. [Google Scholar] [CrossRef] [PubMed]
- Kopecka, D.; Simunek, A.; Brazda, T.; Rota, M.; Slezak, R.; Capek, L. Relationship between subsinus bone height and bone volume requirements for dental implants: A human radiographic study. Int. J. Oral Maxillofac. Implant. 2012, 27, 48–54. [Google Scholar] [PubMed]
- Lundgren, S.; Cricchio, G.; Hallman, M.; Jungner, M.; Rasmusson, L.; Sennerby, L. Sinus floor elevation procedures to enable implant placement and integration: Techniques, biological aspects and clinical outcomes. Periodontology 2000 2017, 73, 103–120. [Google Scholar] [CrossRef] [PubMed]
- Pillai, S.; Ganapathy, D. Bone substitutes for sinus lift. J. Pharm. Sci. Res. 2016, 8, 367–372. [Google Scholar]
- Tatum, O.H., Jr. Maxillary and sinus implant reconstructions. Dent. Clin. North Am. 1986, 30, 207–229. [Google Scholar] [PubMed]
- Boyne, P.J.; James, R.A. Grafting of the maxillary sinus floor with autogenous marrow and bone. J. Oral Surg. 1980, 38, 613–616. [Google Scholar] [PubMed]
- Wallace, S.S.; Froum, S.J. Effect of maxillary sinus augmentation on the survival of endosseous dental implants. A systematic review. Ann. Periodontol. 2003, 8, 328–343. [Google Scholar] [CrossRef]
- Del Fabbro, M.; Testori, T.; Francetti, L.; Weinstein, R. Systematic review of survival rates for implants placed in the grafted maxillary sinus. Int. J. Periodontics Restor. Dent. 2004, 24, 565–577. [Google Scholar] [CrossRef]
- Corbella, S.; Taschieri, S.; Del Fabbro, M. Long-term outcomes for the treatment of atrophic posterior maxilla: A systematic review of literature. Clin. Implant. Dent. Relat. Res. 2015, 17, 120–132. [Google Scholar] [CrossRef]
- Farina, R.; Franceschetti, G.; Travaglini, D.; Consolo, U.; Minenna, L.; Schincaglia, G.P.; Riccardi, O.; Bandieri, A.; Maietti, E.; Trombelli, L. Morbidity following transcrestal and lateral sinus floor elevation: A randomized trial. J. Clin. Periodontol. 2018, 45, 1128–1139. [Google Scholar] [CrossRef]
- Regev, E.; Smith, R.A.; Perrot, D.H.; Pogrel, M.A. Maxillary sinus complications related to endosseous implants. Int. J. Oral Maxillofac. Implant. 1995, 10, 451–461. [Google Scholar]
- Schwartz-Arad, D.; Herzberg, R.; Dolev, E. The prevalence of surgical complications of the sinus graft procedure and their impact on implant survival. J. Periodontol. 2004, 75, 511–516. [Google Scholar] [CrossRef] [PubMed]
- Summers, R.B. A new concept in maxillary implant surgery: The osteotome technique. Compendium 1994, 15, 152–162. [Google Scholar] [PubMed]
- Summers, R.B. The osteotome technique: Part 2—The ridge expansion osteotomy (REO) procedure. Compendium 1994, 15, 422–436. [Google Scholar] [PubMed]
- Summers, R.B. The osteotome technique: Part 3—Less invasive methods of elevating the sinus floor. Compendium 1994, 15, 698–710. [Google Scholar]
- Summers, R.B. The osteotome technique: Part 4—Future site development. Compend. Contin. Educ. Dent. 1995, 16, 1090–1099. [Google Scholar]
- Emmerich, D.; Att, W.; Stappert, C. Sinus floor elevation using osteotomes: A systematic review and meta-analysis. J. Periodontol. 2005, 76, 1237–1251. [Google Scholar] [CrossRef]
- Del Fabbro, M.; Corbella, S.; Weinstein, T.; Ceresoli, V.; Taschieri, S. Implant survival rates after osteotome-mediated maxillary sinus augmentation: A systematic review. Clin. Implant. Dent. Relat. Res. 2012, 14, e159–e168. [Google Scholar] [CrossRef]
- Călin, C.; Petre, A.; Drafta, S. Osteotome-mediated sinus floor elevation: A systematic review and meta-analysis. Int. J. Oral Maxillofac. Implant. 2014, 29, 558–576. [Google Scholar] [CrossRef]
- Rosen, P.S.; Summers, R.; Mellado, J.R.; Salkin, L.M.; Shanaman, R.H.; Marks, M.H.; Fugazzotto, P.A. The bone-added osteotome sinus floor elevation technique: Multicenter retrospective report of consecutively treated patients. Int. J. Oral Maxillofac. Implant. 1999, 14, 853–858. [Google Scholar]
- Zitzmann, N.U.; Schärer, P. Sinus elevation procedures in the resorbed posterior maxilla. Comparison of the crestal and lateral approaches. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 1998, 85, 8–17. [Google Scholar] [CrossRef]
- Nedir, R.; Nurdin, N.; Abi Najm, S.; El Hage, M.; Bischof, M. Short implants placed with or without grafting into atrophic sinuses: The 5-year results of a prospective randomized controlled study. Clin. Oral Implant. Res. 2017, 28, 877–886. [Google Scholar] [CrossRef] [PubMed]
- Winter, A.A.; Pollack, A.S.; Odrich, R.B. Placement of implants in the severely atrophic posterior maxilla using localized management of the sinus floor: A preliminary study. Int. J. Oral Maxillofac. Implant. 2002, 17, 687–695. [Google Scholar]
- Chao, Y.L.; Chen, H.H.; Mei, C.C.; Tu, Y.K.; Lu, H.K. Meta-regression analysis of the initial bone height for predicting implant survival rates of two sinus elevation procedures. J. Clin. Periodontol. 2010, 37, 456–465. [Google Scholar] [CrossRef]
- Annibali, S.; Cristalli, M.P.; Dell’Aquila, D.; Bignozzi, I.; La Monaca, G.; Pilloni, A. Short dental implants: A systematic review. J. Dent. Res. 2012, 91, 25–32. [Google Scholar] [CrossRef]
- Nisand, D.; Renouard, F. Short implant in limited bone volume. Periodontology 2000 2014, 66, 72–96. [Google Scholar] [CrossRef]
- Thoma, D.S.; Haas, R.; Tutak, M.; Garcia, A.; Schincaglia, G.P.; Hämmerle, C.H.F. Randomized controlled multicentre study comparing short dental implants (6 mm) versus longer dental implants (11–15 mm) in combination with sinus floor elevation procedures. Part 1: Demographics and patient-reported outcomes at 1 year of loading. J. Clin. Periodontol. 2015, 42, 72–80. [Google Scholar] [CrossRef]
- Clelland, N.; Chaudhry, J.; Rashid, R.G.; McGlumphy, E. Split-mouth comparison of splinted and nonsplinted prostheses on short implants: 3-year results. Int. J. Oral Maxillofa. Implant. 2016, 31, 1135–1141. [Google Scholar] [CrossRef]
- Lombardo, G.; Signoriello, A.; Simancas-Pallares, M.; Marincola, M.; Nocini, P.F. Survival of short and ultra-short locking-taper implants supporting single crowns in the posterior mandible: A 3-year retrospective study. J. Oral Implantol. 2020. [Google Scholar] [CrossRef]
- Lombardo, G.; Pighi, J.; Marincola, M.; Corrocher, G.; Simancas-Pallares, M.; Nocini, P.F. Cumulative success rate of short and ultrashort implants supporting single crowns in the posterior maxilla: A 3-year retrospective study. Int. J. Dent. 2017, 8434281. [Google Scholar] [CrossRef]
- American Society of Anesthesiologists. Available online: https://www.asahq.org/standards-and-guidelines/asa-physical-status-classification-system (accessed on 20 April 2020).
- Wilson, D.; Wakefield, M.; Owen, N.; Roberts, L. Characteristics of heavy smokers. Prev. Med. 1992, 21, 311–319. [Google Scholar] [CrossRef]
- Lang, N.P.; Tonetti, M.S. Periodontal risk assessment (PRA) for patients in supportive periodontal therapy (SPT). Oral Health Prev. Dent. 2003, 1, 7–16. [Google Scholar] [PubMed]
- Romandini, M.; De Tullio, I.; Congedi, F.; Kalemaj, Z.; D’Ambrosio, M.; Laforí, A.; Quaranta, C.; Buti, J.; Perfetti, G. Antibiotic prophylaxis at dental implant placement: Which is the best protocol? A systematic review and network meta-analysis. J. Clin. Periodontol. 2019, 46, 382–395. [Google Scholar] [CrossRef]
- Dibart, S.; Warbington, M.; Su, M.F.; Skobe, Z. In vitro evaluation of the implant-abutment bacterial seal: The locking taper system. Int. J. Oral Maxillofac. Implant. 2005, 20, 732–737. [Google Scholar]
- Urdaneta, R.A.; Marincola, M. The integrated abutment crownt, a screwless and cementless restoration for single-tooth implants: A report on a new technique. J. Prosthodont. 2007, 16, 311–318. [Google Scholar] [CrossRef] [PubMed]
- Mangano, F.; Shibli, J.A.; Sammons, R.L.; Iaculli, F.; Piattelli, A.; Mangano, C. Short (8-mm) locking-taper implants supporting single crowns in posterior region: A prospective clinical study with 1-to 10-years of follow-up. Clin. Oral Implant. Res. 2014, 25, 933–940. [Google Scholar] [CrossRef]
- Urdaneta, R.A.; Daher, S.; Leary, J.; Emanuel, K.M.; Chuang, S.K. The survival of ultrashort locking-taper implants. Int. J. Oral Maxillofac. Implant. 2012, 27, 644–654. [Google Scholar]
- Maiorana, C.; Farronato, D.; Pieroni, S.; Cicciu, M.; Andreoni, D.; Santoro, F. A four-year survival rate multicenter prospective clinical study on 377 implants: Correlations between implant insertion torque, diameter, and bone quality. J. Oral Implantol. 2015, 41, e60–e65. [Google Scholar] [CrossRef]
- Galgali, S.R.; Gontiya, G. Evaluation of an innovative radiographic technique--parallel profile radiography--to determine the dimensions of dentogingival unit. Indian J. Dent. Res. 2011, 22, 237–241. [Google Scholar] [CrossRef]
- Malchiodi, L.; Cucchi, A.; Ghensi, P.; Consonni, D.; Nocini, P.F. Influence of crown-implant ratio on implant success rates and crestal bone levels: A 36-month follow-up prospective study. Clin. Oral Implant. Res. 2014, 25, 240–251. [Google Scholar] [CrossRef]
- Urdaneta, R.A.; Rodriguez, S.; McNeil, D.C.; Weed, M.; Chuang, S.K. The effect of increased crown-to-implant ratio on single-tooth locking-taper implants. Int. J. Oral Maxillofac. Implant. 2010, 25, 729–743. [Google Scholar]
- Birdi, H.; Schulte, J.; Kovacs, A.; Weed, M.; Chuang, S.K. Crown-to-implant ratios of short-length implants. J. Oral Implantol. 2010, 36, 425–433. [Google Scholar] [CrossRef] [PubMed]
- Blanes, R.J.; Bernard, J.P.; Blanes, Z.M.; Belser, U.C. A 10 year prospective study of ITI dental implants placed in the posterior region. II: Influence of the crown-to-implant ratio and different prosthetic treatment modalities on crestal bone loss. Clin. Oral Implant. Res. 2007, 18, 707–714. [Google Scholar] [CrossRef] [PubMed]
- Si, M.S.; Zhuang, L.F.; Gu, Y.X.; Mo, J.J.; Qiao, S.C.; Lai, H.C. Osteotome sinus floor elevation with or without grafting: A 3-year randomized controlled clinical trial. J. Clin. Periodontol. 2013, 40, 396–403. [Google Scholar] [CrossRef] [PubMed]
- Teng, M.; Liang, X.; Yuan, Q.; Nie, J.; Ye, J.; Cheng, Q.; Zhai, J.; Liao, J.; Sun, X.; Wen, C.; et al. The inlay osteotome sinus augmentation technique for placing short implants simultaneously with reduced crestal bone height. A short-term follow-up. Clin. Implant. Dent. Relat. Res. 2013, 15, 918–926. [Google Scholar] [CrossRef] [PubMed]
- Voutilanen, A.; Pitkäaho, T.; Kvist, T.; Vehviläinen-Julkunen, K. How to ask about patient satisfaction? The visual analogue scale is less vulnerable to confounding factors and ceiling effect than a symmetric Likert scale. J. Adv. Nurs. 2016, 72, 946–957. [Google Scholar] [CrossRef]
- StataCorp. Stata Statistical Software: Release 15; StataCorp LLC: College Station, TX, USA, 2017. [Google Scholar]
- Gonzalez, S.; Tuan, M.C.; Ahn, K.M.; Nowzari, H. Crestal approach for maxillary sinus augmentation in patients with ≤ 4 mm of residual alveolar bone. Clin Implant. Dent. Relat Res. 2014, 16, 827–835. [Google Scholar] [CrossRef]
- Soydan, S.S.; Cubuk, S.; Bayrak, B.; Uckan, S. Comparative evaluation of simultaneous maxillary sinus floor elevation and implant placement with residual bone heights greater or less than 5 mm. Int. J. Oral Maxillofac. Implant. 2015, 30, 179–183. [Google Scholar] [CrossRef]
- Smiler, D.G.; Jonhson, P.W.; Lozada, J.L.; Misch, C.; Rosenlicht, J.L.; Tatum, O.H., Jr.; Wagner, J.R. Sinus lift grafts and endosseous implants. Treatment of the atrophic posterior maxilla. Dent. Clin. North Am. 1992, 36, 151–186. [Google Scholar]
- Garg, A.K. Augmentation grafting of the maxillary sinus for placement of dental implants: Anatomy, physiology, and procedures. Implant. Dent. 1999, 8, 36–46. [Google Scholar] [CrossRef]
- Pjetursson, B.E.; Rast, C.; Bragger, U.; Schmidlin, K.; Zwahlen, M.; Lang, N.P. Maxillary sinus floor elevation using the (transalveolar) osteotome technique with or without grafting material. Part I: Implant survival and patients’ perception. Clin. Oral Implant. Res. 2009, 20, 667–676. [Google Scholar] [CrossRef] [PubMed]
- Nkenke, E.; Stelzle, F. Clinical outcomes of sinus floor augmentation for implant placement using autogenous bone or bone substitutes: A systematic review. Clin. Oral Implant. Res. 2009, 20, 124–133. [Google Scholar] [CrossRef] [PubMed]
- Toffler, M. Treating the atrophic posterior maxilla by combining short implants with minimally invasive osteotome procedures. Pract. Proced. Aesthet. Dent. 2006, 18, 301–308. [Google Scholar] [PubMed]
- Anitua, E.; Pinas, L.; Orive, G. Retrospective study of short and extra-short implants placed in posterior regions: Influence of crown-to-implant ratio on marginal bone loss. Clin. Implant. Dent. Relat. Res. 2015, 17, 102–110. [Google Scholar] [CrossRef]
- Reiser, G.M.; Rabinovitz, Z.; Bruno, J.; Damoulis, P.D.; Griffin, T.J. Evaluation of maxillary sinus membrane response following elevation with the crestal osteotome technique in human cadavers. Int. J. Oral Maxillofac. Implant. 2001, 16, 833–840. [Google Scholar]
- Boffano, P.; Forouzanfar, T. Current concepts on complications associated with sinus augmentation procedures. J. Craniofac. Surg. 2014, 25, e210–e212. [Google Scholar] [CrossRef]
- Pozzi, A.; Agliardi, E.; Tallarico, M.; Barlattani, A. Clinical and radiological outcomes of two implants with different prosthetic interfaces and neck configurations: Randomized, controlled, split-mouth clinical trial. Clin. Implant. Dent. Relat. Res. 2014, 16, 96–106. [Google Scholar] [CrossRef]
- Corrente, G.; Abundo, R.; des Ambrois, A.B.; Savio, L.; Perelli, M. Short porous implants in the posterior maxilla: A 3-year report of a prospective study. Int. J. Periodontics Restor. Dent. 2009, 29, 23–29. [Google Scholar]
- Surapaneni, H.; Yalamanchili, P.S.; Basha, M.H.; Potluri, S.; Elisetti, N.; Kiran Kumar, M.V. Antibiotics in dental implants: A review of literature. J. Pharm. Bioallied Sci. 2016, 8, S28–S31. [Google Scholar]
- Crespi, R.; Caparrè, P.; Gherlone, E. Sinus floor elevation by osteotome: Hand mallet versus electric mallet. A prospective clinical study. Int. J. Oral Maxillofac. Implant. 2012, 27, 1144–1150. [Google Scholar]
- Peñarrocha-Diago, M.; Rambla-Ferrer, J.; Perez, V.; Pérez-Garrigues, H. Benign paroxysmal vertigo secondary to placement of maxillary implants using the alveolar expansion technique with osteotomes: A study of 4 cases. Int. J. Oral Maxillofac. Implant. 2008, 23, 129–132. [Google Scholar]
- Leonetti, J.A.; Rambo, H.M.; Throndson, R.R. Osteotome sinus elevation and implant placement with narrow size bioactive glass. Implant. Dent. 2000, 9, 177–182. [Google Scholar] [CrossRef] [PubMed]


| VARIABLE | Overall (N = 51) | 5 mm (N = 21) | 6 mm (N = 23) | 8 mm (N = 7) | p-Value | ||||
|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | ||
| SEX | |||||||||
| Male | 20 | 39.22 | 9 | 42.86 | 7 | 30.43 | 4 | 57.14 | 0.42 |
| Female | 31 | 60.78 | 12 | 57.14 | 16 | 69.57 | 3 | 42.86 | |
| AGE AT FOLLOW-UP | 56.22 ± 18.86 | 56.68 ± 11.11 | 58.04 ± 9.99 | 62.70 ± 9.26 | 0.35 | ||||
| MONTHS AT LOADING TIME | 11.50 ± 5.54 | 12.47 ± 5.49 | 11.30 ± 5.70 | 9.28 ± 5.18 | 0.41 | ||||
| MONTHS AT FOLLOW-UP TIME | 42.86 ± 20.33 | 41.04 ± 17.52 | 43.73 ± 23.31 | 45.42 ± 20.14 | 0.85 | ||||
| SMOKING | |||||||||
| No | 42 | 82.35 | 15 | 71.43 | 20 | 86.96 | 7 | 100.00 | 0.23 |
| Yes | 9 | 17.65 | 6 | 28.57 | 3 | 13.04 | 0 | 0.00 | |
| ASA STATUS | |||||||||
| I | 20 | 39.22 | 7 | 33.33 | 12 | 52.17 | 1 | 14.29 | 0.17 |
| II | 31 | 60.78 | 14 | 66.67 | 11 | 47.83 | 6 | 85.71 | |
| ORAL HYGIENE SESSIONS/YEAR | 3.11 ± 1.05 | 2.95 ± 1.16 | 3.30 ± 0.97 | 3.00 ± 1.00 | 0.52 | ||||
| INTERPROXIMAL ORAL HYGIENE | |||||||||
| No | 10 | 19.61 | 3 | 14.29 | 5 | 21.74 | 2 | 28.57 | 0.74 |
| Yes | 41 | 80.39 | 18 | 85.71 | 18 | 78.26 | 5 | 71.43 | |
| HISTORY OF PERIODONTAL DISEASE | |||||||||
| No | 14 | 27.45 | 5 | 23.81 | 8 | 34.78 | 1 | 14.29 | 0.57 |
| Yes | 37 | 72.55 | 16 | 76.19 | 15 | 65.22 | 6 | 85.71 | |
| TYPE OF TOOTH | |||||||||
| Premolar | 13 | 25.49 | 5 | 23.81 | 3 | 13.04 | 5 | 71.43 | 0.01 |
| Molar | 38 | 75.51 | 16 | 76.19 | 20 | 86.96 | 2 | 28.57 | |
| IMPLANT DIAMETER | |||||||||
| 4 mm | 2 | 3.92 | 2 | 9.52 | 0 | 0.00 | 0 | 0.00 | <0.001 |
| 4.5 mm | 15 | 29.41 | 0 | 0.00 | 8 | 34.78 | 7 | 100.00 | |
| 5 mm | 29 | 56.86 | 14 | 66.67 | 15 | 65.22 | 0 | 0.00 | |
| 6 mm | 5 | 9.8 | 5 | 23.81 | 0 | 0.00 | 0 | 0.00 | |
| PROSTHETIC MATERIAL | |||||||||
| Resin | 7 | 13.73 | 5 | 23.81 | 1 | 4.35 | 1 | 14.29 | 0.15 |
| Porcelain | 44 | 86.27 | 16 | 76.19 | 22 | 95.65 | 6 | 85.71 | |
| CROWN-TO-IMPLANT RATIO | |||||||||
| <2 | 26 | 50.98 | 5 | 23.81 | 14 | 60.87 | 7 | 100.00 | 0.01 |
| 2–2.99 | 16 | 31.37 | 7 | 33.33 | 9 | 39.13 | 0 | 0.00 | |
| >2.99 | 9 | 17.65 | 9 | 42.86 | 0 | 0.00 | 0 | 0.00 | |
| VARIABLE | Implant Survival | Implant Failure | p-Value | ||
|---|---|---|---|---|---|
| n | % | n | % | ||
| SEX | |||||
| Male | 20 | 100.00 | 0 | 0.00 | 0.51 |
| Female | 29 | 93.55 | 2 | 6.45 | |
| SMOKING | |||||
| No | 41 | 97.62 | 1 | 2.38 | 0.32 |
| Yes | 8 | 88.89 | 1 | 11.11 | |
| ASA STATUS | |||||
| I | 19 | 95.00 | 1 | 5.00 | 0.63 |
| II | 30 | 96.77 | 1 | 3.23 | |
| ORAL HYGIENE SESSIONS/YEAR | 3.47 ± 0.32 | 2.88 ± 0.65 | 0.15 | ||
| INTERPROXIMAL ORAL HYGIENE | |||||
| No | 10 | 100.00 | 0 | 0.00 | 0.64 |
| Yes | 39 | 95.12 | 2 | 4.88 | |
| HISTORY OF PERIODONTAL DISEASE | |||||
| No | 13 | 92.86 | 1 | 7.14 | 0.47 |
| Yes | 36 | 97.30 | 1 | 2.70 | |
| IMPLANT LENGTH | |||||
| 5 mm | 21 | 100.00 | 0 | 0.00 | 0.62 |
| 6 mm | 21 | 91.30 | 2 | 8.70 | |
| 8 mm | 7 | 100.00 | 0 | 0.00 | |
| IMPLANT DIAMETER | 0.89 | ||||
| 4 mm | 2 | 100.00 | 0 | 0.00 | |
| 4.5 mm | 14 | 93.33 | 1 | 6.67 | |
| 5 mm | 28 | 96.55 | 1 | 3.45 | |
| 6 mm | 5 | 100.00 | 0 | 0.00 | |
| TYPE OF TOOTH | |||||
| Premolar | 13 | 100.00 | 0 | 0.00 | 0.55 |
| Molar | 36 | 94.74 | 2 | 5.26 | |
| PROSTHETIC MATERIAL | |||||
| Resin | 6 | 85.71 | 1 | 14.29 | 0.25 |
| Porcelain | 43 | 97.73 | 1 | 2.27 | |
| CROWN-TO-IMPLANT RATIO | |||||
| <2 | 25 | 96.15 | 1 | 3.85 | 0.74 |
| 2–2.99 | 15 | 93.75 | 1 | 6.25 | |
| >2.99 | 9 | 100.00 | 0 | 0.00 | |
| PRE-OPERATIVE | AFTER IMPLANT PLACEMENT | p-Value | AFTER LOADING | p-Value | AT 3-YEAR FOLLOW-UP | p-Value | |
|---|---|---|---|---|---|---|---|
| RCBH | 5.20(1.41) [10.66;2.74] | 10.27(2.15) [15.08;7.81] | <0.001 | 8.88(2.35) [15.00;6.09] | <0.001 | 7.59(1.97) [14.27;5.23] | <0.001 |
| IBHG | 4.84 ± 1.38 [8.02;2.17] | 3.96 ± 1.25 [6.33;1.19] | <0.001 | 3.17 ± 1.13 [6.01;0.76] | <0.001 | ||
| CBL | 1.87(0.93) [4.14;0.15] | 1.46(0.81) [3.39;0.45] | <0.001 | 1.09(0.86) [3.24;−1.92] | <0.001 | ||
| F-BIC | 0.26(0.33) [1.08;−1.34] | 0.37(0.45) [1.92;−0.31] | <0.001 |
| VARIABLE | Overall | 5 mm | 6 mm | 8 mm | p-Value |
|---|---|---|---|---|---|
| RCBH | |||||
| Pre-operative | 5.20(1.41) [10.66;2.74] | 5.43(1.13) [10.66;2.97] | 5.20(1.36) [10.30;2.74] | 4.92(2.86) [7.68;4.07] | 0.87 |
| After implant placement | 10.27(2.15) [15.08;7.81] | 10.27(2.13) [15.01;8.01] | 10.12(2.31) [15.08;7.95] | 10.52(4.29) [13.53;7.81] | 0.97 |
| After loading | 8.88(2.35) [15.00;6.09] | 9.54(1.91) [12.16;6.34] | 8.88(2.28) [15.00;6.09] | 8.83(3.12) [10.84;6.26] | 0.87 |
| At 3-year follow-up | 7.59(1.97) [14.27;5.23] | 7.75(1.61) [11.92;5.23] | 7.34(1.97) [14.27;5.69] | 7.12(3.34) [9.58;5.94] | 0.73 |
| IBHG | |||||
| After implant placement | 4.84 ± 1.38 [8.02;2.17] | 4.74 ± 1.27 [8.02;3.01] | 4.84 ± 1.48 [7.69;2.17] | 5.12 ± 1.53 [7.5;3.35] | 0.82 |
| After loading | 3.96 ± 1.25 [6.33;1.19] | 3.81 ± 1.17 [6.2;1.98] | 3.99 ± 1.36 [5.86;1.18] | 4.3 ± 1.21 [6.33;3.01] | 0.67 |
| At 3-year follow-up | 3.17 ± 1.13 [6.01;0.76] | 2.95 ± 1.07 [6.01;1.59] | 3.35 ± 1.27 [5.2;0.76] | 3.22 ± 0.75 [4.69;2.2] | 0.51 |
| CBL | |||||
| After implant placement | 1.87(0.93) [4.14;0.15] | 1.89(1.22) [4.14;0.15] | 1.84(0.78) [3.12;1.19] | 1.87(1.01) [3.11;0.83] | 0.98 |
| After loading | 1.46(0.81) [3.39;0.45] | 1.70(0.80) [3.39;0.45] | 1.38(0.81) [2.58;0.70] | 1.23(0.61) [2.52;0.67] | 0.28 |
| At 3-year follow-up | 1.09(0.86) [3.24;−1.92] | 1.33(0.65) [3.24;−0.04] | 1.09(0.86) [2.76;−1.92] | 0.62(0.84) [2.43;−0.00] | 0.2 |
| F-BIC | |||||
| After loading | 0.26(0.33) [1.08;−1.34] | 0.26(0.40) [1.08;0.00] | 0.25(0.33) [0.72;−1.34] | 0.27(0.32) [1.04;−1.03] | 0.9 |
| At 3-year follow-up | 0.37(0.45) [1.92;−0.31] | 0.36(0.35) [1.42;0.00] | 0.42(0.42) [1.92;−0.31] | 0.37(0.43) [0.84;0.18] | 0.59 |
| PRE-OPERATIVE | AT 3-YEAR FOLLOW-UP | p-Value | |
|---|---|---|---|
| SATISFACTION SCORES | 8(2) [10;5] | 9(1) [10;7] | <0.001 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lombardo, G.; Marincola, M.; Signoriello, A.; Corrocher, G.; Nocini, P.F. Single-Crown, Short and Ultra-Short Implants, in Association with Simultaneous Internal Sinus Lift in the Atrophic Posterior Maxilla: A Three-Year Retrospective Study. Materials 2020, 13, 2208. https://doi.org/10.3390/ma13092208
Lombardo G, Marincola M, Signoriello A, Corrocher G, Nocini PF. Single-Crown, Short and Ultra-Short Implants, in Association with Simultaneous Internal Sinus Lift in the Atrophic Posterior Maxilla: A Three-Year Retrospective Study. Materials. 2020; 13(9):2208. https://doi.org/10.3390/ma13092208
Chicago/Turabian StyleLombardo, Giorgio, Mauro Marincola, Annarita Signoriello, Giovanni Corrocher, and Pier Francesco Nocini. 2020. "Single-Crown, Short and Ultra-Short Implants, in Association with Simultaneous Internal Sinus Lift in the Atrophic Posterior Maxilla: A Three-Year Retrospective Study" Materials 13, no. 9: 2208. https://doi.org/10.3390/ma13092208
APA StyleLombardo, G., Marincola, M., Signoriello, A., Corrocher, G., & Nocini, P. F. (2020). Single-Crown, Short and Ultra-Short Implants, in Association with Simultaneous Internal Sinus Lift in the Atrophic Posterior Maxilla: A Three-Year Retrospective Study. Materials, 13(9), 2208. https://doi.org/10.3390/ma13092208






