Synthetic Material for Bone, Periodontal, and Dental Tissue Regeneration: Where Are We Now, and Where Are We Heading Next?
Abstract
:1. Introduction
2. Calcium Compounds
2.1. Calcium Phosphate Cements
2.2. β-Tricalcium Phosphate Ceramic and Biphasic Calcium Phosphate
2.3. Calcium Sulphate and β-Tricalcium Phosphate
- Non-requirement of a membrane leading to reduced surgical time and cost;
- Self-stabilizing through hardening;
- Suitable resorption profile allowing cell occlusive properties, adequate porosity, volume maintenance and high rate of turnover to new host bone.
3. Bioactive Glasses
4. Polymer-Based Bone Substitutes
- A. Development
- B. Synthetic polymer biomaterials
4.1. Poly(Methyl Methacrylate) (PMMA)
4.2. Polycaprolactone (PCL)
4.3. Poly(Lactic Acid) (PLA), Polyglycolic Acid (PGA), and Poly(Lacticco-Glycolic Acid) (PLGA)
5. Discussion and Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Campana, V.; Milano, G.; Pagano, E.; Barba, M.; Cicione, C.; Salonna, G.; Lattani, W.; Logroscino, G. Bone substitutes in orthopaedic surgery: From basic science to clinical practice. J. Mater. Sci. Mater. Med. 2014, 25, 2445–2461. [Google Scholar] [CrossRef]
- Zhao, R.; Yang, R.; Cooper, P.R.; Khurshid, Z.; Shavandi, A.; Ratnayake, J. Bone grafts and substitutes in dentistry: A review of current trends and developments. Molecules 2021, 26, 3007. [Google Scholar] [CrossRef]
- Murata, M. Bone engineering using human demineralized dentin matrix and recombinant human BMP-2. J. Hard Tissue Biol. 2005, 14, 80–81. [Google Scholar] [CrossRef] [Green Version]
- Murata, M.; Sato, D.; Hino, J.; Akazawa, T.; Tazaki, J.; Ito, K.; Arisue, M. Acid-insoluble human dentin as carrier material for recombinant human BMP-2. J. Biomed. Mater. Res. Part A 2012, 100, 571–577. [Google Scholar] [CrossRef]
- Binderman, I.; Hallel, G.; Nardy, C.; Yaffe, A.; Sapoznikof, L. A novel procedure to process extracted teeth for immediate grafting autogenous dentin. J. Interdiscip. Med. Dent. Sci. 2014, 2, 154–158. [Google Scholar]
- Koga, T.; Minamizato, T.; Kawai, Y.; Muira, K.I.; Takashi, I.; Nakatani, Y.; Sumita, Y.; Asahina, I. Bone regeneration using dentin matrix depends on the degree of demineralization and particle size. PLoS ONE 2016, 11, e0147235. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kabir, M.A.; Murata, M.; Kusano, K.; Zakaria, S.M.; Noor, A.H.M.; Khuda, F.; Hossain, I.; Sultana, S.; Saito, T. Radiological evaluation of human dentin autografts in Bangladesh. J. Hard Tissue Biol. 2014, 23, 363–370. [Google Scholar] [CrossRef] [Green Version]
- Bernardi, S.; Macchiarelli, G.; Bianchi, S. Autologous materials in regenerative dentistry: Harvested bone, platelet concentrates and dentin derivates. Molecules 2020, 25, 5330. [Google Scholar] [CrossRef]
- Xiao, W.; Hu, C.; Rong, S.; Zhu, C.; Wu, Y. Application of dentin in bone tissue engineering. J. Prev. Treat. Stomatol. Dis. 2020, 12, 127–130. [Google Scholar]
- Roberts-Clark, D.; Smith, A.J. Angiogenic growth factors in human dentine matrix. Arch. Oral Biol. 2000, 45, 1013–1016. [Google Scholar] [CrossRef]
- Um, I.W.; Kim, Y.K.; Mitsugi, M. Demineralized dentin matrix scaffolds for alveolar bone engineering. J. Indian Prosthodont. Soc. 2017, 17, 120–127. [Google Scholar] [CrossRef]
- Silva, T.A.; Rosa, A.L.; Lara, V.S. Dentin matrix proteins and soluble factors: Intrinsic regulatory signals for healing and resorption of dental and periodontal tissues? Oral Diseases. 2004, 10, 63–74. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.K.; Kim, S.G.; Byeon, J.H.; Lee, H.J.; Um, I.U.; Lim, S.C.; Kim, S.Y. Development of a novel bone grafting material using autogenous teeth. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontol. 2010, 109, 496–503. [Google Scholar] [CrossRef] [PubMed]
- Park, S.M.; Um, I.W.; Kim, Y.K.; Kim, K.W. Clinical application of auto-tooth bone graft material. J. Korean Assoc. Oral Maxillofac. Surg. 2012, 38, 2–8. [Google Scholar] [CrossRef] [Green Version]
- Kim, Y.K.; Lee, H.J.; Kim, K.W.; Kim, S.G.; Um, I.W. Guide bone regeneration using autogenous teeth. J. Korean Assoc. Oral Maxillofac. Surg. 2011, 37, 142–147. [Google Scholar] [CrossRef] [Green Version]
- Han, M.W.; Lee, J.K. Clinical study on the efficacy of the autogenous tooth bone graft material (AutoBT). Maxillofac. Plast. Reconstr. Surg. 2013, 35, 221–226. [Google Scholar]
- Kim, Y.K.; Lee, J.H.; Um, I.W.; Cho, W.J. Guided bone regeneration using demineralized dentin matrix: Long-term follow-up. J. Oral Maxillofac. Surg. 2016, 74. [Google Scholar] [CrossRef]
- Lee, J.Y.; Kim, Y.K.; Yi, Y.J.; Choi, J.H. Clinical evaluation of ridge augmentation using autogenous tooth bone graft material: Case series study. J. Korean Assoc. Oral Maxillofac. Surg. 2013, 39, 156–160. [Google Scholar] [CrossRef] [Green Version]
- Palma, P.J.; Matos, S.; Ramos, J.; Guerra, F.; Figueiredo, M.H.; Kauser, J. New formulations for space provision and bone regeneration. Biodental Eng. I 2010, 1, 71–76. [Google Scholar]
- Tsapikouni, T.S.; Missirlis, Y.F. Protein-material interactions: From micro-to-nano scale. Mater. Sci. Eng. B 2008, 152, 2–7. [Google Scholar] [CrossRef]
- Riddle, R.C.; Taylor, A.F.; Genetos, D.C.; Donahue, H.J. MAP kinase and calcium signaling mediate fluid flow-induced human mesenchymal stem cell proliferation. Am. J. Physiol.-Cell Physiol. 2006, 290, C776–C784. [Google Scholar] [CrossRef]
- Kuroda, Y.; Hisatsune, C.; Nakamura, T.; Matsuo, K.; Mikoshiba, K. Osteoblasts induce Ca2+ oscillation-independent NFATc1 activation during osteoclastogenesis. Proc. Natl. Acad. Sci. USA 2008, 105, 8643–8648. [Google Scholar] [CrossRef] [Green Version]
- Zhang, R.; Lu, Y.; Ye, L.; Yuan, B.; Yu, S.; Qin, C.; Xie, Y.; Gao, T.; Drezner, M.K.; Bonewald, L.F.; et al. Unique roles of phosphorus in endochondral bone formation and osteocyte maturation. J. Bone Miner. Res. 2011, 26, 1047–1056. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brown, L.; Brown, W.E.; Chow, L.; Brown, W.E. A new calcium phosphate, water-setting cement. Cem. Res. Prog. 1987, 351–379. [Google Scholar]
- Jeong, J.; Kim, J.H.; Shim, J.H.; Hwang, N.S.; Heo, C.Y. Bioactive calcium phosphate materials and applications in bone regeneration. Biomater. Res. 2019, 23, 4. [Google Scholar] [CrossRef] [Green Version]
- Ambard, A.J.; Mueninghoff, L. Calcium phosphate cement: Review of mechanical and biological properties. J. Prosthodont. 2006, 15, 321–328. [Google Scholar] [CrossRef]
- Wu, X.; Tang, Z.; Wu, K.; Bai, Y.; Lin, X.; Yang, H.; Yang, Q.; Wang, Z.; Ni, X.; Liu, H.; et al. Strontium-calcium phosphate hybrid cement with enhanced osteogenic and angiogenic properties for vascularised bone regeneration. J. Mater. Chem. B 2021, 9, 5982–5997. [Google Scholar] [CrossRef] [PubMed]
- Legeros, R.Z. Properties of osteoconductive biomaterials: Calcium phosphates. Clin. Orthop. Relat. Res. 2002, 395, 81–98. [Google Scholar] [CrossRef] [PubMed]
- Lodoso-Torrecilla, I.; Klein Gunnewiek, R.; Grosfeld, E.C.; de Vries, R.B.M.; Habibović, P.; Jansen, J.A.; van den Beucken, J.J. Bioinorganic supplementation of calcium phosphate-based bone substitutes to improve in vivo performance: A systematic review and meta-analysis of animal studies. Biomater. Sci. 2020, 8, 4792–4809. [Google Scholar] [CrossRef]
- Fernandez de Grado, G.; Keller, L.; Idoux-Gillet, Y.; Wagner, Q.; Musset, A.M.; Benkirane-Jessel, N.; Bornert, F.; Offner, D. Bone substitutes: A review of their characteristics, clinical use, and perspectives for large bone defects management. J. Tissue Eng. 2018, 9, 1–18. [Google Scholar] [CrossRef] [Green Version]
- Burguera, E.F.; Xu, H.H.; Weir, M.D. Injectable and rapid-setting calcium phosphate bone cement with dicalcium phosphate dihydrate. J. Biomed. Mater. Res. Part B Appl. Biomater. 2006, 77, 126–134. [Google Scholar] [CrossRef] [PubMed]
- Russell, T.A.; Leighton, R.K. Comparison of autogenous bone graft and endothermic calcium phosphate cement for defect augmentation in tibial plateau fractures. A multicenter, prospective, randomized study. J. Bone Jt. Surg. 2008, 90, 2057–2061. [Google Scholar] [CrossRef] [PubMed]
- Ben-Nissan, B. Advances in Calcium Phosphate Biomaterials; Springer: Berlin/Heidelberg, Germany, 2014; p. 74. [Google Scholar]
- Afifi, A.M.; Gordon, C.R.; Pryor, L.S.; Sweeney, W.; Papay, F.A.; Zins, J.E. Calcium phosphate cements in skull reconstruction: A meta-analysis. Plast. Reconstr. Surg. 2010, 126, 1300–1309. [Google Scholar] [CrossRef]
- Horowitz, R.A.; Leventis, M.D.; Rohrer, M.D.; Prasad, H.S. Bone grafting: History, rationale, and selection of materials and techniques. Compend. Contin. Educ. Dent. 2014, 35 (Suppl. 4), 1–6. [Google Scholar] [PubMed]
- Zhao, J.; Watanabe, T.; Bhawal, U.K.; Kubota, E.; Abiko, Y. Transcriptome analysis of β-TCP implanted in dog mandible. Bone 2011, 48, 864–877. [Google Scholar] [CrossRef] [PubMed]
- Stähli, C.; Bohner, M.; Bashoor-Zadeh, M.; Doebelin, N.; Baroud, G. Aqueous impregnation of porous β-tricalcium phosphate scaffolds. Acta Biomater. 2010, 6, 2760–2772. [Google Scholar] [CrossRef] [PubMed]
- Chawla, K.; Lamba, A.K.; Faraz, F.; Tandon, S. Evaluation of β-tricalcium phosphate in human infrabony periodontal osseous defects: A clinical study. Quintessence Int. 2011, 42, 291–300. [Google Scholar]
- Gorla, L.F.; Spin-Neto, R.; Boos, F.B.; Pereira Rdos, S.; Garcia-Junior, I.R.; Hochuli-Vieira, E. Use of autogenous bone and beta-tricalcium phosphate in maxillary sinus lifting: A prospective, randomized, volumetric computed tomography study. Int. J. Oral Maxillofac. Surg. 2015, 44, 1486–1491. [Google Scholar] [CrossRef] [PubMed]
- Harel, N.; Moses, O.; Palti, A.; Ormianer, Z. Long-term results of implants immediately placed into extraction sockets grafted with β-tricalcium phosphate: A retrospective study. J. Oral Maxillofac. Surg. 2013, 71, e63–e68. [Google Scholar] [CrossRef]
- LeGeros, R.Z.; Lin, S.; Rohanizadeh, R.; Mijares, D.; LeGeros, J.P. Biphasic calcium phosphate bioceramics: Preparation, properties and applications. J. Mater. Sci. Mater. Med. 2003, 14, 201–209. [Google Scholar] [CrossRef]
- Bouwman, W.F.; Bravenboer, N.; Frenken, J.; Ten Bruggenkate, C.M.; Schulten, E. The use of a biphasic calcium phosphate in a maxillary sinus floor elevation procedure: A clinical, radiological, histological, and histomorphometric evaluation with 9- and 12-month healing times. Int. J. Implant Dent. 2017, 3, 34. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kakar, A.; Rao, B.H.S.; Hegde, S.; Deshpande, N.; Lindner, A.; Nagursky, H.; Patney, A.; Mahajan, H. Ridge preservation using an in situ hardening biphasic calcium phosphate (β-TCP/HA) bone graft substitute-a clinical, radiological, and histological study. Int. J. Implant Dent. 2017, 3, 25. [Google Scholar] [CrossRef] [Green Version]
- Kano, S.; Yamazaki, A.; Otsuka, R.; Ohgaki, M.; Akao, M.; Aoki, H. Application of hydroxyapatite-sol as drug carrier. Bio-Med. Mater. Eng. 1994, 4, 283–290. [Google Scholar] [CrossRef]
- Bianco, A.; Cacciotti, I.; Lombardi, M.; Montanaro, L.; Gusmano, G. Thermalstability and sintering behaviour of hydroxyapatite nanopowders. J. Therm. Anal. Calorim. 2007, 88, 237–243. [Google Scholar] [CrossRef]
- Shiwaku, Y.; Neff, L.; Nagano, K.; Takeyama, K.-I.; De Bruijn, J.; Dard, M.; Gori, F.; Baron, R. The crosstalk between osteoclasts and osteoblasts is dependent upon the composition and structure of biphasic calcium phosphates. PLoS ONE 2015, 10, e0132903. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, C.; Liss, P.; Jacquemaire, B.; Lecestre, P.; Frayssinet, P. Biphasic synthetic bone substitute use in orthopaedic and trauma surgery: Clinical, radiological and histological results. J. Mater. Sci. Mater. Med. 1999, 10, 821–825. [Google Scholar] [CrossRef]
- Dreesmann, H. Ueber Knochenplombierung bei Hohlenformigen Defekten des Knochens. Beitr. Klin. Chir. 1892, 9, 804–810. [Google Scholar]
- Kluin, O.S.; van der Mei, H.C.; Busscher, H.J.; Neut, D. Biodegradable vs. non-biodegradable antibiotic delivery devices in the treatment of osteomyelitis. Expert Opin. Drug Deliv. 2013, 10, 341–351. [Google Scholar] [CrossRef]
- Pecora, G.; Andreana, S.; Margarone, J.E., 3rd; Covani, U.; Sottosanti, J.S. Bone regeneration with a calcium sulfate barrier. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontol. 1997, 84, 424–429. [Google Scholar] [CrossRef]
- Thomas, M.V.; Puleo, D.A. Calcium sulfate: Properties and clinical applications. J. Biomed. Mater. Res. Part B Appl. Biomater. 2009, 88, 597–610. [Google Scholar] [CrossRef] [PubMed]
- Ricci, J.; Alexander, H.; Nadkarni, P.; Hawkins, M.; Turner, J.; Rosenblum, S.; Brezenoff, L.; DeLeonardis, D.; Pecora, G. Biological mechanisms of calcium sulfate replacement by bone. In Bone Engineering; Davies, J.E., Ed.; Em2 Inc.: Toronto, ON, Canada, 2000; pp. 332–344. [Google Scholar]
- Mazor, Z.; Mamidwar, S.; Ricci, J.L.; Tovar, N.M. Bone repair in periodontal defect using a composite of allograft and calcium sulfate (DentoGen) and a calcium sulfate barrier. J. Oral Implantol. 2011, 37, 287–292. [Google Scholar] [CrossRef]
- Coetzee, A.S. Regeneration of bone in the presence of calcium sulfate. Arch. Otolaryngol. 1980, 106, 405–409. [Google Scholar] [CrossRef] [PubMed]
- Bell, W.H. Resorption characteristics of bone and bone substitutes. Oral Surg. Oral Med. Oral Pathol. 1964, 17, 650–657. [Google Scholar] [CrossRef]
- Huchim-Chablé, M.; de Arredondo, R.S.; Rivero-Navarrete, J.A.; Mendiburu-Zavala, C.; Cárdenas-Erosa, R.; Peñaloza-Cuevas, R. Calcium sulfate and plasma rich in growth factors enhance bone regeneration after extraction of the mandibular third molar: A proof of concept study. Materials 2021, 14, 1126. [Google Scholar] [CrossRef]
- Marx, R.E.; Carlson, E.R.; Eichstaedt, R.M. Platelet-rich-plasma: Growth factor enhancement for bone grafts. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontol. 1998, 85, 638–646. [Google Scholar] [CrossRef]
- Sultan, T.; Cheah, C.W.; Ibrahim, N.B.; Asif, M.K.; Vaithilingam, R.D. Three-dimensional assessment of the extraction sockets, augmented with platelet-rich fibrin and calcium sulfate: A clinical pilot study. J. Dent. 2020, 101, 103455. [Google Scholar] [CrossRef] [PubMed]
- Dohan, E.; de Peppo, G.M.; Doglioli, P.; Sammartino, G. Slow release of growth factors and thrombospondin-1 in Choukroun’s platelet-rich fibrin (PRF): A gold standard to achieve for all surgical platelet concentrates technologies. Growth Factors 2009, 27, 63–69. [Google Scholar] [CrossRef]
- Yuan, H.; Fernandes, H.; Habibovic, P.; de Boer, J.; Barradas, A.; de Ruiter, A.; Walsh, W.; van Blitterswijk, C.; de Bruijn, J.D. Osteoinductive ceramics as a synthetic alternative to autologous bone grafting. Proc. Natl. Acad. Sci. USA 2010, 107, 13614–13619. [Google Scholar] [CrossRef] [Green Version]
- Miron, R.J.; Zhang, Q.; Sculean, A.; Buser, D.; Pippenger, B.; Dard, M.; Shirakata, Y.; Chandad, F.; Zhang, Y. Osteoinductive potential of 4 commonly employed bone grafts. Clin. Oral Investig. 2016, 20, 2259–2265. [Google Scholar] [CrossRef]
- Malhotra, A.; Habibovic, P. Calcium phosphates and angiogenesis: Implications and advances for bone regeneration. Trends Biotechnol. 2016, 34, 983–992. [Google Scholar] [CrossRef] [Green Version]
- Chen, Y.; Wang, J.; Zhu, X.; Tang, Z.; Yang, X.; Tan, Y.; Fan, Y.; Zhang, X. Enhanced effect of β-tricalcium phosphate phase on neovascularization of porous calcium phosphate ceramics: In vitro and in vivo evidence. Acta Biomater. 2015, 11, 435–448. [Google Scholar] [CrossRef] [PubMed]
- Artzi, Z.; Weinreb, M.; Givol, N.; Rohrer, M.D.; Nemcovsky, C.E.; Prasad, H.S.; Tal, H. Biomaterial resorption rate and healing site morphology of inorganic bovine bone and beta-tricalcium phosphate in the canine: A 24-month longitudinal histologic study and morphometric analysis. Intenational J. Oral Maxillofac. Implant. 2004, 19, 357–368. [Google Scholar]
- Hollinger, J.O.; Brekke, J.; Gruskin, E.; Lee, D. Role of bone substitutes. Clin. Orthop. Relat. Res. 1996, 324, 55–65. [Google Scholar] [CrossRef]
- Sukumar, S.; Drizhal, I. Bone grafts in periodontal therapy. Acta Med. 2008, 51, 203–207. [Google Scholar] [CrossRef] [Green Version]
- Fairbairn, P.; Leventis, M. Protocol for bone augmentation with simultaneous early implant placement: A retrospective multicenter clinical study. Int. J. Dent. 2015, 2015, 589135. [Google Scholar] [CrossRef] [PubMed] [Green Version]
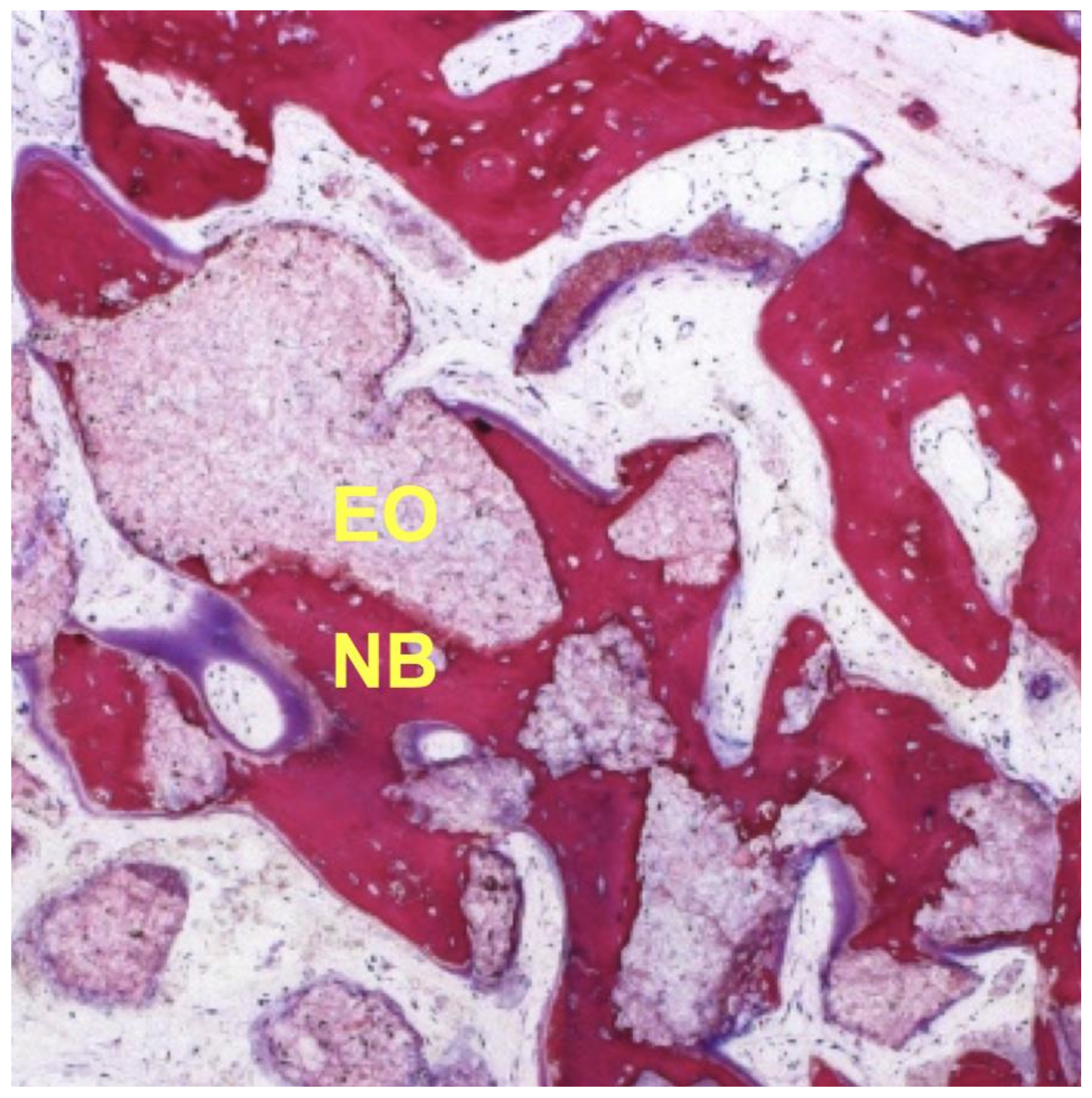
- Leventis, M.D.; Fairbairn, P.; Dontas, I.; Faratzis, G.; Valavanis, K.D.; Khaldi, L.; Kostakis, G.; Eleftheriadis, E. Biological response to β-tricalcium phosphate/calcium sulfate synthetic graft material: An experimental study. Implant Dent. 2014, 23, 37–43. [Google Scholar] [CrossRef] [Green Version]
- Ruga, E.; Gallesio, C.; Chiusa, L.; Boffano, P. Clinical and histologic outcomes of calcium sulfate in the treatment of postextraction sockets. J. Craniofacial Surg. 2011, 22, 494–498. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Anson, D. Using calcium sulfate in guided tissue regeneration: A recipe for success. Compend. Contin. Educ. Dent. 2000, 21, 365–370. [Google Scholar]
- Eleftheriadis, E.; Leventis, M.D.; Tosios, K.I.; Faratzis, G.; Titsinidis, S.; Eleftheriadi, I.; Dontas, I. Osteogenic activity of beta-tricalcium phosphate in a hydroxyl sulphate matrix and demineralized bone matrix: A histological study in rabbit mandible. J. Oral Sci. 2010, 52, 377–384. [Google Scholar] [CrossRef] [Green Version]
- Podaropoulos, L.; Veis, A.A.; Papadimitriou, S.; Alexandridis, C.; Kalyvas, D. Bone regeneration using beta-tricalcium phosphate in a calcium sulfate matrix. J. Oral Implantol. 2009, 35, 28–36. [Google Scholar] [CrossRef]
- Yahav, A.; Kurtzman, G.M.; Katzap, M.; Dudek, D.; Baranes, D. Bone regeneration: Properties and clinical applications of biphasic calcium sulfate. Dent. Clin. 2020, 64, 453–472. [Google Scholar]
- Dimitriou, R.; Mataliotakis, G.I.; Calori, G.M.; Giannoudis, P.V. The role of barrier membranes for guided bone regeneration and restoration of large bone defects: Current experimental and clinical evidence. BMC Med. 2012, 10, 81. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Buser, D.; Dahlin, C.; Schenk, R.K. Guided Bone Regeneration in Implant Dentistry; Quintessence Publishing: London, UK, 1995. [Google Scholar]
- Sukumar, S.; Drizhal, I.; Bukac, J.; Paulusova, V.; Pilathadka, S. Surgical treatment of periodontal intrabony defects with calcium sulphate in combination with beta tricalcium phosphate—A 12-month retrospective clinical evaluation. Acta Med. 2010, 53, 229–234. [Google Scholar] [CrossRef] [Green Version]
- Fairbairn, P.; Leventis, M.; Mangham, C.; Horowitz, R. Alveolar ridge preservation using a novel synthetic grafting material: A case with two-year follow-up. Case Rep. Dent. 2018, 2018, 6412806. [Google Scholar] [CrossRef] [Green Version]
- Jambhekar, S.; Kernen, F.; Bidra, A.S. Clinical and histologic outcomes of socket grafting after flapless tooth extraction: A systematic review of randomized controlled clinical trials. J. Prosthet. Dent. 2015, 113, 371–382. [Google Scholar] [CrossRef] [PubMed]
- Stein, J.M.; Fickl, S.; Yekta, S.S.; Hoischen, U.; Ocklenburg, C.; Smeets, R. Clinical evaluation of a biphasic calcium composite grafting material in the treatment of human periodontal intrabony defects: A 12-month randomized controlled clinical trial. J. Periodontol. 2009, 80, 1774–1782. [Google Scholar] [CrossRef]
- Hench, L.L.; Splinter, R.J.; Allen, W.C.; Greenlee, T.K. Bonding mechanisms at the interface of ceramic prosthetic materials. J. Biomed. Mater. Res. 1971, 5, 117–141. [Google Scholar] [CrossRef]
- Välimäki, V.V.; Aro, H.T. Molecular basis for action of bioactive glasses as bone graft substitute. Scand. J. Surg. 2006, 95, 95–102. [Google Scholar] [CrossRef] [Green Version]
- Hench, L.L. The story of Bioglass. J. Mater. Sci. Mater. Med. 2006, 17, 967–978. [Google Scholar] [CrossRef]
- Zamet, J.S.; Darbar, U.R.; Griffiths, G.; Bulman, J.; Brägger, U.; Burgin, W.; Newman, H.N. Particulate bioglass as a grafting material in the treatment of periodontal intrabony defects. J. Clin. Periodontol. 1997, 24, 410–418. [Google Scholar] [CrossRef]
- Carvalho, S.M.; Moreira, C.D.F.; Oliveira, A.C.X.; Oliveira, A.A.R.; Lemos, E.M.F.; Pereira, M.M. Chapter 15—Bioactive glass nanoparticles for periodontal regeneration and applications in dentistry. In Nanobiomaterials in Clinical Dentistry, 2nd ed.; Subramani, K., Ahmed, W., Eds.; Elsevier: Amsterdam, The Netherlands, 2019; pp. 351–383. [Google Scholar]
- Brink, M.; Turunen, T.; Happonen, R.P.; Yli-Urpo, A. Compositional dependence of bioactivity of glasses in the system Na2O-K2O-MgO-CaO-B2O3-P2O5-SiO2. J. Biomed. Mater. Res. 1997, 37, 114–121. [Google Scholar] [CrossRef]
- Hench, L.L. Bioactive Glass Bone Grafts: History and clinical applications. In Handbook of Bioceramics and Biocomposites; Antoniac, I.V., Ed.; Springer International Publishing: Cham, Switzerland, 2016; pp. 23–33. [Google Scholar]
- Webster, T.J.; Ergun, C.; Doremus, R.H.; Siegel, R.W.; Bizios, R. Enhanced functions of osteoblasts on nanophase ceramics. Biomaterials 2000, 21, 1803–1810. [Google Scholar] [CrossRef]
- Jones, J.R. Reprint of: Review of bioactive glass: From Hench to hybrids. Acta Biomater. 2015, 23, S53–S82. [Google Scholar] [CrossRef]
- Hench, L.L.; Thompson, I. Twenty-first century challenges for biomaterials. J. R. Soc. Interface 2010, 7 (Suppl. 4), S379–S391. [Google Scholar] [CrossRef] [Green Version]
- Lu, Q.; Han, W.J.; Choi, H.J. Smart and functional conducting polymers: Application to electrorheological fluids. Molecules 2018, 23, 2854. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rahmati, M.; Pennisi, C.P.; Budd, E.; Mobasheri, A.; Mozafari, M. Biomaterials for regenerative medicine: Historical perspectives and current trends. Adv. Exp. Med. Biol. 2018, 1119, 1–19. [Google Scholar] [CrossRef] [PubMed]
- Al-Namnam, N.M.N.; Kim, K.H.; Chai, W.L.; Ha, K.O.; Siar, C.H.; Ngeow, W.C. Modified poly(caprolactone trifumarate) with embedded gelatin microparticles as a functional scaffold for bone tissue engineering. J. Appl. Polym. Sci. 2016, 133. [Google Scholar] [CrossRef]
- Donnaloja, F.; Jacchetti, E.; Soncini, M.; Raimondi, M.T. Natural and synthetic polymers for bone scaffolds optimization. Polymers 2020, 12, 905. [Google Scholar] [CrossRef] [Green Version]
- Charnley, J. Anchorage of the femoral head prosthesis to the shaft of the femur. J. Bone Jt. Surg. Br. 1960, 42, 28–30. [Google Scholar] [CrossRef] [Green Version]
- Handoll, H.H.; Watts, A.C. Bone grafts and bone substitutes for treating distal radial fractures in adults. Cochrane Database Syst. Rev. 2008, 2008, Cd006836. [Google Scholar] [CrossRef] [Green Version]
- Ratner, B.D.; Hoffman, A.S.; Schoen, F.J.; Lemons, J.E.; Wagner, W.R.; Sakiyama-Elbert, S.E.; Zhang, G.U.; Yaszemski, M.J. Introduction—Biomaterials science: An evolving, multidisciplinary endeavor. In Biomaterials Science: An Introduction to Materials in Medicine; Wagner, W., Sakiyama-Elbert, S., Zhang, G., Yaszemski, M., Eds.; Academic Press: Cambridge, MA, USA, 2013; pp. 3–19. [Google Scholar]
- Jayash, S.N.; Hashim, N.M.; Misran, M.; Ibrahim, N.; Al-Namnam, N.M.; Baharuddin, N.A. Analysis on efficacy of chitosan-based gel on bone quality and quantity. Front. Mater. 2021, 8, 46. [Google Scholar] [CrossRef]
- Nicodemus, G.D.; Bryant, S.J. Cell encapsulation in biodegradable hydrogels for tissue engineering applications. Tissue Eng. Part B Rev. 2008, 14, 149–165. [Google Scholar] [CrossRef]
- Mano, J.F.; Silva, G.A.; Azevedo, H.S.; Malafaya, P.B.; Sousa, R.A.; Silva, S.S.; Boesel, L.F.; Oliveira, J.M.; Santos, T.C.; Marques, A.P.; et al. Natural origin biodegradable systems in tissue engineering and regenerative medicine: Present status and some moving trends. J. R. Soc. Interface 2007, 4, 999–1030. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Islam, S.; Bhuiyan, M.A.R.; Islam, M.N. Chitin and chitosan: Structure, properties and applications in biomedical engineering. J. Polym. Environ. 2017, 25, 854–866. [Google Scholar] [CrossRef]
- Pappalardo, D.; Mathisen, T.; Finne-Wistrand, A. Biocompatibility of resorbable polymers: A historical perspective and framework for the future. Biomacromolecules 2019, 20, 1465–1477. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, Y.; Wang, J.; Ma, Y.; Han, B.; Niu, X.; Liu, J.; Gao, L.; Wang, J.; Zhai, X.; Chu, K.; et al. Preparation of poly(lactic acid)/sintered hydroxyapatite composite biomaterial by supercritical CO2. Bio-Med. Mater. Eng. 2018, 29, 67–79. [Google Scholar] [CrossRef]
- Toosi, S.; Naderi-Meshkin, H.; Kalalinia, F.; Hosseinkhani, H.; Heirani-Tabasi, A.; Havakhah, S.; Nekooei, S.; Jafarian, A.H.; Rezaie, F.; Peivandi, M.T.; et al. Bone defect healing is induced by collagen sponge/polyglycolic acid. J. Mater. Sci. Mater. Med. 2019, 30, 33. [Google Scholar] [CrossRef]
- Yamauchi, K.; Goda, T.; Takeuchi, N.; Einaga, H.; Tanabe, T. Preparation of collagen/calcium phosphate multilayer sheet using enzymatic mineralization. Biomaterials 2004, 25, 5481–5489. [Google Scholar] [CrossRef] [PubMed]
- Narayan, R.J. The next generation of biomaterial development. Philos. Trans. Ser. A Math. Phys. Eng. Sci. 2010, 368, 1831–1837. [Google Scholar] [CrossRef]
- Ma, X.; He, Z.; Han, F.; Zhong, Z.; Chen, L.; Li, B. Preparation of collagen/hydroxyapatite/alendronate hybrid hydrogels as potential scaffolds for bone regeneration. Colloids Surf. B Biointerfaces 2016, 143, 81–87. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.-Y.; Chen, C.-C.; Wang, C.-Y.; Lee, A.K.; Yeh, C.-L.; Lin, C.-P. Assessment of the release of vascular endothelial growth factor from 3D-printed poly-ε-caprolactone/hydroxyapatite/calcium sulfate scaffold with enhanced osteogenic capacity. Polymers 2020, 12, 1455. [Google Scholar] [CrossRef] [PubMed]
- Wiria, F.E.; Leong, K.F.; Chua, C.K.; Liu, Y. Poly-epsilon-caprolactone/hydroxyapatite for tissue engineering scaffold fabrication via selective laser sintering. Acta Biomater. 2007, 3, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Sikora, A.; Czylkowski, D.; Hrycak, B.; Moczała-Dusanowska, M.; Łapiński, M.; Dors, M.; Jasiński, M. Surface modification of PMMA polymer and its composites with PC61BM fullerene derivative using an atmospheric pressure microwave argon plasma sheet. Sci. Rep. 2021, 11, 9270. [Google Scholar] [CrossRef] [PubMed]
- Wuisman, P.I.; Smit, T.H. Bioresorbable polymers: Heading for a new generation of spinal cages. Eur. Spine J. 2006, 15, 133–148. [Google Scholar] [CrossRef] [Green Version]
- Manavitehrani, I.; Fathi, A.; Badr, H.; Daly, S.; Negahi Shirazi, A.; Dehghani, F. Biomedical applications of biodegradable polyesters. Polymers 2016, 8, 20. [Google Scholar] [CrossRef] [Green Version]
- Chiulan, I.; Frone, A.N.; Brandabur, C.; Panaitescu, D.M. Recent advances in 3D printing of aliphatic polyesters. Bioengineering 2017, 5, 2. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gohil, S.V.; Suhail, S.; Rose, J.; Vella, T.; Nair, L.S. Chapter 8—Polymers and composites for orthopedic applications. In Materials for Bone Disorders; Bose, S., Bandyopadhyay, A., Eds.; Academic Press: Cambridge, MA, USA, 2017; pp. 349–403. [Google Scholar]
- Siracusa, V.; Maimone, G.; Antonelli, V. State-of-art of standard and innovative materials used in cranioplasty. Polymers 2021, 13, 1452. [Google Scholar] [CrossRef]
- Wang, W.; Caetano, G.; Ambler, W.S.; Blaker, J.J.; Frade, M.A.; Mandal, P.; Diver, C.; Bártolo, P. Enhancing the hydrophilicity and cell attachment of 3D printed PCL/graphene scaffolds for bone tissue engineering. Materials 2016, 9, 992. [Google Scholar] [CrossRef]
- Ku, J.K.; Kim, Y.K.; Yun, P.Y. Influence of biodegradable polymer membrane on new bone formation and biodegradation of biphasic bone substitutes: An animal mandibular defect model study. Maxillofac. Plast. Reconstr. Surg. 2020, 42, 34. [Google Scholar] [CrossRef]
- Al-Namnam, N.; Nagi, S. Recent advances in bone graft substitute for oral and maxillofacial applications: A review. Int. J. Biosci. 2019, 15, 70–94. [Google Scholar]
- Al-Namnam, N.M.; Kutty, M.G.; Chai, W.L.; Ha, K.O.; Kim, K.H.; Siar, C.H.; Ngeow, W.C. An injectable poly(caprolactone trifumarate-gelatin microparticles) (PCLTF-GMPs) scaffold for irregular bone defects: Physical and mechanical characteristics. Mater. Sci. Eng. C 2017, 72, 332–340. [Google Scholar] [CrossRef] [PubMed]
- Jeong, H.-J.; Gwak, S.-J.; Seo, K.D.; Lee, S.; Yun, J.-H.; Cho, Y.-S.; Lee, S.-J. Fabrication of three-dimensional composite scaffold for simultaneous alveolar bone regeneration in dental implant installation. Int. J. Mol. Sci. 2020, 21, 1863. [Google Scholar] [CrossRef] [Green Version]
- Goh, B.T.; Teh, L.Y.; Tan, D.B.; Zhang, Z.; Teoh, S.H. Novel 3D polycaprolactone scaffold for ridge preservation- A pilot randomised controlled clinical trial. Clin. Oral Implant. Res. 2015, 26, 271–277. [Google Scholar] [CrossRef] [PubMed]
- Louvrier, A.; Euvrard, E.; Nicod, L.P.; Rolin, G.; Gindraux, F.; Pazart, L.; Houdayer, C.; Risold, P.Y.; Meyer, F. Odontoblastic differentiation of dental pulp stem cells from healthy and carious teeth on an original PCL-based 3D scaffold. Int. Endod. J. 2018, 51 (Suppl. 4), e252–e263. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Warren, S.M.; Fong, K.D.; Nacamuli, R.P.; Song, H.M.; Fang, T.D.; Longaker, M.T. Biomaterials for skin and bone replacement and repair in plastic surgery. Oper. Tech. Plast. Reconstr. Surg. 2002, 9, 10–15. [Google Scholar] [CrossRef]
- Corcione, C.E.; Gervaso, F.; Scalera, F.; Montagna, F.; Maiullaro, T.; Sannino, A.; Maffezzoli, A. 3D printing of hydroxyapatite polymer-based composites for bone tissue engineering. J. Polym. Eng. 2017, 37, 741–746. [Google Scholar] [CrossRef]
- Cao, H.; Kuboyama, N. A biodegradable porous composite scaffold of PGA/beta-TCP for bone tissue engineering. Bone 2010, 46, 386–395. [Google Scholar] [CrossRef]
- Pajoumshariati, S.; Shirali, H.; Yavari, S.K.; Sheikholeslami, S.N.; Lotfi, G.; Abbas, F.M.; Abbaspourrad, A. GBR membrane of novel poly (butylene succinate-co-glycolate) co-polyester co-polymer for periodontal application. Sci. Rep. 2018, 8, 7513. [Google Scholar] [CrossRef]
- Makadia, H.K.; Siegel, S.J. Poly lactic-co-glycolic acid (PLGA) as biodegradable controlled drug delivery carrier. Polymers 2011, 3, 1377–1397. [Google Scholar] [CrossRef]
- Yun, Y.P.; Kim, S.E.; Lee, J.B.; Heo, D.N.; Bae, M.S.; Shin, D.R.; Lim, S.B.; Choi, K.K.; Park, S.J.; Kwon, I.K. Comparison of osteogenic differentiation from adipose-derived stem cells, mesenchymal stem cells, and pulp cells on PLGA/hydroxyapatite nanofiber. Tissue Eng. Regen. Med. 2009, 6, 336–345. [Google Scholar]
- Ohara, T.; Itaya, T.; Usami, K.; Ando, Y.; Sakurai, H.; Honda, M.J.; Ueda, M.; Kagami, H. Evaluation of scaffold materials for tooth tissue engineering. J. Biomed. Mater. Res. Part A 2010, 94, 800–805. [Google Scholar] [CrossRef] [PubMed]
- Thomas, N.G.; Sanil, G.P.; Rajmohan, G.; Prabhakaran, J.V.; Panda, A.K. Fabrication and anti-microbial evaluation of drug loaded polylactide space filler intended for ridge preservation following tooth extraction. J. Indian Soc. Periodontol. 2011, 15, 260–264. [Google Scholar] [CrossRef] [PubMed]
- Serino, G.; Biancu, S.; Iezzi, G.; Piattelli, A. Ridge preservation following tooth extraction using a polylactide and polyglycolide sponge as space filler: A clinical and histological study in humans. Clin. Oral Implant. Res. 2003, 14, 651–658. [Google Scholar] [CrossRef] [Green Version]
- Akita, D.; Morokuma, M.; Saito, Y.; Yamanaka, K.; Akiyama, Y.; Sato, M.; Mashimo, T.; Toriumi, T.; Arai, Y.; Kaneko, T.; et al. Periodontal tissue regeneration by transplantation of rat adipose-derived stromal cells in combination with PLGA-based solid scaffolds. Biomed. Res. 2014, 35, 91–103. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chang, P.C.; Dovban, A.S.; Lim, L.P.; Chong, L.Y.; Kuo, M.Y.; Wang, C.H. Dual delivery of PDGF and simvastatin to accelerate periodontal regeneration in vivo. Biomaterials 2013, 34, 9990–9997. [Google Scholar] [CrossRef] [PubMed]
- Genova, T.; Roato, I.; Carossa, M.; Motta, C.; Cavagnetto, D.; Mussano, F. Advances on bone substitutes through 3D bioprinting. Int. J. Mol. Sci. 2020, 21, 7012. [Google Scholar] [CrossRef] [PubMed]

| Compound | Chemical Formula | Ca/P Ratio |
|---|---|---|
| Dicalcium phosphate anhydrous (DCPA) | CaHPO4 | 1 |
| Dicalcium phosphate dihydrate (DCPD) | CaHPO4·H2O | 1 |
| Amorphous calcium phosphate (ACP) | CaxHy(PO4)z·nH2O n = 3–4.5; 15–20% H2O | 1.2–2.2 |
| α-Tricalcium phosphate (α-TCP) | α-Ca3(PO4)2 | 1.5 |
| β-Tricalcium phosphate (β-TCP) | β-Ca3(PO4)2 | 1.5 |
| Calcium deficient hydroxyapatite (CDHA) | Ca10−x(HPO4)x(PO4)6−x(OH)2−x | 1.5–1.67 |
| Hydroxyapatite (HA) | Ca10(PO4)6(OH)2 | 1.67 |
| Tetracalcium phosphate (TTCP) | CaO·Ca3(PO4)2 | 2.0 |
| Material | Advantage | Disadvantage | Indication/Application |
|---|---|---|---|
| Beta tricalcium phosphate (β-TCP) (i.e., IngeniOs™ Zimmer Biomet Dental, Carlsbad, CA, USA; Cerasorb™ Zimmer Biomet Dental, Carlsbad, CA, USA; OSferionTM Olympus terumo biomaterials coorperation, Sasazuka, Japan; OrthograftTM DePuy, Chester County, PA, USA) | Ease of handling Radiopacity allowing monitoring of healing Resorb readily Low immunogenicity Compressive strength similar to cancellous bone | Poor mechanical properties in particular compressive strength | Filler for alveolar defects (periodontal, periapical surgery, peri-implant and cyst enucleation) Extraction sockets grafting Sinus floor elevation |
| Biphasic calcium phosphate (i.e., MastergraftTM Medtronic, Minneapolis, MN, USA; Maxresorb® Botiss dental, Berlin, Germany) * HA/β-TCP = 40/60 | Resorb readily Greater mechanical strengths than either TCP or HA alone | Compressive strength remains lower than that of cortical bone | Filler for alveolar, periodontal and cystic defects Extraction sockets grafting Ridge augmentation Sinus floor elevation Periapical surgery |
| Typical Mechanical Properties | Wet CS | Dry CS | Cancellous Bone | Cortical Bone |
|---|---|---|---|---|
| Compressive strength (MPa) | 10–15 | 20–30 | 5–10 | 162.2 |
| Tensile Strength (MPa) | 2–4 | 4–6 | 10–15 | 151.8 |
| Bioactive glasses | Composition | Borate |
| Phosphate | ||
| Method of processing | Melt-derived | |
| Sol-gel |
| Polymer Bone-Based Material | Type | Advantages | Disadvantage | Applications |
|---|---|---|---|---|
| Non-biodegradable | ||||
| Poly methyl methacrylate (PMMA) | Acrylic glass | Biocompatible, biologically inert durable, superior osseointegration | Non-degradable, residual monomer can enter the bloodstream and cause embolism, limited biological response, shrink during polymerization leading to free spaces between cement and prosthesis or bone, excess of tension can cause cement fractures and release of cement particles caused inflammatory reaction, exothermic polymerization | Orthopaedic prostheses fixation, craniofacial defects, dentures, vertebroplasty and kyphoplasty |
| Biodegradable | ||||
| Poly(lactic acid) (PLA) | Aliphatic polyester. | Biodegradable, tunable physical and mechanical properties. osteoconductive, biodegradable, biocompatible, promote bone regeneration, Crystallinity tunable by changing hydroxylation degree | Acidic degradation products that might cause adverse tissue reactions, and lack of cellular adhesion due to hydrophobicity | Orthopaedic fixation tools, tendon and ligament repair, vascular stents, bone graft extender, carriers of bioactive factors. PLA, PLGA block copolymers use for drug eluting coatings |
| Poly(glycolic acid) (PGA) | ||||
| Poly(lactic-co-glycolic acid) (PLGA) | Act as a copolymer of PLA and PGA, similar application spectrum as PLA | |||
| Poly caprolactone (PCL) | Biodegradable, Machinability, good mechanical strength, high porosity, crystallinity and thermal stability, crosslink in situ, printed by injection | Slow degradation rate, poor water wettability, lack of cell adhesion, low mechanical strength | Production of specialty polyurethanes, composite with other biomaterial to create tissue-engineered scaffolds, injectable implants for controlled release drug-delivery systems | |
| Poly (vinyl alcohol) (PVA) | Polyalcohol | Biodegradable, tunable water solubility and crystallinity, biocompatible | Lower water solubility and crystallinity, cross-linking of polymers to maintain integrity | Used in tissue-engineering applications from the laboratory to the pre-clinical research |
| Poly (propylene fumarate) (PPF) | Unsaturated linear polyester | Osteoconductive, biocompatible, tunable degradation time, controllable mechanical properties, double bond along its backbone permits cross-linking in situ | Cross-linking of polymers to maintain integrity | Holds promise for use as regenerative scaffolds and bone cements often as part of an injectable bone replacement composite |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cheah, C.W.; Al-Namnam, N.M.; Lau, M.N.; Lim, G.S.; Raman, R.; Fairbairn, P.; Ngeow, W.C. Synthetic Material for Bone, Periodontal, and Dental Tissue Regeneration: Where Are We Now, and Where Are We Heading Next? Materials 2021, 14, 6123. https://doi.org/10.3390/ma14206123
Cheah CW, Al-Namnam NM, Lau MN, Lim GS, Raman R, Fairbairn P, Ngeow WC. Synthetic Material for Bone, Periodontal, and Dental Tissue Regeneration: Where Are We Now, and Where Are We Heading Next? Materials. 2021; 14(20):6123. https://doi.org/10.3390/ma14206123
Chicago/Turabian StyleCheah, Chia Wei, Nisreen Mohammed Al-Namnam, May Nak Lau, Ghee Seong Lim, Renukanth Raman, Peter Fairbairn, and Wei Cheong Ngeow. 2021. "Synthetic Material for Bone, Periodontal, and Dental Tissue Regeneration: Where Are We Now, and Where Are We Heading Next?" Materials 14, no. 20: 6123. https://doi.org/10.3390/ma14206123
APA StyleCheah, C. W., Al-Namnam, N. M., Lau, M. N., Lim, G. S., Raman, R., Fairbairn, P., & Ngeow, W. C. (2021). Synthetic Material for Bone, Periodontal, and Dental Tissue Regeneration: Where Are We Now, and Where Are We Heading Next? Materials, 14(20), 6123. https://doi.org/10.3390/ma14206123







