In Vitro Assessment of the Effect of Implant Position on Biomechanical Behaviors of Implant-Supported Removable Partial Dentures in Kennedy Class II Condition
Abstract
1. Introduction
2. Materials and Methods
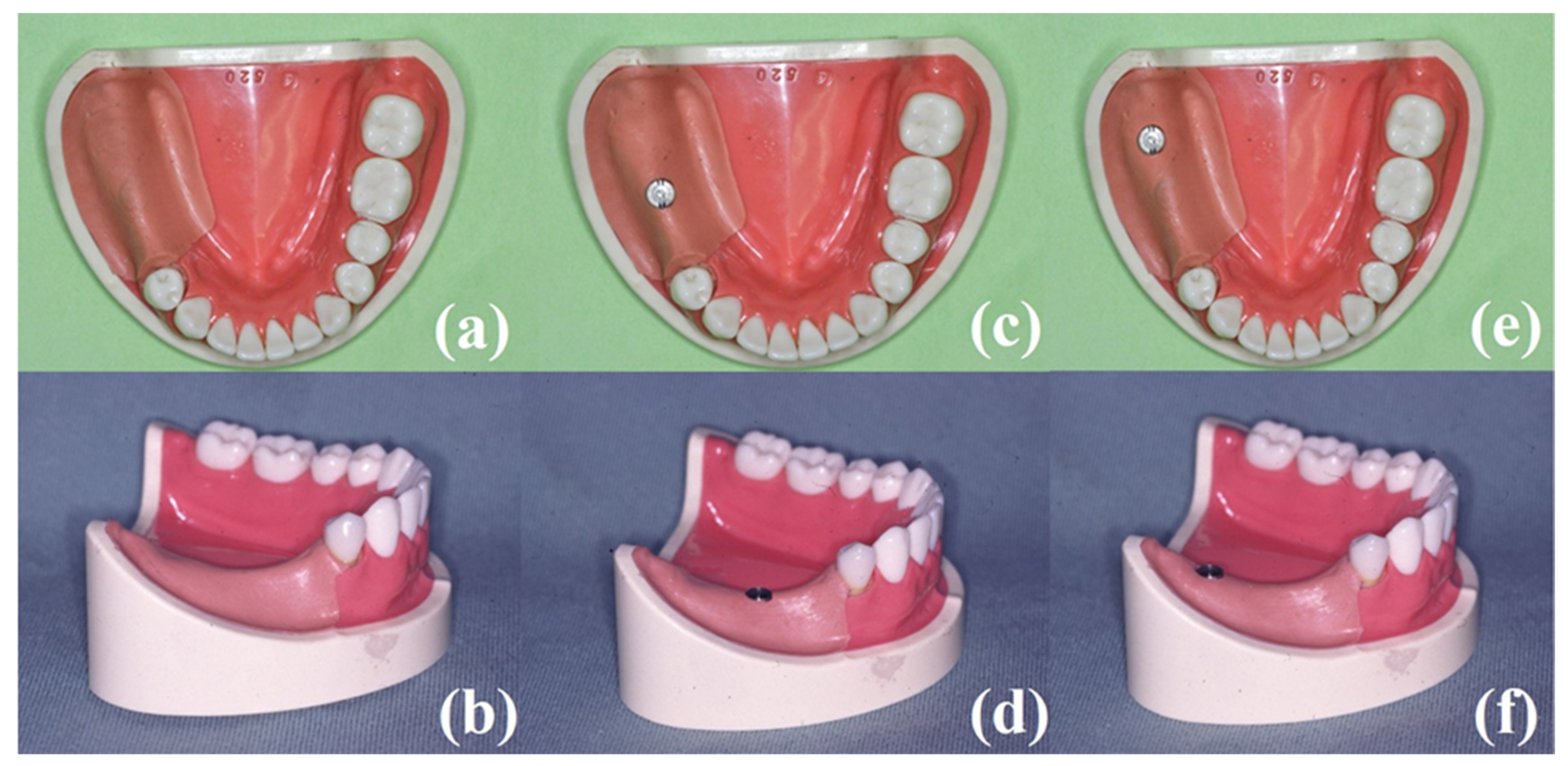
2.1. Experimental Model
2.2. RPDs for Analyses
2.3. Measuring Devices and Procedures
2.4. Statistical Analyses
3. Results
3.1. Vertical Displacement at Loading Point of CRPD and ISRPD
3.2. Mesio-Distal Displacement of Abutment Tooth (#44)
3.3. Bending Moment of Abutment Tooth (#44)
3.4. Bending Moment of the Implant
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bilhan, H.; Erdogan, O.; Ergin, S.; Celik, M.; Ates, G.; Geckili, O. Complication rates and patient satisfaction with removable dentures. J. Adv. Prosthodont. 2012, 4, 109–115. [Google Scholar] [CrossRef] [PubMed]
- Keltjens, H.M.; Kayser, A.F.; Hertel, R.; Battistuzzi, P.G. Distal extension removable partial dentures supported by implants and residual teeth: Considerations and case reports. Int. J. Oral Maxillofac. Implant. 1993, 8, 208–213. [Google Scholar]
- Halterman, S.M.; Rivers, J.A.; Keith, J.D.; Nelson, D.R. Implant support for removable partial overdentures: A case report. Implant. Dent. 1999, 8, 74–78. [Google Scholar] [CrossRef]
- Kaufmann, R.; Friedli, M.; Hug, S.; Mericske-Stern, R. Removable dentures with implant support in strategic positions followed for up to 8 years. Int. J. Prosthodont. 2009, 22, 233–241. [Google Scholar]
- Wismeijer, D.; Tawse-Smith, A.; Payne, A.G. Multicentre prospective evaluation of implant-assisted mandibular bilateral distal extension removable partial dentures: Patient satisfaction. Clin. Oral Implant. Res. 2013, 24, 20–27. [Google Scholar] [CrossRef]
- Payne, A.G.; Tawse-Smith, A.; Wismeijer, D.; De Silva, R.K.; Ma, S. Multicentre prospective evaluation of implant-assisted mandibular removable partial dentures: Surgical and prosthodontic outcomes. Clin. Oral Implant. Res. 2017, 28, 116–125. [Google Scholar] [CrossRef] [PubMed]
- Threeburuth, W.; Aunmeungtong, W.; Khongkhunthian, P. Comparison of immediate-load mini dental implants and conventional-size dental implants to retain mandibular Kennedy class I removable partial dentures: A randomized clinical trial. Clin. Implant. Dent. Relat. Res. 2018, 20, 785–792. [Google Scholar] [CrossRef]
- Kang, S.H.; Kim, S.K.; Heo, S.J.; Koak, J.Y. Survival rate and clinical evaluation of the implants in implant assisted removable partial dentures: Surveyed crown and overdenture. J. Adv. Prosthodont. 2020, 12, 239–249. [Google Scholar] [CrossRef] [PubMed]
- Ohkubo, C.; Kurihara, D.; Shimpo, H.; Suzuki, Y.; Kokubo, Y.; Hosoi, T. Effect of implant support on distal extension removable partial dentures: In vitro assessment. J. Oral Rehabil. 2007, 34, 52–56. [Google Scholar] [CrossRef]
- Ohkubo, C.; Kobayashi, M.; Suzuki, Y.; Hosoi, T. Effect of implant support on distal-extension removable partial dentures: In vivo assessment. Int. J. Oral Maxillofac. Implant. 2008, 23, 1095–1101. [Google Scholar] [CrossRef] [PubMed]
- Grossmann, Y.; Nissan, J.; Levin, L. Clinical effectiveness of implant-supported removable partial dentures: A review of the literature and retrospective case evaluation. J. Oral Maxillofac. Surg. 2009, 67, 1941–1946. [Google Scholar] [CrossRef]
- Hirata, K.; Takahashi, T.; Tomita, A.; Gonda, T.; Maeda, Y. The Influence of Loading Variables on Implant Strain When Supporting Distal-Extension Removable Prostheses: An In Vitro Study. Int. J. Prosthodont. 2015, 28, 484–486. [Google Scholar] [CrossRef]
- Hirata, K.; Takahashi, T.; Tomita, A.; Gonda, T.; Maeda, Y. Loading Variables on Implant-Supported Distal-Extension Removable Partial Dentures: An In Vitro Pilot Study. Int. J. Prosthodont. 2016, 29, 17–19. [Google Scholar] [CrossRef][Green Version]
- Hirata, K.; Takahashi, T.; Tomita, A.; Gonda, T.; Maeda, Y. Influence of Abutment Angle on Implant Strain When Supporting a Distal Extension Removable Partial Dental Prosthesis: An In Vitro Study. Int. J. Prosthodont. 2017, 30, 51–53. [Google Scholar] [CrossRef]
- Nogawa, T.; Saito, M.; Murashima, N.; Takayama, Y.; Yokoyama, A. Influence of rigidity of retainers on dynamic behavior of implant-supported removable partial dentures. Int. J. Implant. Dent. 2020, 6, 60. [Google Scholar] [CrossRef]
- Gates, W.D., 3rd; Cooper, L.F.; Sanders, A.E.; Reside, G.J.; De Kok, I.J. The effect of implant-supported removable partial dentures on oral health quality of life. Clin. Oral Implant. Res. 2014, 25, 207–213. [Google Scholar] [CrossRef] [PubMed]
- Jensen, C.; Raghoebar, G.M.; Kerdijk, W.; Meijer, H.J.A.; Cune, M.S. Implant-supported mandibular removable partial dentures; Patient-based outcome measures in relation to implant position. J. Dent. 2016, 55, 92–98. [Google Scholar] [CrossRef] [PubMed]
- Jensen, C.; Meijer, H.J.A.; Raghoebar, G.M.; Kerdijk, W.; Cune, M.S. Implant-supported removable partial dentures in the mandible: A 3-16 year retrospective study. J. Prosthodont. Res. 2017, 61, 98–105. [Google Scholar] [CrossRef] [PubMed]
- Jensen, C.; Ross, J.; Feenstra, T.L.; Raghoebar, G.M.; Speksnijder, C.; Meijer, H.J.A.; Cune, M.S. Cost-effectiveness of implant-supported mandibular removable partial dentures. Clin. Oral Implant. Res. 2017, 28, 594–601. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, Y.; Kono, K.; Shimpo, H.; Sato, Y.; Ohkubo, C. Clinical Evaluation of Implant-Supported Removable Partial Dentures With a Stress-Breaking Attachment. Implant. Dent. 2017, 26, 516–523. [Google Scholar] [CrossRef] [PubMed]
- Tribst, J.P.; de Araújo, R.M.; Ramanzine, N.P.; Santos, N.R.; Dal Piva, A.O.; Borges, A.L.; da Silva, J.M. Mechanical behavior of implant assisted removable partial denture for Kennedy class II. J. Clin. Exp. Dent. 2020, 12, e38–e45. [Google Scholar] [CrossRef]
- Vahidi, F.; Pinto-Sinai, G. Complications associated with implant-retained removable prostheses. Dent. Clin. N. Am. 2015, 59, 215–226. [Google Scholar] [CrossRef]
- Goodacre, B.J.; Goodacre, S.E.; Goodacre, C.J. Prosthetic complications with implant prostheses (2001–2017). Eur. J. Oral Implant. 2018, 11, S27–S36. [Google Scholar]
- Mijiritsky, E.; Lorean, A.; Mazor, Z.; Levin, L. Implant Tooth-Supported Removable Partial Denture with at Least 15-Year Long-Term Follow-Up. Clin. Implant. Dent. Relat. Res. 2015, 17, 917–922. [Google Scholar] [CrossRef] [PubMed]
- Brudvik, J.S. (Ed.) Implants and removable partial dentures. In Advanced Removable Partial Dentures; Quitnessence Publishing Co.: Chicago, IL, USA, 1999; pp. 153–159. [Google Scholar]
- Matsudate, Y.; Yoda, N.; Nanba, M.; Ogawa, T.; Sasaki, K. Load distribution on abutment tooth, implant and residual ridge with distal-extension implant-supported removable partial denture. J. Prosthodont. Res. 2016, 60, 282–288. [Google Scholar] [CrossRef] [PubMed]
- Tokuhisa, M.; Matsushita, Y.; Koyano, K. In vitro study of a mandibular implant overdenture retained with ball, magnet, or bar attachments: Comparison of load transfer and denture stability. Int. J. Prosthodont. 2003, 16, 128–134. [Google Scholar]
- Carlsson, G.E. Responses of jawbone to pressure. Gerodontology 2004, 21, 65–70. [Google Scholar] [CrossRef] [PubMed]
- Turkyilmaz, I.; McGlumphy, E.A. Influence of bone density on implant stability parameters and implant success: A retrospective clinical study. BMC Oral Health 2008, 8, 32. [Google Scholar] [CrossRef] [PubMed]
- Attanasio, F.; Antonelli, A.; Brancaccio, Y.; Averta, F.; Figliuzzi, M.M.; Fortunato, L.; Giudice, A. Primary Stability of Three Different Osteotomy Techniques in Medullary Bone: An in Vitro Study. Dent. J. 2020, 8, 21. [Google Scholar] [CrossRef] [PubMed]
- Mijiritsky, E.; Ormianer, Z.; Klinger, A.; Mardinger, O. Use of dental implants to improve unfavorable removable partial denture design. Compend. Contin. Educ. Dent. 2005, 26, 744–746. [Google Scholar]
- Giudice, A.; Bennardo, F.; Antonelli, A.; Barone, S.; Wagner, F.; Fortunato, L.; Traxler, H. Influence of clinician’s skill on primary implant stability with conventional and piezoelectric preparation techniques: An ex-vivo study. J. Biol. Regul Homeost. Agents 2020, 34, 739–745. [Google Scholar] [CrossRef] [PubMed]
- Cunha, L.D.; Pellizzer, E.P.; Verri, F.R.; Pereira, J.A. Evaluation of the influence of location of osseointegrated implants associated with mandibular removable partial dentures. Implant. Dent. 2008, 17, 278–287. [Google Scholar] [CrossRef]
- Memari, Y.; Geramy, A.; Fayaz, A.; Rezvani Habib Abadi, S.; Mansouri, Y. Influence of Implant Position on Stress Distribution in Implant-Assisted Distal Extension Removable Partial Dentures: A 3D Finite Element Analysis. J. Dent. 2014, 11, 523–530. [Google Scholar]
- Ortiz-Puigpelat, O.; Lázaro-Abdulkarim, A.; de Medrano-Reñé, J.M.; Gargallo-Albiol, J.; Cabratosa-Termes, J.; Hernández-Alfaro, F. Influence of Implant Position in Implant-Assisted Removable Partial Denture: A Three-Dimensional Finite Element Analysis. J. Prosthodont. 2019, 28, e675–e681. [Google Scholar] [CrossRef]
- Ohyama, T.; Nakabayashi, S.; Yasuda, H.; Kase, T.; Namaki, S. Mechanical analysis of the effects of implant position and abutment height on implant-assisted removable partial dentures. J. Prosthodont. Res. 2020, 64, 340–345. [Google Scholar] [CrossRef] [PubMed]
- Van der Bilt, A. Assessment of mastication with implications for oral rehabilitation: A review. J. Oral Rehabil. 2011, 38, 754–780. [Google Scholar] [CrossRef]






Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kihara, M.; Ogino, Y.; Matsushita, Y.; Morita, T.; Sawae, Y.; Ayukawa, Y.; Koyano, K. In Vitro Assessment of the Effect of Implant Position on Biomechanical Behaviors of Implant-Supported Removable Partial Dentures in Kennedy Class II Condition. Materials 2021, 14, 2145. https://doi.org/10.3390/ma14092145
Kihara M, Ogino Y, Matsushita Y, Morita T, Sawae Y, Ayukawa Y, Koyano K. In Vitro Assessment of the Effect of Implant Position on Biomechanical Behaviors of Implant-Supported Removable Partial Dentures in Kennedy Class II Condition. Materials. 2021; 14(9):2145. https://doi.org/10.3390/ma14092145
Chicago/Turabian StyleKihara, Masafumi, Yoichiro Ogino, Yasuyuki Matsushita, Takehiro Morita, Yoshinori Sawae, Yasunori Ayukawa, and Kiyoshi Koyano. 2021. "In Vitro Assessment of the Effect of Implant Position on Biomechanical Behaviors of Implant-Supported Removable Partial Dentures in Kennedy Class II Condition" Materials 14, no. 9: 2145. https://doi.org/10.3390/ma14092145
APA StyleKihara, M., Ogino, Y., Matsushita, Y., Morita, T., Sawae, Y., Ayukawa, Y., & Koyano, K. (2021). In Vitro Assessment of the Effect of Implant Position on Biomechanical Behaviors of Implant-Supported Removable Partial Dentures in Kennedy Class II Condition. Materials, 14(9), 2145. https://doi.org/10.3390/ma14092145






