Transplantation of Mature Adipocyte-Derived Dedifferentiated Fat Cells Facilitates Periodontal Tissue Regeneration of Class II Furcation Defects in Miniature Pigs
Abstract
:1. Introduction
2. Materials and Methods
2.1. Experimental Animals
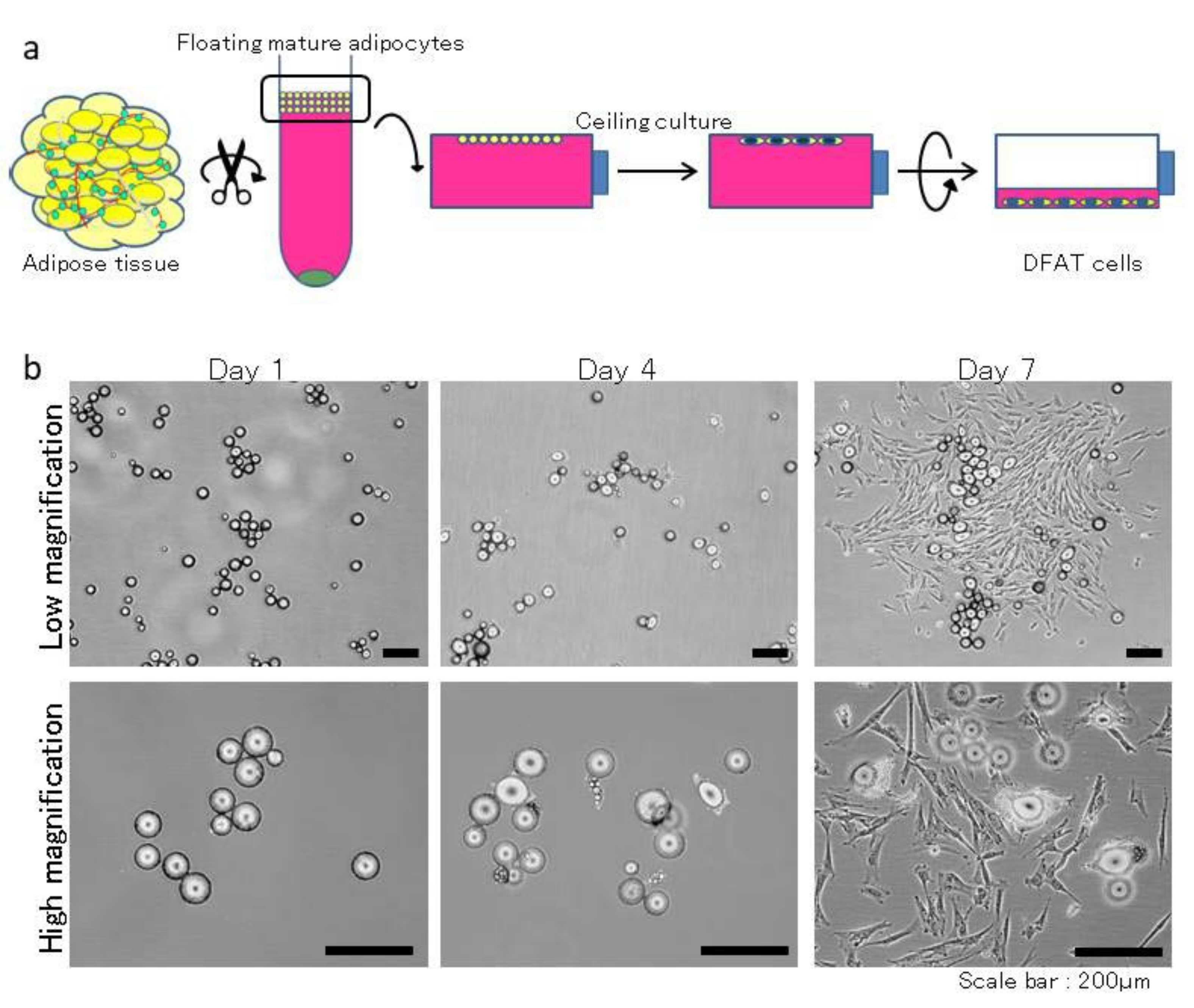
2.2. Isolation and Culture of DFAT Cells
2.3. In Vivo Experiment
2.4. Micro-Computed Tomography (CT) Imaging and Analysis
2.5. Histological and Immunohistochemical Staining and Analysis
2.6. Statistical Analysis
3. Results
3.1. Generation of Furcation Defects and Clinical Assessment in the Adult MMPs
3.2. CT Analysis
3.3. DFAT Cell Transplantation Enhanced Periodontal Tissue Regeneration
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kinane, D.F.; Marshall, G.J. Periodontal Manifestations of Systemic Disease. Aust. Dent. J. 2001, 46, 2–12. [Google Scholar] [CrossRef] [PubMed]
- Moutsopoulos, N.M.; Madianos, P.N. Low-Grade Inflammation in Chronic Infectious Diseases: Paradigm of Periodontal Infections. Ann. N. Y. Acad. Sci. 2006, 1088, 251–264. [Google Scholar] [CrossRef] [PubMed]
- Guan, J.; Zhang, D.; Wang, C. Identifying periodontitis risk factors through a retrospective analysis of 80 cases. Pak. J. Med. Sci. 2022, 38, 293–296. [Google Scholar] [CrossRef] [PubMed]
- Taba, M., Jr.; Jin, Q.; Sugai, J.V.; Giannobile, W.V. Current Concepts in Periodontal Bioengineering. Orthod. Craniofac. Res. 2005, 8, 292–302. [Google Scholar] [CrossRef] [PubMed]
- Rios, H.F.; Lin, Z.; Oh, B.; Park, C.H.; Giannobile, W.V. Cell- and Gene-Based Therapeutic Strategies for Periodontal Regenerative Medicine. J. Periodontol. 2011, 82, 1223–1237. [Google Scholar] [CrossRef] [Green Version]
- Górski, B.; Jalowski, S.; Górska, R.; Zaremba, M. Treatment of intrabony defects with modified perforated membranes in aggressive periodontitis: A 12-month randomized controlled trial. Clin. Oral Investig. 2018, 22, 2819–2828. [Google Scholar] [CrossRef] [Green Version]
- Kawaguchi, H.; Hirachi, A.; Hasegawa, N.; Iwata, T.; Hamaguchi, H.; Shiba, H.; Takata, T.; Kato, Y.; Kurihara, H. Enhancement of Periodontal Tissue Regeneration by Transplantation of Bone Marrow Mesenchymal Stem Cells. J. Periodontol. 2004, 75, 1281–1287. [Google Scholar] [CrossRef]
- Hasegawa, N.; Kawaguchi, H.; Hirachi, A.; Takeda, K.; Mizuno, N.; Nishimura, M.; Koike, C.; Tsuji, K.; Iba, H.; Kato, Y.; et al. Behavior of Transplanted Bone Marrow-Derived Mesenchymal Stem Cells in Periodontal Defects. J. Periodontol. 2006, 77, 1003–1007. [Google Scholar] [CrossRef] [PubMed]
- Mizuno, H.; Hata, K.; Kojima, K.; Bonassar, L.J.; Vacanti, C.A.; Ueda, M. A Novel Approach to Regenerating Periodontal Tissue by Grafting Autologous Cultured Periosteum. Tissue Eng. 2006, 12, 1227–1335. [Google Scholar] [CrossRef]
- Liu, Y.; Zheng, Y.; Ding, G.; Fang, D.; Zhang, C.; Bartold, P.M.; Gronthos, S.; Shi, S.; Wang, S. Periodontal Ligament Stem Cell-Mediated Treatment for Periodontitis in Miniature Swine. Stem Cells 2008, 26, 1065–1073. [Google Scholar] [CrossRef] [Green Version]
- Iwata, T.; Yamato, M.; Tsuchioka, H.; Takagi, R.; Mukobata, S.; Washio, K.; Okano, T.; Ishikawa, I. Periodontal Regeneration With Multi-Layered Periodontal Ligament-Derived Cell Sheets in a Canine Model. Biomaterials 2009, 30, 2716–2723. [Google Scholar] [CrossRef]
- Kishimoto, N.; Honda, Y.; Momota, Y.; Tran, S.D. Dedifferentiated Fat (DFAT) Cells: A Cell Source for Oral and Maxillofacial Tissue Engineering. Oral Dis. 2018, 24, 1161–1167. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fraser, J.K.; Wulur, I.; Alfonso, Z.; Hedrick, M.H. Fat Tissue: An Underappreciated Source of Stem Cells for Biotechnology. Trends Biotechnol. 2006, 24, 150–154. [Google Scholar] [CrossRef] [PubMed]
- Akita, D.; Morokuma, M.; Saito, Y.; Yamanaka, K.; Akiyama, Y.; Sato, M.; Mashimo, T.; Toriumi, T.; Arai, Y.; Kaneko, T.; et al. Periodontal Tissue Regeneration by Transplantation of Rat Adipose-Derived Stromal Cells in Combination With PLGA-Based Solid Scaffolds. Biomed. Res. 2014, 35, 91–103. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tobita, M.; Uysal, A.C.; Ogawa, R.; Hyakusoku, H.; Mizuno, H. Periodontal Tissue Regeneration with Adipose-Derived Stem Cells. Tissue Eng. Part A 2008, 14, 945–953. [Google Scholar] [CrossRef] [PubMed]
- Venkataiah, V.S.; Handa, K.; Njuguna, M.M.; Hasegawa, T.; Maruyama, K.; Nemoto, E.; Yamada, S.; Sugawara, S.; Lu, L.; Takedachi, M.; et al. Periodontal Regeneration by Allogeneic Transplantation of Adipose Tissue Derived Multi-Lineage Progenitor Stem Cells In Vivo. Sci. Rep. 2019, 9, 921. [Google Scholar] [CrossRef]
- Yagi, K.; Kondo, D.; Okazaki, Y.; Kano, K. A Novel Preadipocyte Cell Line Established From Mouse Adult Mature Adipocytes. Biochem. Biophys. Res. Commun. 2004, 321, 967–974. [Google Scholar] [CrossRef]
- Nobusue, H.; Endo, T.; Kano, K. Establishment of a Preadipocyte Cell Line Derived From Mature Adipocytes of GFP Transgenic Mice and Formation of Adipose Tissue. Cell Tissue Res. 2008, 332, 435–446. [Google Scholar] [CrossRef]
- Nobusue, H.; Kano, K. Establishment and Characteristics of Porcine Preadipocyte Cell Lines Derived from Mature Adipocytes. J. Cell. Biochem. 2010, 109, 542–552. [Google Scholar] [CrossRef]
- Matsumoto, T.; Kano, K.; Kondo, D.; Fukuda, N.; Iribe, Y.; Tanaka, N.; Matsubara, Y.; Sakuma, T.; Satomi, A.; Otaki, M.; et al. Mature Adipocyte-Derived Dedifferentiated Fat Cells Exhibit Multilineage Potential. J. Cell. Physiol. 2008, 215, 210–222. [Google Scholar] [CrossRef]
- Ijichi, N.; Ikeda, K.; Horie-Inoue, K.; Yagi, K.; Okazaki, Y.; Inoue, S. Estrogen-Related Receptor Alpha Modulates the Expression of Adipogenesis-Related Genes During Adipocyte Differentiation. Biochem. Biophys. Res. Commun. 2007, 358, 813–818. [Google Scholar] [CrossRef] [PubMed]
- Oki, Y.; Watanabe, S.; Endo, T.; Kano, K. Mature Adipocyte-Derived Dedifferentiated Fat Cells Can Trans-Differentiate into Osteoblasts In Vitro and In Vivo Only by All-Trans Retinoic Acid. Cell Struct. Funct. 2008, 33, 211–222. [Google Scholar] [CrossRef] [Green Version]
- Kishimoto, N.; Momota, Y.; Hashimoto, Y.; Ando, K.; Omasa, T.; Kotani, J. Dedifferentiated Fat Cells Differentiate Into Osteoblasts in Titanium Fiber Mesh. Cytotechnology 2013, 65, 15–22. [Google Scholar] [CrossRef] [Green Version]
- Kazama, T.; Fujie, M.; Endo, T.; Kano, K. Mature Adipocyte-Derived Dedifferentiated Fat Cells Can Transdifferentiate Into Skeletal Myocytes In Vitro. Biochem. Biophys. Res. Commun. 2008, 377, 780–785. [Google Scholar] [CrossRef] [PubMed]
- Sakuma, T.; Matsumoto, T.; Kano, K.; Fukuda, N.; Obinata, D.; Yamaguchi, K.; Yoshida, T.; Takahashi, S.; Mugishima, H. Mature, Adipocyte Derived, Dedifferentiated Fat Cells Can Differentiate into Smooth Muscle-Like Cells and Contribute to Bladder Tissue Regeneration. J. Urol. 2009, 182, 355–365. [Google Scholar] [CrossRef] [PubMed]
- Obinata, D.; Matsumoto, T.; Ikado, Y.; Sakuma, T.; Kano, K.; Fukuda, N.; Yamaguchi, K.; Mugishima, H.; Takahashi, S. Transplantation of Mature Adipocyte-Derived Dedifferentiated Fat (DFAT) Cells Improves Urethral Sphincter Contractility in a Rat Model. Int. J. Urol. 2011, 18, 827–834. [Google Scholar] [CrossRef]
- Jumabay, M.; Matsumoto, T.; Yokoyama, S.; Kano, K.; Kusumi, Y.; Masuko, T.; Mitsumata, M.; Saito, S.; Hirayama, A.; Mugishima, H.; et al. Dedifferentiated Fat Cells Convert to Cardiomyocyte Phenotype and Repair Infarcted Cardiac Tissue in Rats. J. Mol. Cell. Cardiol. 2009, 47, 565–575. [Google Scholar] [CrossRef]
- Planat-Benard, V.; Silvestre, J.S.; Cousin, B.; André, M.; Nibbelink, M.; Tamarat, R.; Clergue, M.; Manneville, C.; Saillan-Barreau, C.; Duriez, M.; et al. Plasticity of Human Adipose Lineage Cells toward Endothelial Cells: Physiological and Therapeutic Perspectives. Circulation 2004, 109, 656–663. [Google Scholar] [CrossRef]
- Jumabay, M.; Abdmaulen, R.; Urs, S.; Heydarkhan-Hagvall, S.; Chazenbalk, G.D.; Jordan, M.C.; Roos, K.P.; Yao, Y.; Boström, K.I. Endothelial Differentiation in Multipotent Cells Derived from Mouse and Human White Mature Adipocytes. J. Mol. Cell. Cardiol. 2012, 53, 790–800. [Google Scholar] [CrossRef] [Green Version]
- Akita, D.; Kano, K.; Saito-Tamura, Y.; Mashimo, T.; Sato-Shionome, M.; Tsurumachi, N.; Yamanaka, K.; Kaneko, T.; Toriumi, T.; Arai, Y.; et al. Use of Rat Mature Adipocyte-Derived Dedifferentiated Fat Cells as a Cell Source for Periodontal Tissue Regeneration. Front. Physiol. 2016, 7, 50. [Google Scholar] [CrossRef] [Green Version]
- Tsurumachi, N.; Akita, D.; Kano, K.; Matsumoto, T.; Toriumi, T.; Kazama, T.; Oki, Y.; Tamura, Y.; Tonogi, M.; Isokawa, K.; et al. Small Buccal Fat Pad Cells Have High Osteogenic Differentiation Potential. Tissue Eng. Part C Methods 2016, 22, 250–259. [Google Scholar] [CrossRef]
- Suzuki, D.; Akita, D.; Tsurumachi, N.; Kano, K.; Yamanaka, K.; Kaneko, T.; Kawano, E.; Iguchi, S.; Toriumi, T.; Arai, Y.; et al. Transplantation of Mature Adipocyte-Derived Dedifferentiated Fat Cells into Three-Wall Defects in the Rat Periodontium Induces Tissue Regeneration. J. Oral Sci. 2017, 59, 611–620. [Google Scholar] [CrossRef] [Green Version]
- Tsurumachi, N.; Akita, D.; Kano, K.; Matsumoto, T.; Toriumi, T.; Kazama, T.; Oki, Y.; Saito-Tamura, Y.; Tonogi, M.; Shimizu, N.; et al. Effect of Collagenase Concentration on the Isolation of Small Adipocytes from Human Buccal Fat Pad. J. Oral Sci. 2018, 60, 14–23. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sugawara, A.; Sato, S. Application of Dedifferentiated Fat Cells for Periodontal Tissue Regeneration. Hum. Cell 2014, 27, 12–21. [Google Scholar] [CrossRef] [PubMed]
- Tateno, A.; Asano, M.; Akita, D.; Toriumi, T.; Tsurumachi-Iwasaki, N.; Kazama, T.; Arai, Y.; Matsumoto, T.; Kano, K.; Honda, M. Transplantation of Dedifferentiated Fat Cells Combined with a Biodegradable Type I Collagen-Recombinant Peptide Scaffold for Critical-Size Bone Defects in Rats. J. Oral Sci. 2019, 61, 534–538. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, S.; Liu, Y.; Fang, D.; Shi, S. The Miniature Pig: A Useful Large Animal Model for Dental and Orofacial Research. Oral Dis. 2007, 13, 530–537. [Google Scholar] [CrossRef] [PubMed]
- Ide, Y.; Nakahara, T.; Nasu, M.; Matsunaga, S.; Iwanaga, T.; Tominaga, N.; Tamaki, Y. Postnatal Mandibular Cheek Tooth Development in the Miniature Pig Based on Two-Dimensional and Three-Dimensional X-ray Analyses. Anat. Rec. 2013, 296, 1247–1254. [Google Scholar] [CrossRef] [PubMed]
- Ando, A.; Ota, M.; Sada, M.; Katsuyama, Y.; Goto, R.; Shigenari, A.; Kawata, H.; Anzai, T.; Iwanaga, T.; Miyoshi, Y.; et al. Rapid Assignment of the Swine Major Histocompatibility Complex (SLA) Class I and II Genotypes in Clawn Miniature Swine Using PCR-SSP and PCR-RFLP Methods. Xenotransplantation 2005, 12, 121–126. [Google Scholar] [CrossRef]
- Tudor, C.; Bumiller, L.; Birkholz, T.; Stockmann, P.; Wiltfang, J.; Kessler, P. Static and Dynamic Periosteal Elevation: A Pilot Study in a Pig Model. Int. J. Oral Maxillofac. Surg. 2010, 39, 897–903. [Google Scholar] [CrossRef]
- Sonoyama, W.; Liu, Y.; Fang, D.; Yamaza, T.; Seo, B.M.; Zhang, C.; Liu, H.; Gronthos, S.; Wang, C.Y.; Wang, S.; et al. Mesenchymal Stem Cell-Mediated Functional Tooth Regeneration in Swine. PLoS ONE 2006, 1, e79. [Google Scholar] [CrossRef] [Green Version]
- Oltramari, P.V.; Navarro, R.L.; Henriques, J.F.; Capelozza, A.L.; Granjeiro, J.M. Dental and Skeletal Characterization of the BR-1 Minipig. Vet. J. 2007, 173, 399–407. [Google Scholar] [CrossRef]
- Ibi, M.; Ishisaki, A.; Yamamoto, M.; Wada, S.; Kozakai, T.; Nakashima, A.; Iida, J.; Takao, S.; Izumi, Y.; Yokoyama, A.; et al. Establishment of Cell Lines That Exhibit Pluripotency from Miniature Swine Periodontal Ligaments. Arch. Oral Biol. 2007, 52, 1002–1008. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Abukawa, H.; Zhang, W.; Young, C.S.; Asrican, R.; Vacanti, J.P.; Kaban, L.B.; Troulis, M.J.; Yelick, P.C. Reconstructing Mandibular Defects Using Autologous Tissue-Engineered Tooth and Bone Constructs. J. Oral Maxillofac. Surg. 2009, 67, 335–347. [Google Scholar] [CrossRef] [PubMed]
- Ando, Y.; Honda, M.J.; Ohshima, H.; Tonomura, A.; Ohara, T.; Itaya, T.; Kagami, H.; Ueda, M. The Induction of Dentin Bridge-Like Structures by Constructs of Subcultured Dental Pulp-Derived Cells and Porous HA/TCP in Porcine Teeth. Nagoya J. Med. Sci. 2009, 71, 51–62. [Google Scholar] [PubMed]
- Honda, M.J.; Shinmura, Y.; Shinohara, Y. Enamel Tissue Engineering Using Subcultured Enamel Organ Epithelial Cells in Combination With Dental Pulp Cells. Cells Tissues Organs 2009, 189, 261–267. [Google Scholar] [CrossRef]
- Zhang, W.; Abukawa, H.; Troulis, M.J.; Kaban, L.B.; Vacanti, J.P.; Yelick, P.C. Tissue Engineered Hybrid Tooth-Bone Constructs. Methods 2009, 47, 122–128. [Google Scholar] [CrossRef]
- Zheng, Y.; Liu, Y.; Zhang, C.M.; Zhang, H.Y.; Li, W.H.; Shi, S.; Le, A.D.; Wang, S.L. Stem Cells from Deciduous Tooth Repair Mandibular Defect in Swine. J. Dent. Res. 2009, 88, 249–254. [Google Scholar] [CrossRef]
- Ding, G.; Liu, Y.; Wang, W.; Wei, F.; Liu, D.; Fan, Z.; An, Y.; Zhang, C.; Wang, S. Allogeneic Periodontal Ligament Stem Cell Therapy for Periodontitis in Swine. Stem Cells 2010, 28, 1829–1838. [Google Scholar] [CrossRef] [Green Version]
- Yang, J.R.; Hsu, C.W.; Liao, S.C.; Lin, Y.T.; Chen, L.R.; Yuan, K. Transplantation of Embryonic Stem Cells Improves the Regeneration of Periodontal Furcation Defects in a Porcine Model. J. Clin. Periodontol. 2013, 40, 364–371. [Google Scholar] [CrossRef]
- Fawzy El-Sayed, K.M.; Paris, S.; Becker, S.T.; Neuschl, M.; De Buhr, W.; Sälzer, S.; Wulff, A.; Elrefai, M.; Darhous, M.S.; El-Masry, M.; et al. Periodontal Regeneration Employing Gingival Margin-Derived Stem/Progenitor Cells: An Animal Study. J. Clin. Periodontol. 2012, 39, 861–870. [Google Scholar] [CrossRef]
- Takahashi, T.; Watanabe, T.; Nakada, H.; Sato, H.; Tanimoto, Y.; Sakae, T.; Kimoto, S.; Mijares, D.; Zhang, Y.; Kawai, Y. Improved Bone Micro Architecture Healing Time After Implant Surgery in an Ovariectomized Rat. J. Hard Tissue Biol. 2016, 25, 257–262. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Magnusson, I.; Nyman, S.; Karring, T.; Egelberg, J. Connective Tissue Attachment Formation Following Exclusion of Gingival Connective Tissue and Epithelium During Healing. J. Periodont. Res. 1985, 20, 201–208. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Huang, Y.; Deng, X. External Cervical Resorption-A Review of Pathogenesis and Potential Predisposing Factors. Int. J. Oral Sci. 2021, 13, 19. [Google Scholar] [CrossRef] [PubMed]
- Watanabe, H.; Goto, S.; Kato, R.; Komiyama, S.; Nagaoka, Y.; Kazama, T.; Yamamoto, C.; Li, Y.; Konuma, N.; Hagikura, K.; et al. The Neovascularization Effect of Dedifferentiated Fat Cells. Sci. Rep. 2020, 10, 9211. [Google Scholar] [CrossRef] [PubMed]












Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Akita, D.; Kazama, T.; Tsukimura, N.; Taniguchi, Y.; Takahashi, R.; Arai, Y.; Tsurumachi-Iwasaki, N.; Yasuda, H.; Okubo, T.; Kano, K.; et al. Transplantation of Mature Adipocyte-Derived Dedifferentiated Fat Cells Facilitates Periodontal Tissue Regeneration of Class II Furcation Defects in Miniature Pigs. Materials 2022, 15, 1311. https://doi.org/10.3390/ma15041311
Akita D, Kazama T, Tsukimura N, Taniguchi Y, Takahashi R, Arai Y, Tsurumachi-Iwasaki N, Yasuda H, Okubo T, Kano K, et al. Transplantation of Mature Adipocyte-Derived Dedifferentiated Fat Cells Facilitates Periodontal Tissue Regeneration of Class II Furcation Defects in Miniature Pigs. Materials. 2022; 15(4):1311. https://doi.org/10.3390/ma15041311
Chicago/Turabian StyleAkita, Daisuke, Tomohiko Kazama, Naoki Tsukimura, Yoshiki Taniguchi, Rie Takahashi, Yoshinori Arai, Niina Tsurumachi-Iwasaki, Hiroyasu Yasuda, Takahisa Okubo, Koichiro Kano, and et al. 2022. "Transplantation of Mature Adipocyte-Derived Dedifferentiated Fat Cells Facilitates Periodontal Tissue Regeneration of Class II Furcation Defects in Miniature Pigs" Materials 15, no. 4: 1311. https://doi.org/10.3390/ma15041311





