Assessment of Preload Loss after Cyclic Loading in the OT Bridge System in an “All-on-Four” Rehabilitation Model in the Absence of One and Two Prosthesis Screws
Abstract
:1. Introduction
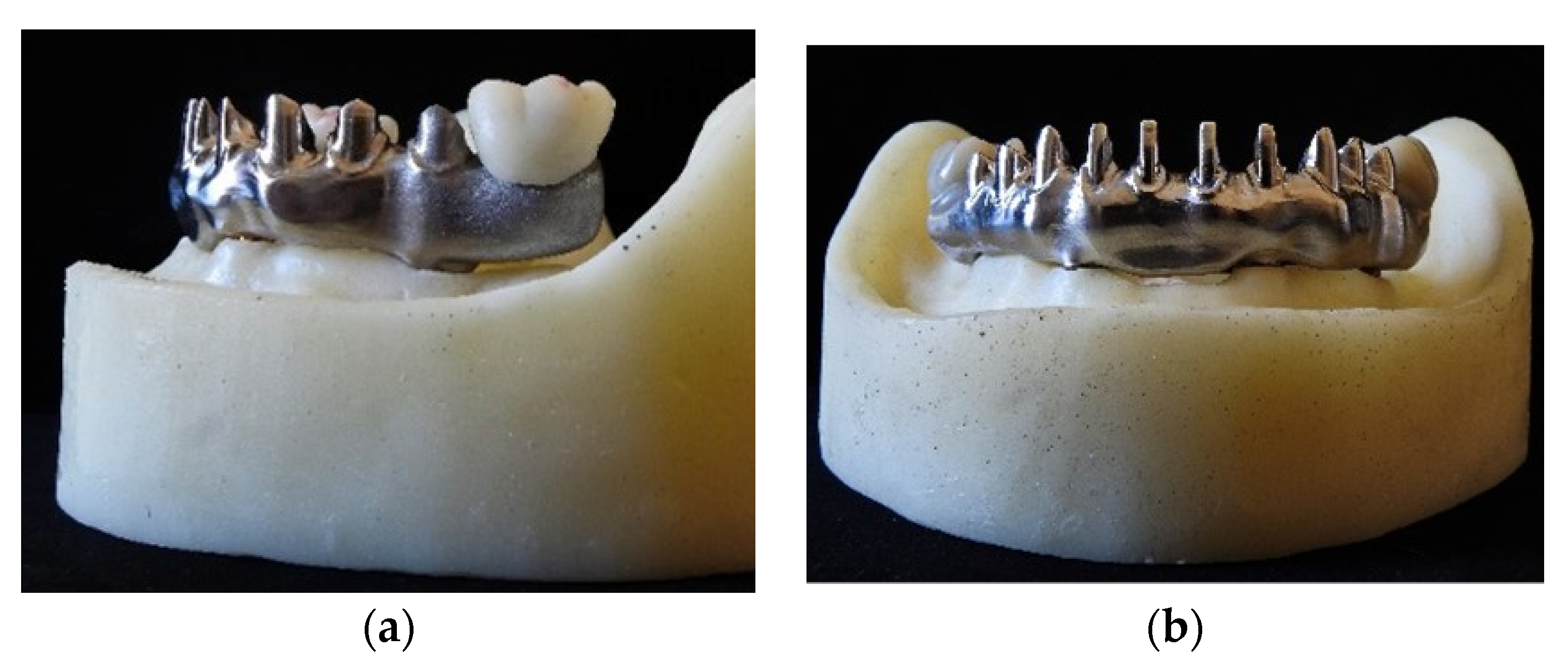
2. Materials and Methods
2.1. Samples Preparation
- Group 1 (Gr.1): Group with 3 tightening screws (33, 36, 46) inserted on 4 implant analogs without the screw in position 43.
- Group 2 (Gr.2): Group with 2 tightening screws (36, 46) inserted on 4 implant analogs without the anterior screws 33 and 43.
- Control Group (Gr.CTR): Group with 4 tightening screws (33, 43, 36, 46 inserted) on 4 implant analogs. This group was the same as that a previous study by Catapano et al. [16].
2.2. Cyclic Test
2.3. Statistical Analysis
- differences between the averages mean values of preload loss for Gr.1, Gr.2, and Gr.CTR;
- differences in preload loss percentage values of the screws in positions 36 and 46 between the three different groups;
- differences in preload loss percentage values of the screws inside each group;
- differences in percentage torque loss of screws positioned in zone 33 for Gr.1 and Gr.CTR.
- differences in percentage torque loss between the screws positioned in zones 36 and 46 in Gr.2.
- absence of removal torque difference between the three groups (intergroups analysis—H0 nr.1);
- absence of removal torque difference between the values of the screws within each group (intragroup analysis—H0 nr.2).
3. Results
- There were no significant statistical differences in torque mean values between Gr.1, Gr.2, and Gr.CTR (p-value = 0.2670).
- There were no significant statistical differences between the percentages of preload loss for the screw in position 36 between the three different groups (p-value = 0.0569).
- There were no significant statistical differences between the percentages in preload loss for the screw in position 46 between the three different groups (p-value = 0.4177).
- The difference between the screws in positions 36 and 46 and 33 and 46 in Gr.1 showed no statistically significant difference, with p-value = 0.0193.
- A statistically significant difference between the percentages of preload loss between the screws in positions 33 and 36 in Gr.1 was found equal to 15.2% (p-value = 0.0176) (Table 2).
- There was no statistical significant difference between the percentages of torque loss between screws in positions 33 and 46 (p-value = 0.4184) and between screws in positions 36 and 46 (p-value = 0.3123) in Gr.1.
- There were no statistically significant differences between Gr.1 and Gr.CTR for the screw in position 33 (p-value = 0.1114).
- A p-value = 0.6465 was calculated, and therefore there was no statistical significant difference between the individual screws 36 and 46 within Gr.2.
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Soto-Peñaloza, D.; Zaragozí-Alonso, R.; Peñarrocha-Diago, M.; Peñarrocha-Diago, M. The all-on-four treatment concept: Systematic review. J. Clin. Exp. Dent. 2017, 9, e474–e488. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Moraschini, V.; Poubel, L.D.C.; Ferreira, V.; Barboza, E.D.S. Evaluation of survival and success rates of dental implants reported in longitudinal studies with a follow-up period of at least 10 years: A systematic review. Int. J. Oral Maxillofac. Surg. 2015, 44, 377–388. [Google Scholar] [CrossRef] [PubMed]
- Maló, P.; Nobre, M.D.A.; Lopes, A.; Francischone, C.; Rigolizzo, M. “All-on-4” Immediate-Function Concept for Completely Edentulous Maxillae: A Clinical Report on the Medium (3 Years) and Long-Term (5 Years) Outcomes. Clin. Implant Dent. Relat. Res. 2012, 14 (Suppl. 1), e139–e150. [Google Scholar] [CrossRef] [PubMed]
- Maló, P.; Rangert, B.; Nobre, M. “All-on-Four” Immediate-Function Concept with Brånemark System® Implants for Completely Edentulous Mandibles: A Retrospective Clinical Study. Clin. Implant Dent. Relat. Res. 2003, 5 (Suppl. 1), 2–9. [Google Scholar] [CrossRef] [PubMed]
- Duyck, J.; Van Oosterwyck, H.; Sloten, J.V.; De Cooman, M.; Puers, R.; Naert, I. Magnitude and distribution of occlusal forces on oral implants supporting fixed prostheses: An in vivo study. Clin. Oral Implant. Res. 2000, 11, 465–475. [Google Scholar] [CrossRef]
- Shadid, R.; Sadaqa, N. A Comparison Between Screw- and Cement-Retained Implant Prostheses. A Literature Review. J. Oral Implant. 2012, 38, 298–307. [Google Scholar] [CrossRef] [Green Version]
- Ortensi, L.; Ortensi, M.; Minghelli, A.; Grande, F. Implant-Supported Prosthetic Therapy of an Edentulous Patient: Clinical and Technical Aspects. Prosthesis 2020, 2, 140–152. [Google Scholar] [CrossRef]
- Pellegrino, G.; Basile, F.; Relics, D.; Ferri, A.; Grande, F.; Tarsitano, A.; Marchetti, C. Computer-Aided Rehabilitation Supported by Zygomatic Implants: A Cohort Study Comparing Atrophic with Oncologic Patients after Five Years of Follow-Up. J. Clin. Med. 2020, 9, 3254. [Google Scholar] [CrossRef]
- Gonçalves, F.; Lucia, V.; Campestrini, L.; Rigo-Rodrigues, M.A.; Rocha Zanardi, P. Effect of the Attachment System on the Biomechanical and Clinical Performance of Overdentures: A Systematic Review. J. Prosthet. Dent. 2020, 123, 589–594. [Google Scholar] [CrossRef]
- Nithyapriya, S.; Ramesh, A.; Kirubakaran, A.; Mani, J.; Raghunathan, J. Systematic analysis of factors that cause loss of preload in dental implants. J. Indian Prosthodont. Soc. 2018, 18, 189–195. [Google Scholar] [CrossRef]
- Byrne, D.; Jacobs, S.; O’Connell, B.; Houston, F.; Claffey, N. Preloads Generated with Repeated Tightening in Three Types of Screws Used in Dental Implant Assemblies. J. Prosthodont. 2006, 15, 164–171. [Google Scholar] [CrossRef] [PubMed]
- Pjetursson, B.E.; Brägger, U.; Lang, N.P.; Zwahlen, M. Comparison of survival and complication rates of tooth-supported fixed dental prostheses (FDPs) and implant-supported FDPs and single crowns (SCs). Clin. Oral Implant. Res. 2007, 18 (Suppl. 3), 97–113. [Google Scholar] [CrossRef] [PubMed]
- Goodacre, C.J.; Bernal, G.; Rungcharassaeng, K.; Kan, J.Y. Clinical complications with implants and implant prostheses. J. Prosthet. Dent. 2003, 90, 121–132. [Google Scholar] [CrossRef]
- Pellegrino, G.; Grande, F.; Ferri, A.; Pisi, P.; Gandolfi, M.G.; Marchetti, C. Three-Dimensional Radiographic Evaluation of the Malar Bone Engagement Available for Ideal Zygomatic Implant Placement. Methods Protoc. 2020, 3, 52. [Google Scholar] [CrossRef]
- Sailer, I.; Mühlemann, S.; Zwahlen, M.; Hämmerle, C.H.; Schneider, D. Cemented and screw-retained implant reconstructions: A systematic review of the survival and complication rates. Clin. Oral Implant. Res. 2012, 23 (Suppl. 6), 163–201. [Google Scholar] [CrossRef] [PubMed]
- Catapano, S.; Ferrari, M.; Mobilio, N.; Montanari, M.; Corsalini, M.; Grande, F. Comparative Analysis of the Stability of Prosthetic Screws under Cyclic Loading in Implant Prosthodontics: An In Vitro Study. Appl. Sci. 2021, 11, 622. [Google Scholar] [CrossRef]
- Davoudi, A.; Rismanchian, M. Effects of modifying implant screw access channels on the amount of extruded excess cement and retention of cement-retained implant-supported dental prostheses: A systematic review. J. Prosthet. Dent. 2018, 121, 52–58. [Google Scholar] [CrossRef]
- Wittneben, J.G.; Joda, T.; Weber, H.P.; Brägger, U. Screw retained vs. cement retained implant-supported fixed dental prosthesis. Periodontology 2000 2017, 73, 141–151. [Google Scholar] [CrossRef]
- Mobilio, N.; Catapano, S. Use of monolithic lithium disilicate for implant abutment and crown: A clinical report. J. Osseointegration 2019, 11, 504–506. [Google Scholar] [CrossRef]
- Mobilio, N.; Fasiol, A.; Catapano, S. Survival Rates of Lithium Disilicate Single Restorations: A Retrospective Study. Int. J. Prosthodont. 2018, 31, 283–286. [Google Scholar] [CrossRef]
- Mobilio, N.; Catapano, S. The use of monolithic lithium disilicate for posterior screw-retained implant crowns. J. Prosthet. Dent. 2017, 118, 703–705. [Google Scholar] [CrossRef] [PubMed]
- Kher, U.; Tunkiwala, A.; Patil, P.G. Management of unfavorable implant positions and angulations in edentulous maxillae with different complete-arch fixed prosthetic designs: A case series and clinical guidelines. J. Prosthet. Dent. 2020, 127, 6–14. [Google Scholar] [CrossRef] [PubMed]
- Acampora, R.; Montanari, M.; Scrascia, R.; Ferrari, E.; Pasi, M.; Cervino, G.; Meloni, S.M.; Lumbau, A.I.; Xhanari, E.; Koshovari, A.; et al. 1-Year Evaluation of OT Bridge Abutments for Immediately Loaded Maxillary Fixed Restorations: A Multicenter Study. Eur. J. Dent. 2021, 15, 290–294. [Google Scholar] [CrossRef] [PubMed]
- Cervino, G.; Cicciù, M.; Fedi, S.; Milone, D.; Fiorillo, L. FEM Analysis Applied to OT Bridge Abutment with Seeger Retention System. Eur. J. Dent. 2021, 15, 47–53. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez, A.M.; Aquilino, S.A.; Lund, P.S. TOPICS OF INTEREST Cantilever and implant biomechanics: A review of the literature, Part 2. J. Prosthodont. 1994, 3, 114–118. [Google Scholar] [CrossRef]
- Storelli, S.; Del Fabbro, M.; Scanferla, M.; Palandrani, G.; Romeo, E. Implant-supported cantilevered fixed dental rehabilitations in fully edentulous patients: Systematic review of the literature. Part II. Clin. Oral Implant. Res. 2018, 29, 275–294. [Google Scholar] [CrossRef] [Green Version]
- Sistemi Di Prova Elettrodinamici MTS Acumen ® Fornire Modi Più Silenziosi, Semplici e Rapidi per Ottenere Dati Migliori. Available online: https://www.mts.com/it/products/materials/dynamic-materials-test-systems/acumen-electrodynamic (accessed on 18 January 2022).
- Wiskott, H.W.; Nicholls, J.I.; Belser, U.C. Stress fatigue: Basic principles and prosthodontic implications. Int. J. Prosthodont. 1995, 8, 105–116. Available online: https://pubmed.ncbi.nlm.nih.gov/7575960/ (accessed on 18 January 2022).
- Zhu, Y.; Hsu, W.H.; Hollis, J.H. Increasing the number of masticatory cycles is associated with reduced appetite and altered postprandial plasma concentrations of gut hormones, insulin and glucose. Br. J. Nutr. 2013, 110, 384–390. [Google Scholar] [CrossRef]
- Gaddale, R.; Mishra, S.K.; Chowdhary, R. Complications of screw- and cement-retained implant-supported full-arch restorations: A systematic review and meta-analysis. Int. J. Oral Implantol. 2020, 13, 11–40. Available online: http://www.ncbi.nlm.nih.gov/pubmed/32186285 (accessed on 18 January 2022).
- de Carvalho, L.P.; de Carvalho, A.M.; Francischone, C.E.; Amaral, F.L.B.D.; Sotto-Maior, B.S. Biomechanical behavior of atrophic maxillary restorations using the all-on-four concept and long trans-sinus implants: A finite element analysis. J. Dent. Res. Dent. Clin. Dent. Prospect. 2021, 15, 106–110. [Google Scholar] [CrossRef]



| GR.CTR Screwed at 25 Ncm | GR.1 Screwed at 25 Ncm | GR.2 Screwed at 25 Ncm | |||||||
| 33 | 43 | 36 | 46 | 33 | 36 | 46 | 36 | 46 | |
| First unscrewing | 16 Ncm = 36% | 14 Ncm = 44% | 13 Ncm = 48% | 12 Ncm = 52% | 12 Ncm = 52% | 15 Ncm = 40% | 15 Ncm = 40% | 13 Ncm = 48% | 12 Ncm = 52% |
| Second unscrewing | 15 Ncm = 40% | 14 Ncm = 44% | 13 Ncm = 48% | 13 Ncm = 48% | 18 Ncm = 28% | 18 Ncm = 28% | 15 Ncm = 40% | 15 Ncm = 40% | 12 Ncm = 52% |
| Third unscrewing | 14 Ncm = 44% | 14 Ncm = 44% | 15 Ncm = 40% | 13 Ncm = 48% | 13 Ncm = 48% | 16 Ncm = 36% | 15 Ncm = 40% | 18 Ncm = 28% | 16 Ncm = 36% |
| Fourth unscrewing | 17 Ncm = 32% | 15 Ncm = 40% | 11 Ncm = 56% | 16 Ncm = 36% | 11 Ncm = 56% | 18 Ncm = 28% | 15 Ncm = 40% | 16 Ncm = 36% | 16 Ncm = 36% |
| Second unscrewing | 16 Ncm = 36% | 10 Ncm = 60% | 15 Ncm = 40% | 16 Ncm = 36% | 12 Ncm = 52% | 18 Ncm = 28% | 15 Ncm = 40% | 10 Ncm = 60% | 12 Ncm = 52% |
| SD | 1.14 Ncm = 4.56% | 1.95 Ncm = 7.80% | 1.67 Ncm = 6.69% | 1.87 Ncm = 7.48% | 2.77 Ncm = 11.10% | 1.41 Ncm = 5.66% | 0 | 2.52 Ncm = 12.20% | 2.31 Ncm = 8.76% |
| Mean | 15.6 Ncm = 37.6% | 13.4 Ncm = 46.4% | 13.4 Ncm = 46.4% | 14 Ncm = 44% | 13.2 Ncm = 47.2% | 17 Ncm = 32% | 15 Ncm = 40% | 14.4 Ncm = 42.4% | 13.6 Ncm = 45.6% |
| Bonferroni’s Multiple Comparisons Test | Mean Diff | 95.00% CI of Diff | Below Threshold? | Summary | Adjusted p Value | |
|---|---|---|---|---|---|---|
| 33 vs. 36 | 15.20 | 2.556 to 27.84 | Yes | * | 0.0176 | A–B |
| 33 vs. 46 | 7.200 | −5.444 to 19.84 | No | ns | 0.4184 | A–C |
| 36 vs. 46 | −8.000 | −20.64 to 4.644 | No | ns | 0.3123 | B–C |
| Test details | Mean 1 | Mean 2 | Mean Diff | SE of diff | n1 | n2 |
| 33 vs. 36 | 47.20 | 32.00 | 15.20 | 4.549 | 5 | 5 |
| 33 vs. 46 | 47.20 | 40.00 | 7.200 | 4.549 | 5 | 5 |
| 36 vs. 46 | 32.00 | 40.00 | −8.000 | 4.549 | 5 | 5 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pozzan, M.C.; Grande, F.; Mochi Zamperoli, E.; Tesini, F.; Carossa, M.; Catapano, S. Assessment of Preload Loss after Cyclic Loading in the OT Bridge System in an “All-on-Four” Rehabilitation Model in the Absence of One and Two Prosthesis Screws. Materials 2022, 15, 1582. https://doi.org/10.3390/ma15041582
Pozzan MC, Grande F, Mochi Zamperoli E, Tesini F, Carossa M, Catapano S. Assessment of Preload Loss after Cyclic Loading in the OT Bridge System in an “All-on-Four” Rehabilitation Model in the Absence of One and Two Prosthesis Screws. Materials. 2022; 15(4):1582. https://doi.org/10.3390/ma15041582
Chicago/Turabian StylePozzan, Mario Cesare, Francesco Grande, Edoardo Mochi Zamperoli, Fabio Tesini, Massimo Carossa, and Santo Catapano. 2022. "Assessment of Preload Loss after Cyclic Loading in the OT Bridge System in an “All-on-Four” Rehabilitation Model in the Absence of One and Two Prosthesis Screws" Materials 15, no. 4: 1582. https://doi.org/10.3390/ma15041582








