Conventional and Digital Impressions for Fabrication of Complete Implant-Supported Bars: A Comparative In Vitro Study
Abstract
:1. Introduction
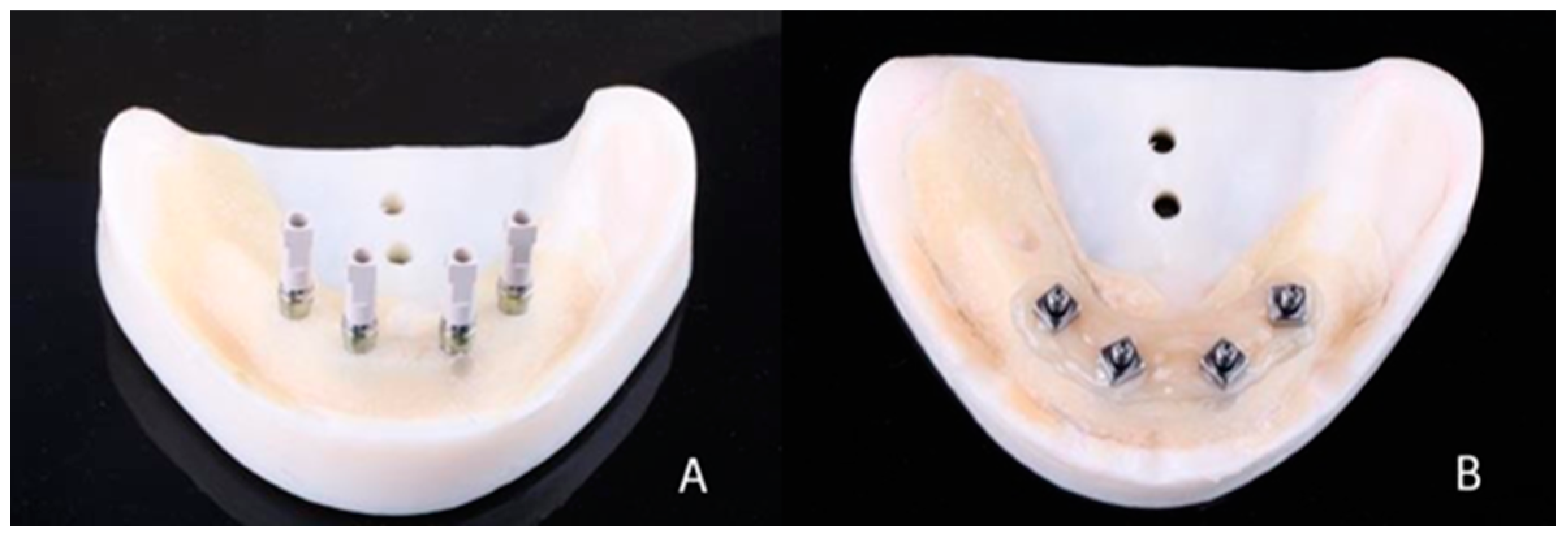
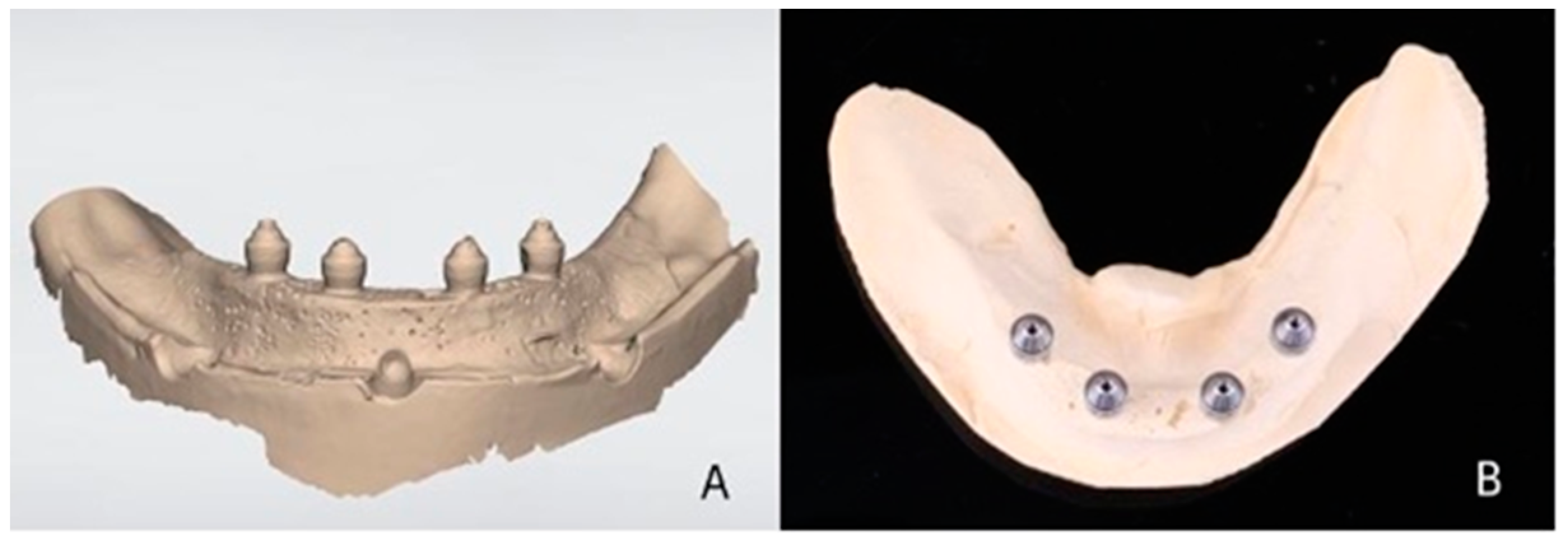
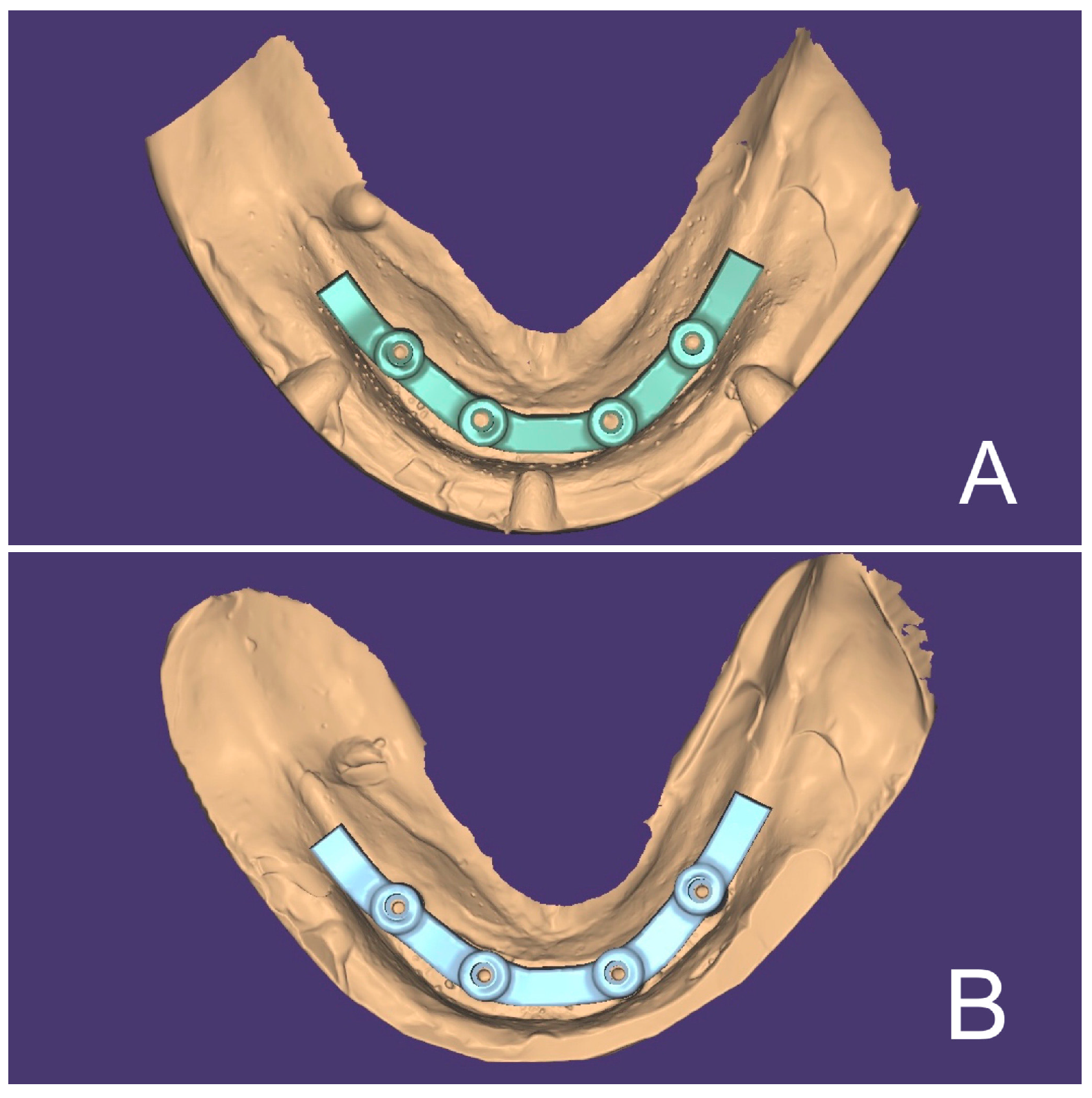
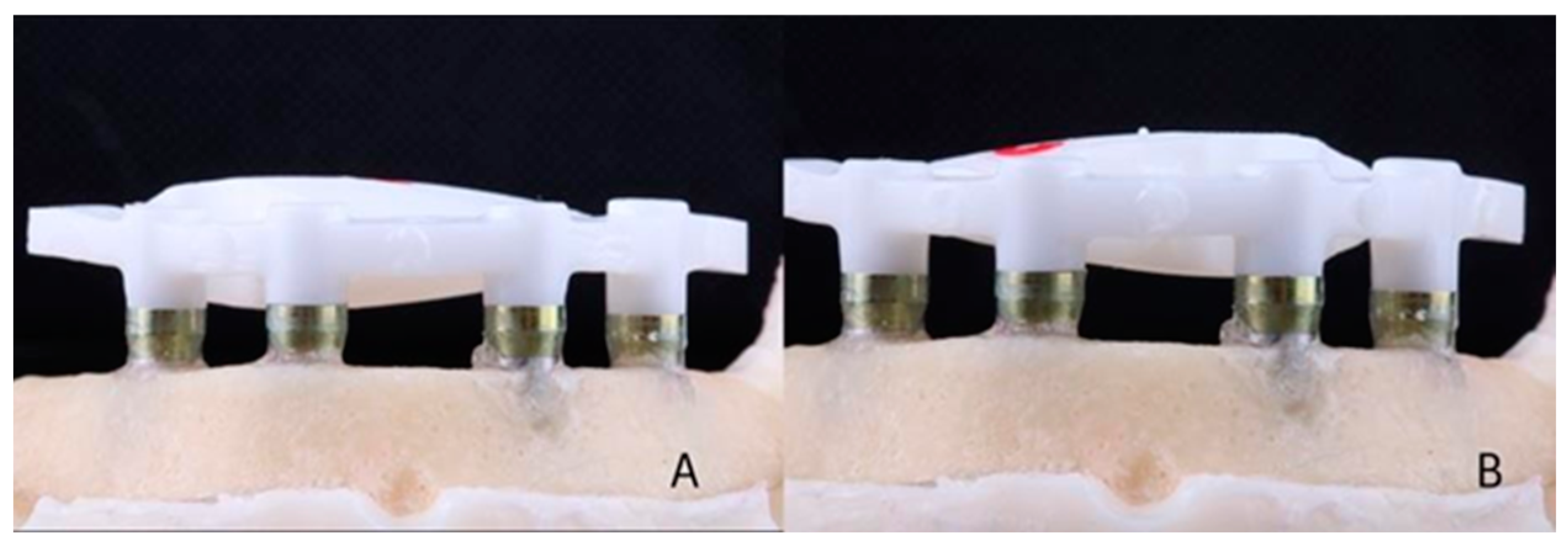
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Chrcanovic, B.R.; Kisch, J.; Larsson, C. Retrospective evaluation of implant-supported full-arch fixed dental prostheses after a mean follow-up of 10 years. Clin. Oral Implants Res. 2020, 31, 634–645. [Google Scholar] [CrossRef] [Green Version]
- Pjetursson, B.E.; Thoma, D.; Jung, R.; Zwahlen, M.; Zembic, A. A systematic review of the survival and complication rates of implant-supported fixed dental prostheses (FDPs) after a mean observation period of at least 5 years. Clin. Oral Implants Res. 2012, 23 (Suppl. S6), 22–38. [Google Scholar] [CrossRef] [PubMed]
- Wittneben, J.G.; Buser, D.; Salvi, G.E.; Burgin, W.; Hicklin, S.; Bragger, U. Complication and failure rates with implant- supported fixed dental prostheses and single crowns: A 10-year retrospective study. Clin. Implant Dent. Relat. Res. 2013, 16, 356–364. [Google Scholar] [CrossRef] [PubMed]
- Francetti, L.; Cavalli, N.; Taschieri, S.; Corbella, S. Ten years follow-up retrospective study on implant survival rates and prevalence of peri-implantitis in implant-supported full-arch rehabilitations. Clin. Oral Implants Res. 2019, 30, 252–260. [Google Scholar] [CrossRef] [PubMed]
- Abduo, J.; Judge, R.B. Implications of implant framework misfit: A systematic review of biomechanical sequelae. Int. J. Oral Maxillofac. Implants 2014, 29, 608–621. [Google Scholar] [CrossRef]
- Pan, Y.; Tsoi, J.K.H.; Lam, W.Y.H.; Pow, E.H.N. Implant framework misfit: A systematic review on assessment methods and clinical complications. Clin. Implant Dent. Relat. Res. 2021, 23, 244–258. [Google Scholar] [CrossRef]
- Karl, M.; Taylor, T.D.; Wichmann, M.G.; Heckmann, S.M. In vivo stress behavior in cemented and screw-retained five- unit implant FPDs. J. Prosthodont. 2006, 15, 20–24. [Google Scholar] [CrossRef] [PubMed]
- Hoods-Moonsammy, V.J.; Owen, P.; Howes, D.G. A comparison of the accuracy of polyether, polyvinyl siloxane, and plaster impressions for long-span implant-supported prostheses. Int. J. Prosthodont. 2014, 27, 433–438. [Google Scholar] [CrossRef] [Green Version]
- Abduo, J.; Yin, L. Fits of Implant Zirconia Custom Abutments and Frameworks: A Systematic Review and Meta-Analyses. Int. J. Oral Maxillofac. Implants 2019, 34, 99–114. [Google Scholar] [CrossRef]
- Papaspyridakos, P.; Chen, C.J.; Gallucci, G.O.; Doukoudakis, A.; Weber, H.P.; Chronopoulos, V. Accuracy of implant impressions for partially and completely edentulous patients: A systematic review. Int. J. Oral Maxillofac. Implants 2014, 29, 836–845. [Google Scholar] [CrossRef]
- Azpiazu-Flores, F.X.; Lee, D.J.; Jurado, C.A.; Nurrohman, H. 3D-Printed Overlay Template for Diagnosis and Planning Complete Arch Implant Prostheses. Healthcare 2023, 11, 1062. [Google Scholar] [CrossRef]
- Chochlidakis, K.; Papaspyridakos, P.; Tsigarida, A.; Romeo, D.; Chen, Y.W.; Natto, Z.; Ercoli, C. Digital versus conventional full-arch implant impressions: A prospective study on 16 edentulous maxillae. J. Prosthodont. 2020, 29, 281–286. [Google Scholar] [CrossRef] [PubMed]
- Giachetti, L.; Sarti, C.; Cinelli, F.; Russo, D.S. Accuracy of digital impressions in fixed prosthodontics: A systematic review of clinical studies. Int. J. Prosthodont. 2020, 33, 192–201. [Google Scholar] [CrossRef] [PubMed]
- Al-Meraikhi, H.; Yilmaz, B.; McGlumphy, E.; Brantley, W.; Johnson, W.M. In vitro fit of CAD-CAM complete arch screw-retained titanium and zirconia implant prostheses fabricated on 4 implants. J. Prosthet. Dent. 2018, 119, 409–416. [Google Scholar] [CrossRef]
- Karl, M.; Graef, F.; Schubinski, P.; Taylor, T. Effect of intraoral scanning on the passivity of fit of implant-supported fixed dental prostheses. Quintessence Int. 2012, 43, 555–562. [Google Scholar] [PubMed]
- Lee, S.J.; Betensky, R.A.; Gianneschi, G.E.; Gallucci, G.O. Accuracy of digital versus conventional implant impressions. Clin. Oral Implants Res. 2015, 26, 715–719. [Google Scholar] [CrossRef] [Green Version]
- Wismeijer, D.; Joda, T.; Flügge, T.; Fokas, G.; Tahmaseb, A.; Bechelli, D.; Bohner, L.; Bornstein, M.; Burgoyne, A.; Caram, S.; et al. Group 5 ITI consensus report: Digital technologies. Clin. Oral Implants Res. 2018, 29, 436–442. [Google Scholar] [CrossRef] [Green Version]
- Flügge, T.; van der Meer, W.J.; Gonzalez, B.G.; Vach, K.; Wismeijer, D.; Wang, P. The accuracy of different dental impression techniques for implant- supported dental prostheses: A systematic review and meta-analysis. Clin. Oral Implants Res. 2018, 29 (Suppl. 16), 374–392. [Google Scholar] [CrossRef] [Green Version]
- Mühlemann, S.; DKraus, R.; Hämmerle, C.H.F.; Thoma, D.S. Is the use of digital technologies for the fabrication of implant-supported reconstructions more eficiente and/or more effective than conventional techniques: A systematic review. Clin. Oral Implants Res. 2018, 29, 184–195. [Google Scholar] [CrossRef] [Green Version]
- Joda, T.; Brägger, U. Digital vs. conventional implant prosthetic workflows: A cost/time analysis. Clin. Oral Implants Res. 2015, 26, 1430–1435. [Google Scholar] [CrossRef]
- Lee, S.J.; Gallucci, G.O. Digital vs. conventional implant impressions: Efficiency outcomes. Clin. Oral Implants Res. 2013, 24, 111–115. [Google Scholar] [CrossRef] [PubMed]
- Wismeijer, D.; Mans, R.; van Genuchten, M.; Reijers, H.A. Patients’ preferences when comparing analogue implant impressions using a polyether impression material versus digital impressions (intraoral scan) of dental implants. Clin. Oral Implants Res. 2014, 25, 1113–1138. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.J.; Macarthur, R.X., 4th; Gallucci, G.O. An evaluation of student and clinician perception of digital and conventional implant impressions. J. Prosthet. Dent. 2013, 110, 420–423. [Google Scholar] [CrossRef] [PubMed]
- Basaki, K.; Alkumru, H.; De Souza, G.; Finer, Y. Accuracy of digital vs conventional implant impression approach: A three-dimensional comparative in vitro analysis. Int. J. Oral Maxillofac. Implants 2017, 32, 792–799. [Google Scholar] [CrossRef] [Green Version]
- Uribarri, A.; Bilbao-Uriarte, E.; Segurola, A.; Ugarte, D.; Verdugo, F. Marginal and internal fit of CAD/CAM frameworks in multiple implant-supported restorations: Scanning and milling error analysis. Clin. Implant Dent. Relat. Res. 2019, 21, 1062–1072. [Google Scholar] [CrossRef]
- Canullo, L.; Colombo, M.; Menini, M.; Sorge, P.; Pesce, P. Trueness of Intraoral Scanners Considering Operator Experience and Three Different Implant Scenarios: A Preliminary Report. Int. J. Prosthodont. 2021, 34, 250–253. [Google Scholar] [CrossRef]
- Kihara, H.; Hatakeyama, W.; Komine, F.; Takafuji, K.; Takahashi, T.; Yokota, J.; Oriso, K.; Kondo, H. Accuracy and practicality of intraoral scanner in dentistry: A literature review. J. Prosthodont. Res. 2020, 64, 109–113. [Google Scholar] [CrossRef]
- Watanabe, H.; Fellows, C.; An, H. Digital Technologies for Restorative Dentistry. Dent. Clin. N. Am. 2022, 66, 567–590. [Google Scholar] [CrossRef]
- Chen, Y.; Zhai, Z.; Watanabe, S.; Nakano, T.; Ishigaki, S. Understanding the effect of scan spans on the accuracy of intraoral and desktop scanners. J. Dent. 2022, 124, 104220. [Google Scholar] [CrossRef]
- Kosago, P.; Ungurawasaporn, C.; Kukiattrakoon, B. Comparison of the accuracy between conventional and various digital implant impressions for an implant-supported mandibular complete arch-fixed prosthesis: An in vitro study. J. Prosthodont. 2022; Epub ahead of print. [Google Scholar] [CrossRef]
- Zingari, F.; Meglioli, M.; Gallo, F.; Macaluso, G.M.; Tagliaferri, S.; Ghezzi, B.; Lumetti, S. Predictability of intraoral scanner error for full-arch implant-supported rehabilitation. Clin. Oral Investig. 2023; Epub ahead of print. [Google Scholar] [CrossRef]
- Di Fiore, A.; Meneghello, R.; Graiff, L.; Savio, G.; Vigolo, P.; Monaco, C.; Stellini, E. Full arch digital scanning systems performances for implant-supported fixed dental prostheses: A comparative study of 8 intraoral scanners. J. Prosthodont. Res. 2019, 63, 396–403. [Google Scholar] [CrossRef]
- Carneiro Pereira, A.L.; Medeiros, V.R.; da Fonte Porto Carreiro, A. Influence of implant position on the accuracy of intraoral scanning in fully edentulous arches: A systematic review. J. Prosthet. Dent. 2021, 126, 749–755. [Google Scholar] [CrossRef] [PubMed]
- Abdel-Azim, T.; Zandinejad, A.; Elathamna, E.; Lin, W.; Morton, D. The influence of digital fabrication options on the accuracy of dental implant-based single units and complete-arch frameworks. Int. J. Oral Maxillofac. Implants 2014, 29, 1281–1288. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Papaspyridakos, P.; De Souza, A.; Finkelman, M.; Sicilia, E.; Gotsis, S.; Chen, Y.W.; Vazouras, K.; Chochlidakis, K. Digital vs Conventional Full- Arch Implant Impressions: A Retrospective Analysis of 36 Edentulous Jaws. J. Prosthodont. 2023, 32, 325–330. [Google Scholar] [CrossRef]
- Wulfman, C.; Naveau, A.; Rignon-Bret, C. Digital scanning for complete-arch implant-supported restorations: A systematic review. J. Prosthet. Dent. 2020, 124, 161–167. [Google Scholar] [CrossRef] [PubMed]
- Floriani, F.; Lopes, G.C.; Cabrera, A.; Duarte, W.; Zoidis, P.; Oliveira, D.; Rocha, M.G. Linear Accuracy of Intraoral Scanners for Full-Arch Impressions of Implant-Supported Prostheses: A Systematic Review and Meta-Analysis. Eur. J. Dent. 2023; Epub ahead of print. [Google Scholar] [CrossRef]
- Pera, F.; Pesce, P.; Bagnasco, F.; Pancini, N.; Carossa, M.; Baldelli, L.; Annunziata, M.; Migliorati, M.; Baldi, D.; Menini, M. Comparison of Milled Full-Arch Implant-Supported Frameworks Realized with a Full Digital Workflow or from Conventional Impression: A Clinical Study. Materials 2023, 16, 833. [Google Scholar] [CrossRef]
- Holmes, J.R.; Bayne, S.C.; Holland, G.A.; Sulik, W.D. Considerations in measurement of marginal fit. J. Prosthet. Dent. 1989, 62, 405–408. [Google Scholar] [CrossRef] [PubMed]


| Bar | Digital Impression (DI) | Conventional Impression (CI) | ||
|---|---|---|---|---|
| 1 screw (DI1) | 4 screws (DI4) | 1 screw (CI1) | 4 screws (CI4) | |
| 1 | 103.80 | 38.47 | 167.39 | 31.36 |
| 2 | 39.04 | 34.54 | 60.18 | 34.95 |
| 3 | 64.38 | 55.42 | 20.27 | 14.02 |
| 4 | 84.16 | 66.37 | 100.48 | 114.57 |
| 5 | 180.88 | 102.34 | 161.21 | 183.22 |
| 94.45 (mean) | 59.43 (mean) | 101.90 (mean) | 75.62 (mean) | |
| 53.94 (SD) | 27.22 (SD) | 63.66 (SD) | 71.59 (SD) | |
| Groups | F Value | p Value |
|---|---|---|
| DI1 vs. DI4 | 2.926 | 0.123 |
| CI1 vs. CI4 | 0.013 | 0.907 |
| DI4 vs. CI4 | 2.655 | 0.139 |
| DI1 vs. CI1 | 0.096 | 0.761 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vieira, S.N.V.; Lourenço, M.F.; Pereira, R.C.; França, E.C.; Vilaça, Ê.L.; Silveira, R.R.; Silva, G.C. Conventional and Digital Impressions for Fabrication of Complete Implant-Supported Bars: A Comparative In Vitro Study. Materials 2023, 16, 4176. https://doi.org/10.3390/ma16114176
Vieira SNV, Lourenço MF, Pereira RC, França EC, Vilaça ÊL, Silveira RR, Silva GC. Conventional and Digital Impressions for Fabrication of Complete Implant-Supported Bars: A Comparative In Vitro Study. Materials. 2023; 16(11):4176. https://doi.org/10.3390/ma16114176
Chicago/Turabian StyleVieira, Samanta N. V., Matheus F. Lourenço, Rodrigo C. Pereira, Esdras C. França, Ênio L. Vilaça, Rodrigo R. Silveira, and Guilherme C. Silva. 2023. "Conventional and Digital Impressions for Fabrication of Complete Implant-Supported Bars: A Comparative In Vitro Study" Materials 16, no. 11: 4176. https://doi.org/10.3390/ma16114176
APA StyleVieira, S. N. V., Lourenço, M. F., Pereira, R. C., França, E. C., Vilaça, Ê. L., Silveira, R. R., & Silva, G. C. (2023). Conventional and Digital Impressions for Fabrication of Complete Implant-Supported Bars: A Comparative In Vitro Study. Materials, 16(11), 4176. https://doi.org/10.3390/ma16114176







