Flexural Strength Analysis of Different Complete Denture Resin-Based Materials Obtained by Conventional and Digital Manufacturing
Abstract
:1. Introduction
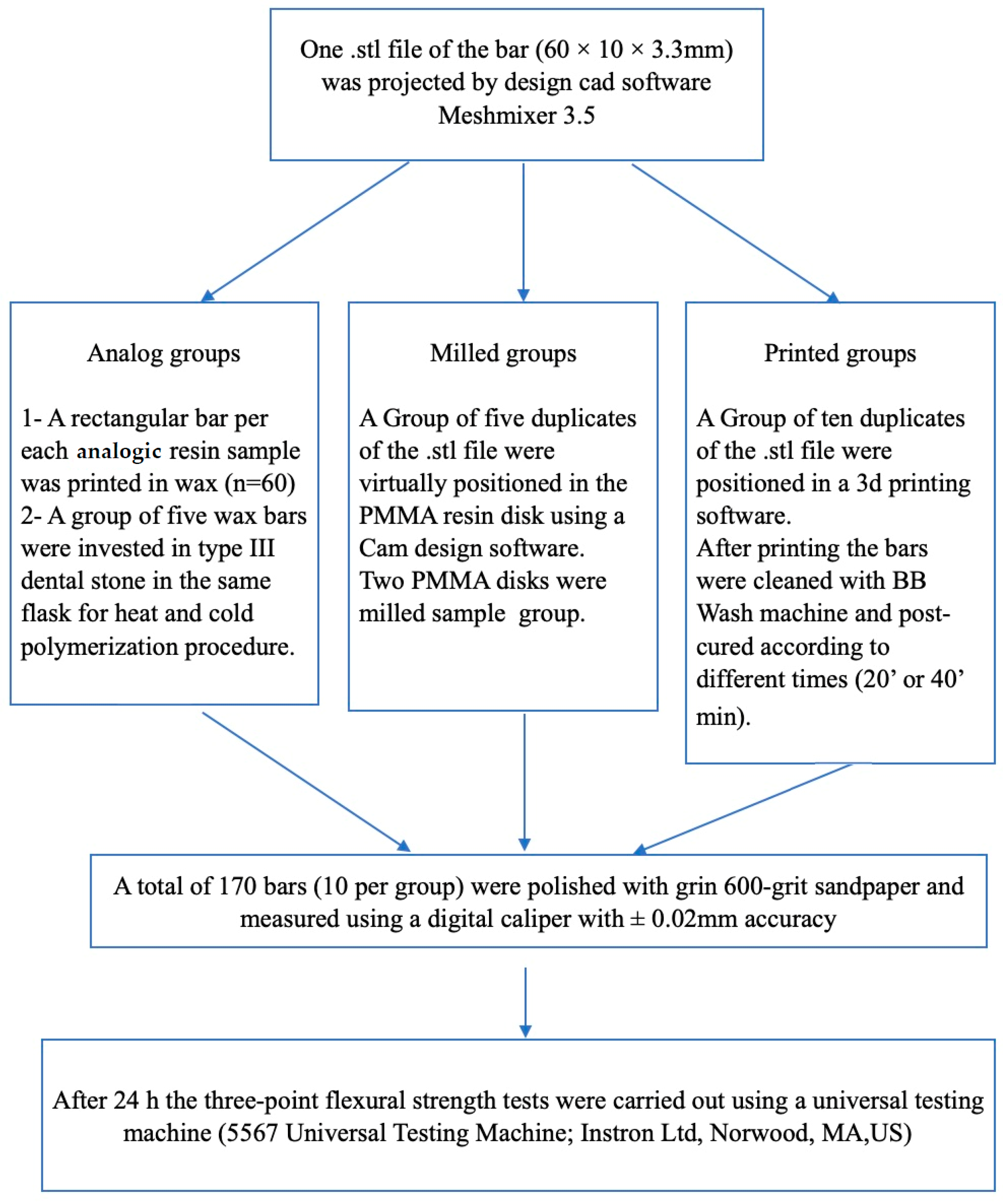
2. Materials and Methods
2.1. Analog Process
2.2. CAD-CAM and Milling Process
2.3. 3D Printing and Curing Process
2.4. Fabrication Accuracy
2.5. Flexural Strength Analysis
2.6. Statistical Analysis
3. Results
3.1. Analog Group
3.2. Milled Group
3.3. 3D-Printed Group Comparison
4. Discussion
5. Conclusions
- Temp Print specimens reported no statistically significant differences with both control groups, Ivotion and AADVA discs, proving that it can be a potential alternative to fabricating removable dentures.
- The experimental 3D-printed Temp Print composite showed promising results with the highest flexural strength within the combination of pink color resin.
- It was confirmed that flexural strength and polymerization methods are correlated.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Xie, Q.; Ding, T.; Yang, G. Rehabilitation of oral function with removable dentures—Still an option? J. Oral Rehabil. 2015, 42, 234–242. [Google Scholar] [CrossRef]
- Ali, S.; Kumar, M.A. Denture Base Resins From Past to New Era. Eur. J. Mol. Clin. Med. 2020, 7, 972–977. [Google Scholar]
- Gautam, R.; Singh, R.D.; Sharma, V.P.; Siddhartha, R.; Chand, P.; Kumar, R. Biocompatibility of polymethylmethacrylate resins used in dentistry. J. Biomed. Mater. Res. B Appl. Biomater. 2012, 100, 1444–1450. [Google Scholar] [CrossRef]
- Alp, G.; Johnston, W.M.; Yilmaz, B. Optical properties and surface roughness of prepolymerized poly(methyl methacrylate) denture base materials. J Prosthet. Dent. 2019, 121, 347–352. [Google Scholar] [CrossRef]
- Sahin, O.; Koroglu, A.; Dede, D.Ö.; Yilmaz, B. Effect of surface sealant agents on the surface roughness and color stability of denture base materials. J. Prosthet. Dent. 2016, 116, 610–616. [Google Scholar] [CrossRef] [PubMed]
- Beyli, M.S.; von Fraunhofer, J.A. An analysis of causes of fracture of acrylic resin dentures. J. Prosthet. Dent. 1981, 46, 238–241. [Google Scholar] [CrossRef] [PubMed]
- Chen, R.; Han, Z.; Huang, Z.; Karki, J.; Wang, C.; Zhu, B.; Zhang, X. Antibacterial activity, cytotoxicity and mechanical behavior of nano-enhanced denture base resin with different kinds of inorganic antibacterial agents. Dent. Mater. J. 2017, 36, 693–699. [Google Scholar] [CrossRef]
- Gad, M.M.; Abualsaud, R.; Al-Thobity, A.M.; Baba, N.Z.; Al-Harbi, F.A. Influence of Addition of Different Nanoparticles on the Surface Properties of Polymethylmethacrylate Denture Base Material. J. Prosthodont. 2020, 29, 422–428. [Google Scholar] [CrossRef]
- Abdulrazzaq Naji, S.; Behroozibakhsh, M.; Jafarzadeh Kashi, T.S.; Eslami, H.; Masaeli, R.; Mahgoli, H.; Tahriri, M.; Lahiji, M.G.; Rakhshan, V. Effects of incorporation of 2.5 and 5 wt% TiO2nanotubes on fracture toughness, flexural strength, and microhardness of denture base poly methyl methacrylate (PMMA). J. Adv. Prosthodont. 2018, 10, 113–121. [Google Scholar] [CrossRef]
- Turagam, N.; Mudrakola, D.P. Effect of micro-additions of carbon nanotubes to polymethylmethacrylate on reduction in polymerization shrinkage. J. Prosthodont. 2013, 22, 105–111. [Google Scholar] [CrossRef]
- Balos, S.; Puskar, T.; Potran, M.; Milekic, B.; Djurovic Koprivica, D.; Laban Terzija, J.; Gusic, I. Modulus, Strength and Cytotoxicity of PMMA-Silica Nanocomposites. Coatings 2020, 10, 583. [Google Scholar] [CrossRef]
- Pryor, W.J. Injection Molding of Plastics for Dentures. J. Am. Dent. Assoc. 1942, 29, 1400–1408. [Google Scholar] [CrossRef]
- Moslehifard, E.; Ghaffari, T.; Abolghasemi, H.; Maleki Dizaj, S. Comparison of Conventional Pressure-packed and Injection Molding Processing Methods for an Acrylic Resin Denture based on Microhardness, Surface Roughness, and Water Sorption. Int. J. Dent. 2022, 2022, 7069507. [Google Scholar] [CrossRef]
- Khan, A.A.; Fareed, M.A.; Alshehri, A.H.; Aldegheishem, A.; Alharthi, R.; Saadaldin, S.A.; Zafar, M.S. Mechanical Properties of the Modified Denture Base Materials and Polymerization Methods: A Systematic Review. Int. J. Mol. Sci. 2022, 23, 5737. [Google Scholar] [CrossRef] [PubMed]
- Steinmassl, P.A.; Wiedemair, V.; Huck, C.; Klaunzer, F.; Steinmassl, O.; Grunert, I.; Dumfahrt, H. Do CAD/CAM dentures really release less monomer than conventional dentures? Clin. Oral Investig. 2017, 21, 1697–1705. [Google Scholar] [CrossRef]
- Steinmassl, O.; Dumfahrt, H.; Grunert, I.; Steinmassl, P.A. CAD/CAM produces dentures with improved fit. Clin. Oral Investig. 2018, 22, 2829–2835. [Google Scholar] [CrossRef] [PubMed]
- Janeva, N.M.; Kovacevska, G.; Elencevski, S.; Panchevska, S.; Mijoska, A.; Lazarevska, B. Advantages of CAD/CAM versus Conventional Complete Dentures—A Review. J. Med. Sci. 2018, 6, 1498–1502. [Google Scholar] [CrossRef] [PubMed]
- Taormina, G.; Sciancalepore, C.; Messori, M.; Bondioli, F. 3D printing processes for photocurable polymeric materials: Technologies, materials, and future trends. J. Appl. Biomater. Funct. Mater. 2018, 16, 151–160. [Google Scholar] [CrossRef]
- Revilla-León, M.; Özcan, M. Additive Manufacturing Technologies Used for Processing Polymers: Current Status and Potential Application in Prosthetic Dentistry. J. Prosthodont. 2019, 28, 146–158. [Google Scholar] [CrossRef]
- Hazeveld, A.; Huddleston Slater, J.J.; Ren, Y. Accuracy and reproducibility of dental replica models reconstructed by different rapid prototyping techniques. Am. J. Orthod. Dentofac. Orthop. 2014, 145, 108–115. [Google Scholar] [CrossRef]
- Kim, S.Y.; Shin, Y.S.; Jung, H.D.; Hwang, C.J.; Baik, H.S.; Cha, J.Y. Precision and trueness of dental models manufactured with different 3-dimensional printing techniques. Am. J. Orthod. Dentofac. Orthop. 2018, 153, 144–153. [Google Scholar] [CrossRef] [PubMed]
- Alshamrani, A.A.; Raju, R.; Ellakwa, A. Effect of Printing Layer Thickness and Postprinting Conditions on the Flexural Strength and Hardness of a 3D-Printed Resin. Biomed. Res. Int. 2022, 2122, 8353137. [Google Scholar] [CrossRef] [PubMed]
- Reymus, M.; Stawarczyk, B. Influence of Different Postpolymerization Strategies and Artificial Aging on Hardness of 3D-Printed Resin Materials: An In Vitro Study. Int. J. Prosthodont. 2020, 33, 634–640. [Google Scholar] [CrossRef]
- Kazanji, M.; Majeed, A.; Hussien, S. The effect of storage and curing time on dimensional changesof visible light cured acrylic denture base (VLCADB). J. Dent. Med. Sci. 2015, 14, 24–26. [Google Scholar]
- Mishra, S.; Chaturvedi, S.; Ali, M.; Pandey, K.K.; Alqahtani, N.M.; Alfarsi, M.A.; Addas, M.K.; Vaddamanu, S.K.; Al Ahmari, N.M.; Alqahtani, S.M.; et al. Dimensional Stability of Light-Activated Urethane Dimethacrylate Denture Base Resins. Polymers 2023, 15, 744. [Google Scholar] [CrossRef]
- ISO 2039-1:2001; Plastics—Determination of Hardness—Part 1: Ball Indentation Method. International Organization for Standardization (ISO): Geneva, Switzerland, 2001. Available online: https://www.iso.org/standard/31264.html/ (accessed on 3 April 2023).
- Lourinho, C.; Salgado, H.; Correia, A.; Fonseca, P. Mechanical Properties of Polymethyl Methacrylate as Denture Base Material: Heat-Polymerized vs. 3D-Printed-Systematic Review and Meta-Analysis of In Vitro Studies. Biomedicines 2022, 10, 2565. [Google Scholar] [CrossRef]
- Abdulwahhab, S.S. High-impact strength acrylic denture base material processed by autoclave. J. Prosthodont. Res. 2013, 57, 288–293. [Google Scholar] [CrossRef]
- De Oliveira Limírio, J.P.J.; Gomes, J.M.L.; Alves Rezende, M.C.R.; Lemos, C.A.A.; Rosa, C.D.D.R.D.; Pellizzer, E.P. Mechanical properties of polymethyl methacrylate as a denture base: Conventional versus CAD-CAM resin—A systematic review and meta-analysis of in vitro studies. J. Prosthet. Dent. 2022, 128, 1221–1229. [Google Scholar] [CrossRef]
- Altarazi, A.; Haider, J.; Alhotan, A.; Silikas, N.; Devlin, H. Assessing the physical and mechanical properties of 3D printed acrylic material for denture base application. Dent. Mater. 2022, 38, 1841–1854. [Google Scholar] [CrossRef]
- Al-Qarni, F.D.; Gad, M.M. Printing Accuracy and Flexural Properties of Different 3D-Printed Denture Base Resins. Materials 2022, 15, 2410. [Google Scholar] [CrossRef]
- Abualsaud, R.; Gad, M.M. Flexural Strength of CAD/CAM Denture Base Materials: Systematic Review and Meta-analysis of In-vitro Studies. J. Int. Soc. Prev. Community Dent. 2022, 12, 160–170. [Google Scholar] [CrossRef] [PubMed]
- Patankar, R.C.; More, V.; Jadhav, R.; Sabane, A.; Kadam, P.; Gachake, A. Comparative evaluation of flexural strength of denture base resin materials processed using compression molding technique, injection molding technique, and computer-aided design CAM technique: An in vitro study. Dent. Res. J. 2022, 19, 100. [Google Scholar]
- Fiore, A.D.; Meneghello, R.; Brun, P.; Rosso, S.; Gattazzo, A.; Stellini, E.; Yilmaz, B. Comparison of the flexural and surface properties of milled, 3D-printed, and heat polymerized PMMA resins for denture bases: An in vitro study. J. Prosthodont. Res. 2022, 66, 502–508. [Google Scholar] [CrossRef]
- Fouda, S.M.; Gad, M.M.; Abualsaud, R.; Ellakany, P.; AlRumaih, H.S.; Khan, S.Q.; Akhtar, S.; Al-Qarni, F.D.; Al-Harbi, F.A. Flexural Properties and Hardness of CAD-CAM Denture Base Materials. J. Prosthodont. 2023, 32, 318–324. [Google Scholar] [CrossRef] [PubMed]
- Asmussen, E.; Peutzfeldt, A. Influence of UEDMA BisGMA and TEGDMA on selected mechanical properties of experimental resin composites. Dent. Mater. 1998, 14, 51–56. [Google Scholar] [CrossRef]
- Cook, W.D.; Moopnar, M. Influence of chemical structure on the fracture behavior of dimethacrylate composite resins. Biomaterials 1990, 11, 272–276. [Google Scholar] [CrossRef]
- Gharechahi, J.; Asadzadeh, N.; Shahabian, F.; Gharechahi, M. Flexural strength of acrylic resin denture bases processed by two different methods. J. Dent. Res. Dent. Clin. Dent. Prospect. 2014, 8, 148–152. [Google Scholar] [CrossRef]
- Dai, J.; Li, P.; Spintzyk, S.; Liu, C.; Xu, S. Influence of additive manufacturing method and build angle on the accuracy of 3D-printed palatal plates. J. Dent. 2023, 132, 104449. [Google Scholar] [CrossRef]
- Rokaya, D.; Srimaneepong, V.; Sapkota, J.; Qin, J.; Siraleartmukul, K.; Siriwongrungson, V. Polymeric materials and films in dentistry: An overview. J. Adv. Res. 2018, 14, 25–34. [Google Scholar] [CrossRef]
- Xu, X.; He, L.; Zhu, B.; Li, J.; Li, J. Advances in polymeric materials for dental applications. Polym. Chem. 2017, 8, 807–823. [Google Scholar] [CrossRef]
- Kerby, R.E.; Knobloch, L.A.; Schricker, S.; Gregg, B. Synthesis and evaluation of modified urethane dimethacrylate resins with reduced water sorption and solubility. Dent. Mater. 2009, 25, 302–313. [Google Scholar] [CrossRef] [PubMed]
- Stansbury, J.W. Synthesis and evaluation of novel multifunctional oligomers for dentistry. J. Dent. Res. 1992, 71, 434–437. [Google Scholar] [CrossRef] [PubMed]
- Aguirre, B.C.; Chen, J.H.; Kontogiorgos, E.D.; Murchison, D.F.; Nagy, W.W. Flexural strength of denture base acrylic resins processed by conventional and CAD-CAM methods. J. Prosthet. Dent. 2020, 123, 641–646. [Google Scholar] [CrossRef] [PubMed]
- Cerbino, E.; Verniani, G.; Bonadeo, G.; Ferrari Cagidiaco, E. Dimensional stability of 3D-printed fixed prosthetic restorations. J. Osseointegration 2022, 15, 79–86. [Google Scholar] [CrossRef]
- Muddugangadhar, B.C.; Mawani, D.P.; Das, A.; Mukhopadhyay, A. Bond strength of soft liners to denture base resins and the influence of different surface treatments and thermocycling: A systematic review. J. Prosthet. Dent. 2020, 123, 800–806. [Google Scholar] [CrossRef]


| Name | Manufacturer | Material Content | Batch n° |
|---|---|---|---|
| ACRYPOL R | Ruthinium-Dental Manufacturing S.p.A., Rovigo, Italy | Heat curing, acrylic resin (PMMA) Liquid: methyl methacrylate, ethylene dimethacrylate (EDMA) Powder: benzoyl peroxide, methyl methacrylate. | Powder: J1584 Liquid: J1571 |
| ACRYSEL P | Ruthinium-Dental Manufacturing S.p.A., Rovigo, Italy | Polymerizable cold-curing resin (PMMA) Liquid: methyl methacrylate, ethylene dimethacrylate, N-N-dimethylparatoluidine. Powder: benzoyl peroxide, methyl methacrylate. | Powder: LOT J0086 Liquid: LOT I0727 |
| ACRYSELF | Ruthinium-Dental Manufacturing S.p.A., Rovigo, Italy | Polymerizable cold-curing resin (PMMA) Liquid: methyl methacrylate, ethylene dimethacrylate, N-N-dimethylparatoluidine Powder: benzoyl peroxide, methyl methacrylate. | Powder: LOT J2163 Liquid: LOT I0727 |
| ACRYPOL HI | Ruthinium-Dental Manufacturing S.p.A., Rovigo, Italy | Heat curing acrylic resin with a high molecular weight (PMMA) Liquid: methyl methacrylate, ethylene dimethacrylate. Powder: benzoyl peroxide, methyl methacrylate. | Powder: LOT H1172 Liquid: LOT J0890 |
| ACRYPOL LL | Ruthinium-Dental Manufacturing S.p.A., Rovigo, Italy | Heat curing acrylic resin with a high molecular weight (PMMA) Liquid: methyl methacrylate, ethylene dimethacrylate. Powder: benzoyl peroxide, methyl methacrylate. | Powder: LOT J1352 Liquid: LOT I1608 |
| ACRYPOL FAST | Ruthinium-Dental Manufacturing S.p.A., Rovigo, Italy | Fast heat curing acrylic resin with high molecular weight (PMMA) Liquid: methyl methacrylate, ethylene dimethacrylate. Powder: benzoyl peroxide, methyl methacrylate. | Powder: LOT I1160 Liquid: LOT H0759 |
| IVOTION (control group) | Ivoclar vivadent, Schaan, Liechtenstein | PMMA Polymethyl methacrylate, pigments. | IBPink-YB5WNZ-117 IBPink-YB5WNZ-118 |
| AADVA DISC (control group) | GC Corporation, Tokyo, Japan | PMMA. | NA |
| NEXTDENT DENTURE 3D+ | NextDent B.V., Soesterberg, The Netherlands | 3D-printed resin (PMMA) 2-hydroxyethyl methacrylate; diphenyl(2,4,6-trimethylbenzoyl) phosphine oxide; 2-hydroxyethyl methacrylate. | WW465N01 |
| GC TEMP PRINT | GC Corporation, Tokyo, Japan | Urethane dimethacrylate (UDMA) dimethacrylate component ** quartz (SiO2) photoinitiator synergist UV-light absorber. | 2,212,091 |
| GC TEMP PRINT+ Pink | GC Corporation, Tokyo, Japan | Urethane dimethacrylate (UDMA) dimethacrylate component ** quartz (SiO2) photoinitiator synergist UV-light absorber Urethane dimethacrylate methacrylate monomer(s) photoinitiator(s). | NA |
| SprintRayEU Denture Base | SprintRay Inc., Los Angeles, CA, USA | 3D-printed resin Ethoxylated bisphenol A dimethacrylate (BisEMA) 7,7,9 (or 7,9,9)-trimethyl-4,13-dioxo-3,14-dioxa-5,12- diazahexadecane-1,16-diyl bismethacrylate, 2-hydroxyethyl methacrylate, Silicon dioxide, diphenyl(2,4,6-trimethylbenzoyl)phosphine oxide, Titanium dioxide. | 50,920,226 |
| Name | Polymerization |
|---|---|
| ACRYPOL R ACRYPOL LL | Place the flask in water at room temperature until completely immersed. Heat the water in about 40/45 min at 70 °C, keep this temperature for 30 min, then bring the water to a boil and keep it for 30 min, then let it cool slowly in the water for another 30 min. Then, removing it from the water, allow the muffle to cool to room temperature. |
| ACRYPOL HI | Place the flask in water at room temperature until completely immersed. Slowly bring the water to the boil in at least 45 min. Simmer for 30 min, then leave to cool slowly in the water for another 30 min. Then, removing it from the water, cool the muffle at room temperature. |
| ACRYPOL FAST | Heat cured in boiling water for 20 min, remove the flask from water and leave it to cool at room temperature. Then, restart the device and bring the water to the boil and keep the temperature constant for 20 min. Remove from the water and cool to room temperature. |
| ACRYSELF ACRYSELF P | Polymerization at a temperature of 22 °C/23 °C starts approximately 12–15 min after mixing. It is recommended to carry out polymerization in a pot at a pressure of 2 ATM (standard atmosphere) for 10 min at a temperature of 45 °C. |
| Name | Polymerization |
|---|---|
| NEXTDENT DENTURE 3D+ | Polymerization with “LaboLight DUO” curing unit for 20 min. |
| NEXTDENT DENTURE 3D+ BB 40” | Polymerization with BB cure unit for 40 min. |
| SPRINTRAYEU DENTURE BASE | Polymerization with “LaboLight DUO” curing unit for 20 min. |
| SPRINTRAYEU DENTURE BASE BB 40” | Polymerization with BB cure unit for 40 min. |
| GC TEMP PRINT | Polymerization with “LaboLight DUO” curing unit for 20 min. |
| GC TEMP PRINT BB 20” | Polymerization with BB cure unit for 20 min. |
| GC TEMP PRINT BB 40” | Polymerization with BB cure unit for 40 min. |
| GC TEMP PRINT PINK BB 20” | Polymerization with BB cure unit for 20 min. |
| GC TEMP PRINT PINK BB 40” | Polymerization with BB cure unit for 40 min. |
| Resin Type | Mean (MPa) | SD | Sign |
|---|---|---|---|
| ACRYPOL R | 89.15 | 14.31 | adghij |
| ACRYSELF P | 86.07 | 7.09 | adghi |
| ACRYSELF | 74.83 | 7.84 | di |
| ACRYPOL HI | 85.58 | 8.60 | adghie |
| ACRYPOL LL | 92.39 | 17.18 | ghj |
| ACRYPOL FAST | 98.86 | 10.66 | hcj |
| IVOTION | 91.88 | 4.43 | egcj |
| AADVA DISC | 107.87 | 7.56 | cj |
| NEXTDENT LABO LIGHT 20” | 60.11 | 5.72 | b |
| SPRINTRAY LABO LIGHT 20” | 54.07 | 3.55 | b |
| TEMP PRINT LABO LIGHT 20” | 75.58 | 9.36 | i |
| TEMP PRINT PINK BB 20” | 95.39 | 9.49 | cghj |
| TEMP PRINT PINK BB 40” | 102.96 | 9.37 | j |
| TEMP PRINT BB 20” | 90.87 | 7.44 | aghj |
| NEXTDENT BB 40” | 83.32 | 8.38 | adgi |
| TEMP PRINT BB 40” | 96.87 | 6.27 | aghcj |
| SPRINTRAY BB 40” | 85.44 | 5.30 | adghij |
| ANOVA value p | F = 24.421 0.000 | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Casucci, A.; Verniani, G.; Barbieri, A.L.; Ricci, N.M.; Ferrari Cagidiaco, E.; Ferrari, M. Flexural Strength Analysis of Different Complete Denture Resin-Based Materials Obtained by Conventional and Digital Manufacturing. Materials 2023, 16, 6559. https://doi.org/10.3390/ma16196559
Casucci A, Verniani G, Barbieri AL, Ricci NM, Ferrari Cagidiaco E, Ferrari M. Flexural Strength Analysis of Different Complete Denture Resin-Based Materials Obtained by Conventional and Digital Manufacturing. Materials. 2023; 16(19):6559. https://doi.org/10.3390/ma16196559
Chicago/Turabian StyleCasucci, Alessio, Giulia Verniani, Anne Lucrèce Barbieri, Nicolò Maria Ricci, Edoardo Ferrari Cagidiaco, and Marco Ferrari. 2023. "Flexural Strength Analysis of Different Complete Denture Resin-Based Materials Obtained by Conventional and Digital Manufacturing" Materials 16, no. 19: 6559. https://doi.org/10.3390/ma16196559





