Comparison between Different Bulk-Fill and Incremental Composite Materials Used for Class II Restorations in Primary and Permanent Teeth: In Vitro Assessments
Abstract
:1. Introduction
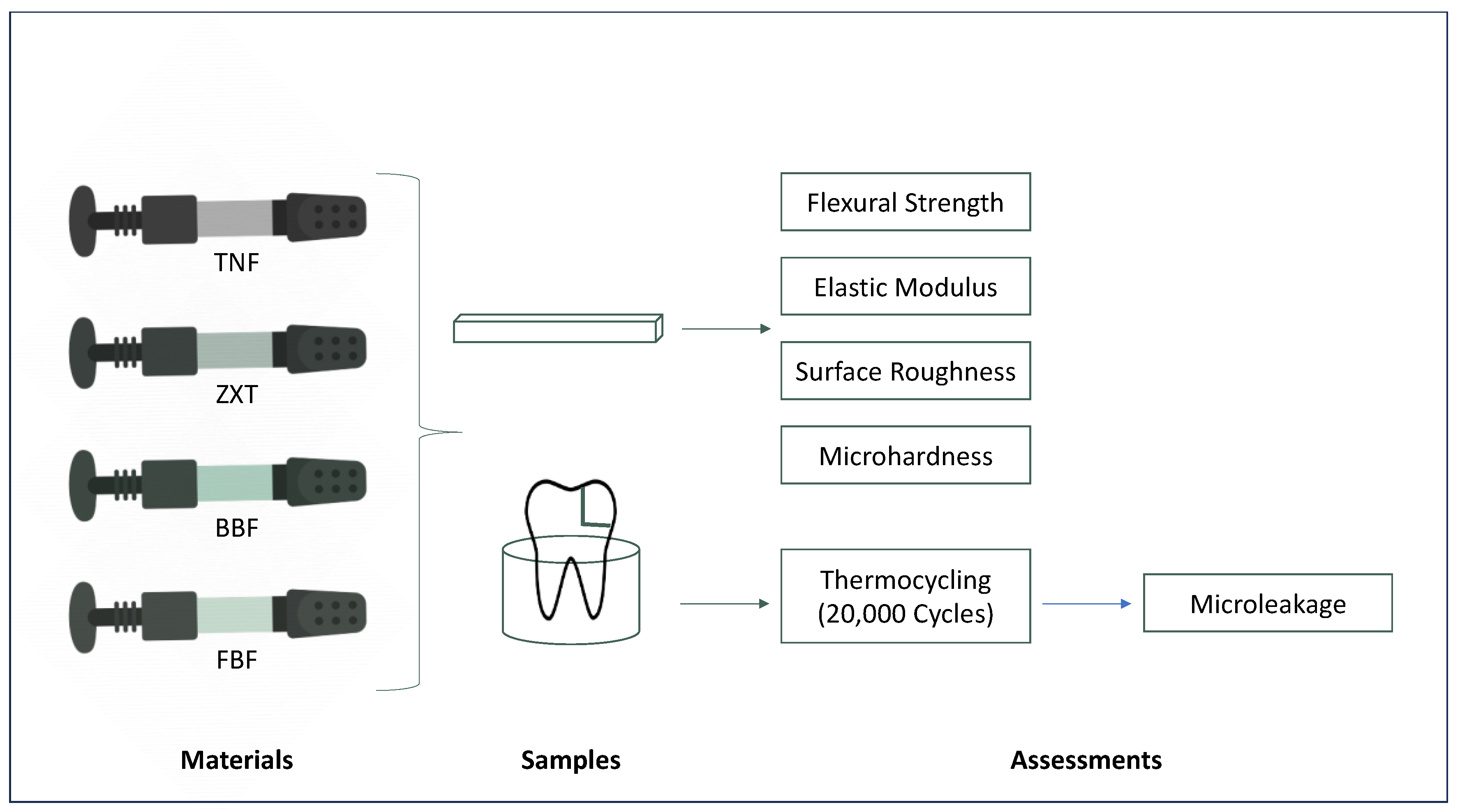
2. Materials and Methods
2.1. Ethical Approval and Study Design
2.2. Flexural Strength and Elastic Modulus
2.2.1. Sample Preparation
2.2.2. Test
2.3. Microhardness
2.3.1. Sample Preparation
2.3.2. Test
2.4. Surface Roughness
2.4.1. Sample Preparation
2.4.2. Test
2.5. Microleakage
2.5.1. Sample Preparation
2.5.2. Test
2.6. Statistical Analysis
3. Results
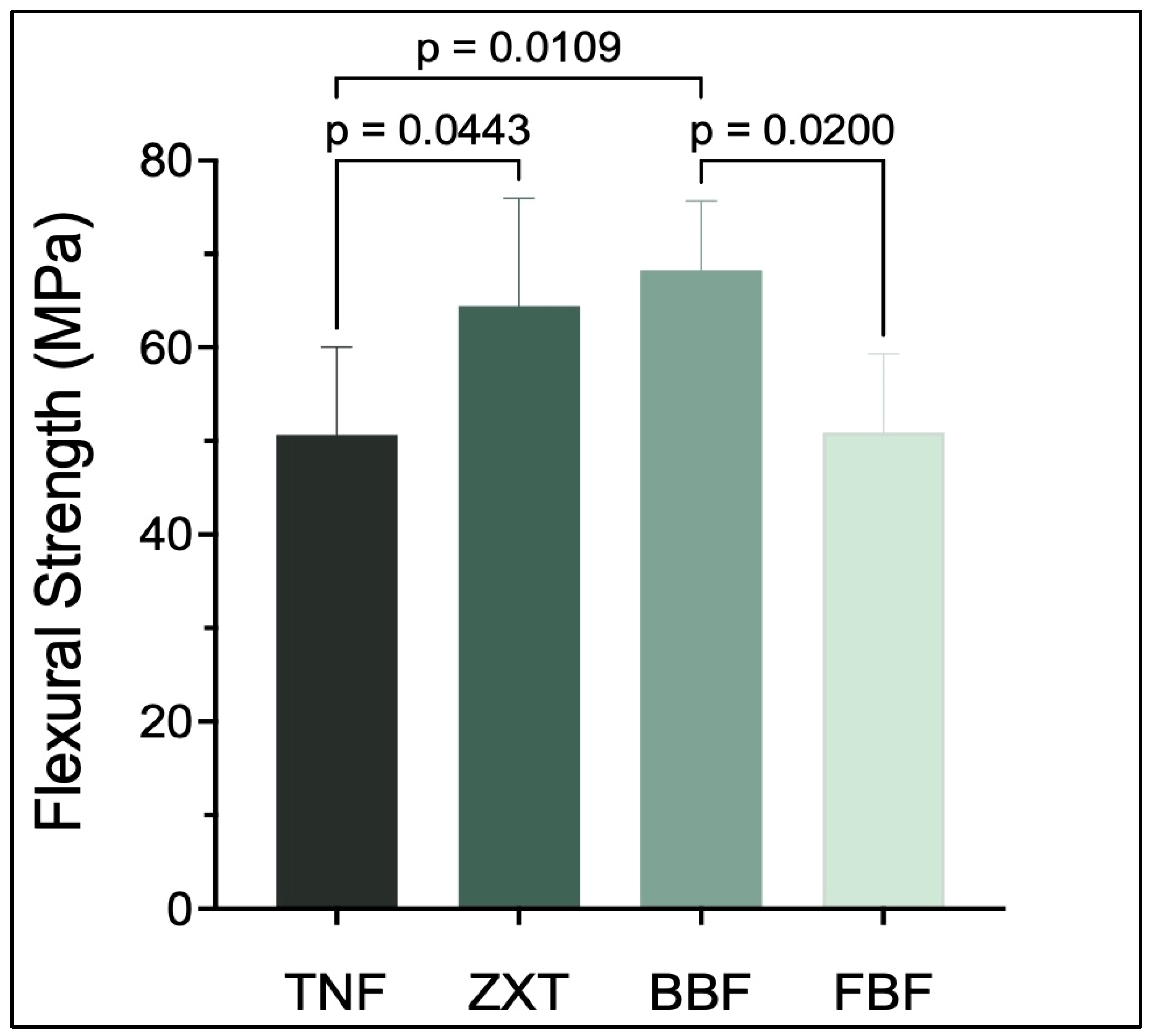
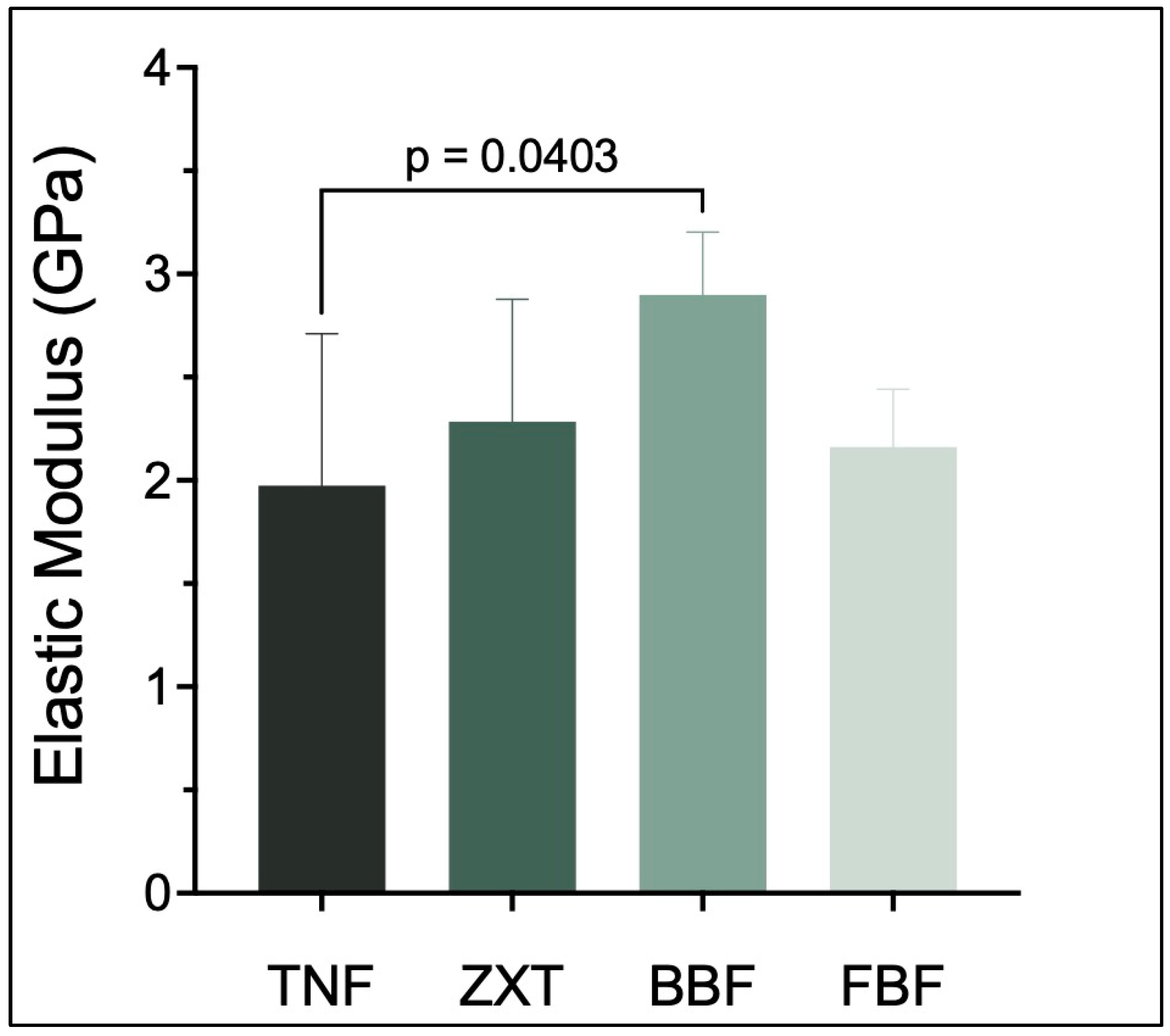
3.1. Flexural Strength and Elastic Modulus
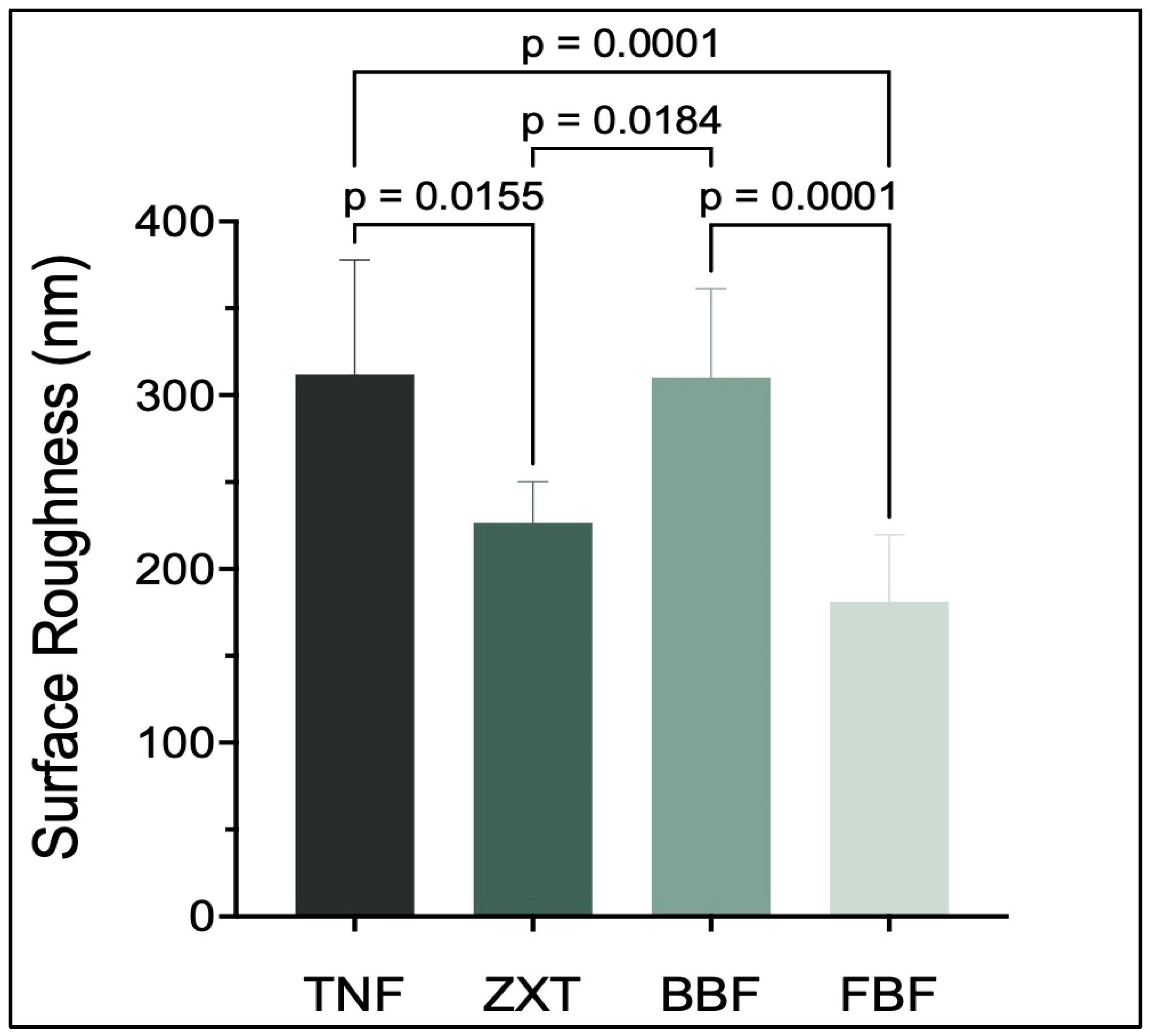
3.2. Surface Roughness
3.3. Microhardness
3.4. Microleakage
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Wei, S.H.Y.; Tang, E.L.K. Composite Resins: A Review of the Types, Properties and Restoration Techniques. Ann. Dent. Univ. Malaya 1994, 1, 28–33. [Google Scholar]
- Chesterman, J.; Jowett, A.; Gallacher, A.; Nixon, P. Bulk-fill resin-based composite restorative materials: A review. Br. Dent. J. 2017, 222, 337–344. [Google Scholar] [CrossRef]
- Fronza, B.M.; Rueggeberg, F.A.; Braga, R.R.; Mogilevych, B.; Soares, L.E.S.; Martin, A.A.; Ambrosano, G.; Giannini, M. Monomer conversion, microhardness, internal marginal adaptation, and shrinkage stress of bulk-fill resin composites. Dent. Mater. 2015, 31, 1542–1551. [Google Scholar] [CrossRef]
- Bahbishi, N.; Mzain, W.; Badeeb, B.; Nassar, H.M. Color stability and micro-hardness of bulk-fill composite materials after exposure to common beverages. Materials 2020, 13, 787. [Google Scholar] [CrossRef]
- Alshali, R.Z.; Salim, N.A.; Satterthwaite, J.D.; Silikas, N. Post-irradiation hardness development, chemical softening, and thermal stability of bulk-fill and conventional resin-composites. J. Dent. 2015, 43, 209–218. [Google Scholar] [CrossRef] [PubMed]
- Tsujimoto, A.; Barkmeier, W.W.; Takamizawa, T.; Latta, M.A.; Miyazaki, M. Depth of cure, flexural properties and volumetric shrinkage of low and high viscosity bulk-fill giomers and resin composites. Dent. Mater. J. 2017, 36, 205–213. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Zhu, M.; Zhu, X. Functional fillers for dental resin composites. Acta Biomater. 2020, 122, 50–65. [Google Scholar] [CrossRef]
- Haugen, H.J.; Marovic, D.; Par, M.; Le Thieu, M.K.; Reseland, J.E.; Johnsen, G.F. Bulk fill composites have similar performance to conventional dental composites. Int. J. Mol. Sci. 2020, 21, 5136. [Google Scholar] [CrossRef] [PubMed]
- Leprince, J.G.; Palin, W.M.; Vanacker, J.; Sabbagh, J.; Devaux, J.; Leloup, G. Physico-mechanical characteristics of commercially available bulk-fill composites. J. Dent. 2014, 42, 993–1000. [Google Scholar] [CrossRef]
- Fronza, B.; Ayres, A.; Pacheco, R.; Rueggeberg, F.; Dias, C.; Giannini, M. Characterization of inorganic filler content, mechanical properties, and light transmission of bulk-fill resin composites. Oper. Dent. 2017, 42, 445–455. [Google Scholar] [CrossRef] [PubMed]
- Rizzante, F.A.P.; Mondelli, R.F.L.; Furuse, A.Y.; Borges, A.F.S.; Mendonça, G.; Ishikiriama, S.K. Shrinkage stress and elastic modulus assessment of bulk-fill composites. J. Appl. Oral Sci. 2019, 27, e20180132. [Google Scholar] [CrossRef]
- AlSahafi, R.; Balhaddad, A.A.; Mitwalli, H.; Ibrahim, M.S.; Melo, M.A.S.; Oates, T.W.; Xu, H.H.; Weir, M.D. Novel crown cement containing antibacterial monomer and calcium phosphate nanoparticles. Nanomaterials 2020, 10, 2001. [Google Scholar] [CrossRef] [PubMed]
- Gowda, V.B.; Murthy, B.V.S.; Hegde, S.; Venkataramanaswamy, S.D.; Pai, V.S.; Krishna, R. Evaluation of Gingival Microleakage in Class II Composite Restorations with Different Lining Techniques: An In Vitro Study. Scientifica 2015, 2015, 896507. [Google Scholar] [CrossRef]
- Arbildo-Vega, H.I.; Lapinska, B.; Panda, S.; Lamas-Lara, C.; Khan, A.S.; Lukomska-Szymanska, M. Clinical Effectiveness of Bulk-Fill and Conventional Resin Composite Restorations: Systematic Review and Meta-Analysis. Polymers 2020, 12, 1786. [Google Scholar] [CrossRef] [PubMed]
- Ilie, N.; Bucuta, S.; Draenert, M. Bulk-fill resin-based composites: An in vitro assessment of their mechanical performance. Oper. Dent. 2013, 38, 618–625. [Google Scholar] [CrossRef] [PubMed]
- van Dijken, J.W.; Pallesen, U. Posterior bulk-filled resin composite restorations: A 5-year randomized controlled clinical study. J. Dent. 2016, 51, 29–35. [Google Scholar] [CrossRef] [PubMed]
- Durão, M.d.A.; de Andrade, A.K.M.; Santos, M.D.C.M.d.S.; Montes, M.A.J.R.; Monteiro, G.Q.d.M. Clinical Performance of Bulk-Fill Resin Composite Restorations Using the United States Public Health Service and Federation Dentaire Internationale Criteria: A 12-Month Randomized Clinical Trial. Eur. J. Dent. 2021, 15, 179–192. [Google Scholar] [CrossRef]
- Lins, R.B.E.; Aristilde, S.; Osório, J.H.; Cordeiro, C.M.; Yanikian, C.R.F.; Bicalho, A.A.; Stape, T.H.S.; Soares, C.J.; Martins, L.R.M. Biomechanical behaviour of bulk-fill resin composites in class II restorations. J. Mech. Behav. Biomed. Mater. 2019, 98, 255–261. [Google Scholar] [CrossRef]
- Marovic, D.; Par, M.; Macan, M.; Klarić, N.; Plazonić, I.; Tarle, Z. Aging-Dependent Changes in Mechanical Properties of the New Generation of Bulk-Fill Composites. Materials 2022, 15, 902. [Google Scholar] [CrossRef]
- de Araújo-Neto, V.G.; Sebold, M.; de Castro, E.F.; Feitosa, V.P.; Giannini, M. Evaluation of physico-mechanical properties and filler particles characterization of conventional, bulk-fill, and bioactive resin-based composites. J. Mech. Behav. Biomed. Mater. 2021, 115, 104288. [Google Scholar] [CrossRef]
- Reis, A.F.; Vestphal, M.; Amaral, R.C.D.; Rodrigues, J.A.; Roulet, J.-F.; Roscoe, M.G. Efficiency of polymerization of bulk-fill composite resins: A systematic review. Braz. Oral Res. 2017, 31 (Suppl. S1), e59. [Google Scholar] [CrossRef]
- ISO 4049:2009; Dentistry-Polymer-Based Restorative Materials. International Organization for Standardization: Geneva, Switzerland, 2009.
- Ibrahim, M.S.; Alabbas, M.S.; Alsomaly, K.U.; AlMansour, A.A.; Aljouie, A.A.; Alzahrani, M.M.; Asseri, A.A.; AlHumaid, J. Flexural strength, elastic modulus and remineralizing abilities of bioactive resin-based dental sealants. Polymers 2022, 14, 61. [Google Scholar] [CrossRef]
- Ibrahim, M.S.; AlQarni, F.D.; Al-Dulaijan, Y.A.; Weir, M.D.; Oates, T.W.; Xu, H.H.K.; Melo, M.A.S. Tuning nano-amorphous calcium phosphate content in novel rechargeable antibacterial dental sealant. Materials 2018, 11, 1544. [Google Scholar] [CrossRef]
- Alshehri, A.; Alhalabi, F.; Robaian, A.; Abuelqomsan, M.A.S.; Alshabib, A.; Ismail, E.; Alzamil, F.; Alotaibi, N.; Algamaiah, H. No-Cap Flowable Bulk-Fill Composite: Physico-Mechanical Assessment. Polymers 2023, 15, 1847. [Google Scholar] [CrossRef]
- Garcia, I.M.; Balhaddad, A.A.; Aljuboori, N.; Ibrahim, M.S.; Mokeem, L.; Ogubunka, A.; Collares, F.M.; de Melo, M.A.S. Wear Behavior and Surface Quality of Dental Bioactive Ions-Releasing Resins Under Simulated Chewing Conditions. Front. Oral Health 2021, 2, 628026. [Google Scholar] [CrossRef]
- Gale, M.S.; Darvell, B.W. Thermal cycling procedures for laboratory testing of dental restorations. J. Dent. 1999, 27, 89–99. [Google Scholar] [CrossRef]
- Cayo-Rojas, C.F.; Hernández-Caba, K.K.; Aliaga-Mariñas, A.S.; Ladera-Castañeda, M.I.; Cervantes-Ganoza, L.A. Microleakage in class II restorations of two bulk fill resin composites and a conventional nanohybrid resin composite: An in vitro study at 10,000 thermocycles. BMC Oral Health 2021, 21, 619. [Google Scholar] [CrossRef] [PubMed]
- Amaireh, A.I.; Al-Jundi, S.H.; Alshraideh, H.A. In vitro evaluation of microleakage in primary teeth restored with three adhesive materials: ACTIVA™, composite resin, and resin-modified glass ionomer. Eur. Arch. Paediatr. Dent. 2019, 20, 359–367. [Google Scholar] [CrossRef] [PubMed]
- Ilie, N.; Hilton, T.J.; Heintze, S.D.; Hickel, R.; Watts, D.C.; Silikas, N.; Stansbury, J.W.; Cadenaro, M.; Ferracane, J.L. Academy of Dental Materials guidance—Resin composites: Part I—Mechanical properties. Dent. Mater. Off. Publ. Acad. Dent. Mater. 2017, 33, 880–894. [Google Scholar] [CrossRef] [PubMed]
- Aminoroaya, A.; Neisiany, R.E.; Khorasani, S.N.; Panahi, P.; Das, O.; Madry, H.; Cucchiarini, M.; Ramakrishna, S. A review of dental composites: Challenges, chemistry aspects, filler influences, and future insights. Compos. Part B Eng. 2021, 216, 108852. [Google Scholar] [CrossRef]
- Eweis, A.; Yap, A.; Yahya, N. Comparison of flexural properties of bulk-fill restorative/flowable composites and their conventional counterparts. Oper. Dent. 2020, 45, 41–51. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.-R.; Du, W.; Zhou, X.-D.; Yu, H.-Y. Review of research on the mechanical properties of the human tooth. Int. J. Oral Sci. 2014, 6, 61–69. [Google Scholar] [CrossRef]
- Van Ende, A.; De Munck, J.; Lise, D.P.; Van Meerbeek, B. Bulk-Fill Composites: A Review of the Current Literature. J. Adhes. Dent. 2017, 19, 95–109. [Google Scholar] [CrossRef]
- Rashid, H. The effect of surface roughness on ceramics used in dentistry: A review of literature. Eur. J. Dent. 2014, 8, 571–579. [Google Scholar] [CrossRef]
- Westerman, G.H.; Ellis, R.W.; Latta, M.A.; Powell, G.L. An in vitro study of enamel surface microhardness following argon laser irradiation and acidulated phosphate fluoride treatment. Pediatr. Dent. 2003, 25, 497–500. [Google Scholar] [PubMed]
- Georgiev, G.; Dikova, T. Hardness investigation of conventional, bulk fill and flowable dental composites. J. Achiev. Mater. Manuf. Eng. 2021, 109, 68–77. [Google Scholar] [CrossRef]
- Singla, M.G.; Relhan, N.; Virdi, I. Comparative Evaluation of Depth of Cure of Three High Viscosity Bulk Fill Composites versus Conventional Composite: An In Vitro Study. Int. J. Clin. Prev. Dent. 2018, 14, 145–151. [Google Scholar] [CrossRef]
- Zotti, F.; Falavigna, E.; Capocasale, G.; De Santis, D.; Albanese, M. Microleakage of Direct Restorations-Comparison between Bulk-Fill and Traditional Composite Resins:Systematic Review and Meta-Analysis. Eur. J. Dent. 2021, 15, 755–767. [Google Scholar] [CrossRef] [PubMed]
- Nainan, M.T.; Benjamin, S.; Swapna, M.U.; Koshy, S.; Kumar, A.; Nanjappa, N. Comparing marginal microleakage of three Bulk Fill composites in Class II cavities using confocal microscope: An in vitro study. J. Conserv. Dent. 2015, 18, 409–413. [Google Scholar] [CrossRef]
- Jain, K.; Katge, F.; Poojari, M.; Shetty, S.; Patil, D.; Ghadge, S. Comparative Evaluation of Microleakage of Bioactive, Ormocer, and Conventional GIC Restorative Materials in Primary Molars: An In Vitro Study Microleakage of Three Restorative Materials. Int. J. Dent. 2022, 2022, 7932930. [Google Scholar] [CrossRef]
- Omidi, B.R.; Naeini, F.F.; Dehghan, H.; Tamiz, P.; Savadroodbari, M.M.; Jabbarian, R. Microleakage of an Enhanced Resin-Modified Glass Ionomer Restorative Material in Primary Molars. J. Dent. Tehran Univ. Med. Sci. 2018, 15, 205–213. [Google Scholar]


| Material | Composition | Manufacturer | Country of Origin | Abbreviation |
|---|---|---|---|---|
| Z350 XT Filtek™ Universal Restorative | Bis-GMA, bis-EMA, UDMA, TEGDMA, silica filler, zirconia filler, zirconia/silica cluster filler | 3M | Saint Paul, MN, USA | ZXT |
| Filtek™ Bulk Fill Flowable Restorative | Bis-GMA, bis-EMA, UDMA, procrylat resins, zirconia/silica filler, ytterbium trifluoride filler | 3M | Saint Paul, MN, USA | FBF |
| Beautifil-Bulk Flowable | Bis-GMA, bis-MPEPP, UDMA TEGDMA, S-PRG fillers | Shofu INC. | Kyoto, Japan | BBF |
| Tetric™ N-Flow | Bis-GMA, UDMA, TEGDMA, silicon dioxide, mixed oxide, ytterbium trifluoride filler, barium glass | Ivoclar Vivadent | Schaan, Liechtenstein | TNF |
| Score | Degree of Dye Penetration |
|---|---|
| 0 | No dye penetration |
| 1 | Dye penetration less than half of the axial/gingival wall |
| 2 | Dye penetration more than half of the axial/gingival wall |
| 3 | Dye penetration spreading along the axial/gingival wall |
| Tukey’s Multiple Comparisons Test | Mean Difference | 95.00% CI of Difference | Below Threshold? | Summary | Adjusted p Value |
|---|---|---|---|---|---|
| TNF vs. ZXT | −13.79 | −27.29 to −0.2774 | Yes | * | 0.0443 |
| TNF vs. BBF | −17.57 | −31.67 to −3.475 | Yes | * | 0.0109 |
| TNF vs. FBF | −0.2271 | −14.32 to 13.87 | No | ns | >0.9999 |
| ZXT vs. BBF | −3.785 | −18.31 to 10.74 | No | ns | 0.8876 |
| ZXT vs. FBF | 13.56 | −0.9624 to 28.08 | No | ns | 0.0731 |
| BBF vs. FBF | 17.34 | 2.275 to 32.41 | Yes | * | 0.0200 |
| Tukey’s Multiple Comparisons Test | Mean Difference | 95.00% CI of Difference | Below Threshold? | Summary | Adjusted p Value |
|---|---|---|---|---|---|
| TNF vs. ZXT | −0.3095 | −1.153 to 0.5339 | No | ns | 0.7358 |
| TNF vs. BBF | −0.9234 | −1.814 to −0.03318 | Yes | * | 0.0403 |
| TNF vs. FBF | −0.1867 | −1.077 to 0.7036 | No | ns | 0.9349 |
| ZXT vs. BBF | −0.6139 | −1.560 to 0.3317 | No | ns | 0.2947 |
| ZXT vs. FBF | 0.1228 | −0.8228 to 1.068 | No | ns | 0.9831 |
| BBF vs. FBF | 0.7368 | −0.2509 to 1.724 | No | ns | 0.1910 |
| Tukey’s Multiple Comparisons Test | Mean Difference | 95.00% CI of Difference | Below Threshold? | Summary | Adjusted p Value |
|---|---|---|---|---|---|
| TNF vs. ZXT | 85.47 | 13.45 to 157.5 | Yes | * | 0.0155 |
| TNF vs. BBF | 1.953 | −62.46 to 66.37 | No | ns | 0.9998 |
| TNF vs. FBF | 130.8 | 61.98 to 199.7 | Yes | *** | 0.0001 |
| ZXT vs. BBF | −83.52 | −155.5 to −11.49 | Yes | * | 0.0184 |
| ZXT vs. FBF | 45.37 | −30.65 to 121.4 | No | ns | 0.3777 |
| BBF vs. FBF | 128.9 | 60.02 to 197.8 | Yes | *** | 0.0001 |
| Tukey’s Multiple Comparisons Test | Mean Difference | 95.00% CI of Difference | Below Threshold? | Summary | Adjusted p Value |
|---|---|---|---|---|---|
| TNF vs. ZXT | −72.02 | −78.42 to −65.61 | Yes | **** | <0.0001 |
| TNF vs. BBF | −23.26 | −29.67 to −16.86 | Yes | **** | <0.0001 |
| TNF vs. FBF | 11.58 | 5.176 to 17.99 | Yes | *** | 0.0002 |
| ZXT vs. BBF | 48.76 | 42.17 to 55.35 | Yes | **** | <0.0001 |
| ZXT vs. FBF | 83.60 | 77.01 to 90.19 | Yes | **** | <0.0001 |
| BBF vs. FBF | 34.84 | 28.25 to 41.43 | Yes | **** | <0.0001 |
| Groups | Score 0 n (%) | Score 1 n (%) | Score 2 n (%) | Score 3 n (%) | Total n (%) |
|---|---|---|---|---|---|
| TNF | 0 (0.0) | 0 (0.0) | 1 (12.5) | 7 (87.5) | 8 (100.0) |
| ZXT | 0 (0.0) | 2 (20.0) | 0 (0.0) | 8 (80.0) | 10 (100.0) |
| BBF | 2 (20.0) | 0 (0.0) | 0 (0.0) | 8 (80.0) | 10 (100.0) |
| FBF | 7 (70.0) | 0 (0.0) | 0 (0.0) | 3 (30.0) | 10 (100.0) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ibrahim, M.S.; AlKhalefah, A.S.; Alsaghirat, A.A.; Alburayh, R.A.; Alabdullah, N.A. Comparison between Different Bulk-Fill and Incremental Composite Materials Used for Class II Restorations in Primary and Permanent Teeth: In Vitro Assessments. Materials 2023, 16, 6674. https://doi.org/10.3390/ma16206674
Ibrahim MS, AlKhalefah AS, Alsaghirat AA, Alburayh RA, Alabdullah NA. Comparison between Different Bulk-Fill and Incremental Composite Materials Used for Class II Restorations in Primary and Permanent Teeth: In Vitro Assessments. Materials. 2023; 16(20):6674. https://doi.org/10.3390/ma16206674
Chicago/Turabian StyleIbrahim, Maria Salem, Ahmed Saleh AlKhalefah, Abdullah Ali Alsaghirat, Read Ahmed Alburayh, and Nezar Ahmed Alabdullah. 2023. "Comparison between Different Bulk-Fill and Incremental Composite Materials Used for Class II Restorations in Primary and Permanent Teeth: In Vitro Assessments" Materials 16, no. 20: 6674. https://doi.org/10.3390/ma16206674






