In-Vitro Investigation of Marginal Adaptation and Fracture Resistance of Resin Matrix Ceramic Endo-Crown Restorations
Abstract
:1. Introduction
2. Materials and Methods
2.1. Specimen Preparation
2.2. Teeth Preparation for Endo-Crowns
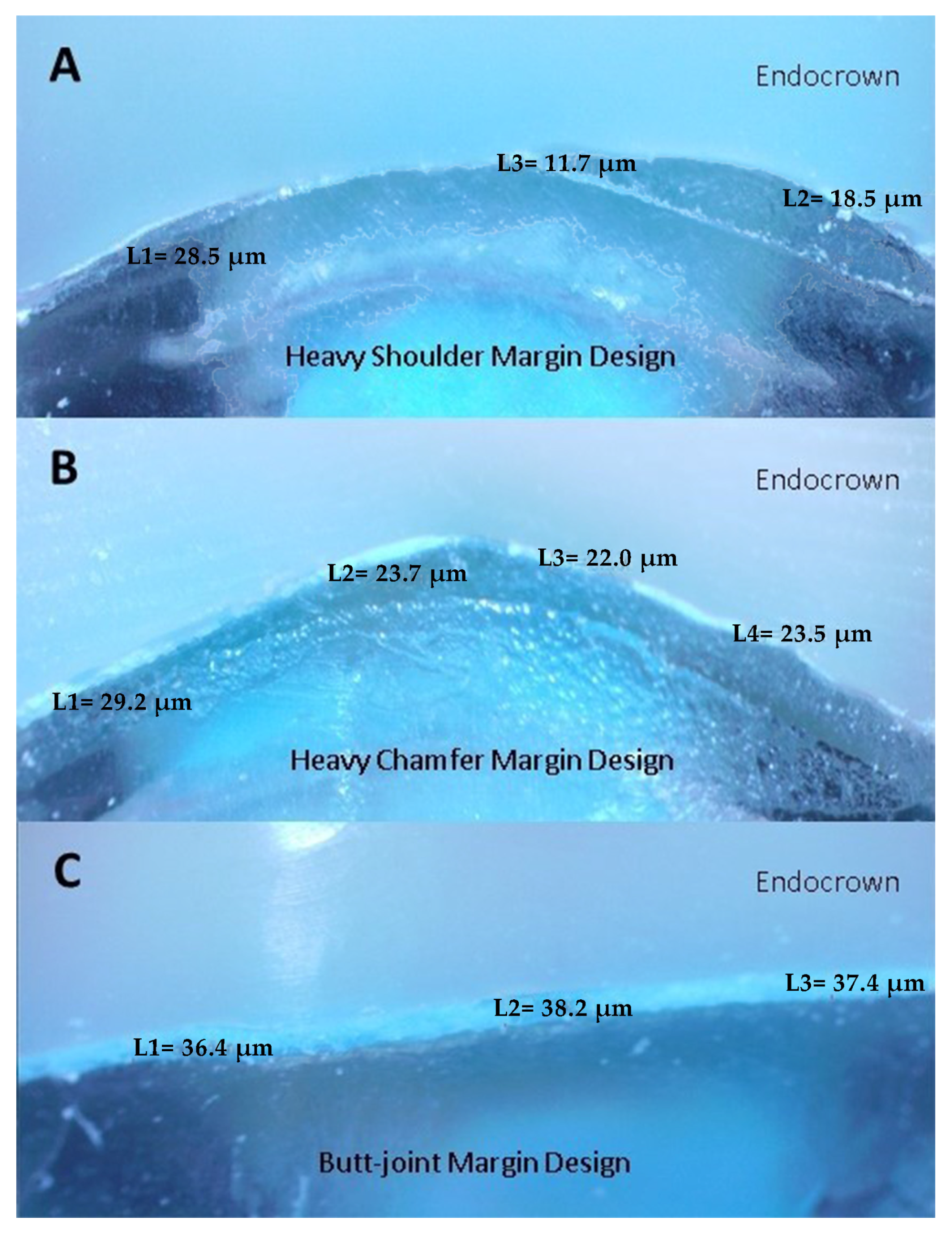
2.3. Evaluation of Marginal Adaptation before Cementation
2.4. Cementation and Fracture-Strength Test
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
- In endo-crown restorations, different margin preparations do not cause a change in the marginal adaptation. The type of material used affects the marginal adaptation.
- Except for the Ambarino High Class material, the lowest fracture resistance was observed in the butt-joint margin preparation in the other three materials, while the lowest fracture resistance was observed in the heavy chamfer margin type in the Ambarino High Class material. The marginal design to be applied in restorations using these materials should be the heavy shoulder margin design.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Biacchi, G.; Basting, R. Comparison of fracture strength of endocrowns and glass fiber post-retained conventional crowns. Oper. Dent. 2012, 37, 130–136. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Topkara, C.; Keleş, A. Examining the adaptation of modified endocrowns prepared with CAD-CAM in maxillary and mandibular molars: A microcomputed tomography study. J. Prosthet. Dent. 2021, 127, 744–749. [Google Scholar] [CrossRef] [PubMed]
- Tribst, J.P.M.; Dal Piva, A.M.O.; de Jager, N.; Bottino, M.A.; de Kok, P.; Kleverlaan, C.J. Full-crown versus endocrown approach: A 3D-analysis of both restorations and the effect of ferrule and restoration material. J. Prosthodont. 2020, 28, 335–344. [Google Scholar] [CrossRef] [PubMed]
- Elashmawy, Y.; Elshahawy, W.; Seddik, M.; Aboushelib, M. Influence of fatigue loading on fracture resistance of endodontically treated teeth restored with endocrowns. J. Prosthodont. Res. 2021, 65, 78–85. [Google Scholar] [CrossRef] [PubMed]
- Gracis, S.; Thompson, V.; Ferencz, J.; Silva, N.; Bonfante, E. A New classification system for all-ceramic and ceramic-like restorative materials. Int. J. Prosthodont. 2016, 28, 227–235. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Awada, A.; Nathanson, D. Mechanical properties of resin-ceramic CAD/CAM restorative materials. J. Prosthet. Dent. 2015, 114, 587–593. [Google Scholar] [CrossRef] [PubMed]
- Chavali, R.; Nejat, A.H.; Lawson, N.C. Machinability of CAD-CAM materials. J. Prosthet. Dent. 2016, 118, 194–199. [Google Scholar] [CrossRef]
- Günal-Abduljalil, B.; Önöral, Ö.; Ongun, S. Micro-shear bond strengths of resin-matrix ceramics subjected to different surface conditioning strategies with or without coupling agent application. J. Adv. Prosthodont. 2021, 13, 180–190. [Google Scholar] [CrossRef]
- Goldin, E.B.; Boyd, N.W.; Goldstein, G.R.; Hittelman, E.L.; Thompson, V.P. Marginal fit of leucite-glass pressable ceramic restorations and ceramic-pressed-to-metal restorations. J. Prosthet. Dent. 2005, 93, 143–147. [Google Scholar] [CrossRef]
- Conrad, H.J.; Seong, W.-J.; Pesun, I.J. Current ceramic materials and systems with clinical recommendations: A systematic review. J. Prosthet. Dent. 2007, 98, 389–404. [Google Scholar] [CrossRef]
- Nawafleh, N.A.; Mack, F.; Evans, J.L.; Mackay, J.; Hatamleh, M.M. Accuracy and Reliability of Methods to Measure Marginal Adaptation of Crowns and FDPs: A Literature Review. J. Prosthodont. 2013, 22, 419–428. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Keleş, M.A.; Metiner, C.; Türker, B. Sabit protetik restorasyonlarda marjinal adaptasyon. Eur. J. Res. Dent. 2019, 1, 35–43. [Google Scholar] [CrossRef]
- Einhorn, M.; DuVall, N.; Wajdowicz, M.; Brewster, J.; Roberts, H. Preparation ferrule design effect on endocrown failure resistance. J. Prosthodont. 2017, 28, e237–e242. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dogui, H.; Abdelmalek, F.; Amor, A.; Douki, N. Endocrown: An alternative approach for restoring endodontically treated molars with large coronal destruction. Case Rep. Dent. 2018, 2018, 1581952. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ghajghouj, O.; Taşar-Faruk, S. Evaluation of fracture resistance and microleakage of endocrowns with different intracoronal depths and restorative materials luted with various resin cements. Materials 2019, 12, 2528. [Google Scholar] [CrossRef] [Green Version]
- Lin, C.-L.; Chang, Y.-H.; Chang, C.-Y.; Pai, C.-A.; Huang, S.-F. Finite element and Weibull analyses to estimate failure risks in the ceramic endocrown and classical crown for endodontically treated maxillary premolar. Eur. J. Oral Sci. 2010, 118, 87–93. [Google Scholar] [CrossRef]
- Chang, C.-Y.; Kuo, J.-S.; Lin, Y.-S.; Chang, Y.-H. Fracture resistance and failure modes of CEREC endo-crowns and conventional post and core-supported CEREC crowns. J. Dent. Sci. 2009, 4, 110–117. [Google Scholar] [CrossRef] [Green Version]
- Sedrez-Porto, J.A.; de Oliveira da Rosa, W.L.; da Silva, A.F.; Münchow, E.A.; Pereira-Cenci, T. Endocrown restorations: A systematic review and meta-analysis. J. Dent. 2016, 52, 8–14. [Google Scholar] [CrossRef]
- Belleflamme, M.M.; Geerts, S.O.; Louwette, M.M.; Grenade, C.F.; Vanheusden, A.J.; Mainjot, A.K. No post-no core approach to restore severely damaged posterior teeth: An up to 10-year retrospective study of documented endocrown cases. J. Dent. 2017, 63, 1–7. [Google Scholar] [CrossRef]
- Hassouneh, L.; Jum’Ah, A.A.; Ferrari, M.; Wood, D.J. Post-fatigue fracture resistance of premolar teeth restored with endocrowns: An in vitro investigation. J. Dent. 2020, 100, 103426. [Google Scholar] [CrossRef]
- Attia, A.; Abdelaziz, K.M.; Freitag, S.; Kern, M. Fracture load of composite resin and feldspathic all-ceramic CAD/CAM crowns. J. Prosthet. Dent. 2006, 95, 117–123. [Google Scholar] [CrossRef] [PubMed]
- Lise, D.P.; Van Ende, A.; De Munck, J.; Suzuki, T.Y.U.; Vieira, L.C.C.; Van Meerbeek, B. Biomechanical behavior of endodontically treated premolars using different preparation designs and CAD/CAM materials. J. Dent. 2017, 59, 54–61. [Google Scholar] [CrossRef] [PubMed]
- Acar, D.H.; Kalyoncuoğlu, E. The fracture strength of endocrowns manufactured from different hybrid blocks under axial and lateral forces. Clin. Oral Investig. 2020, 25, 1889–1897. [Google Scholar] [CrossRef]
- Koenig, A.; Schmidtke, J.; Schmohl, L.; Schneider-Feyrer, S.; Rosentritt, M.; Hoelzig, H.; Kloess, G.; Vejjasilpa, K.; Schulz-Siegmund, M.; Fuchs, F.; et al. Characterisation of the filler fraction in CAD/CAM resin-based composites. Materials 2021, 14, 1986. [Google Scholar] [CrossRef]
- Yamaguchi, S.; Inoue, S.; Sakai, T.; Abe, T.; Kitagawa, H.; Imazato, S. Multi-scale analysis of the effect of nano-filler particle diameter on the physical properties of CAD/CAM composite resin blocks. Comput. Methods Biomech. Biomed. Eng. 2017, 20, 714–719. [Google Scholar] [CrossRef] [PubMed]
- Rosentritt, M.; Krifka, S.; Strasser, T.; Preis, V. Fracture force of CAD/CAM resin composite crowns after in vitro aging. Clin. Oral Investig. 2019, 24, 2395–2401. [Google Scholar] [CrossRef]
- Kassem, I.A.; Farrag, I.E.; Zidan, S.M.; ElGuindy, J.F.; Elbasty, R.S. Marginal gap and fracture resistance of CAD/CAM ceramill COMP and cerasmart endocrowns for restoring endodontically treated molars bonded with two adhesive protocols: An in vitro study. Biomater. Investig. Dent. 2020, 7, 50–60. [Google Scholar] [CrossRef] [Green Version]
- Taha, D.; Spintzyk, S.; Schille, C.; Sabet, A.; Wahsh, M.; Salah, T.; Geis-Gerstorfer, J. Fracture resistance and failure modes of polymer infiltrated ceramic endocrown restorations with variations in margin design and occlusal thickness. J. Prosthodont. Res. 2018, 62, 293–297. [Google Scholar] [CrossRef]
- Bamajboor, A.; Dudley, J. The influence of ferrule on the marginal gap and fracture resistance of zirconia endocrowns. Int. J. Prosthodont. 2022, 35, 494–501. [Google Scholar] [CrossRef]
- Kim, K.-B.; Kim, W.-C.; Kim, H.-Y.; Kim, J.-H. An evaluation of marginal fit of three-unit fixed dental prostheses fabricated by direct metal laser sintering system. Dent. Mater. 2013, 29, e91–e96. [Google Scholar] [CrossRef]
- Park, J.-Y.; Jeong, I.-D.; Lee, J.-J.; Bae, S.-Y.; Kim, J.-H.; Kim, W.-C. In vitro assessment of the marginal and internal fits of interim implant restorations fabricated with different methods. J. Prosthet. Dent. 2016, 116, 536–542. [Google Scholar] [CrossRef] [PubMed]
- Quante, K.; Ludwig, K.; Kern, M. Marginal and internal fit of metal-ceramic crowns fabricated with a new laser melting technology. Dent. Mater. 2008, 24, 1311–1315. [Google Scholar] [CrossRef]

| Material | Endo-Crown Preparation | Product | Shapes | Shades | Ref. | Lot | Composition |
|---|---|---|---|---|---|---|---|
| NANO CERAMIC HYBRID CAD/CAM MATERIAL | Butt-Joint | BRILLIANT Crios | 14 × 98.5 (mm) | A2 LT | 60022900 | J69904 | Organic part: cross-linked methacrylates(Bis-GMA, Bis-EMA, TEGDMA) Inorganic part: 70.7 wt% barium glass and amorphous silica |
| Heavy Chamfer | |||||||
| Heavy Shoulder | |||||||
| Butt-Joint | VOCO Grandio | 15 × 98.4 (mm) | A2 HT | 6058 | 2122709 | Organic part: 14% UDMA+ DMA Inorganic part: 86 wt% nanohybrid fillers | |
| Heavy Chamfer | |||||||
| Heavy Shoulder | |||||||
| Butt-Joint | AMBARINO High-Class | 15 × 98.5 (mm) | A2 | 900200 | 121020 | Organic part: 30 wt% highly cross-linked polymer blends (Bis-GMA, UDMA and BUDMA) Inorganic part: 70 wt% ceramic-like inorganic silicate glass filler particles (0.2–10 µm, average 0.8 µm) | |
| Heavy Chamfer | |||||||
| Heavy Shoulder | |||||||
| Butt-Joint | SHOFU | 14 × 98.5 (mm) | A2 LT | 2189S | 121701 | Filler composition: 61%, İncludes zirconium silicate, silicon dioxide, UDMA, TEGDMA | |
| Heavy Chamfer | |||||||
| Heavy Shoulder |
| Brilliant Crios | Voco Grandio | Ambarino High Class | Shofu | Mean | |
|---|---|---|---|---|---|
| Butt-Joint | 27.47 ± 4.95 A,a | 30.31 ± 4.36 A,a | 35.44 ± 8.08 A,a | 32.41 ± 12 A,a | 31.41 ± 8.19 A |
| Heavy Chamfer | 29.89 ± 3.39 A,a | 39.36 ± 3.84 B,b | 30.76 ± 1.98 A,ab | 38.05 ± 2.65 A,ab | 34.52 ± 5.19 A |
| Heavy Shoulder | 25.39 ± 3.66 A,a | 39.93 ± 19.15 B,b | 27.42 ± 4.67 A,a | 30.42 ± 7.07 A,a | 30.79 ± 11.67 A |
| Mean | 27.58 ± 4.34 a | 36.53 ± 12.01 b | 31.2 ± 6.28 ab | 33.63 ± 8.56 b | 32.24 ± 8.84 |
| Brilliant Crios | Voco Grandio | Ambarino High Class | Shofu | Mean | |
|---|---|---|---|---|---|
| Butt-Joint | 688.83 ± 185.88 A,b | 490.29 ± 27.93 A,ab | 711.14 ± 169.58 AB,b | 357.73 ± 154.51 A,a | 561.99 ± 206.17 A |
| Heavy Chamfer | 845.12 ± 168.86 AB,b | 834.19 ± 97.60 B,b | 517.46 ± 117.53 A,a | 682.04 ± 151.90 B,ab | 719.70 ± 199.05 B |
| Heavy Shoulder | 950.37 ± 245.12 B,b | 954.16 ± 327.80 B,b | 742.36 ± 281.50 B,ab | 718.79 ± 123.99 B,a | 841.42 ± 270.50 C |
| Mean | 828.10 ± 223.87 c | 759.54 ± 276.63 bc | 656.98 ± 231.38 ab | 586.18 ± 216.92 a | 707.70 ± 253.16 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mertsöz, B.; Ongun, S.; Ulusoy, M. In-Vitro Investigation of Marginal Adaptation and Fracture Resistance of Resin Matrix Ceramic Endo-Crown Restorations. Materials 2023, 16, 2059. https://doi.org/10.3390/ma16052059
Mertsöz B, Ongun S, Ulusoy M. In-Vitro Investigation of Marginal Adaptation and Fracture Resistance of Resin Matrix Ceramic Endo-Crown Restorations. Materials. 2023; 16(5):2059. https://doi.org/10.3390/ma16052059
Chicago/Turabian StyleMertsöz, Burak, Salim Ongun, and Mutahhar Ulusoy. 2023. "In-Vitro Investigation of Marginal Adaptation and Fracture Resistance of Resin Matrix Ceramic Endo-Crown Restorations" Materials 16, no. 5: 2059. https://doi.org/10.3390/ma16052059






