Trueness of Extraoral Digital Impressions for Full-Arch Implant Impressions—In Vitro Study
Abstract
1. Introduction
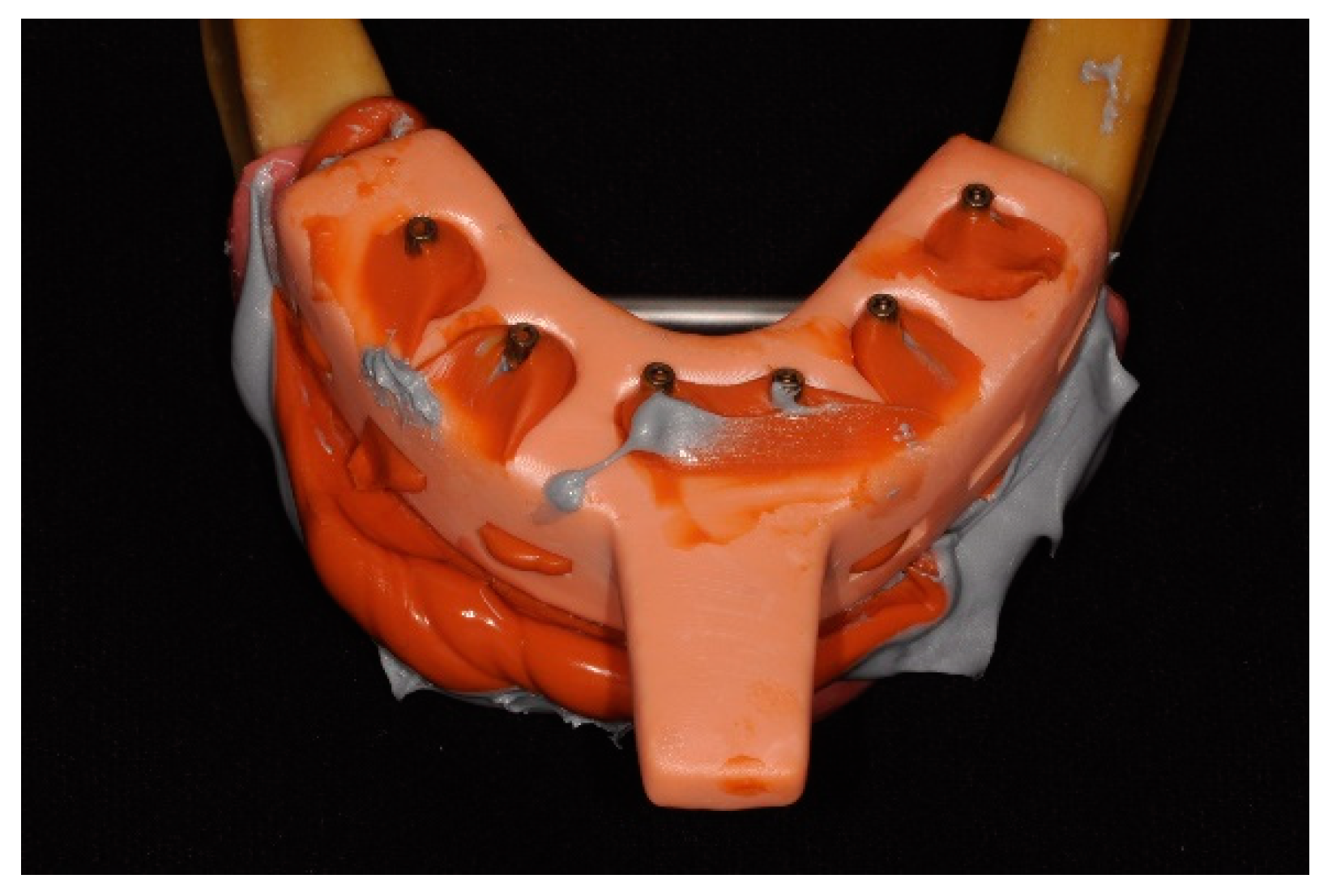
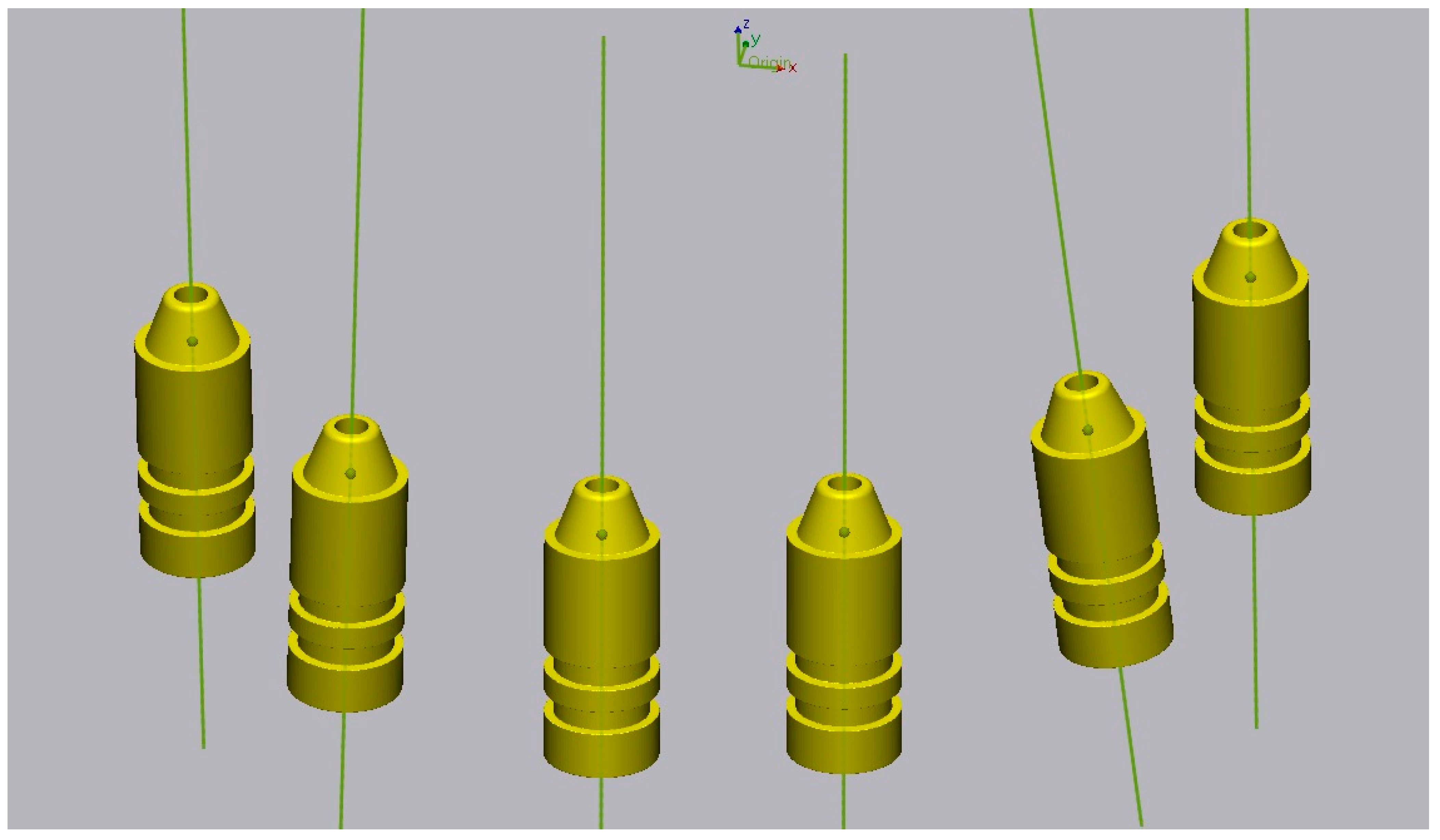
2. Materials and Methods
3. Results
4. Discussion
Limitations
5. Conclusions
- There are no statistically significant differences in the trueness between the two scanners evaluated.
- There are statistically significant differences in trueness between the two silicones evaluated in the vast majority of measured distances.
- The direct scanning of silicone impressions by laboratory scanners presents comparable results to stone cast scanning.
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
References
- da Silva Marques, D.N.; Pinto, R.J.; Alves, R.V.; Baratieri, L.N.; da Mata, A.D.; Caramês, J.M.M. Soft tissue replication in single unit implant impressions—A three dimensional clinical study. J. Esthet. Restor. Dent. 2019, 31, 359–368. [Google Scholar] [CrossRef]
- Ribeiro, P.; Herrero-Climent, M.; Díaz-Castro, C.; Ríos-Santos, J.; Padrós, R.; Mur, J.; Falcão, C. Accuracy of implant casts generated with conventional and digital impressions—An in vitro study. Int. J. Environ. Res. Public Health 2018, 15, 1599. [Google Scholar] [CrossRef]
- Menini, M.; Setti, P.; Pera, F.; Pera, P.; Pesce, P. Accuracy of multi-unit implant impression: Traditional techniques versus a digital procedure. Clin. Oral Investig. 2018, 22, 1253–1262. [Google Scholar] [CrossRef]
- Flügge, T.; van der Meer, W.J.; Gonzalez, B.G.; Vach, K.; Wismeijer, D.; Wang, P. The accuracy of different dental impression techniques for implant-supported dental prostheses: A systematic review and meta-analysis. Clin. Oral Implant. Res. 2018, 16, 374–392. [Google Scholar] [CrossRef]
- Pesce, P.; Pera, F.; Setti, P.; Menini, M. Precision and accuracy of a digital impression scanner in full-arch implant rehabilitation. Int. J. Prosthodont. 2018, 31, 171–175. [Google Scholar] [CrossRef]
- Amin, S.; Weber, H.P.; Finkelman, M.; El Rafie, K.; Kudara, Y.; Papaspyridakos, P. Digital vs. conventional full-arch implant impressions: A comparative study. Clin. Oral Impl. Res. 2017, 28, 1360–1367. [Google Scholar] [CrossRef]
- Banjar, A.; Chen, Y.W.; Kostagianni, A.; Finkelman, M.; Papathanasiou, A.; Chochlidakis, K.; Papaspyridakos, P. Accuracy of 3D printed implant casts versus stone casts: A comparative study in the anterior maxilla. J. Prosthodont. 2021, 30, 783–788. [Google Scholar] [CrossRef]
- Sorrentino, R.; Gherlone, E.F.; Calesini, G.; Zarone, F. Effect of implant angulation, connection length, and impression material on the dimensional accuracy of implant impressions: An in vitro comparative study. Clin. Implant Dent. Relat. Res. 2010, 12 (Suppl. 1), e63–e76. [Google Scholar] [CrossRef]
- Ren, X.; Son, K.; Lee, K. Accuracy of proximal and occlusal contacts of single implant crowns fabricated using different digital scan methods: An in vitro study. Materials 2021, 14, 2843. [Google Scholar] [CrossRef] [PubMed]
- Sampaio-Fernandes, M.A.; Pinto, R.; Sampaio-Fernandes, M.M.; Sampaio-Fernandes, J.C.; Marques, D.; Figueiral, M.H. Accuracy of silicone impressions and stone models using two laboratory scanners: A 3D evaluation. Int. J. Prosthodont. 2022. published online ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Sampaio-Fernandes, M.A.; Pinto, R.; Almeida, P.R.; Sampaio-Fernandes, M.M.; Marques, D.; Figueiral, M.H. Accuracy of Extraoral Digital Impressions with Multi-Unit Implants. Appl. Sci. 2023, 13, 8769. [Google Scholar] [CrossRef]
- Kontis, P.; Güth, J.F.; Schubert, O.; Keul, C. Accuracy of intraoral scans of edentulous jaws with different generations of intraoral scanners compared to laboratory scans. J. Adv. Prosthodont. 2021, 13, 316–326. [Google Scholar] [CrossRef]
- Bi, C.; Wang, X.; Tian, F.; Qu, Z.; Zhao, J. Comparison of accuracy between digital and conventional implant impressions: Two and three dimensional evaluations. J. Adv. Prosthodont. 2022, 14, 236–249. [Google Scholar] [CrossRef]
- Abou-Ayash, S.; Mathey, A.; Gäumann, F.; Mathey, A.; Donmez, M.B.; Yilmaz, B. In vitro scan accuracy and time efficiency in various implant-supported fixed partial denture situations. J. Dent. 2022, 128, 104358. [Google Scholar] [CrossRef]
- Emir, F.; Ayyildiz, S. Evaluation of the trueness and precision of eight extraoral laboratory scanners with a complete-arch model: A three-dimensional analysis. J. Prosthodont. Res. 2019, 63, 434–439. [Google Scholar] [CrossRef]
- Natsubori, R.; Fukazawa, S.; Chiba, T.; Tanabe, N.; Kihara, H.; Kondo, H. In vitro comparative analysis of scanning accuracy of intraoral and laboratory scanners in measuring the distance between multiple implants. Int. J. Implant Dent. 2022, 8, 1–9. [Google Scholar] [CrossRef]
- Alhelwani, A.; Blom, E.; Leusink, F.; Feilzer, A.J. Comparative Analysis of Intraoral Scanners and Traditional Impression Methods in Full-Arch Implantology: A Systematic Review. Med. Res. Arch. 2024, 12. [Google Scholar] [CrossRef]
- Lee, S.J.; Betensky, R.A.; Gianneschi, G.E.; Gallucci, G.O. Accuracy of digital versus conventional implant impressions. Clin. Oral. Implant. Res. 2015, 26, 715–719. [Google Scholar] [CrossRef]
- Lee, H.; So, J.S.; Hochstedler, J.L.; Ercoli, C. The accuracy of implant impressions: A systematic review. J. Investig. Clin. Dent. 2008, 100, 285–291. [Google Scholar] [CrossRef]
- ISO 12836:2015; Dentistry—Digitizing Devices for CAD/CAM Systems for Indirect Dental Restorations—Test Methods for ASSESSING Accuracy. ISO: Geneva, Switzerland, 2015.
- Jemt, T. Failures and complications in 391 consecutively inserted fixed prostheses supported by Brånemark implants in edentulous jaws: A study of treatment from the time of prosthesis placement to the first annual checkup. Int. J. Oral Maxillofac. Implant. 1991, 6, 270–276. [Google Scholar]
- Giménez, B.; Özcan, M.; Martínez-Rus, F.; Pradíes, G. Accuracy of a digital impression system based on active wavefront sampling technology for implants considering operator experience, implant angulation, and depth. Clin. Implant Dent. Relat. Res. 2015, 17 (Suppl. 1), e54–e64. [Google Scholar] [CrossRef]
- Baig, M.R.; Buzayan, M.M.; Yunus, N. Accuracy of a new elastomeric impression material for complete-arch dental implant impressions. J. Investig. Clin. Dent. 2018, 9, 12320. [Google Scholar] [CrossRef]
- Jeon, J.H.; Jung, I.D.; Kim, J.H.; Kim, H.Y.; Kim, W.C. Three-dimensional evaluation of the repeatability of scans of stone models and impressions using a blue LED scanner. Dent. Mater. J. 2015, 34, 686–691. [Google Scholar] [CrossRef]
- Arieli, A.; Adawi, M.; Masri, M.; Weinberg, E.; Beitlitum, I.; Pilo, R.; Levartovsky, S. The accuracy of open-tray vs. snap on impression techniques in a 6-Implant model: An in vitro 3D study. Materials 2022, 15, 2103. [Google Scholar] [CrossRef]


| Scanner | Material | Casts | Group |
|---|---|---|---|
| Medit | Coltene | Impressions | MCI |
| Stone Casts | MCM | ||
| Zhermack | Impressions | MZI | |
| Stone Casts | MZM | ||
| Zirkonzhan | Coltene | Impressions | ZCI |
| Stone Casts | ZCM | ||
| Zhermack | Impressions | ZZI | |
| Stone Casts | ZZM |
| Linear Distance | Positive Cases | Discrepancies > 150 µm | ||
|---|---|---|---|---|
| Frequency of Positive Cases | Frequency of Positive Cases (%) | Frequency of Discrepancies > 150 µm | Frequency of Discrepancies > 150 µm (%) | |
| M1r-P1r | 3 | 3.75% | 0 | 0% |
| M1r-I1r | 61 | 76.25% | 0 | 0% |
| M1r-I1l | 57 | 71.25% | 6 | 7.5% |
| M1r-P1l | 80 | 100% | 54 | 67.5% |
| M1r-M1l | 80 | 100% | 78 | 97.5% |
| P1r-I1r | 77 | 96.25% | 1 | 1.25% |
| P1r-I1l | 72 | 90% | 8 | 1% |
| P1r-P1l | 80 | 100% | 28 | 35% |
| P1r-M1l | 80 | 100% | 46 | 57.5% |
| I1r-I1l | 38 | 47.5% | 6 | 7.5% |
| I1r-P1l | 67 | 83.75% | 7 | 8.75% |
| I1r-M1l | 72 | 90% | 6 | 7.5% |
| I1l-P1l | 24 | 30% | 0 | 0% |
| I1l-M1l | 27 | 33.75% | 0 | 0% |
| P1l-M1l | 46 | 57.5% | 0 | 0% |
| Total | 864 | 72% | 240 | 20% |
| Medit Scanner | Zirkonzahn Scanner | |||||||
|---|---|---|---|---|---|---|---|---|
| Linear Distance | Coltene Silicone | Coltene Stone Casts | Zhermack Silicone | Zhermack Stone Casts | Coltene Silicone | Coltene Stone Casts | Zhermack Silicone | Zhermack Stone Casts |
| M1r-P1r | 56.02 [36.02; 72.02] | 42.67 [18.82; 66.52] | 53.76 [39.17; 67.76] | 46.20 [25.89; 66.50] | 69.78 [51.86; 87.70] | 50.14 [28.60; 71.68] | 57.98 [40.06; 75.90] | 54.90 [25.20; 84.60] |
| M1r-I1r | 20.02 [9.15; 30.89] | 60.99 [38.69; 83.29] | 14.05 [7.64; 20.46] | 46.33 [31.12; 61.54] | 16.39 [5.01; 27.77] | 34.52 [13.47; 55.57] | 14.89 [9.69; 20.09] | 29.66 [21.92; 37.40] |
| M1r-I1l | 25.51 [13.84; 37.18] | 55.31 [34.66; 75.96] | 47.59 [−0.79; 95.97] | 85.88 [33.07; 138.69] | 20.68 [13.44; 27.92] | 39.39 [16.81; 61.97] | 55.83 [5.68; 105.98] | 73.50 [31.54; 115.46] |
| M1r-P1l | 152.82 [125.05; 180.59] | 191.89 [162.73; 221.05] | 196.50 [163.65; 229.35] | 231.26 [188.29; 274.23] | 116.05 [95.90; 136.20] | 165.06 [129.08; 201.04] | 182.16 [149.44; 214.88] | 228.22 [196.15; 260.29] |
| M1r-M1l | 217.65 [180.38; 254.92] | 278.83 [252.34; 305.32] | 279.62 [257.02; 302.22] | 305.69 [275.09; 336.29] | 173.45 [145.77; 201.09] | 250.39 [225.73; 275.05] | 251.04 [221.26; 280.82] | 313.68 [281.99; 345.37] |
| P1r-I1r | 46.56 [32.15; 60.97] | 75.81 [38.88; 112.74] | 42.99 [34.95; 51.03] | 79.78 [49.31; 110.25] | 42.15 [27.21; 57.09] | 71.56 [40.06; 103.06] | 41.20 [26.05; 56.35] | 67.21 [41.25; 93.17] |
| P1r-I1l | 31.24 [17.13; 45.35] | 52.71 [27.02; 78.40] | 69.07 [5.82; 132.32] | 117.11 [51.06; 183.16] | 22.48 [10.43; 34.53] | 61.08 [29.62; 92.54] | 78.81 [5.13; 148.49] | 98.70 [36.61; 160.79] |
| P1r-P1l | 101.54 [78.59; 124.49] | 124.16 [93.97; 154.35] | 142.04 [96.04; 188.04] | 206.71 [157.36; 256.06] | 77.16 [56.22; 98.10] | 127.27 [92.23; 162.31] | 125.67 [75.25; 176.09] | 188.00 [139.75; 236.25] |
| P1r-M1l | 113.96 [88.04; 139.88] | 166.86 [147.77; 185.95] | 175.49 [141.83; 209.15] | 230.09 [187.58; 272.60] | 84.64 [58.12; 111.16] | 162.35 [125.13; 199.57] | 150.53 [111.55; 189.51] | 220.84 [180.73; 260.95] |
| I1r-I1l | 18.66 [8.63; 28.69] | 39.52 [13.05; 65.99] | 48.68 [−6.02;103.38] | 54.99 [7.16; 102.82] | 19.80 [10.44; 29.16] | 26.66 [8.28; 45.04] | 49.79 [−8.03; 107.61] | 65.53 [22.34; 108.72] |
| I1r-P1l | 28.09 [19.25; 36.93] | 33.48 [11.85; 55.11] | 68.10 [27.57; 108.63] | 82.92 [40.65; 125.19] | 19.11 [10.15; 28.07] | 49.56 [35.27; 63.85] | 55.70 [15.36; 96.04] | 95.35 [55.49; 135.21] |
| I1r-M1l | 24.94 [9.19; 40.69] | 64.89 [34.25; 95.53] | 86.66 [57.80; 115.52] | 85.86 [53.18; 118.54] | 123.88 [−108.47; 356.23] | 66.13 [48.53; 83.73] | 72.77 [44.20; 101.34] | 113.74 [78.38; 149.10] |
| I1l-P1l | 30.42 [20.45; 40.39] | 29.00 [10.70; 47.30] | 26.81 [15.04; 38.58] | 22.08 [3.96; 40.20] | 41.43 [28.29; 54.57] | 24.35 [11.19; 37.51] | 32.43 [15.87; 49.00] | 44.45 [31.81; 57.09] |
| I1l-M1l | 49.28 [31.22; 67.34] | 30.64 [18.75; 42.53] | 26.85 [12.63; 41.07] | 20.08 [5.30; 34.85] | 59.62 [39.13; 80.11] | 13.24 [5.43; 21.05] | 27.31 [11.93; 42.69] | 36.88 [12.25; 61.51] |
| P1l-M1l | 26.71 [12.33; 41.09] | 27.63 [7.99; 47.27] | 21.66 [9.78; 33.54] | 17.78 [9.38; 26.18] | 23.47 [13.28; 33.66] | 23.40 [11.97; 34.83] | 26.10 [14.49; 37.71] | 31.54 [17.70; 45.38] |
| Medit Scanner | Zirkonzahn Scanner | |||||||
|---|---|---|---|---|---|---|---|---|
| Angular Distance | Coltene Silicone | Coltene Stone Casts | Zhermack Silicone | Zhermack Stone Casts | Coltene Silicone | Coltene Stone Casts | Zhermack Silicone | Zhermack Stone Casts |
| M1r-P1r | 0.46 [0.38; 0.54] | 0.54 [0.37; 0.72] | 0.42 [0.27; 0.56] | 0.59 [0.34;0.84] | 0.53 [0.30; 0.76] | 0.54 [0.36; 0.72] | 0.48 [0.32; 0.65] | 0.49 [0.29; 0.69] |
| M1r-I1r | 0.13 [0.06; 0.20] | 0.21 [0.03; 0.39] | 0.24 [0.01; 0.47] | 0.33 [0.17; 0.49] | 0.29 [0.04; 0.54] | 0.09 [0.04; 0.14] | 0.19 [0.09; 0.29] | 0.15 [0.07; 0.22] |
| M1r-I1l | 0.14 [0.06; 0.22] | 0.26 [0.14; 0.38] | 0.20 [0.11; 0.29] | 0.40 [0.23; 0.58] | 0.27 [0.05; 0.49] | 0.23 [0.12; 0.34] | 0.32 [0.20; 0.43] | 0.37 [0.23; 0.51] |
| M1r-P1l | 0.18 [0.09; 0.28] | 0.26 [0.14; 0.38] | 0.25 [0.18; 0.33] | 0.38 [0.19; 0.58] | 0.23 [0.11; 0.35] | 0.17 [0.09; 0.26] | 0.24 [−0.01; 0.48] | 0.26 [0.14; 0.38] |
| M1r-M1l | 0.49 [−0.27; 1.25] | 0.26 [0.16; 0.37] | 0.25 [0.06; 0.44] | 0.29 [0.13; 0.45] | 0.30 [−0.04; 0.63] | 0.23 [0.14; 0.33] | 0.21 [0.05; 0.36] | 0.24 [0.09; 0.39] |
| P1r-I1r | 0.10 [0.04; 0.15] | 0.21 [0.09; 0.33] | 0.43 [0.10; 0.77] | 0.40 [0.11; 0.70] | 0.18 [0.07; 0.29] | 0.16 [0.05; 0.26] | 0.25 [0.11; 0.39] | 0.22 [0.10; 0.33] |
| P1r-I1l | 0.15 [0.05; 0.25] | 0.30 [0.08; 0.51] | 0.31 [0.05; 0.57] | 0.32 [0.05; 0.58] | 0.21 [0.09; 0.33] | 0.19 [0.03; 0.36] | 0.36 [0.23; 0.50] | 0.30 [0.15; 0.45] |
| P1r-P1l | 0.35 [0.24; 0.47] | 0.45 [0.28; 0.63] | 0.53 [0.19; 0.86] | 0.56 [0.30; 0.81] | 0.44 [0.14; 0.74] | 0.48 [0.35; 0.60] | 0.78 [0.29; 1.28] | 0.43 [0.25; 0.62] |
| P1r-M1l | 0.54 [−0.29; 1.37] | 0.38 [0.28; 0.49] | 0.47 [0.20; 0.74] | 0.45 [0.19; 0.72] | 0.28 [−0.05; 0.60] | 0.37 [0.22; 0.52] | 0.46 [0.20; 0.71] | 0.41 [0.21; 0.60] |
| I1r-I1l | 0.14 [0.06; 0.23] | 0.27 [0.04; 0.50] | 0.24 [0.06; 0.41] | 0.40 [0.12; 0.67] | 0.22 [0.12; 0.31] | 0.22 [0.07; 0.36] | 0.25 [0.12; 0.38] | 0.37 [0.21; 0.53] |
| I1r-P1l | 0.08 [0.04; 0.14] | 0.26 [0.07; 0.45] | 0.43 [0.13; 0.72] | 0.25 [0.04; 0.47] | 0.21 [−0.09; 0.51] | 0.18 [0.04; 0.32] | 0.44 [−0.28; 1.15] | 0.22 [0.09; 0.35] |
| I1r-M1l | 0.18 [0.05; 0.31] | 0.29 [0.13; 0.45] | 0.44 [0.18; 0.71] | 0.39 [0.20; 0.57] | 0.36 [0.03; 0.69] | 0.25 [0.13; 0.37] | 0.39 [0.27; 0.51] | 0.28 [0.15; 0.42] |
| I1l-P1l | 0.17 [0.05; 0.28] | 0.24 [0.11; 0.38] | 0.26 [0.06; 0.45] | 0.40 [0.19; 0.61] | 0.16 [0.06; 0.26] | 0.19 [0.03; 0.36] | 0.52 [−0.11; 1.15] | 0.27 [0.12; 0.42] |
| I1l-M1l | 0.32 [0.09; 0.56] | 0.32 [0.17; 0.47] | 0.27 [0.16; 0.38] | 0.55 [0.41; 0.69] | 0.29 [0.06; 0.51] | 0.33 [0.20; 0.46] | 0.52 [0.39; 0.65] | 0.61 [0.44; 0.79] |
| P1l-M1l | 0.55 [−0.06; 1.16] | 0.30 [0.07; 0.53] | 0.31 [0.18; 0.45] | 0.32 [0.09; 0.55] | 0.40 [0.27; 0.53] | 0.19 [0.07; 0.31] | 0.44 [−0.03; 0.91] | 0.28 [0.10; 0.45] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sampaio-Fernandes, M.A.; Pinto, R.; Almeida, P.R.; Sampaio-Fernandes, M.M.; Marques, D.; Figueiral, M.H. Trueness of Extraoral Digital Impressions for Full-Arch Implant Impressions—In Vitro Study. Materials 2024, 17, 2932. https://doi.org/10.3390/ma17122932
Sampaio-Fernandes MA, Pinto R, Almeida PR, Sampaio-Fernandes MM, Marques D, Figueiral MH. Trueness of Extraoral Digital Impressions for Full-Arch Implant Impressions—In Vitro Study. Materials. 2024; 17(12):2932. https://doi.org/10.3390/ma17122932
Chicago/Turabian StyleSampaio-Fernandes, Manuel António, Ricardo Pinto, Paulo Rocha Almeida, Maria Margarida Sampaio-Fernandes, Duarte Marques, and Maria Helena Figueiral. 2024. "Trueness of Extraoral Digital Impressions for Full-Arch Implant Impressions—In Vitro Study" Materials 17, no. 12: 2932. https://doi.org/10.3390/ma17122932
APA StyleSampaio-Fernandes, M. A., Pinto, R., Almeida, P. R., Sampaio-Fernandes, M. M., Marques, D., & Figueiral, M. H. (2024). Trueness of Extraoral Digital Impressions for Full-Arch Implant Impressions—In Vitro Study. Materials, 17(12), 2932. https://doi.org/10.3390/ma17122932








